Today it is successfully used for the timely detection of diseases of the bladder and urethra. cystoscopy And cystourethroscopy - a procedure that allows you to look inside the patient's bladder and urethra. Cystoscopy and cystourethroscopy is an endoscopic method for examining the bladder and urethra, which consists of examining the mucous membranes of these organs using a special optical system - a cystoscope. A cystoscope looks like a long metal tube to which a light source and a video camera are attached. The difference between the methods is that with cystoscopy, only the bladder cavity is examined, and with cystourethroscopy, when removing the instrument, additional fluid is supplied under pressure, and the walls of the urethra are examined. Cystoscopy is a fairly accurate method for diagnosing diseases of the bladder and urethra (urethra), sometimes the information obtained by modern methods (ultrasound, computed tomography) is not enough to make a diagnosis, in some cases these methods are generally uninformative. A urologist performs a cystoscopy.
Medical cystoscopy is performed by experienced, highly qualified specialists, taking into account your individual characteristics. When examining the bladder, the procedure involves inserting a cystoscope through the urethra into the bladder. The remaining urine is released from the bladder and filled with sterile fluid, creating a clear environment. After this, the mucous membrane of the bladder is examined. The technique of cystoscopy of the bladder involves the possibility of simultaneously taking histological analysis (small pieces of tissue) for biopsy - if suspicious areas are detected. This makes cystoscopy one of the most effective and convenient methods for diagnosing tumors and diseases accompanied by changes in the mucous membrane of a given organ. When examining the urethra, the procedure involves removing the cystoscope from the bladder and dispensing sterile liquid under slight pressure, which allows the walls of the urethra to straighten. This allows the doctor to visually examine the entire length of the urethra for the presence of polyps, narrowing of the canal, atypical neoplasms and other pathologies.
Is the examination painful? A common question that worries patients is: how will they feel during and after cystoscopy? Is the cystoscopy procedure painful? There is no need to worry: the procedure is simple, however, since the device is inserted into the bladder through the urethra, unpleasant sensations may occur. You may feel discomfort as the cystoscope is inserted into the urethra and bladder. You may feel the urge to urinate as fluid fills your bladder. If a biopsy is taken, you may feel a slight pinch. After the procedure, the urethra may be painful, and you will feel a burning sensation when urinating for one to two days. In addition, after the study, to prevent the occurrence or exacerbation of cystitis, a short course of antibiotic is prescribed. At the Omega-Kiev clinic you can undergo a cystoscopy procedure without pain . This will slightly increase the cost of the procedure, since general anesthesia will be used, which meets high European standards. The use of anesthesia eliminates fear of the procedure and completely relieves the patient of pain.
Indications for cystoscopy
- hematuria (detection of blood in the urine)
- chronic cystitis
- suspicion of a tumor
- chronic urethritis
Cystoscopy can reveal:
- inflammatory changes on the walls of the bladder and urethra
- bladder stones
- diverticula
- fistulas
- tumors
- injuries
- cause of hematuria
Very often, cystoscopy can be used not only for diagnostic, but also for therapeutic purposes:
- removal of small papillomas
- endovesical electrocoagulation of a simple ulcer,
- dissection of the ureteral orifice for ureterocele,
- injection under the bladder mucosa of various medications,
- bougienage of the urethra with its stricture,
- catheterization or stenting of the ureter,
- removing stones from the ureter using extractors,
- cystolithotripsy (crushing bladder stones).
How the cystoscopy procedure is performed The cystoscopy procedure at the Omega-Kiev clinic is performed under local or general anesthesia. The appropriate type of anesthesia is determined at a preliminary consultation. In case of general anesthesia, the patient should not eat for 8 hours before the procedure. Urethroscopy and cystoscopy for diagnostic purposes are most often performed on an outpatient basis and under local anesthesia: substances containing local anesthetics are injected into the urethra and bladder, which provide both pain relief and complete lubrication when the cystoscope is inserted. If the purpose of cystoscopy is not only an examination, but a series of manipulations or procedures (pinch biopsy, hydrodistension), then you will be offered general anesthesia (intravenous or epidural). The entire cystoscopy procedure takes up to 30 minutes, but direct examination of the bladder takes no more than 5-10 minutes, and thanks to the use of the most modern equipment (this is exactly what the Omega-Kyiv clinic has), the examination time is reduced even more. But the diagnosis turns out to be more accurate. After the procedure is completed, if it was performed under local anesthesia, the patient can immediately leave the clinic on their own. If cystoscopy was performed under general anesthesia, then after the procedure the patient is usually under observation for some time.
After cystoscopy:
- Before you go home, the doctor will discuss the results of the cystoscopy with you, the plan for further treatment and give the necessary recommendations.
- Regarding the procedure itself:
- in most cases you will be able to lead a normal life.
- you need to drink more fluid in order to dilute the urine and reduce discomfort during urination and burning.
- After a cystoscopy, you may notice blood in your urine, but the appearance of blood usually stops after a few hours.
- Contact your doctor if you have any of the following symptoms after a cystoscopy:
- fever and/or chills
- frequent urge to urinate, accompanied by pain and severe burning in the urethra
- urinary retention (inability to urinate)
- lower back pain
- blood in urine with clots
Contraindications to cystoscopy:
- acute inflammation of the bladder
- exacerbation of inflammation in the urethra, prostate or testicles
- bleeding
- damage to the urethral wall
- urethral (resorptive) fever.
Indications for cystoscopy
Which doctor prescribes cystoscopy and why?
Cystoscopy of the bladder is prescribed by a urologist to diagnose the following conditions:
- chronic cystitis with frequently recurring exacerbations (relapses);
- suspicion of urolithiasis;
- urinary disorders not diagnosed by other means;
- urinary incontinence;
- blood in the urine;
- detection of atypical cells in urine analysis;
- prolonged pain in the pelvic area;
- increased bladder activity;
- suspicion of interstitial (non-infectious) cystitis.
In addition, cystoscopy of the bladder is performed to clarify the results of standard research methods (ultrasound, x-ray, etc.) if an oncological process in the urinary tract is suspected.
The role of cystoscopy in the treatment of urological diseases
A number of therapeutic procedures are performed using cystoscopy:
- stopping bleeding;
- removal of benign and malignant tumors of the bladder;
- performing a punch biopsy;
- crushing and removing stones;
- placement of ureteral catheters;
- dissection of the stricture (narrowing of the internal lumen) of the urethra or the mouth of the ureter;
- removal of obstructions in the bladder.
Contraindications
Cystoscopy cannot be performed in the following cases:
- first trimester of pregnancy;
- renal failure and chronic liver pathologies;
- high temperature caused by various inflammatory processes in the body;
- diseases of the genitourinary system in the acute stage;
- bleeding of unknown etiology;
- elderly age of the patient;
- poor blood clotting.
Expert opinion
Daria Shirochina (obstetrician-gynecologist)
For patients with symptoms of acute cystitis, cystoscopy is contraindicated, since it can be extremely painful if the tissue is severely inflamed. In addition, the tube of the device can injure the mucous membranes, and the infection can easily penetrate deep into the tissue and spread to other organs.
Preparation for cystoscopy
Before the examination, the doctor conducts an explanatory conversation with the patient, during which the essence of the procedure and the features of preparation for it are revealed.
You may need to stop taking certain medications for a while: painkillers and non-steroidal anti-inflammatory drugs, aspirin and anticoagulants, insulin;
Some experts recommend taking the antibacterial drug Monural on the eve of the examination (in the evening around 10 p.m.) in order to prevent inflammatory and infectious complications after cystoscopy;
If the cystoscopy procedure is performed under general anesthesia, then you should not eat anything in the morning. Certain types of local anesthesia also require compliance with this condition;
Tests for cystoscopy:
- general urine analysis;
- biochemical urine analysis;
- blood for clotting.
They must be submitted a few days before the study.
Immediately before the procedure, it is imperative to hygienically wash the external genitalia, and if there is a lot of hair, shave it off to avoid individual hairs getting into the urethra along with the cystoscope.
How to prepare: recommendations
Cystoscopy requires simple actions from the patient. Recommendations are given by the endoscopist when registering for the procedure. It is important to follow the recommendations: proper preparation ensures the most accurate result of the study and prevents complications.
How to proceed:
- two days before the procedure, avoid alcoholic beverages;
- eating before the study - 12 hours;
- in the evening you need to do an enema, then drink a laxative to completely cleanse the intestines;
- For infectious and inflammatory pathologies, the doctor selects broad-spectrum antibiotics for a preventive course. The drugs are taken before and after cystoscopy as prescribed by the urologist;
- before the procedure, the patient talks with the anesthesiologist, the doctor chooses the optimal method of pain relief;
- an important point is to reduce the fear of manipulation using an endoscope;
- When a person is unsure or panicky, the doctor prescribes sedatives.
To reduce risks during or after the procedure, the urologist prescribes additional studies:
- blood sugar test;
- electrocardiography;
- general analysis of urine and blood;
- analysis of the liver complex (venous blood);
- analysis for HIV, viral hepatitis, Wasserman reaction;
- clarification of the Rh factor and blood group.
Carrying out cystoscopy
The duration of cystoscopy depends on the disease, the type of cystoscope and the qualifications of the doctor and can range from 5-10 to 45-60 minutes. The procedure is performed both in outpatient and inpatient settings.
Both therapeutic manipulations and diagnostic tests during cystoscopy are carried out in a special chair, reminiscent of a gynecological one: the patient lies on his back with his legs raised and bent at the knees. For convenience, the patient's legs are fixed on special supports.
Note: to eliminate pain during the procedure, the patient is given anesthesia. This may be a local anesthetic in the form of a solution or gel, which is injected directly into the urethra, spinal or general anesthesia.
The choice of anesthesia method is determined by the purpose of the procedure (examination or treatment) and the individual characteristics of the human body.
The patient’s external genitalia are first treated with an antiseptic, and the cystoscope tube is lubricated with sterile glycerin, which does not interfere with the transparency of the optical media. Immediately after inserting the device into the bladder, residual urine is removed from it, and then the bladder is thoroughly washed with warm furatsilin.
To assess the capacity of the bladder, it is filled with a clear solution until the patient feels the urge to urinate (the average amount of solution is 200 ml).
Next, the doctor begins to examine the bladder cavity. The examination begins with the anterior wall, then moves to the left lateral, posterior and right lateral surfaces.
Special attention is paid to the study of Lieto's triangle (the area of the bottom of the bladder). It is in this area that various pathologies are most often localized. The orifices of the ureters are also closely examined (location, number, shape, symmetry).
After removing the cystoscope, if local anesthesia was used, the patient can go home immediately. If the examination was carried out under spinal or general anesthesia, then for some time the patient remains in the hospital under the supervision of medical workers.
Features of cystoscopy in men and women
Cystoscopy in women
Women have a short urethra, so local anesthesia is usually used for diagnostic cystoscopy. When performing medical procedures that require more time than a simple examination, regional (spinal) or general anesthesia is used.
Cystoscopy in men
In men, the urethra is much longer, and the sensation when inserting a cystoscope is more painful. Therefore, male patients are given general or spinal anesthesia (regardless of the purpose of the study), and while moving the device along the urethra in order to straighten it, the penis is first raised and then lowered. This technique allows you to avoid mechanical damage to the urethral mucosa.
Types of cystoscopic examination
Today, doctors have two types of cystoscopes at their disposal - rigid and flexible. Therefore, cystoscopy is divided into two types - rigid and mobile. Rigid cystoscopy is often indicated for women. Their wide and short urethra is physiologically more suitable for a static device. Cystoscopy with a flexible cystoscope is usually recommended for men whose urethra is elongated and has a smaller diameter, as well as for children.
Tough
What does rigid cystoscopy show? As a rule, the procedure is used to study a specific “pain point” of a particular organ, and therefore does not require moving the cystoscope.
Using a rigid cystoscope, the doctor can examine the patient's organs through a special eyepiece. In this way, doctors conduct examinations of the urethra, examination and lavage of the bladder, and catheterization of the ureters.
The set of instruments for rigid cystoscopy includes optical tubes with different viewing angles, lifting mechanisms, operating and diagnostic adapters, rigid biopsy forceps and other instruments depending on the set.
Movable
Mobile (flexible) cystoscopy is done for the purpose of a comprehensive examination of the organ for accurate diagnosis of the disease. It is also used to treat an already identified disease. This method of examining the organs of the urinary system allows you to evaluate the structure of the mucous membranes, detect bleeding, defects, injuries and neoplasms.
The peculiarity of mobile cystoscopy is the use of a cystoscope, on the flexible barrel of which a video camera and a lighting device are located. A metal cord, capable of changing position, is inserted through the urethra and allows you to display an image of the bladder cavity and ureters on the screen.
Before the procedure begins, a special solution is injected there, which improves the clarity of the image. Thus, the doctor can examine the diseased organ in detail, identify the problem area and more accurately make a diagnosis.
The set of instruments for flexible cystoscopy, in addition to flexible shafts with video cameras and lighting devices, includes telescopic bridges with a deflection mechanism and instrumental channels, high-frequency electrodes of various configurations, electrosurgical loops and knives, grasping and biopsy forceps, and other instruments.
Both types of cystoscopy also allow operations with biopsy, coagulation and removal of foreign bodies.
Chromocystoscopy
To obtain information about kidney functionality, diagnostic cystoscopy in adults is often combined with another procedure, chromocystoscopy.
This study requires preliminary intravenous administration of a contrast agent, after which the doctor assesses from which ureter, after what time and at what speed colored urine will be released.
If the appearance of urine with dye is detected 3-5 minutes after the contrast is introduced into the vein, then this is normal. If excretion is delayed for up to 10 minutes, renal dysfunction is diagnosed.
What it shows: survey results
The results of cystoscopy allow the urologist to understand what processes are occurring inside the bladder and how dangerous the formations previously detected on ultrasound are. Before the procedure, it is important to thoroughly cleanse the intestines, go without food for 12 hours to avoid distortion of the results and complications, and facilitate the insertion of the cystoscope.
The results of the study reveal:
- calculi (stones that appear when salts are deposited);
- tumors;
- cysts;
- injury to the walls of the bladder;
- inflammatory processes;
- abnormalities of organ development;
- chronic type of cystitis;
- papillomas;
- internal bleeding in the bladder;
- polyps.
Cystoscopy in children
The examination of children is carried out according to the same scheme as for adults. But for children, special children's cystoscopes are used, the diameter of which is selected individually in accordance with the age of the child and the anatomical features of his urethra. In modern urology, even cystoscopes have been developed for newborn babies.
For very young children and overly active older children, the procedure is performed under general anesthesia. In other cases, local anesthesia is used.
Parents will be required to provide written consent for their child to undergo research.
Possible complications
After applying local anesthesia and performing diagnostic cystoscopy, the patient after a certain period can engage in normal activities, with the exception of heavy physical activity. If there are no complications, hospital stay is not required.
Discomfort in the bladder area should disappear within 24 hours or less. If, after this period, you experience pain or notice blood in your urine, you need to urgently visit a urologist, get examined, and rule out dangerous complications.
After general anesthesia, the patient is under the supervision of doctors until the condition returns to normal. After the operation, the patient needs hospital treatment. The duration of therapy depends on the type of surgery and general condition.
Possible complications:
- pain during urination;
- injuries to the walls of the bladder, bleeding due to damage to blood vessels;
- aspiration of the respiratory tract when the rules are violated: the patient drank water, ate food;
- relaxation of the anal sphincter if the patient has poorly cleaned the intestines;
- allergy to anesthesia with intolerance to certain medications;
- weakness, fever during anesthesia;
- penetration of infection during the introduction of a cystoscope, inflammation of the urethra, bladder;
- urinary disturbance.
Learn how to treat pyelonephritis at home in men and women.
The composition of kidney herbs and the rules for using the medicinal drink are written on this page.
Go to https://vseopochkah.com/lechenie/preparaty/urolesan.html and read the instructions for using Urolesan tablets.
Side effects and complications of cystoscopy
Blood in the urine after cystoscopy can be observed for 1-2 days. This is the norm. In addition, burning in the urethra and pain when urinating may also be felt for several days. Over time, these symptoms will disappear on their own.
Relatively often, patients may complain of the development of cystitis after cystoscopy. However, infection during the procedure and subsequent inflammation of the bladder are not always the fault of the doctors. This usually occurs due to insufficient cleanliness of the patient's external genitalia.
A puncture (perforation) of the bladder can occur as a result of the actions of an inexperienced doctor, for example, when collecting histological material, the doctor did not calculate the length of the needle and accidentally pierced the wall of the bladder.
In this case, there is severe pain after cystoscopy that does not go away for a long time, a decrease in the amount of urine excreted, an admixture of blood in it, an increase in body temperature, and chills. In such a situation, the patient requires urgent surgical care.
If the patient does not have any negative symptoms after cystoscopy, then he returns to his usual rhythm of life as soon as possible.
One of the most serious complications of cystoscopy is considered to be damage to the urethra, which results in the formation of a false tract. In this case, the patient is fitted with a cystostomy - a system for draining urine in addition to the urethra. Through a puncture of the abdominal wall in the suprapubic region, a thin tube (catheter) is inserted into the bladder, through which urine flows into an attached container. After qualified treatment, the process of normal urination is restored, and the cystostomy is removed.
What is this procedure
Features of the method:
- During a cystoscopy, the doctor gains access to the inside of the bladder. Endoscopic examination provides the most complete picture of all processes occurring inside an important organ;
- the procedure is carried out under local or general anesthesia (depending on the severity of the case and the type of manipulation);
- the doctor inserts a cystoscope (a special device) into the urethra, then into the bladder, at the end of which there is an optical device that allows you to examine every millimeter of tissue;
- When examining the walls of the bladder, polyps, foci of inflammation, stones in the ureters, erosions, papillomas, areas of traumatic injuries and bleeding, and tumors of various types are clearly visible.
Which doctor should I contact?
A urologist, nephrologist or oncologist can prescribe a cystoscopy. Indications for performing such a procedure may include: frequent pain in the lower abdomen or cystitis, blood in the urine, urolithiasis, injuries, suspected cancer, urinary incontinence, the need for a biopsy, therapeutic procedures, etc.
Cystoscopy is a highly informative diagnostic procedure and in some cases can be supplemented with therapeutic manipulations. To perform it, the patient must properly prepare for the study. After cystoscopy, the patient’s condition quickly stabilizes and is not accompanied by the development of negative consequences. Complications can only arise if the specialist performing the procedure is insufficiently qualified.
CT
One of the modern methods of studying the bladder is computed tomography. In particular, to determine urological diseases, they resort to the use of multislice CT. To enhance the diagnostic effect, the patient is injected intravenously with a radiocontrast agent. With this approach, 3-D images of the organ are obtained, showing tumors, diverticula, and stones.
Bladder cancer on a CT scan. Source: medsovet.guru
Also in medicine there is such a research method as positron emission tomography. In most cases, it is used to identify tumor formations. Unlike the previous type of CT, with this study, instead of a contrast agent, radionuclides are introduced into the body.
MRI
Magnetic resonance imaging is one of the modern methods of examining the bladder to identify pathological processes in the organ. Its main advantage is that it is highly informative, but does not have a detrimental effect on the patient’s body.
In most cases, such diagnostics are recommended for people in whom doctors suspect the presence of tumor tumors in the bladder. Thanks to this, you can find out as accurately as possible how deeply the pathological cells have spread. The only disadvantage is the high cost of MRI.
Features of the procedure in men and women
The length of the ureter in women is only 3–5 cm, which is almost 6 times shorter than in men. Therefore, in women, the procedure is faster, less painful, and even, by agreement with the patient, can be performed without pain relief.
True, in ordinary life, infection penetrates into the urinary system of women just as easily. Therefore, they need cystoscopy examinations more often than men.
If during cystoscopy it becomes necessary to perform any medical procedures on the patient, the anesthesiologist will administer general anesthesia to her.
The male urethra is longer - 15–22 cm. When inserting a cystoscope, men experience pain, and anesthesia is always used. The cystoscope is inserted gently and non-violently, with a possible spasm of the external sphincter waiting for this moment. Sometimes the doctor may ask the patient to take several breathing movements. At the first stage, the penis is lifted upward and an endoscope is inserted to the level of the sphincter ring. Then the penis is lowered and the endoscope overcomes the obstacle in the form of the sphincter.
The procedure is also complicated by the fact that the cystoscope must pass through the location of the prostate. Therefore, the procedure must be carried out extremely delicately and sparingly, otherwise the device can injure the mucous membranes of the urethra, the seminal tubercle, and even temporarily impair potency.
WHEN IS CYSTOSCOPY NOT PERFORMED?
There are a number of contraindications.
- Diagnosis is prohibited in the presence of acute inflammation of the mucous membranes and acute inflammation in the urethra.
- Cystoscopy is not performed for chronic diseases affecting the testicles and urethra.
- It is prohibited if there is an infection in the body and when a person experiences a fever or is in a state of intoxication.
Before conducting a diagnostic examination, the doctor analyzes the child’s complaints; He also explains the essence of cystoscopy and how to prepare for the procedure. If the doctor deems it necessary, you should stop taking certain medications: these may be painkillers, non-steroidal drugs, aspirin, anticoagulants. To prevent complications of cystoscopy, your doctor may recommend Monural. General anesthesia is required to perform cystoscopy. Please note that the examination is carried out only on an empty stomach. The child first undergoes blood tests. Before the procedure, hygienic cleaning of the genitals is required.
How is endoscopy performed?
Endoscopy of the urinary system allows you to examine the urethra (urethra), bladder, ureters and renal pelvis. For research, endoscopes are used - rigid or flexible (plastic or silicone) tubes equipped with optical elements (fiber optics).
As a rule, diagnosis is carried out by retrograde (transurethal) access. Examination of the renal pelvis sometimes involves an antegrade approach, in which the endoscope is inserted through a translumbar puncture into the kidney or through a nephrostomy fistula left after previous surgery.
In preparation for manipulations, a conversation is held with the patient to prevent stress and they are told in detail about the procedure. Endoscopy involves the implementation of preventive antibiotic therapy to avoid infectious complications . A cephalosporin antibiotic, Cefazolin (Kefzol), is administered intravenously.
The patient is advised to drink plenty of fluids; in addition, up to 1.5 liters of saline solution is administered intravenously and urine output is stimulated with a diuretic (Lasix, 40 mg).
To prevent the patient from experiencing discomfort, the urinary tract endoscopy procedure is performed under local or epidural anesthesia . Excessive mental lability of the subject in some cases is an indication for the use of general anesthesia, i.e. anesthesia.
With retrograde access, rigid (hard) metal catheters are used. When examining the ureter, the patient is in the usual horizontal position, and for examining the renal pelvis, the Trendelenburg position (lying on the back with the pelvis elevated at an angle of 45° relative to the head) can be used. Special dilators are often inserted into the mouth of the ureter to expand it.
Taking into account the time required for preparation, the procedure lasts on average 1 hour, although a direct examination of the organs of the urinary system takes several minutes.
After diagnostic ureteropyeloscopy, drainage of the pelvis is indicated; the catheter is left in place for 24-48 hours.
Execution method
Cystoscopy of the bladder is performed using general or spinal anesthesia. Local anesthesia can also be used if the study is carried out for diagnostic purposes.
In order to facilitate insertion of the cystoscope into the urethra, it is lubricated with sterile glycerin. With gradual advancement of the instrument, during cystoscopy the inner wall of the urethra is first examined (ureteroscopy is performed). When the tip of the cystoscope is close to the pubic symphysis, it is directed downward and enters the bladder.
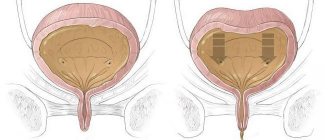
Procedure for examining the bladder
First of all, the urothelium of the anterior wall of the organ and its apex is examined. Next, the internal mucous membrane of the organ is examined in a circle by turning the cystoscope clockwise. Particular attention is paid to the area called the Lieto Triangle. The boundaries of this area are determined by the orifices of the ureters and the internal opening of the organ’s neck. The mucous membrane of Lieto's triangle is most often affected by various pathological processes.
For ease of orientation, the bladder is conventionally divided into four parts according to the watch dial. In this case, normally the air bubble, which is located at the top of the organ, will correspond to 12 o’clock, the mouth of the right ureter will correspond to 7 o’clock, and the left ureter will correspond to 5 o’clock.
During the study, the color of the endothelium is assessed, the presence of certain changes on the surface of the mucous membrane (ulcerations, areas of tissue degeneration, neoplasms, etc.). The specialist also pays attention to the location and shape of the ureteric orifices.
Normally, the urothelium has a pale pinkish color and a characteristic shine. A network of small vessels is determined on its surface. In the area of Lieto's triangle there are a significant number of larger vessels. The orifices of the ureters should be located symmetrically. Normally, they are slit-like, oval, or round in shape.
Biopsy
Cystoscopy is widely used to obtain biopsy material from pathologically altered areas of the bladder wall. Histological examination is used to diagnose neoplasms and other pathological processes. Material for analysis can be obtained in the following ways:
- Cold biopsy - tissue is collected using special forceps that are inserted through an endoscope.
- Transurethral resection (TUR biopsy) is carried out as a result of cutting off a section or completely removing the formation with an electrocoagulator. Removal instruments are also guided into the bladder to the tumor through a flexible cystoscope.
Each of these methods has its own disadvantages and advantages. With a cold biopsy, the tissue sample and the inner wall of the organ are practically not damaged, but there are difficulties in assessing the depth of spread of the tumor. TUR biopsy, in turn, allows you to determine the degree of tumor growth. In addition, thanks to the use of a coagulator, there is virtually no risk of bleeding when using this technique. The disadvantage of TUR biopsy is its relatively high invasiveness.
Laboratory methods
Bladder examinations in women can be carried out differently. In most clinical cases, laboratory diagnostics are prescribed to identify pathological processes. For example, if inflammation progresses, there will be deviations from the norm in blood tests.
This principle is often used to diagnose bladder cancer, which is indicated by persistent anemia and an increased erythrocyte sedimentation rate. Unfortunately, such studies and the indicators themselves cannot be called specific, since they fluctuate under the influence of various reasons.
Greater preference is given to urine analysis, for which either fresh morning urine or daily urine is collected. Examination of the bladder in men can be carried out using the portion method, when, for example, a three-glass test is prescribed. To understand the condition of the organ, examine the middle portion, and deviations from the norm in other glasses indicate diseases of the urethra and prostate.
If during the study an increased content of leukocytes in urine is revealed, this indicates the development of infection or inflammation. It is also worth noting that the biological fluid contains bladder cancer antigen and cells of other neoplasms. The disadvantage of diagnosis is that it is impossible to determine the exact location of the tumor.