Every woman should know what uterine adenomyosis is, since as this pathology progresses, tumor processes can occur in the reproductive system of an adult woman, and this disease also leads to infertility.
In simple terms, this is a hormone-dependent pathology, which in most cases is diagnosed in women of childbearing age, but in some cases the disease can develop in very young girls, as well as in women in the premenopausal period.
Disease code according to ICD-10 No. 80.1.
The essence of pathology
Every month, the endometrium grows in the inner layer of the reproductive organ - this is the layer that is necessary for the egg, after fertilization, to attach to the uterus and continue its development.
If conception does not occur, most of the endometrium is torn off and expelled, that is, menstruation occurs.
The endometrium is not completely rejected - a growth layer remains, which grows again until the next menstruation or conception.
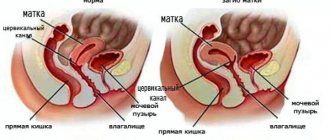
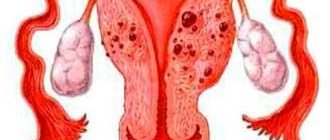
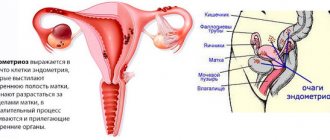
With adenomyosis, endometrial cells divide with excessive activity, and they not only pathologically increase inside the uterus, but also grow into its muscle layer, and even extend beyond the organ.
Endometrioid cells can grow into neighboring organs that are not reproductive, and significantly impair their function.
In fact, adenomyosis is a form of endometriosis.
Expert opinion
Shustova Olga Leonidovna
Obstetrician-gynecologist of the highest category
Adenomyosis in the initial stages is rarely accompanied by a clear clinical picture, and a woman, even noticing minor pathological signs, is in no hurry to see a doctor. However, it is necessary to understand that such a negligent attitude towards one’s health can lead to extremely serious consequences. As the disease progresses, the affected muscle fibers of the reproductive organ thicken unevenly, resulting in deformation of the organ. In this case, disturbances in the monthly cycle are observed, and problems with conception naturally arise. The insidiousness of this disease is that the endometrium, which has grown into the muscular layer of the uterus, is not removed from the body, which means that the development and increase in the number of functional cells occurs constantly, such processes can provoke the development of neoplasms, as well as persistent infertility.
https://youtu.be/ToQYW4nB99U
Diagnostics
To prescribe safe treatment, it is worth discussing the plan with a general practitioner, hematologist, endocrinologist and gastroenterologist. Special preparation is required before surgery. First, your current health status is assessed using various blood and urine tests. The blood type and Rh factor are also determined (transfusion is required during the operation). Vaginal smears are re-examined to determine the state of the microflora. The condition of the heart and lungs is also checked.
These precautions are not always necessary, but they help avoid complications and negative consequences.
Methods for diagnosing adenomyosis:
- examination on a gynecological chair;
- colposcopy;
- Ultrasound of the pelvic organs;
- study of smears;
- laparoscopy, hysteroscopy.
Signs of adenomyosis on ultrasound:
- increased organ size;
- heterogeneous structure of the muscle layer or heterogeneous echogenicity;
- unclear border between myometrium and endometrium;
- the presence of foreign lesions in the muscle layer;
- sharp thickening of one wall of the uterus.
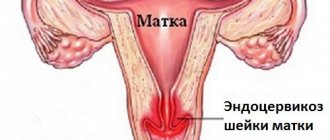
When examined in a gynecological chair, the doctor diagnoses an enlarged uterus and its rounded shape. Hysteroscopy can confirm the diagnosis. It shows points on the endometrium that correspond to areas where the tissue has grown into the muscle layer.
Sometimes magnetic resonance imaging is used to make a diagnosis. MRI is indicated when ultrasound does not find reliable signs of adenomyosis. Most often this occurs in the nodular form, combined with uterine fibroids. The method allows for differential diagnosis, that is, to distinguish adenomyosis nodes from fibroids.
First signs
As already mentioned, the initial stages of adenomyosis proceed unnoticed.
But after some time, the woman notices disruptions in the monthly cycle. As a rule, the duration of physiological bleeding increases, the volume of discharge increases, and bloody clots are observed.
NOTE!
Quite often, the pathology does not appear at all for a long time, and it can only be suspected if infertility develops.
If a woman cannot conceive a child within six months, subject to regular and unprotected sexual intercourse with one sexual partner, she is recommended to undergo a thorough examination for adenomyosis, among other things.
Forecast
Adenomyosis is a disease with a chronically relapsing course. The statistics of relapses after successful non-radical treatment (conservative therapy, organ-saving surgery) is about 20% per year. After five years, the relapse rate reaches 74%.
The most lasting effect is observed with the combined use of surgical (organ-preserving operations) and conservative (hormonal therapy) methods of treating adenomyosis, however, in most cases, relapses are still inevitable.
The prognosis for premenopausal women is somewhat better, since the activity of the process subsides with the physiological decline of ovarian function. In patients who have undergone radical surgery (removal of the uterus and ovaries), the process does not resume.
Symptoms of the disease
Common clinical manifestations of adenomyosis in later stages are as follows :
- Disruptions in the menstrual cycle.
- Presence of clots.
- Pain in the lower abdomen, which becomes more intense during menstruation. How severe the pain will be depends on the nature of the changes in the tissues of the organ, on the presence or absence of the inflammatory process, as well as on the exact location of the nodular formations of the pathology. If they are localized in the cervical region, the pain will be quite severe. In addition, if a bacteriological infection is included in the pathological process, the patient’s general condition will worsen and the pain will intensify.
- Intermenstrual bleeding, which is possible when the blood vessels in the walls of the reproductive organ are damaged.
- Dyspareunia is the presence of pain in the vaginal part.
If a woman experiences intermenstrual bleeding, as well as heavy and prolonged menstruation, this leads to the development of anemic syndrome.
In this case, weakness, pallor of the skin and mucous membranes develop. With complications of a bacterial nature, body temperature rises, headaches and other signs of intoxication appear.
An increase in temperature due to adenomyosis is a good reason for urgent consultation with a doctor..
Adenomyosis (Uterine Endometriosis)
The most characteristic sign of adenomyosis is long (over 7 days), painful and very heavy menstruation. Clots are often detected in the blood. Brownish spotting is possible 2-3 days before menstruation and 2-3 days after it ends. Intermenstrual uterine bleeding and brownish discharge in the middle of the cycle are sometimes observed. Patients with adenomyosis often suffer from severe premenstrual syndrome.
Another typical symptom of adenomyosis is pain. Pain usually occurs several days before the start of menstruation and stops 2-3 days after it begins. Features of the pain syndrome are determined by the localization and prevalence of the pathological process. The most severe pain occurs with damage to the isthmus and widespread adenomyosis of the uterus, complicated by multiple adhesions. When localized in the area of the isthmus, the pain can radiate to the perineum; when located in the area of the angle of the uterus, it can radiate to the left or right groin area. Many patients complain of pain during sexual intercourse, which intensifies on the eve of menstruation.
Clinical manifestations of the disease may not correspond to the severity and extent of the process. Grade 1 adenomyosis is usually asymptomatic. In grades 2 and 3, both an asymptomatic or low-symptomatic course and severe clinical symptoms can be observed. Grade 4 adenomyosis is usually accompanied by pain caused by widespread adhesions; the severity of other symptoms may vary.
During a gynecological examination, changes in the shape and size of the uterus are revealed. With diffuse adenomyosis, the uterus becomes spherical and increases in size on the eve of menstruation; with a widespread process, the size of the organ can correspond to 8-10 weeks of pregnancy. With nodular adenomyosis, tuberosity of the uterus or tumor-like formations in the walls of the organ are detected. When adenomyosis and fibroids are combined, the size of the uterus corresponds to the size of the fibroids, the organ does not shrink after menstruation, and other symptoms of adenomyosis usually remain unchanged.
Etiology of the phenomenon
For what reason adenomyosis develops, scientists still have not reliably found out, however, there is reason to believe that this disease can be provoked by the following reasons:
- congenital anlage of endometriosis, which occurs due to pathologies of embryonic development,
- the introduction of endometrioid cells into surrounding tissues as a result of traumatic childbirth or surgical manipulations in the reproductive organs;
- the onset of sexual activity is too late or absent;
- late pregnancy and childbirth;
- early onset of menstruation;
- hereditary predisposition to the development of benign or malignant neoplasms in the reproductive organs;
- excess weight;
- long-term and uncontrolled use of oral contraceptives;
- intrauterine device;
- immune pathologies;
- stress;
- excessive physical activity.
Reasons for appearance
Experts note that today the causes and mechanisms of the pathology have not been fully determined. They speak with confidence about one thing - the disease is hormone-dependent, its development is often triggered by disturbances in the functioning of the immune system.
The cause of the disease may be mechanical damage to the uterus and the integrity of its inner layer. Curettage causes the development of an inflammatory process, and the “protective” layer between the endometrium and muscles is disrupted. As a result, endometrial cells freely penetrate deeper, continuing the process of cyclic function.
Risk factors
Experts have identified risk factors that increase the possibility of developing pathology:
- hereditary predisposition;
- early or late onset of menstruation;
- overweight, obesity;
- late onset of sexual activity;
- difficult childbirth;
- abortions, diagnostic curettages;
- use of a vaginal device or oral contraception as contraception;
- diseases of the inflammatory process of the appendages, uterus, bleeding;
- previous immune and allergic diseases that impair the functioning of the immune system;
- low standard of living;
- physically hard work;
- constant stress, sedentary lifestyle;
- diseases of the gastrointestinal tract, hypertension;
- state of ecology.
What is the danger?
Adenomyosis is a rather dangerous disease that requires quality treatment.
If this pathology is ignored, the following consequences may develop::
- Transformation into oncology. Of course, it is impossible to say that adenomyosis will necessarily end in cancer, but women with this diagnosis increase the risk of developing this disease. This happens due to constant hormonal fluctuations. Adenomyosis does not lead to cancer, but only increases its possible risk (the pathology is shown in the photo).
- Anemia. With constant bleeding and prolonged heavy menstruation, anemia develops, which entails oxygen starvation of the entire body.
- Infertility. If adenomyosis progresses to grades 3 and 4, the endometrium becomes incompetent and pregnancy is impossible. But even in the first two stages, when conception is in principle possible, maintaining a pregnancy is quite difficult.
- Disruptions in the menstrual cycle, which can significantly worsen a woman’s quality of life.
What happens in the body?
The endometrium is the inner layer of the uterus, which normally does not extend beyond the reproductive organ. With pathological cell division, they can spread not only to other organs of the female reproductive system (ovaries, fallopian tubes, vagina), but also to other tissues of the body - for example, to the gastrointestinal tract, urinary system, navel and post-operative wounds.
Most often, endometriosis is concentrated specifically on the genitals, and can be either external (when abnormal cell division is observed in the ovaries or vagina) or internal, concentrated in the uterus. ICD 10 lists all types of endometriosis according to its location:
- On the ovaries. The presence of nodes can lead to the formation of endometrioid cysts. In the international classification, this disease is assigned the number 80.1;
- On the fallopian tubes, which can lead to the lumen of the tube closing and the inability to get pregnant. Classification number – 80.2;
- On the peritoneum - number 80.3;
- In the vagina and in the area between the uterine cervix and the rectum - number 80.4;
- On the intestines, as a result of which obstruction and problems with stool may develop - number 80.5;
- On sutures after operations - number 80.6, characterized by bleeding of the suture during menstruation;
- In other organs and tissues of the body - number 80.8.
Once in the wrong place, the cells of the inner uterine layer continue to work as if they were in the uterus, that is, they are exfoliated according to the menstrual cycle. This leads to the development of an inflammatory process that must be urgently stopped, otherwise it will lead not only to disruptions in the functioning of the organ, but also to its complete stop. For example, if endometrial cells get into the myometrium, this can lead to degenerative changes, so adenomyosis of the uterine body will sooner or later lead to the inability to conceive and carry a child.
Types of illness
The following types of pathology are distinguished::
- Focal adenomyosis - single lesions. This form is more common in women over 40 years of age.
- Diffuse - uniform distribution of pathologically overgrown endometrium over the entire surface of the myometrium. This form is characterized by the presence of so-called “blind pockets” that penetrate into the deep layers of the uterus and can open into the pelvic space.
- Nodal. In this case, the formation of nodes that contain bloody fluid is observed. The formation of nodes is due to the fact that menstrual blood penetrates into the muscles of the reproductive organ. Nodules do not have capsules, since the node consists of tissue particles and lipolytic enzymes that destroy protein and fat molecules.
Types of adenomyosis
The disease can take several forms and develop to different levels. There are 3 known types of it:
- Diffuse. With it, mucosal cells form foci of varying depths in the thickness of the myometrium;
- Nodal. In this case, endometrial tissue leaks through the protective membrane, forming corridors. Then they begin to rapidly divide, spreading into the myometrium with the formation of nodules, wrapped on the outside with connecting material and filled with brown liquid on the inside;
- Mixed. This type of internal endometriosis is diagnosed more often than others and is a mix of diffuse tissue growths and nodular ones.
Whatever category adenomyosis belongs to in a particular case, the ICD 10 code will be No. 80.0.
Degrees of adenomyosis
The degree of adenomyosis is determined depending on the depth to which the pathological tissue penetrates:
- The first degree - endometrial germination is observed only in the submucosal layer.
- Second degree - pathological lesions reach half of the muscular layer of the reproductive organ.
- Third degree - the entire thickness of the myometrium is penetrated.
- Fourth degree - endometrioid tissue extends beyond the uterus and affects the peritoneum and the organs that are located in it.
Treatment of adenomyosis
Since endometriosis depends on the level of estrogen in the blood (this situation improves during pregnancy, when a physiological low level of estrogen is created), its drug treatment is aimed at suppressing estrogen secretion.
The focus of endometriosis responds to changes in the level of sex hormones in a similar, but not identical, way to normal endometrium. Methyltestosterone and other androgenic drugs (except danazol), as well as diethylsilbestrol, are not currently used for endometriosis because they are ineffective, have many side effects and have an adverse effect on the fetus when pregnancy occurs during treatment.
Drugs used in the treatment of adenomyosis
1) Oral contraceptives - they simulate pregnancy, cause amenorrhea and decidual reaction of normal endometrium and foci of endometriosis. Often with such treatment, necrosis of endometriosis foci occurs and their complete disappearance. For treatment, any oral contraceptives containing at least 0.03 mg of ethinyl estradiol can be used. They are prescribed continuously for 6-12 months. A decrease in painful periods and lower abdominal pain is observed in 60-95% of patients. The pregnancy rate immediately after treatment reaches 50%. The relapse rate is 17-18% and increases every year by 5-6%.
2) Progestogens are quite effective, at a cheaper cost (than, for example, danazol). Cause atrophy of endometrial foci. Typically the following drugs are used:
- Gestrinone – 1.25-2.5 mg 2 times a week; suppresses the growth of endometriosis foci, but does not lead to their disappearance. Leads to drug-induced amenorrhea. Menstruation returns a month after discontinuation of the drug.
- Dydrogesterone – 10 mg 203 times/day
- Medroxyprogesterone - the most studied for endometriosis - is used as follows: at a dose of 30 mg / day eliminates pain; can be increased with bloody discharge.
Side effects of this group of drugs include: nausea, weight gain. Bloody discharge is possible, for the relief of which estrogen is often prescribed in short courses.
3) Androgens. Danazol – prevents the growth of old foci, and causing amenorrhea, and new foci of endometriosis. Causes long-term remission in endometriosis and is effective in a number of autoimmune diseases. Prescribed at a dose of 800 mg/day or 600 mg/day. First, it is used in a dose of 200 mg 2 times a day, then increased until drug-induced amenorrhea occurs and the manifestations of the disease begin to decrease. This drug has serious side effects: weight gain, decreased sex drive, cosmetic defects (acne, rash). May damage liver cells, therefore it is contraindicated for liver diseases. It is canceled when pregnancy occurs, since the risk of virilization of a female fetus (appearance of male sexual characteristics) is extremely high.
4) GnRH analogs . These include: leuprolelin, buserilin, nafarelin, histrelin, goserelin, etc. Directions for use: intranasally (drops or spray), subcutaneously or intramuscularly. Treatment is carried out until the level of estradiol in the blood serum reaches 20-40 pg/ml. It is necessary to control ethinyl estradiol in the blood, since its further decrease can lead to osteoparosis. Complications include: atrophic vaginitis, decreased libido and osteoparosis. To prevent the latter complication, it is necessary to administer it simultaneously with estrogens and progestogens. Osteoparosis remains a pressing problem when treated with these drugs (the most applicable in our country is buserilin), since treatment often lasts more than 6 months, while bone density improves just after 6 months. starts to decline.
The doctor decides which drug to prescribe depending on the severity of adenomyosis and the presence of contraindications. Any self-treatment of adenomyosis is impossible and inherently stupid.
Diagnostic methods
In the early stages of the pathology, it is difficult to diagnose. To identify the disease, a thorough clinical examination of the patient is necessary.
Most often prescribed:
- Gynecological examination in a chair. In this case, the doctor assesses the size of the uterus and its cervix, its shape, position, mobility and the presence of pain.
- Smear for cytology.
- Colposcopy of the cervical region. During this study, single cells of the germinating endometrium can be seen.
- Ultrasound. In most cases, transvaginal examination is used, which provides the maximum amount of information about the pathology.
- Hysteroscopy.
- Examination of all systems and organs for the presence of endometriotic lesions.
Adenomyosis in ICD 10
In the international classification system of diseases ICD 10, pathology is included in the class of endometriosis. Has code N80.0 along with endometriosis. This subclass in ICD 10 is included in the class of non-inflammatory diseases of the female genital organs. The fact that in ICD 10 these 2 pathologies are not separated by code indicates their comparability.
With adenomyosis, the tissue grows in the other direction, into the muscle layer, but has the same structure as with classic endometriosis of the uterus. It should be noted that the main role of ICD 10 is statistical. At the same time, the document is normative; it provides a general standard of approaches to defining diseases.
According to ICD 10, the methodological approaches to adenomyosis and endometriosis are the same. Endometriosis of other organs in ICD 10 has different codes, but belongs to the same class N80.
Conservative treatment
Conservative treatment involves taking hormonal medications.
Oral contraceptives are the most common medications prescribed for the treatment of adenomyosis..
The intake must be supervised by a doctor, since it is important to monitor the concentration of hormones in the body.
When oral contraceptives are taken correctly, pain is reduced, intermenstrual bleeding is stopped, and hormonal balance is improved.
The most commonly prescribed are Jess, Marvelon, Janine, Logest.
Antigonadotropins are prescribed to reduce the concentration of pituitary hormones. They affect the activity of the ovary and also prevent the endometrium from growing pathologically. Danol or Danazol are prescribed.
IMPORTANT!
Do not be alarmed if menstruation does not occur while taking medications; this is a temporary phenomenon, and after the course of treatment the menstrual cycle will improve.
Progestogens are needed to reduce estrogen concentrations.
Thus, you can quickly eliminate the negative symptoms of the disease. These drugs do not affect the functionality of the ovaries, but they reduce the volume of menstruation and eliminate excessive growth of the endometrium.
The doctor may prescribe Norkolut or Duphaston.
Antiestrogens are synthetic drugs that slow down the production of hormones by the pituitary gland, and also reduce the concentration of other hormones that can provoke the growth of the endometrial layer.
Prescribed Depo-Prover, Gestrinone.
Smear for cytology. They are necessary to stimulate the sex glands.
Antiandrogens - Visanne, affect the general condition of the reproductive system, and also help to increase the concentration of progesterone, resulting in a gradual decrease in estrogen levels.
In addition to hormonal drugs, anti-inflammatory drugs are used to treat adenomyosis - Nurofen, Ibuprofen, Paracetamol and others, which in addition to the anti-inflammatory effect have an analgesic effect.
As for physiotherapeutic techniques, balneotherapy, magnetic therapy, low-frequency pulsed currents, etc. are considered effective..
Treatment
Adenomyosis is treated by a gynecologist-endocrinologist. Therapy for pathology can be conservative, surgical or combined. When choosing treatment tactics, take into account:
- patient's age;
- desire to preserve reproductive function;
- prevalence and severity of the process;
- concomitant gynecological diseases.
Conservative therapy
Based on the intake or administration of hormonal drugs:
- Oral combined contraceptives. They block cyclic processes in the endometrium and endometrioid heterotopias. Long-term use causes sclerosis and obliteration of the endometriotic ducts. They use new generation drugs (Janine, Logest, Visanne, Marvelon and others).
- Progestins (pure gestagens). Promote atrophy of endometrioid lesions (duphaston, norkolut, premalut).
- Androgens. Suppress ovulatory synthesis of gonadotropins. They block receptors for progesterone, estrogens, androgens, inhibit the growth of endometriotic heterotopias and the formation of new ones (danazol).
- Analogues of gonadoliberins. They block the production of gonadotropins, which reduces the production of sex hormones in the ovaries (goserelin, buserilin).
In addition to hormone therapy, iron supplements are prescribed in parallel for the treatment of chronic posthemorrhagic anemia, NSAIDs (indomethacin, ibuprofen) to relieve a painful attack, vitamins, drugs that normalize liver function, sedatives, and in cases of severe disturbance of the psycho-emotional state, antidepressants and tranquilizers. The Mirena IUD (contains gestagen) has been successfully used for a period of 5 years (reduces menstrual flow).
Surgery
It is the only reliable way to get rid of the disease. There are gentle and radical operations. Surgical intervention is performed when:
- nodal forms;
- combination of diffuse adenomyosis and uterine fibroids;
- high risk of malignancy;
- 3 degrees of process.
Gentle methods include electrocoagulation (endometrial ablation) of endometriotic lesions and intrauterine adhesions using an electrocoagulator during hysteroscopy. Radical operations include supravaginal amputation of the uterus, hysterectomy, panhysterectomy. Before surgery, hormone therapy is carried out for several months, which stabilizes the course of adenomyosis and prevents the growth and formation of new endometrioid lesions (combined treatment).
Planning and management of pregnancy
Patients with established adenomyosis are recommended to try to become pregnant no earlier than 6 months after the end of hormone therapy or endometrial coagulation. Indications for IVF are:
- absence of pregnancy for a year;
- obstruction of pipes;
- persistent anovulation.
Pregnancy is diagnosed in 30% of patients with 1–2 degrees of adenomyosis, in 14% with 3–4 degrees. In the first trimester of gestation, gestagens are prescribed (duphaston, utrogestan), subsequent treatment with hormones is carried out according to indications (threat of miscarriage, low progesterone levels). Pregnancy has a positive effect on the course of the process, inhibiting the growth of endometriotic lesions.
Surgical intervention
Surgical treatment is prescribed when conservative methods remain unsuccessful, the patient develops anemia, and also when the disease develops in a menopausal woman.
Also, surgical intervention is indicated for grades 3 and 4 of the disease, when the pathology has a negative impact not only on the reproductive organs, but also on other organs of the pelvic region.
The following types of operations are recommended:
- Abdominal . An incision is made directly above the area of pathology, and after the necessary surgical manipulations, the functionality of the reproductive organs is restored and the symptoms of the disease are eliminated. There is a risk of relapse.
- Hysteroscopy . In this case, surgeons use a hysteroscope for the operation. All manipulations are performed through the vagina, and the doctor monitors the progress of the operation on a monitor.
- Laparoscopy . Several incisions are made in the abdominal cavity, into which a lighted camera and a set of surgical instruments are inserted. Such an intervention does not require sutures and is practically not accompanied by complications.
After surgery, the woman is prescribed medications that will have a positive effect on the functionality of the reproductive organ..
Causes
The occurrence of endometriosis is explained by several theories, the main ones are:
- implantation - based on the reflux of menstrual blood from the uterus through the oviducts into the abdominal cavity;
- metaplastic – explains the formation of endometrioid heterotopias from the remains of embryonic tissues;
- induction – the appearance of endometrioid lesions under the influence of exogenous and endogenous unfavorable factors.
Factors predisposing the development of pathology include:
- heredity (the family has relatives with adenomyosis, uterine cancer, fibroids);
- traumatization of the uterine mucosa (curettage of the uterine cavity, hysteroscopy, hysterosalpingography, insertion/removal of an IUD, abortion, removal of uterine polyps);
- long, complicated labor;
- inflammatory processes in the uterus, organ surgery;
- hormonal disorders (late menarche and onset of sexual activity, irregular cycles, treatment with hormonal drugs, taking COCs, obesity);
- chronic pathology that weakens the immune system (digestive tract diseases, hypertension, allergic reactions, thyroid diseases);
- frequent infectious diseases;
- stress, intense physical activity;
- disturbed ecology, frequent climate change, prolonged insolation, low social level;
- late first birth, refusal of pregnancy.
Effect on pregnancy
In some cases, the lack of pregnancy with adenomyosis is due not only to excessive growth of the endometrium, but also to a hormonal imbalance.
But most often the cause of infertility lies precisely in the mechanical obstruction of pathological foci for the migration of the egg or seminal fluid.
However, despite the small probability, pregnancy with this disease is still possible, but not desirable.
The disease can cause spontaneous abortion and also negatively affect the development of the fetus.
Prevention
Prevention of uterine adenomyosis mainly comes down to regular visits to a gynecologist. A specialist can correctly interpret such symptoms in a timely manner and prescribe appropriate treatment.
Also recommended:
- Undergoing pelvic ultrasound 1-2 times a year.
- Gynecologists believe that stress and constant overwork have a strong impact on women's health and can undoubtedly lead to the development of adenomyosis. To prevent the onset of the disease, a woman needs to: rest more, take relaxing baths, attend a massage, and be in a calm and comfortable environment more often.
- Keeping the body clean. Girls who ignore the rules of personal hygiene from an early age are more prone to this type of disease. And also those who engage in sexual relations in childhood and adolescence.
Taking care of your health is the main way to prevent not only adenomyosis, but also other equally dangerous diseases.
What are the indications for eliminating adenomyosis?
Indications for treatment of adenomyosis are the following factors:
- presence of signs of illness;
- inability to get pregnant;
- irregular menstrual cycle;
- frequent occurrence of painful sensations;
- decreased libido;
- changes in mood, accumulation of fatigue;
- development of depression.
All these factors may indicate that a serious malfunction has occurred in the body, and there is a high probability of illness occurring. In this case, the services of a gynecologist are needed to eliminate adenomyosis. In our clinic, treatment of adenomyosis will be fast and effective.
Symptoms
Clinical manifestations of uterine adenomyosis are practically no different from the symptoms that occur with endometriosis. The patient is concerned about:
- Pain at rest, during intimacy, during menstruation.
- Menstrual irregularities – menstruation occurs at odds with the usual dates, the amount of blood loss is twice the permissible norm.
- The presence of large clots in the secreted blood. In appearance, the fragments resemble liver.
- All signs consistent with the development of anemia. Anemia is a consequence of heavy, prolonged periods. Symptoms of anemia are decreased blood pressure, weakness, the appearance of wounds and cracks near the mouth, dizziness, and increased hair loss.
- Problems with bowel movements and urination (delayed or increased urge). They occur with extensive adenomyosis, when the hypertrophied uterus, located between the rectum and the bladder, compresses the organs.
Other symptoms of adenomyosis are hormonal imbalance and the resulting decrease in libido, irritability, sleep disturbance and other neurological symptoms.
Which doctor should treat adenomyosis: where to go
Adenomyosis is a serious illness, so you should immediately contact a specialist who will help identify the signs, conduct an effective diagnosis and find an effective method to eliminate the problem. But the question is: which doctor should I contact to make a diagnosis and get help?
A gynecologist will help you. It is he who conducts the initial examination and keeps records during diagnosis, describing in detail the patient’s condition. In most cases, it determines which method will be used to resolve the problem. If surgery is prescribed, then a surgeon is also involved.
In the medical department, our specialists will provide professional assistance in the treatment of adenomyosis and other ailments. We employ certified specialists; if a doctor has questions, he seeks advice from foreign colleagues. Maximum care and effective elimination of health problems is our main goal. Choose a specialist and make an appointment.
Locations
Internal endometriosis of the uterine body is a pathology that affects the body of the uterus, the inner part of its tubes. The disease is rarely diagnosed during a gynecological examination. To make a diagnosis, you need to perform an ultrasound with a vaginal sensor, and additionally take a blood test with the appropriate marker.
This pathology can be found in the vagina and ovaries. Due to the ability of the endometrium to extend beyond the uterus, in some cases the disease can affect the bladder and ureter. Endometriotic lesions can even be located in the intestines. The focus of pathology can be detected simultaneously in several places. Adenomyosis, which affects the uterus, is considered by experts to be one of the most serious female diseases. Localized in the organ, it often causes infertility. Despite the possible hidden form of the pathology, it requires competent treatment, which will prevent further negative consequences.
The disease can be treated in several ways. Sometimes conservative therapy is enough. In some cases, surgery cannot be avoided. A combined method may also be used.
Diagnostic measures
A comprehensive examination should be prescribed by a specialist after a woman presents with pain in the pelvic area and menstrual irregularities. Diagnostics include:
- ultrasound;
- MRI of the uterus;
- hysteroscopy;
- colposcopy;
- laparoscopy.
After an initial examination by a specialist, a woman must undergo a transvaginal ultrasound, the results of which can show the presence of pathology and its stage. Adenomyosis is examined by MRI to obtain more accurate, additional information. Only after a comprehensive examination does a specialist make a diagnosis and prescribe the necessary therapy.