What is the pancreas
The pancreas is an organ that is 16-22 cm long and is shaped like a pear, lying on its side. Inside, the organ in question consists of lobules - their cells produce all food enzymes. Inside the lobules there are islets of Langerhans - their cells secrete the hormones insulin, glucagon and somatostatin directly into the blood.
The pancreas is located at the level of the first lumbar vertebrae, but it is not located in the abdominal cavity, but in the retroperitoneal space, next to the kidneys and adrenal glands. The organ is covered at the front by the peritoneum, partially “hidden” behind the stomach, and its tail rests against the spleen - such “secrecy” makes the pancreas a rather difficult-to-reach organ for ultrasound examination. But nevertheless, an experienced ultrasound specialist will immediately see the pathological changes in the organ in question and determine the dysfunction of the pancreas itself.
Please note: the entire pancreas is covered with a capsule of connective tissue - it performs a protective function. Damage to this capsule is fraught with dangerous complications - the enzymes produced by the pancreas do not enter the duct, but into an unprotected place and begin to absorb the cells of the same organ.
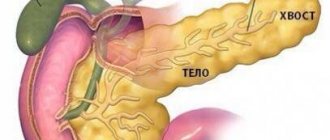
The pancreas is divided into three sections - body, tail and head.
Pancreatic cancer: statistics
According to medical statistics, pancreatic cancer ranks 4th among all deaths from cancer, and this despite the fact that the pathology in question is actually quite rare! Such a high mortality rate from pancreatic cancer is due to the fact that the pathology proceeds generally asymptomatically for a long time, and then the patient’s condition worsens, but the clinical picture remains unclear, treatment for some other diseases begins - precious time is simply lost.
The risk of pancreatic cancer increases after age 30, then increases after age 50, peaking at age 70 and older.
Pancreatic cancer always metastasizes to the liver, bone tissue, and lungs. As the tumor grows, it affects the walls of the stomach, duodenum, and large intestine.
Causes of pancreatic cancer
Cell division occurs in every organ, and during this process, mutated cells inevitably appear, with incorrect DNA - they are recognized by the immune system and destroyed as “non-native”. If the process of such recognition and destruction is disrupted, a malfunction of the immune system occurs, then the “wrong” cells that appear also begin to divide - a cancerous tumor grows. Then everything happens according to the same pattern: growing cancer cells “turn on” the protective mechanism and the body’s immune system simply cannot recognize them, and when they are accurately identified, the body is no longer able to cope with them on its own - the first symptoms of cancer appear.
Scientists have not identified any exact cause for the development of pancreatic cancer, but there are a number of risk factors that may well become a “impetus” for the appearance of a cancerous tumor. These include:
- Chronic pancreatitis. Pancreatic cells, which are in a constant inflammatory process, are the optimal environment for the emergence and division of mutating cells. The risk of developing the disease in question in chronic pancreatitis is reduced only if the pathology is put into a long-term stage of remission, and this is possible if the patient follows the diet and the doctor’s prescriptions.
- Pancreatitis of hereditary etiology. A cancer tumor develops according to the classic “scenario”, but the cause of pancreatitis is exclusively heredity.
- Diabetes. Even a slight lack of insulin leads to an increase in blood glucose levels - this is the risk of developing pancreatic cancer.
- Tobacco smoking. This is perhaps the only risk factor that can be designated as reversible. If a person gives up a bad habit, then his pancreas gets rid of ischemia - the risk of developing cancer immediately decreases.
- Overweight, obesity. In this condition, a person accumulates adipose tissue, which leads to an imbalance of sex hormones. All together can lead to the appearance of mutated cells in the pancreas.
- Nonspecific ulcerative colitis and Crohn's disease. If these pathologies occur in a chronic form and bother a person for a long time, then the pancreas will be regularly poisoned by toxic substances - they are certainly formed during the inflammatory process.
- Stomach ulcer. With this pathology, the microflora of the stomach changes, resulting in the accumulation of toxic compounds in the organs of the gastrointestinal tract. Even if a person has been operated on for a gastric ulcer, the risk of developing the disease in question remains very high.
In addition to these factors, it is worth highlighting poor nutrition - there are some studies that suggest an increased risk of developing pancreatic cancer when consuming certain foods in large quantities. Such dangerous products include, in particular:
- processed meat - sausages, sausages, ham, balyk, bacon and more;
- grilled red meat;
- fatty food.
We recommend reading: Are meat and meat products harmful: the official position of WHO?
Some doctors and scientists argue that several more positions can be considered risk factors:
- person's age over 60 years;
- diseases of the oral cavity - for example, gingivitis, caries, pulpitis;
- direct contact with dyes and toxic substances - this factor is especially common among metallurgy workers;
- allergic diseases that occur in a chronic form - for example, atopic dermatitis, eczema;
- low physical activity of a person;
- already diagnosed cancer of other organs - pharynx, mammary glands, intestines, lungs, ovaries, bladder, kidneys;
- the presence of cancer pathology in close relatives.
Doctors consider chronic pancreatitis, pancreatic adenoma, and organ cyst to be precancerous conditions.
Why does the disease occur?
You will learn about the causes and prevention of pancreatic cancer in the following video:
A number of negative factors lead to pancreatic cancer, such as pancreatic head cancer (PGC). These include:
- An unbalanced and harmful diet associated with excessive consumption of protein and fatty animal foods. In addition, some products may contain carcinogens that contribute to the development of cancer.
- Use of tobacco products. Nicotine as a whole has a negative effect on the body, and not just on the pancreas and especially on its head.
- The presence of high blood sugar and insulin resistance. As a rule, patients who have such deviations in the functioning of the body also have a violation of the structure of epithelial tissues. The latter line the ducts of the gland, and due to diabetes mellitus they are transformed, increasing the risk of developing infection in the internal tissues.
- Presence of pancreatitis. In its chronic form, this disease can lead to a change in the qualitative composition of the head, which leads to atypical cell division in the diseased area.
- Dysfunction of the bile ducts. To date, a relationship has been identified between existing deposits of stones in the bile ducts and the formation of a tumor on the head of the pancreas.
- Genetic predisposition. Heredity is an important factor in assessing the risk of developing PCa.
- Age-related changes in the body and other reasons. Advanced age increases the risk of developing prostate cancer, especially in men. In addition, according to statistics, representatives of the Negroid race are susceptible to this pathology.
However, the listed reasons do not always play a decisive role in the formation of the disease. Sometimes the cause of the disease remains unclear.
Classification of pancreatic cancer
It is very important for the doctor to understand from which cells pancreatic cancer developed - both the clinical picture of the disease and the properties of the tumor will depend on this. There is the following classification:
- acinar cancer - cancer cells have the appearance of a bunch of grapes;
- mucinous cystadenocarcinoma - occurs when a pancreatic cyst degenerates, more often diagnosed in women;
- Ductal adenocarcinoma - the most common type of tumor, develops in the cells that line the pancreatic ducts;
- squamous cell carcinoma - a type of disease that is extremely rare; the tumor develops directly in the duct cells;
- glandular squamous cell carcinoma - arises from two types of cells at once: those that produce enzymes and those that form excretory ducts;
- Giant cell adenocarcinoma is a collection of cystic cavities that are filled with blood.
Please note: there is also undifferentiated pancreatic cancer - the most dangerous type of the disease in question, which progresses rapidly and always ends quickly in death.
In the case of cancer development in the endocrine pancreas, its classification will be as follows:
- Insulinoma – excessive amounts of insulin are produced, which reduces blood glucose levels;
- glucagonoma - the hormone glucagon is produced in large quantities, which increases blood glucose levels;
- gastrinoma - the hormone gastrin is produced, which is designed to stimulate the activity of the stomach.
Most often, pancreatic cancer is localized in the head of the organ. But in general there is a classification of the disease in question according to its location:
- pancreatic tail cancer;
- pancreatic head cancer;
- carcinoma of the body of the organ in question.
Causes
According to research, pancreatic cancer is more common in men than in women, but the definitive and unambiguous cause of this malignant tumor has not been established, however, it is known that the risk of the disease increases with the age of the patient. There are some factors and diseases that can influence the formation of pancreatic cancer, namely:
• chronic pancreatitis;
• diabetes;
• non-healing or poorly treated ulcers;
• smoking;
• excessive consumption of strong alcoholic beverages (especially in combination with smoking);
• diet – the development of pancreatic cancer is promoted by the consumption of large amounts of animal fats and carbohydrates;
• environmental pollution;
• contact with pesticides, benzidine and methylene chlorides.
In addition, tumor inheritance plays an important role. Pancreatic cancer is believed to be a disease acquired due to a gene mutation. Mutant genes lead to uncontrolled cell proliferation, while losing the function of repairing damaged DNA fragments. Identification of defective genes in a given patient allows appropriate procedures and diagnostics to be carried out.
Pancreatic head cancer
At the very beginning of its development, this type of tumor does not have any symptoms. But the first manifestations of this dangerous disease include:
Abdominal pain. It can be “in the pit of the stomach” and at the same time in the hypochondrium; pain radiates to the back. The intensity of pain increases at night, the patient feels better if he tilts his torso slightly forward or takes a lying position with his knees bent.
- Redness of one or another vein in the lower/upper extremities periodically appears. Blood clots may well form in the veins, so part of an arm or leg may suddenly turn blue.
- Without following any diet, the patient begins to lose weight sharply.
- After eating, there is a feeling of heaviness in the pit of the stomach.
- The patient complains of increased fatigue, drowsiness and general weakness.
As the tumor grows, other signs of pathology appear:
- Jaundice begins. Moreover, at first the patient may not even suspect its presence; well, occasionally he will notice yellowing of the eye sclera - nothing more. But as the disease in question progresses, the patient’s skin becomes not just yellow, but greenish-brown.
- The skin of the whole body itches constantly. Such intense itching is associated with congestion in the gallbladder - bile is simply deposited in the skin and causes such a reaction in the body.
- Urine takes on a dark tint, and feces become almost colorless.
- The patient completely loses his appetite and develops complete intolerance to meat and fats.
- There are digestive disorders - nausea, vomiting, changes in stool.
- The stool becomes greasy (it is shiny), runny and smelly.
Cancer of the body or tail of the pancreas
Symptoms of advanced cancer will include the following changes:
- A large amount of urine excreted, constant thirst, dry mouth, frequent urination at night are signs identical to diabetes mellitus.
- Fatty stools, pain in the upper abdomen, nausea, decreased or complete lack of appetite, weight loss are signs identical to chronic pancreatitis.
- The appearance of stickiness in the corners of the mouth, weight loss, a smooth surface and intense red color of the tongue, pallor of the skin, rashes on the upper and lower extremities, the development of dermatitis and eczema - these signs are present only in the case of progression of glucagonoma.
- Pain in the pit of the stomach after eating, a feeling that the stomach is standing still, constant diarrhea, greasy stool and difficult to flush from the toilet are signs that appear as gastrinoma progresses.
In addition, you need to highlight a few more symptoms of cancer of the body or tail of the pancreas:
- menstrual cycle disorders in women;
- wounds on the skin surface heal extremely slowly;
- trophic ulcers form on the lower extremities;
- sexual desire is sharply reduced or completely absent;
- red spots periodically appear on the skin, which are often mistaken for allergies;
- the occurrence of “hot flashes” to the face and upper extremities;
- spasms periodically occur in the face and legs, but without loss of consciousness;
- heaviness is clearly felt in the left hypochondrium.
It can be concluded that pain in the upper abdomen, fatty stools and weight loss are the main signs of pancreatic cancer, regardless of which part of the organ the tumor develops in.
How does the disease manifest?
As already mentioned, it can be difficult to clearly identify the disease in the early stages of development. This is due to the fact that most of the symptoms during this period, when the treatment process can still bring the desired effect, are either blurred or not defined. Only when the tumor grows to the point of being able to penetrate vital organs can we talk about any specific symptoms. These include the presence of:
- Pain symptom. It is noted by the majority of patients (more than 85%). It manifests itself in the upper zone of the peritoneum, responding in the upper back. This occurs due to pressure on the nerve endings and bile ducts from the enlarged tumor. It also leads to an inflammatory reaction. Most often, this symptom occurs during night sleep and after eating.
- Dyspeptic disorders. Due to disruption of the pancreas, there is a lack of the main enzymes that it produces. In addition, the activity of the gastrointestinal tract is disrupted, which together leads to weight loss. The vast majority of patients begin to lose a lot of weight.
- Discoloration of stool. The symptom occurs due to compression of the bile ducts and is interpreted as obstructive jaundice. With it, feces are deprived of a specific pigment - stercobilin, which is a product of bilirubin metabolism, but contain fats and unprocessed fiber.
What can the color of stool tell you? See the picture:
- Nose and intestinal bleeding. The negative impact that the tumor has on the body is also expressed in changes in blood composition. In particular, the blood's normal ability to clot is lost. Compression of the spleen, tumor growth into the digestive organs and disorders in the liver lead to bleeding in the intestines.
- Pulmonary infarction. Most often occurs in the final stage of the disease. It leads to complete destruction of bronchial and pulmonary tissues.
In addition to these symptoms, in the early stages of the disease a person may experience nausea, complete or partial loss of appetite, severe fatigue, and weakness. He may vomit for no reason, belch, dry mouth, and a constant feeling of heaviness in the abdomen.
In some cases, patients develop an accumulation of fluid in the abdominal cavity, which also indicates a developing pathology of the pancreas. This process may be accompanied by the formation of blood clots in the lower extremities, as well as dysfunction of the cardiovascular system and liver failure.
In the latter cases, you must definitely seek medical help, because urgent hospitalization is required.
Metastasis of pancreatic cancer
The disease in question very actively disperses its cancer cells throughout the human body. And this can happen in three ways:
- Through the circulatory system. Thus, cancer cells enter the liver, kidneys, bone tissue, brain, lungs - almost all internal organs.
- Through the lymphatic system. Here, the process of the tumor dispersing its malignant cells occurs in several stages:
- First, the lymph nodes that are located directly around the pancreas are attacked by cancer cells;
- then the tumor spreads to the lymph nodes, which are located behind the pancreas - most often at the junction of the stomach and the duodenum;
- then the lymph nodes, which are located in the mesentery (upper section), begin to be affected;
- the last stage of dispersal promotes the penetration of cancer cells into the lymph nodes located in the retroperitoneal space.
- Along the peritoneum. Cancer cells invade the intestinal walls, the peritoneum itself, and the pelvic organs.
There is such a thing as penetration of a pancreatic tumor - cancer grows into organs located adjacent to an already affected gland. For example, if cancer develops in the tail of the gland, then its cells can grow into the spleen, and if the cancer is localized in the head of the organ, then the tumor will spread to the stomach and bile ducts.
Treatment tactics and prognosis
Not all patients diagnosed with pancreatic cancer can undergo complex multi-stage treatment. For example, if there is already a decompensated course of kidney or liver disease, this significantly limits the possibilities of drug treatment of the tumor.
The formation of a primary focus of cancer in the tail of the gland, or its large size, growth into the nearest veins and arteries will also complicate the preparation of an optimal treatment regimen. Without surgical excision of cancer in the pancreatic tissue, people live no more than 4–6 months. Whereas after surgery at stages 1–2 of the disease, life expectancy is more than two years, provided there is no recurrence of cancer.
If experts recommend an exclusively palliative treatment regimen - vitamins, hepatoprotectors, enzymes, sedatives and analgesics, a person has no more than 2-3 months to live. During this period, relatives should provide him with full support and assistance. Because it becomes more and more difficult for the patient to take care of himself. He already expects a lethal outcome as relief from excruciating pain and extremely poor health.
How pancreatic cancer develops
There are 4 stages of the disease in question - for each of them there are features of the course.
Stage 0 pancreatic cancer
This stage is completely asymptomatic; the mutated cells have just begun to exist and can grow deeper into the organ. If at this stage a person undergoes surgical treatment, then the chances of completely getting rid of cancer are 99%.
Diagnosing pancreatic cancer at this stage can only be done using ultrasound or computed tomography.
Stage 1 pancreatic cancer
IA - a cancerous tumor is localized exclusively in the pancreas and has a size of less than 2 cm. As a rule, the patient does not notice any symptoms, the only exception is the case of localization of a malignant disease in the area of the exit into the duodenum. With this development of events, the patient will indicate nausea and periodic diarrhea if the diet is not followed.
IB – the tumor is also located within the pancreas, its size becomes more than 2 cm. If the cancer is localized in the head of the organ, the patient will experience jaundice, diarrhea and nausea, and mild pain in the left hypochondrium. If a malignant tumor develops in the body or tail of the organ, then symptoms characteristic of glucagonoma, insulinoma or gastrinoma will appear.
Stage 2 pancreatic cancer
IIA - the cancerous tumor has spread beyond the pancreas and grown into the duodenum and bile ducts.
IIB – the tumor can have absolutely any size (even small), but its cells have already dispersed to nearby lymph nodes. This fact does not produce any additional symptoms; the patient complains of weight loss, pain in the upper abdomen, diarrhea and vomiting.
Stage 3 pancreatic cancer
The cancer is already widespread. At this stage, malignant cells are found in the stomach, large blood vessels, spleen, and large intestine. In some cases, cancer cells are also present in regional lymph nodes.
Stage 4 pancreatic cancer
The most severe stage of the disease in question, when cancer metastases are found in very distant organs - lungs, brain, ovaries and others.
Stage 4 pancreatic cancer has several distinctive symptoms:
- pain in the upper abdomen is pronounced and has a girdling character;
- the patient is exhausted due to complete refusal to eat;
- the liver is enlarged and this provokes pain and heaviness in the area of its anatomical location;
- Fluid accumulates in the abdomen;
- the skin simultaneously becomes pale and yellow;
- the spleen is enlarged, which provokes acute pain in the right hypochondrium;
- Soft nodules appear under the skin.
If at stage 4 there are cancer metastases in the liver, the following signs will be present:
- the whites of the eyes and skin acquire a stable yellow color;
- gums and mucous membranes begin to bleed;
- feces become colorless, urine becomes intensely dark in color;
- Fluid accumulates in the abdomen - ascites develops;
- The patient's mouth constantly has an unpleasant odor.
Please note: with liver metastases at stage 4 of pancreatic cancer, even with ultrasound and computed tomography it is extremely difficult to determine which cancer is primary. This can be done only by the procedure of histological examination of tissue fragments of the affected organs.
Damage to brain metastases at stage 4 of the disease in question is characterized by the following changes:
- behavior becomes inappropriate, personality changes almost completely;
- the muscle tone of the limbs changes and, as a rule, this occurs only on one side;
- smell, sight and taste are weakened;
- the patient is unable to perform some simple actions;
- skills acquired during work are lost;
- the patient's voice becomes nasal;
- the face becomes asymmetrical;
- speech is incomprehensible to others.
If cancer cells penetrate the lungs, shortness of breath will be present even at absolute rest, a dry paroxysmal cough, and hemoptysis (in the event of a ruptured blood vessel).
Metastases to bone tissue are manifested by severe pain in the bones - it is especially pronounced with a simple, light tap on the skin at the location of the affected bone.
Predictions at the first stage
Of course, the prediction of living with an oncological process in the gland entirely depends on the stage of the pathology. The value will depend on the patient’s age, the speed of development of cancer cells, general condition, and the number of secondary cancerous formations on nearby organs.
The best prognosis is when diagnosis and treatment are carried out at the first stage of cancer, the formation has not yet left the organ area, and there are no metastases. In the case of a terminal tumor, a couple of months pass from the onset of symptoms to death from the moment the disease is detected.
The first stage of oncology in pancreas IA is characterized by a small tumor, up to 2 cm, that does not extend beyond the edges of the gland. With pathology, the patient does not develop any symptoms, except in the case when the formation is formed in the area of the exit of the duodenum. Then the patient will feel sick, and diarrhea will periodically appear when the diet changes.
Initial stage IB - the tumor is also present in the pancreatic area, but its size is already more than 2 cm. If the cancer is localized in the head of the organ, the patient will complain of the following symptoms:
- diarrhea;
- nausea;
- slight pain under the left rib;
- the skin will turn yellow.
yellowing of the skin
If there are malignant cells in the body or tail region, signs characteristic of insulinoma, glucogonoma, and gastrinoma will appear.
To eliminate the pathology, surgical intervention is allowed. After the manipulation, people who follow all the doctor’s orders live for a long time. However, complete recovery with surgery is not 100% guaranteed.
Prognosis for pancreatic cancer - 2-5% of victims experience good dynamics if the tumor focus is surgically removed in a timely manner. In the future, the patient needs replacement treatment, which includes the use of enzyme agents in order to maintain the proper level of food digestion processes.
The fatal outcome after surgery does not exceed 10%. About 45% of patients live 5 years.
If the cancer is localized in a hard-to-reach area of the gland, or the lesion is large even at the initial stage, surgical treatment may not be possible. In this situation, the patient will be offered chemotherapy and radiation therapy.
Benign tumors of the pancreas often have a favorable prognosis, because only in rare cases do they degenerate into a low-quality neoplasm. When the formation increases in volume, complications such as jaundice and intussusception may occur. If the tumor is removed in a timely manner, it is possible to be cured completely.
intussusception
Diagnostic measures
To make a diagnosis of pancreatic cancer, the doctor will conduct a complete examination of the patient. The following types of tests will help in diagnosis:
- determination of tumor marker in the blood;
- pancreatic elastase in feces;
- blood alkaline phosphatase;
- insulin level;
- pancreatic amylase in urine and blood;
- levels of glucagon and gastrin in the blood.
These tests will only help the doctor suspect advanced pancreatic cancer. General blood and urine tests, coagulation tests and liver tests will help you find out how much homeostasis has changed.
The exact diagnosis is made based on the results of the following examinations:
- Ultrasound examination of the abdominal cavity - allows you to determine only the location of the cancerous tumor that will need to be studied.
- Computed tomography allows you to examine the pancreas in detail; the procedure is very effective.
- Magnetic resonance imaging is a more informative study compared to computed tomography. Allows you to study the condition of the kidneys, liver, gallbladder and other abdominal organs along with the pancreas.
- Endoscopic retrograde cholangiopancreatography. It is performed using an endoscope and injecting a contrast agent into the pancreatic ducts.
- Positron emission tomography. A modern research method that gives accurate results. A contrast agent (sugar isotopes) is injected into the patient’s vein and the study is carried out based on its accumulation in the organs.
- Endoscopic retrograde cholangiography. Under the control of an ultrasound machine, the doctor makes a puncture in the liver and injects a contrast agent into it. After this, you can begin the examination.
- Laparoscopy. It is also performed through a puncture into which a probe is inserted, allowing one to examine the condition of the pancreas; if necessary, the doctor will perform a biopsy procedure - taking a fragment of organ tissue for histological examination.
Please note: Until the results of the biopsy are received, no doctor can make a diagnosis of pancreatic cancer. Therefore, when conducting research using an endoscope or by laparoscopy, a specialist must take a fragment of organ tissue for histological examination.
Diagnostics
Detection of a pancreatic tumor at the initial stage has certain difficulties due to the lack of specific symptoms. Only in 30% of cases the detected cancer lasts less than 2 months. Laboratory research methods:
- General blood analysis. There are signs of anemia, increased platelets, and accelerated ESR. Blood biochemistry shows bilirubinemia, increased activity of alkaline phosphatase, liver enzymes with narrowing of the bile ducts and metastasis. There may be signs of developed malabsorption syndrome.
- Determination of tumor markers: The CA-19-9 marker is determined to resolve the issue of tumor selectivity. It is not detected at an early stage in pancreatic cancer.
- Carcinoembryonic antigen. Is detected in half of patients. It is worth noting that this marker can also be positive in chronic pancreatitis and ulcerative colitis.
- Ca-125. It is observed in half of the patients.
- At later stages, tumor antigens CF-50, CA-242, CA-494 and others may appear.
Instrumental diagnostic methods:
| Diagnostic method | What makes it possible to identify |
| Ultrasonography | Allows you to exclude diseases of the gallbladder and liver and detect a tumor. With endoscopic ultrasound, it is possible to collect material for research |
| CT and MRI | Visualizes gland tissue, detects tumor diseases from 1 cm in size, assesses the condition of the abdominal organs, the presence of metastases and enlarged lymph nodes |
| PET (positron emission tomography) | Makes it possible to determine the presence of cancer cells and metastases |
| ERCP | Detects tumors of any part of the pancreas starting from a size of 2 cm. The procedure is invasive and contributes to the development of complications |
| Diagnostic laparoscopy | Allows detection of small metastases in neighboring organs |
Treatment methods for pancreatic cancer
Treatment of the disease in question is selected on a strictly individual basis - it all depends on the size of the tumor, how much it has grown into the organ, and whether there are metastases. The ideal treatment option would be to remove the cancerous tumor and further irradiate the area with gamma rays. But this option is only possible if pancreatic cancer is diagnosed at stage 0 or stage 1 of development. In all other cases, specialists carry out combined treatment.
Surgical treatment of pancreatic cancer
The following types of operations are performed:
- Operation Whipple. The head of the pancreas (along with the tumor), part of the duodenum, gallbladder and stomach are removed. Such surgical intervention is carried out only in the initial stages of the development of the disease in question, and the patient should not think too long about agreeing to carry out such work - time is too precious.
Complete removal of the pancreas. It is advisable to carry out such an operation in case of growth of a cancerous tumor inside an organ, when it has not yet spread beyond its limits.
- Segmental resection. Only the central part of the pancreas is removed along with the tumor. The remaining two parts are sewn together using an intestinal loop.
- Distal resection. If the cancer is localized in the tail and body of the pancreas, then they are removed, and the head is left.
- Endoscopic stent. If the tumor is inoperable and blocks the bile duct, then a tube is inserted into it, through which bile will flow either into the small intestine or into a special plastic reservoir attached to the outside of the body.
- Gastric bypass surgery. It is advisable to carry out such surgery only if the tumor grows and puts pressure on the stomach, when food cannot enter the intestines. Doctors simply stitch up the stomach and intestines, bypassing the malignant tumor.
If the pancreatic tumor is no longer amenable to any treatment, then doctors can perform palliative operations, which should make life easier for the patient. These include:
- removal of part of the malignant tumor - pressure on nearby organs and nerve endings is relieved;
- removal of metastases;
- elimination of obstruction of the bile ducts and/or intestines;
- elimination of perforation of the wall of the stomach, intestines or the diseased organ itself.
Operations are carried out either using the classical method using a scalpel, or with a gamma knife - this allows not only to remove the tumor, but also to irradiate nearby tissues. In this case, if any cancer cells remain, they are destroyed.
After surgery, radiation or chemotherapy is required.
Chemotherapy for pancreatic cancer
It is carried out with specific drugs that suppress the growth and division of cancer cells. Unfortunately, these drugs also affect healthy cells, which leads to severe side effects - hair loss, constant nausea, neuroses, and frequent infectious pathologies.
There are two types of chemotherapy:
- monotherapy – the patient is prescribed only one drug, the effectiveness of such treatment is 15-30%;
- polychemotherapy - doctors combine different drugs, the effectiveness is 40%.
In order for the patient to endure this type of treatment more or less without consequences, he is given a special diet that includes fermented milk products and abstinence from alcoholic beverages and heavy foods, is recommended to visit a psychologist, and is prescribed antiemetic drugs.
Targeted therapy
A modern type of treatment for pancreatic cancer, which involves taking medications that act exclusively on cancer cells without affecting healthy tissue. Of course, this method of treatment is very effective and well tolerated by patients, but its cost is too high.
Radiation therapy for pancreatic cancer
The tumor is irradiated:
- before surgery – the size of the cancer tumor decreases;
- during surgery and after it - this will prevent relapses;
- in case of an inoperable tumor, the patient’s condition is alleviated and the growth of cancer cells is stopped.
New drugs are constantly being developed to help humanity cope with cancer - for example, scientists from the USA have already developed a vaccine that infects only cancer cells. This vaccine contains radioactive particles, which are designed to destroy malignant cells.
Prognosis for pancreatic cancer
In general, the prognosis for pancreatic cancer is extremely unfavorable. And this is due to the fact that the disease in question grows rapidly, without showing any symptoms.
According to statistics, the following conclusions can be drawn:
If the cancer tumor has already spread beyond the pancreas, then only 20% of patients live more than 5 years. And such a prognosis is valid only if the patient undergoes active treatment.
- If no surgical intervention was performed for the disease in question, then patients live no more than 6 months.
- During a course of chemotherapy, patients with pancreatic cancer live about 6-9 months.
- Radiation therapy without surgery prolongs the patient's life only by 12-13 months.
- If a radical operation was performed, then patients live for another 2 years, but the five-year survival rate is only 8%.
- If doctors already perform palliative operations, then patients will live for a maximum of another year.
Please note: if pancreatic cancer was diagnosed at stage 4 of development, then doctors give a prognosis for only one year, and then no more than 5% of all patients survive until this period. The stronger the pain and poisoning by cancer tumor toxins, the shorter a person’s life!
The cause of death for pancreatic cancer is liver, kidney or heart failure.
Treatment
The only viable treatment for pancreatic cancer is surgery. However, such an operation is possible only in 20% of patients.
Some patients with surgically borderline pancreatic tumors may receive neoadjuvant treatment to make surgery easier and improve the patient's prognosis.
Treatment for metastatic disease (generalized disease) is based on chemotherapy. The general condition of the patient is a decisive factor when choosing treatment.
Almost 80% of patients with pancreatic cancer go to the doctor too late, then only palliative treatment remains, which improves the quality of life and alleviates unpleasant symptoms. The type and extent of surgery depends on the location of the tumor and the severity of the disease. During the operation, the nerves of the visceral plexus are destroyed, due to which the pain is significantly reduced. Another method is decompression of the biliary and digestive tracts by connecting the bile ducts to the intestines. If surgery is not possible, the patient takes strong painkillers.
During treatment, the patient is advised to eat frequent meals that are high in calories and protein, but low in fat. In addition, proper irrigation and administration of pancreatic enzymes are important. In some cases, parenteral nutrition is also necessary.
Preventive measures
This terrible disease, pancreatic cancer, is entirely preventable! Doctors recommend:
- Stop smoking. All changes in human organs that occur when smoking are reversible.
- Avoid foods high in sugar and give preference to non-starchy fruits and vegetables.
- Do not abuse foods from the protein group, and periodically arrange protein-free fasting days for yourself.
- The diet should include cabbage - white cabbage, Savoy, Brussels sprouts.
- Regularly consume raspberries, pomegranates, wild strawberries and strawberries.
- You need to eat fish and milk, dairy products.
- Red meat, egg yolk and offal are dangerous for the pancreas.
- Be sure to monitor the intake of vitamins in the body and, if necessary, increase nutrition or take vitamin-mineral complexes.
Pancreatic cancer is a terrible disease that takes lives almost instantly. In order to timely detect the presence of cancer cells in this organ, you just need to undergo regular examinations with doctors - this will allow treatment to be carried out at the very beginning of the development of pathology.
Tsygankova Yana Aleksandrovna, medical observer, therapist of the highest qualification category
20, total, today
( 189 votes, average: 4.51 out of 5)
The first signs of lung cancer
Brain surgeries: types, complications, rehabilitation