Endometrial hyperplasia is a pathological condition that is characterized by excessive growth of the inner layer of tissue lining the uterus from the inside. Physiological processes in the female body require a constant change of endometrial cells. This is due to the process of ovulation, which occurs regularly after puberty and is regulated at the hormonal level.
The causes of pathological changes are numerous, they will be discussed in detail. The pathological process primarily affects the inner layer of the endometrium (functional) and only with further development can it affect the underlying basal layer. There are several types of hyperplasia, the classification is based on histological analysis of the pathological focus.
Changes in the condition of the endometrium can take many forms, but even simple hyperplasia is a serious cause for concern. Women should know what it is, what the consequences will be if they do not contact specialized specialists and treatment does not begin in a timely manner. This is important, since it ranks second in the structure of all gynecological diseases; only infectious diseases are more common.
The types of this pathology, its symptoms, treatment and prospects for patients with full recovery from hyperplasia will be discussed in detail below. This is important, because pathological changes in the endometrium, although not cancerous, are very dangerous. This disease is classified as a precancerous condition. That is, the risk of a malignant neoplasm with the development of a pathological process and the absence of adequate therapeutic measures is very high.
Since the disease is not “age-related”, the risk of its occurrence is present both in girls during puberty and in postmenopause. If we evaluate the frequency of detection in different age groups, then statistics especially highlight the age from 35 to 50 years. According to some data, this age accounts for almost 50% of cases of GPE. At the same time, at the very beginning, the disease is often asymptomatic; hyperplasia is often detected when the pathological process of the endometrium begins to manifest itself in the form of typical symptoms. That is why it is important to regularly visit a gynecologist for preventive purposes and obtain reliable and detailed information about the disease itself.
Concept of pathology
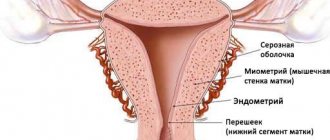
Hyperplasia of the uterine endometrium occurs when the normal restoration of the functional layer is disrupted. The endometrium, which lines the uterus, consists of two different layers. The first is functional, located outside, it first grows during the maturation of the egg, and then (if fertilization does not occur) is completely rejected and removed from the body during menstruation. The second is basal, lies under the first layer and is located from the inside, it is thinner, the structure at the cellular level is poorly expressed and serves as a “building material” for the restoration of the functional layer.
The normal physiological process looks like this:
- Proliferation (growth of the endometrium in the uterus): immediately after the onset of menstruation, the process of proliferation of the functional layer begins, so the body prepares for a potential pregnancy;
- Secretion (maturation): occurs at the moment of ovulation;
- Desquamation (rejection): if fertilization does not occur, the grown layer is rejected and, together with the unfertilized egg, is removed from the body - menstruation begins.
The entire cycle occurs as a result of hormonal influence, estrogen is responsible for the first stage, progesterone is responsible for the second. The level of growth of the functional layer is regulated, proliferation of the first phase of the menstrual cycle is accompanied by aptosis - the death of “extra” cells. Each stage is important in its own way, because such a consistent change in the endometrium maintains the normal thickness of the functional layer at different periods of the menstrual cycle. Any disturbances in regulation lead to pathological thickening, and this is hyperplasia.
Is this disease dangerous? Yes, if it is not treated, then the pathological focus in approximately 40% of cases goes into the stage of cancer, that is, it is a precancerous condition. In addition, hormonal imbalances can lead to diabetes and obesity, and changes in the normal menstrual cycle can lead to infertility. Therefore, women should pay attention to their health and regularly visit a gynecologist. Detection of the disease at the beginning, in the asymptomatic period, will help to cope with the problem before the clinical picture becomes threatening.
https://youtu.be/t2N031WSl3E
Causes
Causes of uterine endometrial hyperplasia
The main pathogenetic cause of this pathological process lies in hormonal imbalance, which can be a consequence of various gynecological and somatic nosological forms.
These include:
- Disorders of the ovarian-menstrual cycle;
- Polycystic ovary syndrome;
- Myomatous neoplasms of the female reproductive organ;
- Metabolic syndrome with obesity;
- Diabetes;
- Diseases of the thyroid gland with dysfunction;
- Also, the cause of endometrial hyperplasia is the incorrect use of COCs by women and non-compliance with treatment regimens.
How often and to whom does it occur?
Hyperplasia is considered one of the most common diseases of non-infectious etiology. In the structure of all gynecological diseases it is in 2nd place, according to various sources - from 15%. If we analyze age groups separately, we can note the following indicators:
- in teenage girls: occurs as a result of hormonal physiological changes, hormonal disruptions or functional disorders of neurohumoral regulation during puberty;
- in women under 35 years of age: the least dangerous age, the hormonal levels in this group are usually stable, all processes proceed within the physiological norm;
- over 35 (period before, after and during menopause): the most dangerous age, this is the main risk group for the occurrence of hormone-dependent gynecological diseases.
Recently, cases of hyperplasia detection have become more frequent. If earlier it was about 5%, now endometrial diseases are recorded much more often. And in the last group, according to some data, from 40 to 50% suffer, that is, every second woman of this age is diagnosed with pathology at one or another stage of development.
Treatment methods
Treatment of endometrial hyperplasia is prescribed after a complete examination. Usually (50-60% of cases) this is the prescription of hormone-containing drugs, but other methods can also be used. Their choice depends on the form and nature of the disease and the woman’s age. So, in the presence of polyps, removal is carried out through hysteroscopy. The diffuse form requires separate curettage, which can be planned or emergency. After curettage, if stable remission is observed for 6 months and there are no complications, you can plan a pregnancy.
The doctor prescribes the drugs after a histological examination. These are combined contraceptive pills that should be taken for at least six months. Also in the second phase of the cycle, progestogen drugs are prescribed. If HPE is diagnosed in a teenage girl and is accompanied by heavy bleeding, the doctor may increase the dose of oral contraceptives.
Since therapy with hormonal complexes has many side effects and contraindications, when treating patients with metabolic disorders and disruptions in the endocrine system, treatment is carried out carefully. The minimum dose is prescribed. At the same time, medications are prescribed to neutralize the negative effects of hormones.
During the course the patient is under observation. The gynecologist conducts regular examinations and ultrasounds. After completion of therapy, the woman should be under the supervision of the attending physician for one to three months. If the cycle is normal and there is no growth of the endometrial layer, this indicates successful treatment.
How is the disease related to the menstrual cycle?
Hyperplasia of the mucous layer directly depends on the menstrual cycle. All stages (proliferation, secretion and desquamation) normally occur during a strictly defined period of the menstrual cycle.
From the first day of your period, the endometrium begins to grow, so the uterus prepares for a potential pregnancy. In the second, at the moment of ovulation, the newly grown cells mature, and the “extra” die (natural aptosis). If fertilization does not occur, rejection begins, the built-up layer is destroyed, and along with the egg is removed from the body - menstruation begins. And at the same time, the next cycle “starts”.
The whole process is controlled by hormones, to which endometrial cells are very sensitive. Any disruption of hormonal function at any stage can lead to abnormal tissue growth, stop the death of overproduced cells, or disrupt the rejection process and lead to hyperplasia.
Hyperplasia and pregnancy
As mentioned above, with hyperplasia there is no ovulation. Therefore, this disease is a sign of infertility. If a woman wants to get pregnant, then the doctor’s task is to restore ovulation.
It must be said that the very diagnosis of this disease, which was made by the gynecologist, suggests that it will not be possible to get pregnant. You must first cure hyperplasia. If the patient is preparing for IVF, then at least 6 months must pass from the start of therapy until possible fertilization. But if a pregnancy does occur, then in frequent cases it is recommended to terminate it. Otherwise, there is a possibility that benign formations may develop into malignant tumors.
Although there is no need to worry too much about this, the likelihood that a woman will become pregnant during treatment for endometrial hyperplasia, or even more so if she does not know about this disease, is equal to 1% out of 100. But in order to still avoid unpleasant consequences, doctors recommend that all women who are planning a pregnancy first consult a gynecologist and undergo a routine examination. Then you will be able to avoid many undesirable moments.
Causes and pathogenesis
The causes of hyperplasia are primarily associated with various changes in hormonal levels. But there are other provoking factors that are not directly related to humoral regulation.
The main causes of pathological growth of the endometrium are:
- disturbances in hormonal regulation associated with an imbalance of estrogen and progesterone of any etiology (age-related changes in hormonal function, hypothalamic-pituitary syndrome, etc.);
- associated with other diseases of the female reproductive system (polypoid, against the background of polycystic disease, hormone-producing tumors, etc.);
- the presence of concomitant diseases associated with hormonal imbalance: diabetes mellitus, adrenal cortex dysfunction, obesity, diseases of the thyroid and/or mammary glands, hypertension;
- disorders caused by prolonged or improper use of hormonal drugs;
- pathologies caused by trauma (during and after childbirth, abortion, diagnostic curettage, etc.);
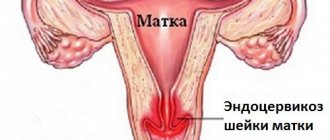
- hyperplasia caused by pathological processes associated with genital tract infections;
- hereditary predisposition;
- psychosomatic disorders that caused the disease.
Hyperplasia against the background of any hormonal problems occurs most often. Other causes of endometrial hyperfunction are not so common, but can become factors that provoke the disease. Separately, it is worth considering how hyperplasia and psychosomatics are related to each other. Illnesses often arise against the background of psychological problems. Medicine has long established a connection between pathological changes in normal functions and psychological disorders.
In this case, in response to experiences, depression or prolonged stress, the body turns on defensive reactions. They can lead to changes in hormonal levels, which will cause the development of hyperplasia. There is such data, cases have been recorded and a direct relationship has been established between pathological growth of the endometrium against the background of psychological problems and disorders.
Since the disease occurs in women of different age groups, it is additionally worth considering the etiology for each of them separately.
During puberty
The reasons for the occurrence in teenage girls during the period of maturation are anovulation, which at this age is caused by certain disorders of the function of the hypothalamic-pituitary system. They lead to disturbances in the hormonal regulation of follicle maturation, which is controlled by the pituitary gland. The result most often is premature follicular atresia.
If violations are repeated many times during successive menstrual cycles, then the normal balance of hormones in the body is disrupted. Estrogen accumulates in excess, and progesterone is not enough. Consequently, the normal sequence of proliferation - secretion - rejection is disrupted. As a result of the appearance of an excess number of cells in the functional layer of the endometrium, hyperplasia develops (mainly due to the glandular epithelium). As a result, cystic or adenomatous forms of the disease are diagnosed.
During reproductive age
In the age category up to 35 (reproductive age), hyperplasia can occur against the background of:
- dysfunctions of the hypothalamic-pituitary system, which can manifest as a result of hyperprolactinemia. Or against the background of problems with the functioning of the hypothalamus, chronic somatic diseases, stress, starvation, etc.;
- anovulation caused by impaired secretion of luteinizing hormone, the activity of which depends on the hormonal feedback mechanism;
- ovarian diseases (polycystic disease, follicular cyst, pathological proliferation of stroma, etc.).
In premenopause and perimenopause
During this period, hyperplasia may occur against the background of age-related changes. The attenuation of reproductive function is associated with a decrease in hormonal activity against the background of a decrease in the activity of the hypothalamic-pituitary system. The consequence of these physiological processes is anovulation due to a lack of estrogen.
An additional factor stimulating the development of pathology is an increase in the activity of the adrenal cortex. As a result, diseases such as obesity (male type), ischemic heart disease and hypertension, diabetes mellitus and other “age-related” diseases associated with hormonal changes in women of this age often occur.
Another risk factor for the development of hyperplasia is the consequences of pregnancy, childbirth and abortion (possible injuries). A decrease in the number of hormone-sensitive receptors, dysfunction of aptosis at the gene level and other physiological changes associated with the aging process.
The endometrium responds to all these influences:
- growth as a result of an imbalance of estrogen and progesterone;
- an abnormal reaction from the glandular cells of the mucosa against the background of a stable hormonal background (at the normal level);
- an imbalance of insulin activity and resistance, which results in a number of pathological conditions (polycystic disease, diabetes, etc.), disruption of normal growth, development and death of the endometrium.
Thus, the etiology and pathogenesis of hyperplasia differs in women of different age categories. But there are common reasons that led to the activation of the process itself.
Endometrial hyperplasia - what is it?
Nature has endowed a woman with the unique ability to bear and give birth to children. And the most important role in this process is played by the endometrium - a special layer of the surface of the uterus, thanks to which this muscular organ is able to secure and retain the developing fetus.
The endometrium has a complex structure. In its lowest part there is a basal layer, and a little higher - a functional one. Normally, the endometrium has a certain thickness. However, the thickness of the functional layer is not constant and varies depending on the phase of the menstrual cycle. At the beginning of the cycle it is very small, and at the end, when the uterus is waiting for a fertilized egg, it reaches its maximum thickness. But if attachment of the fertilized egg does not occur, then the functional layer is rejected and comes out. This process is well known to any woman - this is the process of so-called menstruation, or menstrual bleeding. Then the functional layer begins to recover again. The basal layer is responsible for this process. Thus, the process of growth and separation of the endometrium is repeated many times.
These changes in the endometrium occur under the influence of female hormones - estrogens and progesterone. During the menstrual cycle, the amount of estrogen increases, and at the same time the thickness of the endometrium increases. However, at the end of the cycle, increased amounts of progesterone begin to be produced. This hormone inhibits the growth of the endometrium. Consequently, the maximum thickness of the endometrium does not exceed a certain value, and then its upper part is rejected during menstruation
Obviously, this mechanism only works if the woman has normal levels of sex hormones. If the amount of estrogen increases and the amount of progesterone decreases, then the endometrium grows much more than is prescribed by the norm. There is also no inhibition of endometrial growth at the end of the menstrual cycle due to a lack of progesterone. Moreover, hormonal imbalances can cause menstrual irregularities, and menstruation may not occur for several months. Eventually, the endometrium begins to shed, but this is accompanied by significant bleeding and pain.
How it manifests itself
Symptoms of hyperplasia may not appear immediately; at the beginning of the pathological process they may be poorly expressed, so women often do not pay attention to their appearance. The main and most important manifestation of this endometrial pathology is bleeding, which can be:
- in the form of long delays: menstruation may be absent for 1 – 3 months, after which they resume, being abundant and prolonged or scanty. Such symptoms are most common (almost half of the patients have corresponding complaints) and do not depend on age-related changes. Moreover, most complaints are associated with heavy bleeding; scanty periods are not such a common manifestation of hyperplasia;
- the changes are related to the nature of menstruation: the stability of the cycle is maintained, but the volume of discharge during hyperplasia increases (longer and more abundant), unpleasant or painful sensations appear;
- bleeding during pre- and postmenopause, when the cycle is unstable and the intervals between menstruation are long or absent.
That is, symptoms associated with any bleeding (outside the cycle or unusual in abundance for a woman during a stable cycle) should be the reason for an immediate visit to the gynecologist. This is the main and often the only symptom that characterizes hyperplasia.
Additionally, pathological processes in the endometrium may be indicated by:
- metabolic syndrome, which manifests itself in the form of various pathological conditions (increased insulin levels, obesity, the appearance of secondary male characteristics, etc.);
- chronic inflammatory and infectious diseases;
- infertility and miscarriages can also be considered as alarming signs of the development of pathology;
- fibroids and mastopathy are independent diseases, but can be caused by hormonal disorders, like endometrial pathologies;
- contact bleeding not associated with the menstrual cycle (during sexual intercourse, using tampons, etc.) is not among the main complaints and is rare;
- Complaints of cramping pain are also not common; they are more likely not a sign of endometrial atypia, but indicate other pathological processes, for example, polyps.
Since a delay in menstruation is the main symptom, any changes in the duration or nature of the cycle should alert a woman, regardless of age. What to do in such cases? You should immediately contact a gynecologist. The delay, of course, can be caused by completely different reasons (pregnancy, inflammation, hypothermia, etc.). But you should not neglect checking with a specialized specialist, even if cycle failures are quite understandable (for example, menopause). Women over 35 should regularly visit a gynecologist, since they are at risk, and an asymptomatic course is quite possible in the initial stages of the disease.
Symptoms
Uterine hyperplasia: what it is, symptoms, treatment
Like any pathological condition in the body, placental hyperplasia has its own clinical symptoms, which appear in response to the formation of a pathological process. In the initial stages of hyperplasia, it may not manifest itself in any way and proceed hidden.
Uterine hyperplasia: symptoms and treatment
A change in the nature of the menstrual cycle, which can consist of either a delay in menstruation for a fairly long period or the appearance of intermenstrual spotting or bleeding. Also, menstruation can take on the character of bleeding with heavy blood loss and a fairly long duration.
When a pronounced hemorrhagic syndrome appears, signs of uterine hyperplasia, characteristic of the development of anemia (low levels of hemoglobin in the blood), begin to appear: general weakness, fatigue, pallor of the skin.
Symptoms of uterine endometrial hyperplasia in menopause also manifest themselves in the form of spotting or bleeding. However, during this period, the appearance of any bloody discharge and genital tract greatly alarms doctors, as it may indicate a malignant process of the cervix. That is why a woman should constantly undergo preventive examinations with an obstetrician-gynecologist to exclude such a pathological process. And if it appears, early diagnosis and timely treatment will be carried out
- Pain syndrome of varying intensity can accompany endometrial hyperplasia;
- The appearance of symptoms of algodismenorrhea - painful menstruation;
- Dyspareunia – pain during sexual intercourse;
The appearance of complaints about futile attempts to get pregnant. If a couple is unable to conceive a child for a period of one year or more without using any contraception, a diagnosis of infertility is made. Both women and men are subject to a mandatory set of examinations, during which increased endometrial thickness is detected. The reason for this symptom lies in the growth of the endometrium and the loss of its functional features that facilitate the transportation of the blastocyst and its implantation. With proper therapy and correction of hormonal changes, infertility of this origin can be overcome without any difficulties.
Classification
There are several classification systems that allow the disease to be viewed from different perspectives. For example, according to the volume of pathology, it is customary to distinguish simple, moderate (moderate hyperplasia) and severe forms. And according to their prevalence, they are divided into focal (this includes polypoid hyperplasia) or diffuse. The generally accepted system is based on cytology, i.e. types of pathology are divided into different groups according to the type of cells and tissues that predominate in the modified area. Currently there are:
- simple hyperplasia (glandular). It is characterized by the absence of cystic enlargement of the glands. But in the process of proliferation, such expansion can be observed in certain areas of the mucosa, then they talk about the glandular-cystic form, but at the same time they consider this case not as a separate species, but as a stage of the pathological process;
- glandular-stromal. Mixed type, complex hyperplasia, which is characterized by simultaneous proliferation of glandular and stromal structures, and can be in both active and quiescent forms;
- The atypical glandular and adenomatous forms, which are combined into one group and are characterized by a variety of morphological patterns and the severity of proliferative processes, are considered especially dangerous.
According to the WHO classification, endometrial hyperplasia is divided into:
- NON-ATYPICAL. Hyperplasia without atypia is characterized by the absence of modified cells. It includes simple and complex forms (by complex we mean adenomatous).
- ATYPICAL, which can also be simple or complex. This group includes developmental stages during which cells change and become atypical in their structure.
When describing according to any classification, a number of factors are taken into account. For example, the local form can be represented by polypoid outgrowths from different types of tissue.
The basal form of hyperplasia is considered separately. Since most often the pathological process does not affect the basal layer, but develops in the functional layer, it usually means damage to the outer layer. Initially, the pathological process in the internal underlying tissue begins rarely; its damage is more typical in the later stages, when the pathological focus goes beyond the functional layer and nearby tissues are involved in the process.
Forms of hyperplasia
The endometrium is formed by a base of connective tissue and a covering layer of multirow epithelium with simple tubular glands. Depending on which of these elements will grow rapidly, hyperplasia is divided into:
- Glandular. Characteristic is the proliferation of endometrial glands, an increase in their number without changing the structure.
- Glandular-cystic. Along with the proliferation of glands, their secretory activity increases. In some glands where the ducts are blocked, secretion accumulates and cysts form from them.
- Glandular-fibrous (basal). Both the glands of the integumentary layer and the base of connective tissue grow.
- Adenomatous (atypical). The most dangerous in terms of transformation into malignant neoplasms. It is characterized by the proliferation of glands of altered structure, and single atypical cells can be detected in them.
Diagnostic methods
Diagnostics is currently a comprehensive examination using all methods available in modern medicine. These include:
- APPOINTMENT WITH A PROFILE SPECIALIST with a mandatory interview (history collection) and gynecological examination.
- LABORATORY TESTS: blood is donated to determine hormone levels; in case of concomitant gynecological diseases, a smear is taken.
- HYSTEROSCOPY allows you to: visualize the clinical picture, study and evaluate the condition of the endometrium in detail, identify all pathological processes and obtain material for histological examination. Diagnostic curettage is the most informative method; its accuracy reaches 97%. On what day of the cycle is hysteroscopy performed? If we are talking about a simple examination, then it is prescribed on days 5–7; for diagnostic curettage, the day before menstruation or the first day, immediately after the start of menstrual bleeding, is chosen. The disease is diagnosed if the thickness of the endometrium during hyperplasia is more than 15 mm, and surface and color changes are visible. When curettage, two goals are achieved simultaneously: material is taken for research and the pathological focus is simultaneously removed. Histology allows you to obtain a reliable result about the presence of atypical cells.
- ULTRASONOGRAPHY. In gynecology, the best method is transvaginal ultrasound, which allows us to identify echographic signs of the disease. It is usually prescribed on days 5–7 of the menstrual cycle. If the disease manifests itself as a violation of it, then with prolonged bleeding the day can be chosen arbitrarily. In this case, on what day of the cycle an ultrasound is done does not matter. Echo signs of hyperplasia make it possible to determine the structure, uniformity and thickness of the functional layer. The accuracy of this method is almost 70%; an additional advantage is the ability to differentiate the pathological process. If the thickening is more than 7 mm, then the disease can be defined as hyperplasia; if it is more than 20 mm, oncology can be suspected.
- MAMMOGRAPHY – used as an additional examination to exclude proliferative processes.
- RADIOISOTOPIC RESEARCH. The ability of radioactive phosphorus to accumulate in affected tissues makes it possible to accurately determine the location and volume of the lesion.
Modern diagnostic methods used to identify hyperplasia make it possible to determine the nature and extent of the pathological process as accurately as possible. At its very beginning, curettage can be both a diagnostic and therapeutic measure.
Treatment
Uterine endometrial hyperplasia: treatment
In order to begin treatment of this pathological condition, it is necessary to conduct a high-quality diagnosis of endometrial hyperplasia.
Uterine hyperplasia: treatment based on proper diagnosis
This diagnosis should include a gynecological examination and examination, collection of anamnesis and complaints; after the gynecological examination, the obstetrician-gynecologist should send the woman for ultrasound diagnostics. On an ultrasound, a functional diagnostics doctor will see an enlarged endometrium and give a digital answer to the question of the thickness of the functional layer. If the thickness of the endometrial layer is 15 mm or more, then the doctor has the right to make a diagnosis of endometrial hyperplasia. However, this diagnosis is preliminary; the final diagnosis can be made only after a pathohistological examination. To obtain material for such a study, it is necessary to perform diagnostic manipulations in the form of fractional diagnostic curettage with removal of the functional layer of the endometrium by sharp curettage of the uterine cavity or by performing a hysteroscopic examination. It is carried out using a video laparoscope (optical instruments), with the help of which the functional tissue covering the uterine cavity can be removed.
How to treat uterine endometrial hyperplasia
Treatment of endometrial hyperplasia is divided into stages: this is the removal of the functional layer, which is performed at the time of diagnostic curettage, and then drug treatment to correct the hormonal disorders that caused this tissue proliferation. If you perform only curettage without drug correction of hormonal levels, then the risk of recurrence of this pathological condition is very high, since there is no effect on the etiopathogenesis of the disease.
How is endometrial hyperplasia of the uterus treated: drug therapy
Drug correction of hyperplasia is carried out using several groups of drugs. Combined oral contraceptives are prescribed, which equalize the ratio of estrogen to progesterone, the estrogenic effect on the endometrium, thereby preventing proliferative processes in it. For the same purpose, gestagen preparations such as Duphaston, Utrozhestan, Norkolut are used. These drugs should be selected depending on the concomitant gynecological, somatic pathology, as well as the reproductive history and plans of the patient. The group used in the treatment of endometrial hyperplasia is the use of gonadotropin-releasing hormone agonists and antagonists. However, their negative effect is to introduce a woman into a state of artificial menopause, which will lead to the appearance of corresponding clinical symptoms. Not every woman will be able to satisfactorily tolerate the effect of the drugs used.
How to stop uterine bleeding with endometrial hyperplasia in adolescents? In most cases, doctors try to treat such conditions in girls conservatively without the use of surgical intervention in the form of curettage. Hormonal hemostasis is performed
Hyperplasia of the endometrium of the uterus in menopause: treatment
A pathological condition such as endometrial hyperplasia can overtake a woman during menopause. Is endometrial hyperplasia of the uterus treated in menopause? Treatment of uterine hyperplasia in postmenopause is carried out either hormonally or surgically, depending on the clinical situation. If there is slight thickening of the endometrium, you can limit yourself to hormonal drugs with control diagnostics. And if there is a relapse of the pathological process, or a suspicion of a malignant process, then in such cases it is necessary to perform curettage in order to remove the hyperplastic endometrium and its further histological examination to select further treatment tactics. But postmenopausal doctors prefer, if possible, to subject all cases of bleeding to histological examination.
Can it be cured forever?
We examined the concept of endometrial pathology and the causes of its occurrence. After diagnosis, patients are usually interested in further prospects, how to treat and whether it is possible to get rid of the disease forever. Moreover, both surgical and therapeutic methods. The choice of treatment tactics depends on the clinical picture. Additionally, a course is prescribed aimed at eliminating the causes of the disease. A complete cure is possible if the pathology is detected on time.
The prejudice that concerns some treatment methods forces us to look for alternative solutions to the issue. But it is better for patients to use traditional methods of medicine, which allow them to preserve reproductive function and be completely cured.
It should be understood that hyperplasia itself will not disappear; complex treatment is needed, and if the causes of the disease persist, there is a risk of relapse. But with early detection, the chances of a full recovery are high, so after diagnosis it is necessary to begin treatment immediately.
Diagnostics
The set of diagnostic measures includes:
- Examination by a gynecologist.
- Ultrasound of the abdominal cavity.
- Transvaginal echo scanning of the uterus.
- Hysteroscopy is an examination of the internal cavity of the uterus using a hysteroscope.
- Radioisotope method. Radioactive phosphorus injected into a vein accumulates in areas of the uterus with the most overgrown endothelium.
- Curettage of the uterus for therapeutic and diagnostic purposes. Removal of pathologically overgrown endometrium and examination of the biopsy for the presence of cancer cells.
- Determination of hormonal status.
Is relapse possible?
The diagnosis of “recurrent hyperplasia” is given to patients when the pathological lesion reappears. Since the main cause of the disease is considered to be an imbalance in the hormonal balance of estrogen and progesterone, the possibility of relapse exists if the imbalance is not corrected.
If after treatment the recurrent form continues to bother the patient, it is necessary to change the treatment tactics. For example, instead of organ-preserving surgery (removal of the functional layer of the endometrium), surgery is prescribed to remove the reproductive organ. The absence of the uterus completely eliminates the possibility of resumption of the pathological process.
Often the disease recurs if the cause of its occurrence remains unchanged. Patients are usually prescribed complex treatment aimed at eliminating the pathological focus and etiology. After the course, the patient remains under dispensary observation, which allows timely detection of any signs of resumption of the pathological process.
Removal
Removal of the uterus for endometrial hyperplasia reviews
Surgical treatment of endometrial hyperplasia involves removing the most functional layer of the endometrium by curettage, hysteroscopy, or laser ablation. The resulting tissue must be subject to histological examination. In addition, there is a type of treatment for this pathological process, such as removal of the uterus - hysterectomy. Hysterectomy can be performed if there are such indications: removal of the uterus is indicated in a situation where, when examining the obtained material, histologists give an answer about the presence of atypical cells in the functional layer (with such hyperplasia, it is better to remove the uterus). An established diagnosis of adenomatosis and the presence of clinical symptoms of this pathology are also an indication for surgical intervention. This includes heavy bleeding, and during a control ultrasound examination, the size of the endometrium exceeds all norms.
How to remove the uterus for endometrial hyperplasia
However, choosing a hysterectomy tactic does not mean choosing the volume of intervention. The scope of the surgical operation is performed taking into account both somatic and gynecological pathologies. Hysterectomy can be of the following types:
- Hysterectomy without adnexa with removal of the cervix, the uterus is removed, and the adnexa remain in place. Performed in women of reproductive age to prevent the development of post-castration syndrome and early premature menopause - severe consequences of removal of the reproductive organ;
- Hysterectomy with adnexa;
- Uterine amputation, an operation in which the body of the uterus is removed, but the cervix remains. It can also be performed either with the preservation of the appendages or with their removal.
Another important point is the choice of access for organ removal. When performing a hysterectomy, a laparotomy approach can be used - this is an incision in the anterior abdominal wall and open surgery. As well as a laparoscopic method of removing the uterus using endoscopic instruments through three punctures of the anterior abdominal wall. The operation can also be performed via vaginal access through the vagina.
Removal of the uterus for endometrial hyperplasia: the consequences of such an intervention primarily concern the inability to become pregnant and bear a child; removal of the uterus and appendages during reproductive age threatens premature menopause with the development of all complications for the female body.
How to treat
Treatment of endometrial hyperplasia can be carried out using both therapeutic and surgical methods. The basis for choosing a tactic will be the clinical picture: the type of pathology, its volume and localization, the results of a cytological examination, etc. Since the symptoms of this disease primarily involve bleeding, anemia may develop. Then additional medications containing iron may be prescribed. To improve your general condition - vitamins to maintain immunity. Complex treatment is carried out in stages, so you should strictly follow the recommendations and adhere to the general plan prescribed by the doctor.
Stages of treatment
Treatment usually goes as follows:
- Curettage using hysteroscopy. The procedure is therapeutic and diagnostic in nature at the same time. During its implementation, the functional layer is completely removed, the resulting material and the contents of the uterine cavity are sent for examination.
- Treatment tactics are selected in accordance with the results obtained, taking into account the patient’s age, type of pathology, its volume and other important factors.
-Glandular cystic hyperplasia: treatment is usually therapeutic; special drug regimens have been developed for patients of different ages;
-The atypical form in postmenopausal patients is treated surgically. In reproductive age, hormone therapy is first used with control curettage after 6 months. For complications such as fibroids or metabolic syndrome, surgical intervention is recommended.
Conservative therapy
For hyperplasia, medications are prescribed according to special regimens, and treatment courses are long. Therapeutic drugs are selected according to the form of pathology and the age of the patient.
What hormones are used to treat the disease depends on the age of the patient:
- in reproductive age, preference is given to oral combined contraceptives; single-phase drugs containing progesterone are most often used. Contraceptives are taken for 3 to 6 months, the prognosis with the right tactics is favorable, the risk of relapse is minimal;
- after 35 years and before menopause, it is recommended to take drugs with gestagen;
- In postmenopausal patients, conservative treatment is allowed if there are no tumors.
This is the tactic for the glandular cystic form. If we are talking about an atypical form, then it is recommended to take drugs containing gonadotropin releasing hormone agonists. Monitoring the condition of the body will be mandatory (mammography, ultrasound, and blood tests are performed during the course).
Additionally, during the therapy period, suppositories may be prescribed (suppositories will help relieve inflammation), physiotherapy, and acupuncture. Anti-anemia medications may be prescribed, as well as supportive medications (for example, Carsil to improve liver function or vitamins). Electrophoresis is used as physiotherapy; for obesity, exercise therapy and diets for weight loss may be recommended. The doctor determines whether the disease can be dealt with exclusively by therapeutic means and selects a regimen that will be aimed at eliminating the cause of the development of HPE and improving the general condition of the patient’s body.
Surgery
Surgical intervention is prescribed in several cases:
- therapeutic treatment did not give the desired effect;
- the patient experiences relapses;
- surgery is the only correct tactic: hyperplasia is atypical in nature, the patient has already entered the postmenopausal phase and hormone therapy will be ineffective, the pathology seriously threatens health (the disease is progressing, there is a risk of degeneration into oncology).
In surgery, the operation is performed:
- to remove the endometrium (curettage during hysteroscopy or using a resectoscope when it is necessary to remove both layers);
- removal of reproductive organs (uterus, more complex - along with the ovaries).
Hysteroresectoscopy is performed in a hospital setting; the patient can queue for free treatment or go to a private clinic. For hyperplasia, the price of surgical intervention depends on the degree of complexity, on average from 15 to 30 thousand rubles. The cost depends on the level of the medical institution; in the regions it is usually lower than in Moscow, St. Petersburg and some other cities.
Unconventional treatment
Despite positive reviews of various traditional methods, hyperplasia is treated best if they complement conventional methods. Doctors themselves often recommend supplementation in the form of herbal medicine. Such drugs help fight obesity, relieve local inflammation, restore hormonal levels, etc. Medicinal herbs must be taken as prescribed by the attending doctor, who selects them individually.
Additional treatment methods that can be used include:
- HOMEOPATHY. Taking homeopathic remedies is aimed at reducing the amount of bleeding, restoring hormonal levels, the menstrual cycle, reproductive function, etc. A homeopathic physician should select medications, taking into account the general treatment tactics in each specific case.
- HYRUDOTHERAPY. Helps normalize the cycle, activate protective mechanisms, balance hormonal functions, etc. Treatment with leeches is quite effective (reviews confirm this) and is actively used in gynecology;
- PHYTOTHERAPY. The attending physician will help patients choose an effective remedy based on medicinal herbs. He knows exactly the clinical picture and will be able to recommend the right remedy. Often used: celandine, nettle, burdock, hogweed, plantain, peony and other plants (on their own or in the form of collections).
When choosing treatment tactics, you should understand that hyperplasia will be completely cured if you strictly follow the recommendations of a specialized specialist. Modern medicine opens up great opportunities, some drugs are interchangeable (natural hormones can replace synthetic ones, for example, Utrozhestan). For patients over 50, surgery is often prescribed as the main method; women of reproductive age are trying to preserve reproductive function. Hyperplasia detected in time can be completely cured, and the risk of relapse is reduced if the provoking factors are eliminated.
Viscating
Diagnostic curettage of the uterine cavity for endometrial hyperplasia
Diagnostic curettage of the uterine cavity for the diagnosis of endometrial hyperplasia is carried out in most cases when the diagnosis is established. It is performed both as a therapeutic measure to remove the enlarged functional layer of the endometrium and stop uterine bleeding and pain, but also for diagnostic purposes. The material obtained during this curettage must be sent for histological examination.
What are the dangers of hyperplasia?
Why is gpathology dangerous? During the development of the disease without adequate treatment, the pathological process continues. As a result, it can affect the underlying basal layer, neighboring organs, and develop into oncology. Constant bleeding can cause anemia, and the causes of the disease are concomitant diseases of a similar etiology.
Is further development dangerous? Yes, first of all by the transition to the atypical form. In addition, the pathology can cause infertility.
What consequences should we expect? In the absence of treatment, the pathological process will further develop. If hyperplasia has not been completely cured or the causes of its occurrence have not been eliminated, the disease is dangerous for relapses.
Why is it dangerous?
Why is endometrial hyperplasia of the uterus dangerous?
Endometrial hyperplasia has many negative effects on a woman’s body. Causing hemorrhage up to the volume of bleeding, this pathology contributes to the development of anemia from mild to severe. This pathological process is the cause of infertility, which becomes both a medical and social problem. Hyperplasia of the functional layer of the endometrium can be complicated by the malignancy of the process and be a substrate for the occurrence of cancer. That is why timely diagnosis and treatment of this nosological form is the prevention of cancer. In some cases, removal of the female reproductive organ may be necessary. Of course, there are consequences of removing the uterus for endometrial hyperplasia.
Proper nutrition
The diet is aimed at normalizing hormonal levels. Healthy foods are those that will help control estrogen (vegetables and fruits, nuts, grains, legumes). Products containing omega acids (fish) and vitamins are added to the diet.
Meals for hyperplasia should be fractional, 4-5 times a day. Animal proteins, spicy, pickled and salty foods, alcohol, soda coffee, and confectionery are excluded from the diet (or significantly reduced).