Diagnosis of many gynecological diseases requires histological and cytological studies of the endometrium - the inner mucous membrane of the uterus. Previously, mechanical biopsy was used for this by scraping out a piece of tissue under anesthesia. Modern medical developments have made diagnosis less painful and unpleasant. One such method is uterine cavity aspirate. It can be used to take a sample of endometrial tissue with minimal risk to a woman's health.
What is uterine cavity aspirate?
Uterine cavity aspirate is the collection of endometrial cells by creating negative pressure on the surface of the mucous membrane for cytological examination. The test is done on days 6-9 or 20-25 of the menstrual cycle, depending on the direction of the diagnosis. Endometrial cells are examined for compliance with a certain phase of the menstrual cycle and the presence of atypical shaped elements. The analysis makes it possible to detect pathological processes of various types and malignant neoplasms at an early stage of development.
The need for
The use of this technique makes it possible to detect the atypical component of aspirate cells from the uterine cavity at the initial stages of the disease, which facilitates timely treatment and guarantees a successful recovery.
The need to use the method of aspiration from the uterine cavity appears in cases of bleeding during menopause, in the case of long-term use of the IUD, in cases of suspected hyperplasia of the mucous membrane, and much more. If problems are discovered in the condition of the genital organs, the woman must be examined by a specialist and undergo the necessary tests. This is due to the fact that a successful outcome in the treatment of progressive pathology in cases of oncological formations is possible only in the early stages, which can only be diagnosed using the procedure for examining aspirate from the uterine cavity.
The current level of medicine allows a graduate student to conduct an analysis of the uterine cavity during a visit to the antenatal clinic and, based on the study, determine the nature of changes in the endometrium for the presence of malignant formations in the shortest possible time. The results of the examinations, during which aspirate is collected from the uterine cavity, are usually ready within 2 days.
Indications
Endometrial aspiration biopsy is prescribed for diagnosis in the following cases:
- disturbances in the cyclicity and nature of menstrual flow;
- uterine bleeding and pathological discharge of unknown etiology;
- infertility;
- pathological changes in the endometrium (hyperplasia, hypoplasia);
- suspicion of cancer;
- control of hormonal therapy.
Most often, an analysis of the cellular structure of the uterine mucosa is prescribed to women planning a pregnancy, especially with an unfavorable outcome of previous attempts at conception and poor ultrasound results.
How is aspirate collected from the uterine cavity?
Of course, every woman who is prescribed a uterine cavity aspirate is concerned about how painful the procedure is and how to prepare for it. Previously, the tissue sampling process was carried out using Brown syringes, which could result in pain for the patient. Today, modern methods make it possible to use either special vacuum syringes, which are produced in the States, or Italian cannulas for this procedure. To minimize the degree of pain, an anesthetic pharmacological agent is used an hour before the procedure.
Aspirates from the uterine cavity are taken from days 20 to 25 of the menstrual cycle. During the procedure, the doctor performs the following manipulations:
- The external genital organs are disinfected with iodonate;
- The cervical section of the uterus is exposed using speculum;
- The cervix of the uterine organ is grasped with bullet forceps;
- An aspirate is taken from the uterine body using a syringe (vacuum);
- At the end of the procedure, the external genital organs are processed again.
An aspirate from the uterine cavity takes a few minutes and is usually carried out in a antenatal clinic. The patient does not need to register for a hospital stay. No special preparation is expected on the part of the woman, other than ordinary hygiene procedures.
Contraindications
In order to avoid complications and not put a woman’s health at additional risk, it is prohibited to perform a biopsy in the following conditions:
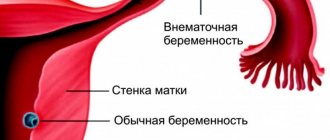
- pregnancy;
- infectious and inflammatory diseases of the genitourinary system;
- acute inflammation of the external and internal genital organs;
- pathologies in the development of the uterus;
- bleeding disorders associated with chronic diseases or medications.
Carrying out the procedure during anticoagulant therapy requires temporary withdrawal of drugs.
Hysteroscopy or aspirate?
Hysteroscopy can be diagnostic and surgical. After hysteroscopy, some consequences are possible: pain in the abdomen and lower back, discharge.
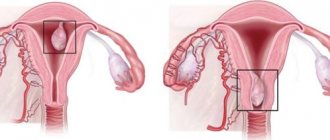
During hysteroscopy, the uterus is examined from the inside using probes equipped with light guides and microvideo cameras. After hysteroscopy, which was performed for diagnostic purposes, the doctor can more accurately establish the diagnosis and prescribe the correct treatment. Surgical hysteroscopy is carried out with the aim of inserting into the uterine cavity the instruments necessary to remove polyps and other tumors. This operation is also performed to collect material for a biopsy.
Hysteroscopy can be performed if there is a suspicion of cervical cancer, perforation after previous surgical interventions and to clarify the correct position of the intrauterine device. The procedure is advisable after treatment with hormonal drugs and in case of infertility, miscarriage and spontaneous miscarriages.
Pregnancy and IVF after hysteroscopy
It is impossible to accurately answer whether pregnancy will occur after hysteroscopy and whether it will be successful. This does not depend on the operation itself, but on the diagnosis that will be given to the woman. Unsuccessful pregnancies or attempts at in vitro fertilization may not always be an indication for hysteroscopy. The gynecologist usually starts from a number of additional reasons.
But it is hysteroscopy that can accurately determine the condition of the fallopian tubes and uterine defects.
As for IVF after hysteroscopy, women should be patient. The in vitro fertilization procedure can be carried out only when the body has fully recovered after hysteroscopy and has undergone preventive rehabilitation.
Contraindications to hysteroscopy
Hysteroscopy is contraindicated in the following cases:
if there is an inflammatory process of the reproductive system; with acute infectious diseases or chronic diseases in the acute stage; with a normally progressing pregnancy; with widespread cancer or stenosis of the cervix; during severe uterine bleeding, bleeding disorders; if the patient is in a serious physical condition (condition after a heart attack, in acute renal and cardiovascular failure, decompensation of diabetes mellitus and others).
Hysteroscopy is an opportunity not only to most accurately establish a diagnosis, but also to cure many female ailments. Do not be afraid, the operation is not complex, is not very painful, and if you follow the doctor’s recommendations, it does not cause complications.
Types and methods of the procedure
The technique for taking an endometrial sample involves creating a vacuum in the uterine cavity and then sucking out the tissue sample. For this purpose, Brown syringes and disposable cannula catheters are used. The procedure technique differs depending on the chosen instrument. Before diagnosis, there is no need to dilate the cervix, which significantly reduces pain and reduces the risk of complications. To prepare for the test, a woman needs to consult with a gynecologist to determine if there are contraindications and carry out standard hygiene procedures, as before a regular visit to the doctor.
Carrying out the procedure, pain relief
Aspiration biopsy is performed on an outpatient basis in a treatment room. It is carried out on a gynecological chair, where the doctor will first install the dilator in the vagina and perform aseptic treatment.
General anesthesia is not required for this procedure; a local anesthetic applied to the cervix is sufficient. This is usually sufficient, although women with a high pain threshold may experience slight discomfort.
After the local anesthesia has taken effect, a cannula is inserted into the cervical canal - a kind of hollow needle with a blunt end.
It is needed to take an aspirate, so it is attached to a flexible probe, where negative pressure is created manually or using a compressor. A section of the endometrium is separated under vacuum and sucked into the cannula.
Next, the doctor treats the taken material with a preservative, performs repeated antiseptic treatment of the vagina and cervix, and removes the dilators. After this, the patient can go home.
The duration of the procedure is 10-15 minutes. After 3-7 days, the attending physician can analyze the cytological data.
For 20-24 hours after taking the aspirate, the woman may feel mild pain and may have some bleeding.
Recommendations after the procedure
Although aspiration biopsy is a harmless procedure, for 3 days after the test a woman should adhere to the following recommendations:
- Do not have sexual intercourse.
- Do not swim in open waters and pools.
- Do not use tampons.
- Avoid hypothermia.
- Regularly perform genital hygiene and change underwear.
According to the indications of the gynecologist, the patient may be prescribed local or systemic antibacterial agents. Compliance with such preventive measures helps to avoid infection and unwanted consequences after the procedure.
Preparation
The patient is not required to take any specific preliminary measures. An hour before taking the aspirate, you should wash your face. Since there is a possibility of bleeding during and after sampling, stop taking blood thinners 4-5 days before the procedure. Before the procedure, you should not take painkillers on your own, douche or insert vaginal suppositories.
Since endometrial biopsy is a surgical diagnostic method, it can only be prescribed after a thorough examination. Medical preparation for tissue aspiration includes:
- gynecological examination of the patient;
- general blood analysis;
- blood testing for HIV, syphilis, hepatitis;
- microscopy of the separated cervical canal to determine the composition of the microflora;
- bacterial culture of a smear from the cervix;
- examination of scrapings from the cervix for herpes, cytomegalovirus, chlamydia and other sexually transmitted infections;
- Ultrasound of the pelvic organs.
If inflammation in the genitals or sexually transmitted infections is detected, the study is carried out only after complete cure or transfer of the disease to an inactive phase. Before aspiration biopsy, the doctor also needs to make sure that the patient is not pregnant.
Possible complications
Taking an aspirate from the uterine cavity does not require invasive intervention into the mucous membrane. But, despite all the precautions, the professionalism of the gynecologist, the safety and sterility of the instruments, sometimes minor injury to the endometrium is possible. It manifests itself with the following symptoms:
- lower abdominal pain;
- bleeding from the vagina;
- general weakness;
- low-grade fever.
Damage to small blood vessels can cause intrauterine bleeding, which is accompanied by low blood pressure, dizziness and nausea. Injury to the mucous membrane often leads to infection of the uterine cavity with further development of the inflammatory process. Externally, this is manifested by pathological discharge, pain and discomfort in the lower abdomen. If any suspicious symptoms appear within a few days after the procedure, you should immediately consult a gynecologist.
Features of the method
The procedure for collecting aspirate from the uterine cavity is carried out on the twenty-fifth day from the start of menstruation. If there is menopause, patients can undergo this examination at any convenient time. Removing material from the uterine cavity for further research occurs in two ways, using a syringe and a catheter inserted into the uterine cavity. The second method uses a flushing method using a sterile sodium chloride solution injected through a syringe and then drawn back in. The resulting liquid, after a series of procedures using rotation, provides material for further study.
Modern medicine offers improved medical instruments for use to obtain material for research. For example, aspirate from the uterine cavity using the vacuum method differs in many ways from previously used options. Through the slightly open cervix, the depth of the fundus of the uterine cavity is measured, then the required amount of material is taken for further research using a vacuum syringe and cannula. The resulting sample is sent for final analysis.
Why is aspiration biopsy prescribed?
The study is used as a screening method for the condition of the endometrial layer of the uterus:
- during hormonal therapy;
- for endometrial diseases;
- with unsatisfactory results of ultrasound of the uterus;
- if neoplasms are suspected, as well as for their diagnosis (fibroids, polyps);
- for menstrual irregularities;
- with extracurricular or excessive uterine bleeding.
Often, an aspiration biopsy is preceded by an extended video colposcopy procedure - a study of the structure of the tissues of the external genitalia, vaginal mucosa and cervix using a gynecological microscope and chemical reagents, which allow identifying possible areas of degeneration of healthy tissue. On the recommendation of a gynecologist, if atypical endometrial cells are suspected, it is advisable to carry out both procedures in one step.
Contraindications for taking endometrial samples from the uterine cavity are pregnancy and the presence of active infectious processes in the urogenital area.
How painful is the endometrial aspiration biopsy procedure?
A standard aspiration biopsy from the uterine cavity can be quite painful. If necessary and at the request of the patient, the doctor uses anesthetics and antispasmodics to alleviate the condition. Endometrial aspiration is also performed using a vacuum method - this method causes less discomfort, however, it also has some likelihood of complications. Among them:
- microtrauma of the walls of the uterus and cervical canal;
- spasmodic pain in the lower abdomen on the day of the procedure;
- bleeding;
- menstrual irregularities (for the next 1 cycle).
Pipelle biopsy is the most gentle version of the procedure, during which no manipulation is required to dilate the cervix. In addition, the likelihood of painful sensations is reduced to a minimum, and the actual collection of endometrial aspirate lasts no more than a minute.
If you have been prescribed an aspiration biopsy from the uterine cavity, entrust it to experienced professionals - gynecologists at the AllergyFree clinic. Make an appointment directly on our website or by phone with the administrators of the diagnostic and treatment center to undergo a pipel biopsy and receive reliable information about the state of your health - in a comfortable environment, using modern equipment and advanced methods.
Contraindications and possible complications
Contraindications for uterine probing are:
- suspicion of intrauterine pregnancy.
When probing the uterus, a false tract can be formed or its wall can be perforated. This can happen if a vaginal examination is not performed before probing and the position of the uterus is not determined, as well as if the probe is inserted with force.
The diagnostic operation of uterine probing is easily tolerated by patients and, if all the rules of preparation for its implementation are followed, has a minimal number of complications.
Possible complications after the procedure
When uterine cavity aspirate is collected, there is a fairly small percentage that serious consequences may occur. In rare cases, injury to the mucous membrane of the uterine body may occur, which entails pain in the abdominal area, radiating upward, closer to the collarbone. If blood vessels are injured during manipulation, there is a high probability of internal bleeding. And, as you know, as a result of blood loss, blood pressure drops, nausea appears, and dizziness occurs. Also, for some time the patient may notice small bloody discharge.
Another possible consequence after aspiration may be the onset of an inflammatory process in the uterine cavity. In this case, the woman experiences weakness, pain in the abdominal area, and the overall body temperature may rise significantly. Inflammatory symptoms may appear immediately after the procedure or several days later. However, many patient reviews indicate that such complications occur quite rarely.