What is uterine fibroid
Uterine fibroids are a benign hormone-dependent tumor in the form of a node(s) arising from the muscular layer of the uterus (myometrium).
A node is a round formation of smooth muscle fibers with a diameter from several millimeters to tens of centimeters. The weight of fibroids varies greatly, but in rare advanced cases it reaches 50 kilograms. Uterine fibroids do not become cancerous, but women with uterine fibroids are more likely to develop cervical cancer than those without. Uterine fibroids are the most common gynecological disease on Earth. Every 3rd woman after 35 years suffers from it.
Among the many possible causes of nodule formation, female hormonal imbalance is identified, primarily due to irregular sex life, lack of childbirth and breastfeeding, chronic diseases of the genital organs and urogenital infections.
The disease is manifested by pain in the lower abdomen, uterine bleeding, spontaneous abortion, disruption of the activity of the female genital and nearby organs.
Uterine fibroids rarely go away on their own. Conservative (including medication) and/or surgical treatment is required, including removal of nodes (myomectomy) and uterus (hysterectomy). Without treatment, complications occur in half of the cases: polyps in the uterus, torsion of the tumor stalk, malnutrition of the node with tumor necrosis, prolonged and heavy uterine bleeding with anemia, ectopic pregnancy, infertility, ovarian cancer.
Myoma often complicates the course of pregnancy.
Pregnancy and uterine fibroids
The course of pregnancy after conservative removal of uterine fibroids very much depends on the surgical technique performed.
If surgery for uterine fibroids was accompanied by coagulation (cauterization) of the bed of the myomatous node without suturing it, then the risk of uterine rupture during pregnancy is very high. And this is accompanied by massive bleeding, which can be fatal for the woman and cause the death of the fetus.
However, even if correct suturing was performed, the risk of rupture at the end of pregnancy and during childbirth also exists, but it is much lower. Therefore, such women require constant attention from obstetricians.
If pregnancy occurs against the background of existing fibroids, then the risk of pregnancy complications not associated with the presence of a scar on the uterus increases:
- Placental insufficiency, disrupting the normal development of the baby.
- Threat of interruption.
- Incorrect location of the placenta and its detachment.
During childbirth, the likelihood of weak labor forces, bleeding and acute fetal hypoxia increases. Therefore, if fibroids are diagnosed, it is first recommended to treat it (the best option at present is medication, i.e., Esmiya), and then plan a pregnancy.
Causes of uterine fibroids
Not fully established, but predisposing pathological factors are identified:
- late onset of menstruation;
- absence of childbirth, breastfeeding until 33 years of age;
- abortions;
- incorrect medicinal contraception;
- chronic gynecological diseases and sexually transmitted infections (gonorrhea, ureaplasma, chlamydia, adnexitis, colpitis, etc.);
- heart and vascular diseases;
- stress, neurosis, depression;
- overweight and physical inactivity;
- bad heredity.
Prevention
In addition to general recommendations, according to which it is desirable to adhere to a rational lifestyle, prevent common diseases in childhood and adulthood, it is important to exclude abortions, carry out timely correction of hormonal disorders, and adequate treatment of gynecological diseases. Specific prevention of the occurrence of uterine fibroids includes the timely implementation of reproductive function: it is recommended to give birth for the first time at 22 years old, the second time at 25 years old, then until 35 years old. Due to late first birth, premature aging of myocytes and a decrease in the adaptive ability to stretch and contract are possible. As a result of abortion and inflammation, the structure of the myometrium is damaged.
The most common time for diagnosing uterine fibroids is a woman’s age of 30–35 years, when the effects of damaging factors are cumulative.
- To prevent the occurrence of uterine fibroids, it is necessary to preserve the first pregnancy, especially for young women with the presence of so-called hereditary fibroids. Abortion can cause the growth of myomatous nodes, and intensive formation of growing fibroids occurs from microscopic nodes.
- In addition, it is advisable to avoid excessive ultraviolet radiation and exposure to elevated temperatures, especially after the age of 30.
- By continuing breastfeeding for 4-6 months after birth, the content of prolactin is normalized, which influences the change in the growth of fibroids.
- Regular visits to the gynecologist and an ultrasound scan are recognized as an effective way to prevent uterine fibroids.
Symptoms of uterine fibroids
The disease develops over several years. Here are the typical clinical manifestations of the disease:
- prolonged heavy menstruation, including with blood clots; anemia;
- pain in the lower abdomen and pelvic area;
- a feeling of heaviness and pressure in the pelvic area;
- painful sexual intercourse;
- frequent urination, cystitis due to compression of the bladder by a large myomatous node;
- constipation, colitis due to compression of the colon;
- abdominal enlargement.
In 30% of women, the disease is asymptomatic or with mild symptoms. An asymptomatic course occurs with small intermuscular and subperitoneal nodes (see below).
Signs and symptoms of uterine fibroids
Clinical signs and symptoms of uterine fibroids may be minimal or absent. The presence of pronounced symptoms, observed in 30% of cases, can significantly reduce a woman’s quality of life.
The main symptoms of uterine fibroids that appear in these patients:
- Pain in the lower abdomen.
- Bleeding and spotting on non-menstrual days.
- Increased urination.
- Tendency to constipation.
- Slight increase in body temperature.
- Pain and weakness in the legs (these are manifestations of nerve root compression syndrome when the tumor size is more than 14 weeks).
Cervical fibroids are a specific type of fibroids that are very rare. It manifests itself with slightly different signs:
- Bloody discharge during sexual intercourse (due to injury to the node).
- Cramping pain associated with the “birth” of a myomatous node.
- Infertility.
Classification of uterine fibroids
The disease is divided by the number and location of nodes in the uterus.
In count:
- single node (single myoma);
- multiple nodes (multiple fibroids).
By node location:
Causes of fibroids
There are 3 theories that explain the cause and mechanism of uterine fibroids. Researchers have not come to a consensus which of them is correct; rather, they complement each other:
- Hormonal theory. This theory is based on a hormonal imbalance, in which there is an increase in estrogen, FSH and LH monthly, and anovulation occurs. Against the background of hormonal imbalance, the receptor apparatus of the muscles of the uterus and its circulatory system, together with the ovaries, change, which leads to a malfunction of the ovaries; accordingly, there is a disruption in the maturation of follicles and metabolism in fibroid tissue and normal uterine tissue.
- Extramedium theory. Explains the stimulation of epidermal, insulin-like, vascular and heparin-binding growth factors against the background of hormonal imbalance, which triggers the formation and growth of tumor nodes.
- Theory of myogenic hyperplasia. Proponents of this theory believe that fibroids are not tumors, but myometrial hyperplasia, which forms when the menstrual cycle is not disrupted. The process is triggered by hypoxia of the muscle fibers of the uterus, which causes their proliferation and the formation of muscle hyperplasia.
Factors predisposing to fibroids:
- disruptions in the production of hormones by the ovaries;
- irregular sex life (blood flow in the pelvis is disrupted);
- inflammatory diseases of the female genital organs;
- lack of sex life;
- metabolic disorders (obesity);
- immunodeficiency states;
- prolonged anovulation and infertility;
- underdevelopment of the genital organs;
- heredity (cancer of the abdominal cavity and pelvis in the family);
- concomitant extragenital pathology;
- refusal to give birth before 30 years of age and lactation;
- surgical interventions on the uterus (abortion, diagnostic curettage, metrosalpingography, hysteroscopy, removal and wearing of an IUD, cesarean section);
- long-term and constant insolation;
- chronic stress;
- hidden sexually transmitted infections;
- algomenorrhea (against the background of painful menstruation, constant hypoxia of the myometrium occurs, which leads to its ischemia).
note
The presence of one or more predisposing factors does not mean that uterine fibroids will necessarily develop.
Treatment of uterine fibroids
There are conservative and surgical.
Indications for conservative treatment:
- small muscle knots;
- absence of uterine deformities;
- childbearing age.
- Prescribe hormonal medications, antibiotics (to treat concomitant infections), iron supplements (if there is anemia), multivitamins, and herbal medicines.
Indications for surgical treatment:
- rapid growth of fibroids (especially after the cessation of menstruation);
- large size nodes, uterine deformation;
- submucosal and cervical location of nodes;
- uterine bleeding with anemia;
- compression of the rectum and bladder;
- disruption of node nutrition with the formation of its necrosis.
- Surgical treatment is performed by an obstetrician-gynecologist. Surgical treatment is reduced to:
- removal of the uterus (hysterectomy). Currently, hysterectomy is used less and less, since low-traumatic, minimally invasive, organ-preserving methods have become widespread. They are given below;
- removal of individual nodes (myomectomy) using minimally invasive methods: laparoscopy (for subperitoneal nodes) and hysteroscopy (for submucosal nodes);
- embolization of the uterine arteries using x-ray endovascular technology. Through a puncture of the femoral artery, a special catheter is used to enter the uterine artery and embolization material is injected into it. Blood circulation in the node stops, and it is gradually replaced by connective tissue;
- focused ultrasound ablation of nodes (FUS ablation). In this case, intense heating of the node and its gradual thermal necrosis occurs. FUS ablation is carried out, including under MRI control.
Diagnosis and differences of diseases
The presence of nodes can be suspected based on the characteristic complaints presented by the patient. During a gynecological examination, the doctor notes changes in the size, shape and structure of the uterus.
You can confirm the disease using:
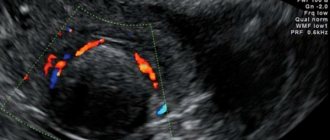
- Ultrasound of the pelvic organs.
- Intravaginal ultrasound examination.
- Colposcopy and hysteroscopy.
- Hormonal studies.
To make a final diagnosis and select a treatment method, it is important to perform a biopsy of the node and histological examination of the obtained material. With its help, you can understand how fibroids differ from uterine fibroids.
If the bulk of the tumor is connective tissue, this pathology is called fibroma ; if smooth muscle cells predominate, it is called leiomyoma (fibroids). If both types of tissue are found in the biopsy specimen, the tumor is called fibromyoma or myofibroma.
Myoma and uterine fibroid: what is the difference
In fact, this is one disease, since the source of the benign tumor in both cases is the muscle tissue of the uterus. As the tumor grows, the fibroma fibers become connective tissue (fibrous) rather than muscle. This means that the type of tumor can only be clarified using histological (microscopic) examination. There is also an intermediate form - fibromyoma, in which the tumor is represented by fibrous and muscle fibers.
The clinical differences between myoma and fibroma are not great. Fibroids are thought to have a slightly wider range of symptoms, but this belief is disputed. It is also believed that fibroids never go away on their own, have less predictable growth than fibroids, and can even turn into a malignant tumor. Considering the latter circumstance, special attention should be paid to early diagnosis, timely treatment and prevention of benign uterine tumors.
Treatment
If uterine fibroids are detected, the patient is prescribed conservative or surgical treatment. In the first case, therapy is carried out on an outpatient basis, in the second, hospitalization in the gynecology department is required. Drug treatment is indicated for small tumors.
Considering its dependence on the level of sex hormones in a woman’s blood, the following is prescribed:
- oral contraceptives (Regulon, Yarinu, Zhanin)
- products containing androgens (Gestrinone, Danazol) for a course of 6-8 months
- drugs containing gestagens (Duphaston, Norkolut) for a course of 4 months to six months
- installation of an intrauterine device (often Mirena)
Additionally, the patient is given symptomatic treatment - iron supplements are administered to normalize the level of hemoglobin in the blood, analgesics and antispasmodics are prescribed. During the course, medications can be replaced or reduced in dosage - this depends on the body’s response to the therapy.
If hormonal treatment does not provide a positive result, the woman is recommended to undergo surgery. There are 3 types of it: in the first case, the tumor is removed without affecting the uterine tissue, in the second, the tumor is removed along with the reproductive organ. The third option for removing nodes is to block the veins and arteries that supply them with blood, which leads to regression of the development of the tumor.
Indications for surgical tumor removal:
- Her rapid growth
- Massive blood loss during and between periods
- The uterus has reached the size observed at 12 weeks of pregnancy
- Partial necrotic changes (necrosis) of nodes
The type of surgical intervention planned depends on many factors, including the location of the tumor. Regardless of the type of elimination of benign nodes, the patient is prescribed a diet. It is aimed at replenishing nutrients removed from a woman’s body during massive blood loss.
Prevention of fibroids
Here are recommendations for preventing fibroids:
- timely (up to 33 years of age) childbirth;
- regular sex life;
- competent selection of contraceptives;
- proper nutrition; body weight control;
- healthy lifestyle, regular physical activity;
- quitting smoking and limiting alcohol intake;
- taking multivitamins in spring and autumn;
- timely treatment of diseases of the pelvic organs, including chronic infections;
- regular examinations by an obstetrician-gynecologist.
Disease prevention
Currently, there really are measures to prevent this disease, taking into account the recently discovered pathogenetic features of fibroids (in 2013).
Therefore, to reduce the likelihood of this tumor, especially in women at risk (family predisposition, black women, etc.), it is recommended:
- Minimize the number of abortions, especially in adolescence.
- Prevent inflammatory processes in the reproductive system.
- Take hormonal contraception if you are not planning to give birth within the next few years. This will avoid unnecessary stress on the body associated with ovulation and menstruation.
- Treatment of painful periods (hormonal contraceptives and anti-inflammatory non-steroids such as Ibuprofen are prescribed for this purpose).
Which doctor should I contact?
If you suspect uterine fibroids, consult an obstetrician-gynecologist. Contact the doctors of the Botkin.pro medical video consultation service. See how our doctors answer patient questions. service doctors for free, without leaving this page, or here. Consult your favorite doctor.
Causes of uterine fibroids
The true causes of uterine fibroids are still unknown, but there is a connection with hormonal disorders and heredity.
The disease does not affect girls before puberty and women who have entered menopause.
If a fibroid is detected in a woman in menopause, it means that it was there before the onset of menopause, but did not cause symptoms.
During pregnancy, the size of fibroids may increase, and after childbirth the tumor will return to its original size.
Based on this, we can say that female sex hormones play a role in the occurrence of such diseases as uterine fibroids.
Factors that increase the risk of developing the disease:
- excess weight;
- African American origin.
- constant stress;
- late or too early formation of the menstrual cycle;
- a large number of abortions and intrauterine manipulations;
- no births at age 30;
- long-term uncontrolled use of hormonal drugs containing estrogen;
- chronic inflammation of the reproductive system;
- other diseases - obesity, diabetes, hypertension.
Questions from patients – answers from Botkin.pro doctors online:
Mirena spiral for fibroids
Good afternoon, I am from Crimea and I am 44 years old. They removed the polyp and RDV, but in addition to everything I have 2 small uterine fibroids, fibrocystic mastopathy of both breasts. The doctor says to put on the Mirena coil. I have a question: is it possible to install a spiral if there is a hemangioma of the lumbosacral spine? Will the spiral provoke the growth of uterine fibroids, hymangiomas and cysts in the breasts? There were no complaints before or after the cleaning; I didn’t bleed either before or after. Cycle + -2 days, menstruation passed and passed painlessly. I know it’s OK, but there’s one thing, I also smoke. In my family there is deep vein thrombosis. Thank you.
Alekseenko Elena AleksandrovnaObstetrician-gynecologist (Gynecologist)
Sign up for a video consultation
Write to the doctor
Good afternoon. There is no data on the connection between Mirena and fibroids and hemangioma, this is one time. Secondly, it won’t be worse for the uterus and breasts, you can put it on. Having weighed the harm and benefits, the spiral is more suitable for you than not.
Treatment of fibroids is conservative
In some cases, thanks to conservative treatment, which is carried out immediately after identifying myomatous nodes of small and medium size, further tumor growth is inhibited, surgery to remove the uterus is prevented, and the opportunity to give birth to a child is preserved.
Conservative treatment of uterine fibroids is indicated for:
- young age of the patient;
- small size of the myomatous uterus (up to 10–12 weeks of pregnancy);
- intermuscular location of myomatous nodes;
- relatively slow growth of fibroids;
- no deformation of the uterine cavity.
Conservative treatment of uterine fibroids is to normalize:
- chronic anemia;
- inflammatory processes occurring in the uterus and appendages;
- impaired blood supply to the pelvic organs, in which venous stagnation and decreased arterial blood supply predominate;
- disturbances in the functional state of autonomic balance and the nervous system.
Correction of systemic disorders includes a number of measures, including:
- maintaining a healthy lifestyle (rational nutrition, normalization of sleep, giving up bad habits, physical activity, body weight control);
- taking vitamins and microelements in winter and spring;
- treatment of anemia;
- normalization of sex life;
- providing neurotropic effects if the patient exhibits traits of a disharmonious personality.
If pregnancy occurs, it is necessary to preserve it, since postpartum reduction of the uterus and breastfeeding the child for at least 4-6 months helps to change the composition of fibroids, so that they become simple and, in some cases, stop their further development. In order to prevent the inevitable removal of the uterus when the tumor grows, it is very important to preserve and maintain reproductive function until the age of 40.
Treatment of fibroids with hormonal drugs
Depending on the nature of hormonal disorders, the density of receptors in myomatous nodes and myometrium, the effectiveness of hormonal therapy varies. As a rule, in fibroids, where connective tissue predominates, and in large nodes, there are no hormonal receptors, and therefore hormonal therapy is not very effective.
Hormone therapy is advisable when correcting an irregular menstrual cycle. For this purpose, the use of progesterone and its derivatives (dydrogesterone, cyproterone acetate), as well as androgen derivatives, 19-norsteroids (levonorgestrel, norethisterone acetate) is provided. The use of the latter is undesirable at a young age, in the presence of obesity, diabetes, and cardiovascular diseases.
In the treatment of patients with uterine fibroids, the most effective drugs include antigonadotropins (gestrinone, danazol), which are characterized by having an antiestrogenic and antiprogesterone effect, which causes temporary amenorrhea. In addition, it is necessary to use gonadotropin-releasing hormone agonists (triptorelin, goserelin, buserelin), which cause a state of reversible hypogonadism.
ANDROGENS. To suppress the synthesis of ovarian steroids in the presence of uterine fibroids, it is possible to use androgen derivatives (Gestrinone, Danazol). Androgens should be taken in a continuous course for up to 8 months, as a result of which it is possible to reduce the size of uterine fibroids.
GESTAGENS. Thanks to the use of gestagens (Duphaston, Utrozhestan, Norkolut), endometrial growth is normalized during hyperplastic processes. Since the effectiveness of gestagens against fibroids is low, their use may be justified when identifying small fibroid tumors of the uterus with concomitant endometrial hyperplasia. Treatment with gestagens can last up to 8 months.
MIRENA SPIRAL. Uterine fibroids can be treated using the Mirena intrauterine hormonal system, which contains the progestin hormone levonorgestrel. With the regular release of the hormone into the uterine cavity, the growth of fibroids becomes difficult and has a contraceptive effect.
COOK. In the presence of small fibroid nodes, the size of which is up to 2 cm, their growth can be effectively slowed down by taking COCs (Yarina, Zhanina, Regulon). The course of treatment for uterine fibroids using combination drugs is 3 months or more.
GnRH ANALOGUES. The use of GnRH analogues (Buserelin, Zoladex) is aimed at achieving hypoestrogenism. Against the background of their regular use, there is a decrease in blood flow to the uterus and fibroid nodes, as a result of which the size of the fibroid decreases. The effectiveness of therapy with GnRH analogues is reversible, because 4-6 months after stopping their use, the nodes reach their original size. In gynecology, GnRH analogues are often used in the preoperative period to reduce the size of nodes for easier removal. Side effects from the use of these drugs include the occurrence of hot flashes, the onset of pseudomenopause, the appearance of vaginal dryness, mood instability, and the development of osteoporosis.