Osteoarthritis of the knee joint is the deformation and destruction of cartilage tissue. The disease is chronic and degenerative, accompanied by pain of varying severity. It can lead to complete immobilization and loss of functionality. The disease develops more often in women than in men. Moreover, excess weight and venous disease are considered factors that increase the risk of arthrosis significantly. It is no coincidence that most obese women over the age of 40 suffer from such joint problems. Most older people experience arthrosis. It can be bilateral or unilateral depending on whether only one leg or both are affected. At a young age, the disease is usually caused by injuries received during sports or physical work.
Initially, changes are observed at the molecular level, and then they affect the physicochemical properties of cartilage tissue. The cartilage becomes minty, thins, becomes cracked and delaminates. All these processes can be detected by studying cartilage tissue. If the necessary treatment is not carried out, the cartilage will be completely destroyed. This will eventually lead to bone exposure.
Causes of gonarthrosis
The main reasons that can trigger the pathological process are:
- Obesity.
- Congenital pathologies of muscle and ligament development that can cause gonarthrosis in children.
- Inflammatory processes in the knee joint (for example, arthritis).
- Disorders of cellular metabolism, diseases of the nervous system.
- Injuries and other damage to cartilage pads (menisci), joint dislocations, fractures of leg bones.
- Surgical interventions to remove the meniscus or part of it.
- Sports with a high degree of load on the lower extremities, especially those inappropriate for the person’s age.
- Spasms of the thigh muscles, often due to stress and nervous shock.
- Varicose veins of the limbs, vein thrombosis.
Deforming arthrosis of the knee joints develops gradually as the functioning of the intra-articular cartilages lining the surface of the condyles of the femur and the articular surfaces of the patella and tibia is disrupted. This condition is a consequence of circulatory failure in the knee joint.
As a result, the lack of necessary nutrients for the cartilage leads to its drying out, delamination and destruction. With thinning or complete disappearance of hyaline cartilage, bone tissue becomes denser, forming compensatory growths along the periphery.
What is the essence of the disease
Osteoarthritis of the knee joint is destruction, dystrophic damage to the connective tissue of the cartilaginous cells of the femoral-knee joint. More often, women suffer from it, especially those who have crossed the 40-year mark and are overweight. The disease can be unilateral, arthrosis of the right or left knee joint, or bilateral, affecting one or both legs at once.
Without proper treatment, the disease progresses, affecting muscles, fibrous compounds (ligaments), and bones. Because of it, you can completely lose the ability to move: with the final destruction of the cartilage, the bone will be exposed.
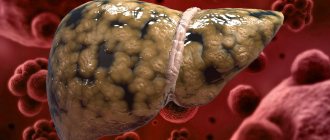
The photo shows the differences between healthy and damaged cartilage
The concepts of gonarthrosis, osteoarthritis, and deforming arthrosis are identical and are characterized by identical morphological and biological characteristics. This disease is typical for older people, but there are more and more cases when symptoms of abnormalities are diagnosed in children.
Symptoms of arthrosis of the knee joint
Clinical manifestations of gonarthrosis are very diverse and, depending on the degree of damage to the joint, can be more or less pronounced. The following symptoms can confirm that there is arthrosis of the knee joint:
- Pain syndrome. At the beginning of the disease it is practically unnoticeable, but as it progresses it intensifies. The duration of pain may vary depending on how much stress the joints were subjected to.
- Crunching in the joint during certain movements. Many people do not pay attention to this manifestation of the disease for a long time, as a result of which arthrosis develops. Without treatment, the disease progresses, leading to significant joint destruction.
- Decreased range of motion of the limb. Most often, the patient cannot fully bend the leg at the knee or straighten it. This happens for the reason that the patient tries to involuntarily minimize the pain syndrome, even in moments of its absence.
- Stiffness of movements. This phenomenon occurs because the joint is somewhat restrained by protective films that form around the nerves, which are exposed due to the destruction of the joints.
- Jamming of the knee joint in any position. With this symptom, the joint is blocked in one position and responds to all attempts to move it with acute pain. Most often, this jamming occurs due to the fact that, due to a violation of the structure of the joint, the knee ligaments extend beyond the boundaries of their normal location and spasm in this state.
- Dislocation or subluxation of the knee. This symptom occurs at a time when the disease has gone too far and the ligaments, as well as the joint capsule, do not perform their functions.
A person must clearly understand that the later he begins treatment, the more difficult it will be and the higher the risk that joint replacement surgery will be required.
Signs and symptoms
In order for the prognosis for future life to be as favorable as possible, it is important not only to know how to treat knee arthrosis, but also what symptoms the disease manifests. This is necessary for timely contact with a specialist and early detection of possible deformations and other damage to the knee joint. At the initial stage, the pathology has rather sparse symptoms, so grade 1 knee arthrosis can be detected only after hardware and instrumental diagnostics.
- The first symptoms of the disease include:
- morning stiffness in the knee;
- pain when walking when covering a distance exceeding 1-1.5 km;
- pain in the knees when sitting for long periods of time (more than 2 hours in a row);
- painful sensations in the knee joint after prolonged standing;
- knee pain that occurs at the end of the day or in the first half of the night.
If the patient does not receive the necessary treatment at this stage, the disease will progress.
To choose the right medicine for arthrosis of the knee joint, it is necessary to undergo a series of diagnostic examinations (MRI, computed tomography, radiography, etc.) and determine the degree of deformation, the level of synovial fluid in the joint cavity, the density of cartilage tissue and synovial membrane. Symptoms of grade 2 and 3 knee arthrosis are given in the table below. Differential diagnosis of arthrosis of the knee joint grades 2 and 3:
| Diagnostic sign | Arthrosis of the knee 2 degrees | Arthrosis of the knee 3 degrees |
| Pain while resting at night | May appear when changing body position or getting out of bed. | Occurs without any movement. |
| Possibility of using public transport (except for low-floor buses) | The patient experiences pain when climbing stairs, but with certain restrictions he can use public transport without assistance. | The patient cannot get on a bus or tram on his own due to limited mobility of the knee joint. |
| Lameness | Slightly expressed. | The lameness is severe and additional supports (canes) are required for movement. |
| Stiffness in the knee after waking up | Lasts less than 10-15 minutes. | Lasts about 20-30 minutes or longer. |
| Pain when walking | Occurs after passing 800-1000 m. | They begin at the beginning of the movement and intensify after traveling a distance of less than 500 m. |
| Self-care ability | Usually saved. | The patient cannot perform a number of actions without assistance. |
Osteoarthritis of the knee joint 2nd degree
The joint space narrows and the cartilage tissue is damaged to a significant extent. In the X-ray image, bone growths can be seen. Acute pain is accompanied by any movement in which the knee joint takes part. At rest, the unpleasant sensations disappear, but then appear again. The pain is accompanied by a characteristic crunching sound when performing flexion-extension movements.
Gradually, the function of the joint becomes impossible. The knee stops bending and straightening. Externally, the doctor can determine bone deformation.
What kind of physiotherapist do you need?
All physical therapists are trained through education and clinical experience to treat a variety of conditions or injuries:
- A physiotherapist who has experience treating people with knee osteoarthritis and after knee replacement surgery. Some physical therapists have practices with an orthopedic focus.
- A physical therapist who is a certified orthopedic clinical specialist. This physical therapist will have advanced knowledge, experience and skills that can be applied to the condition.
- You can find physical therapists who have these and other credentials by using MRI, an online tool to help find physical therapists with specific clinical expertise.
General tips for when to find a physical therapist (or any other health care provider):
- Get recommendations from family and friends or other health care providers;
- When making an appointment with a physical therapy clinic, you should ask about the physical therapists' experience helping people with arthritis.
During your first visit with a physical therapist, you should be prepared to describe your symptoms in as much detail as possible and report activities that worsen your symptoms.
Diagnostics
The diagnosis of gonarthrosis is based on a patient interview, examination and radiography of the affected joint. Sometimes the doctor prescribes an ultrasound of the joint to the patient; less often, a tomography or computed tomography scan of the affected knee is performed. In doubtful cases, the doctor can use a puncture to take a sample of the synovial fluid located in the joint cavity for examination, however, as a rule, this is not necessary.
Many joint diseases have very similar manifestations and symptoms to a layman. Therefore, only a specialist can understand the situation and make the correct diagnosis of arthrosis of the knee joint. Accordingly, if any signs of a knee joint disease appear, there is no need to engage in self-diagnosis and self-medication; you should consult a doctor as soon as possible. Diagnosis and treatment of arthrosis of the knee joint (gonarthrosis) is carried out by a rheumatologist or arthrologist.
Important information about the disease
Let's start this section with a description of the causes, stages, symptoms, and then delve into the treatment of arthrosis of the knee joint. Before studying treatment tactics, it is important for patients to familiarize themselves with the material below in order to have full information regarding the mechanism of origin and clinical manifestations of the pathology. Let us immediately note that arthrosis and arthritis are closely related, since the disease in question is a consequence of an arthritic disease. But where do unfortunate ailments come from that mercilessly destroy the most important bone connection? What is the severity of gonarthrosis and by what manifestations can it be recognized?
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Causes
Degenerative-dystrophic pathogenesis is “triggered” by the following provoking factors:
- previously suffered injuries - shin fractures, knee dislocations, damage to the body of the meniscus, tears and ruptures of ligaments, falls to the knees, all kinds of bruises, etc.;
- excessive physical activity;
- sedentary lifestyle;
- high body mass index;
- systemic pathologies of the rheumatoid, gouty, psoriatic type, as well as ankylosing spondylitis, systemic lupus erythematosus;
- genetically inherited weakness of the ligamentous-muscular system or congenital underdevelopment of the structural elements of the joint;
- metabolic and blood flow disorders;
- hormonal imbalance, diabetes mellitus and other endocrine pathologies;
- past or chronic infectious and inflammatory diseases.
Quite often, people themselves become responsible for the development of intractable joint disease. Often, having received an injury, they ignore contacting a specialist, preferring to make do with the first available pain medication, homemade lotions, and the like. And several years later, due to inadequate treatment carried out in the past, they come to see a doctor already with gonarthrosis, at best - of moderate severity. And here, just physical prophylaxis and pain-relieving ointments, as in the very early course, will not be enough; you often have to act radically, using surgical tactics.
There is no scientific evidence that obesity is the cause of arthrosis, but it is completely logical to assume that the greater the mass, the stronger the friction of the articular surfaces, the faster their wear.
How to treat knee arthrosis?
There is no single treatment regimen for gonarthrosis, just as there is no one medicine that would help all people equally. When planning treatment tactics, the doctor takes into account the age and condition of the patient, the stage of the disease, the severity of the pain syndrome and the degree of joint deformation.
Combination therapy is very important in conservative drug treatment, so it is necessary to combine treatment so as to solve several problems at once:
- Establish an accurate diagnosis as quickly as possible. Therapy should be started as soon as possible, this will increase the chances of prolonging the period of remission with minimal destruction of cartilage tissue.
- It is necessary to improve the nutrition of the cartilage to speed up its recovery.
- Take painkillers prescribed by your doctor.
- Increase joint mobility.
- Strengthen the muscles surrounding the damaged joint.
- Reduce the pressure on the areas of bone articulation as much as possible and strive to increase the distance between them.
- Activate blood circulation in the area of the damaged joint.
Therefore, the main methods of treating arthrosis are:
- NSAIDs are nonsteroidal anti-inflammatory drugs that are prescribed intramuscularly or intravenously. Medicines in the form of injections provide a longer-lasting and stronger pain-relieving effect. These include drugs such as diclofenac, olfen, diclac, ibuprofen, indomethacin, ketoprofen.
- Chondroprotectors. Such preparations contain substances that are part of the cartilage matrix. These medications are natural, well accepted by the body and actively stimulate collagen synthesis. The drugs justifiably used for arthrosis of the knee joint include structum, DONA, alflutop, rumalon, mucosat. All of them are slow-acting medications that need to be taken over long periods. Some of them are available in the form of injection solutions. This form of application is the most effective.
- Hormonal drugs. This group of medications is used for intra-articular injections in the presence of synovitis of the knee joint (inflammation of the synovial membrane). The goal of therapy is to relieve inflammation and pain as quickly as possible. The disadvantage of use is the damaging effect on cartilage tissue, a large number of contraindications and side effects. The most commonly used synthetic hormones for gonarthrosis are hydrocortisone, Kenalog, Diprospan.
- Trituration. To do this, you can use various kinds of gels, ointments and creams. For the most part, they are warming and anti-inflammatory. The purpose of their use is to activate local blood circulation and relieve inflammation. The most well-known drugs in this group: apizartron, finalgon, dolobene, feloran, fastum gel, nikoflex.
- Antienzyme drugs. They neutralize the synthesis of certain enzymes and prevent further joint degeneration. The most well-known drugs in this group are: contrical, ovomine, gordox. For gonarthrosis they are administered intra-articularly.
- Removing tone. Antispasmodics such as mydocalm, sirdalud, tizalud and drotaverine (no-shpa) can remove excess muscle tension in the damaged segment. It often occurs as a compensatory reaction of the body.
- Improved blood circulation. Vasodilators are used to reduce intravascular muscle tone. Such medications allow you to increase internal blood flow and improve the trophism of tissues located around the joint. For gonarthrosis, Cavinton, Trental and Actovegin are recommended. To strengthen the vascular walls, upsavit or ascorutin are used.
- Hyaluronic acid. It is a natural component of articular cartilage and synovial fluid. Therefore, its introduction into the knee joint does not cause inflammation, rejection or other negative reactions. At the same time, the use of drugs such as otrovisk, sinocorm or hyalual can soften movements and relieve pain caused by friction of articular surfaces. For gonarthrosis, the most recommended drug in this group is fermatron.
The author's methods of treating gonarthrosis include:
- Evdokimov's technique;
- Bubnovsky's technique;
- Gita Method.
They have different principles of action, but without exception, they have all proven themselves to be effective ways to support knee joints affected by gonarthrosis. Unfortunately, we are not talking about a complete recovery.
Clinical picture
In most cases, arthrosis of the knee joint manifests itself with aching, dull pain after regular physical activity. The cause of its occurrence is the irritating effect of osteophytes on nearby soft tissues, venous stagnation, intra-articular hypertension, and muscle spasm. Arthrosis is characterized by “starting” pain, which appears due to swelling of the joint or reactive synovitis. When a person sits for a long time and then stands up, some pain is felt during the first steps. So-called “blockade” pains of a periodic nature also occur. The knee joints “jam” during walking as a result of pinching of part of the damaged cartilage tissue between the two surfaces of the articulation. The following symptoms are also characteristic of arthrosis:
- crepitus, or crunching when bending or extending the knee, which occurs when bone structures are displaced relative to each other against the background of thinned cartilage;
- stiffness, the severity of which increases as the joint space fusions;
- spasms of the muscles located in the knee area, usually appearing to relieve pain;
- articulation deformation provoked by destructive changes in the subchondral bones.
With arthrosis, it is difficult for a person to climb stairs and take long walks due to constant knee pain.
The course of the pathology is very often complicated by synovitis - inflammation of the synovial membranes. Clinically, they are manifested by the formation of a round elastic seal, hyperemia, severe swelling, and an increase in body temperature to 37.1-38 °C.
In the absence of medical intervention, arthrosis is complicated by spontaneous hemarthrosis (bleeding into the cavity of the knee joint), complete or partial loss of mobility, osteonecrosis of the femoral condyle, and external subluxation of the patella.
Other treatment options for gonarthrosis
In recent years, modern methods of treating arthrosis of the knee joint have become increasingly popular, which can be used in combination with drug therapy and as independent therapy. In some cases, they can replace or be combined with medication.
New methods of treating arthrosis of the knee joint:
- kinesitherapy – treatment of a joint using a special set of exercises aimed at a therapeutic result;
- ozone therapy is a type of physiotherapeutic treatment using ozone, which is injected into the joint or applied externally;
- homeopathy;
- treatment with Tianshi drugs - the use of biologically active additives on a natural basis as treatment and prevention of disease.
Kinesitherapy can significantly prolong the activity of damaged tissues and stop the progression of the disease. This technique is based on individual selection for each patient of a set of so-called “correct” movements, which can be performed by the patient independently or using special multifunctional simulators and devices. Performing these exercises involves not only the muscles, but also helps to normalize the functions of ligaments, tendons, nerve endings, cardiovascular, respiratory, digestive and endocrine systems.
Kinesitherapy promotes the production of substances in the body such as endorphins, which can have an analgesic effect and have a beneficial effect on the patient’s psycho-emotional state. Individual exercises, affecting the muscles, allow you to:
- relieve the joint and spine;
- improve blood flow and lymphatic drainage in the affected areas of the knee joint tissue;
- restore the elasticity of the ligaments, their contractile and trophic function;
- improve nutrition and mobility of the joint as a whole;
- stimulate the processes of regeneration of cartilage and bone tissue;
- eliminate pain syndrome.
Ozone therapy, which is gaining increasing popularity in the treatment of arthrosis of the knee joint, is characterized by ease of use, high efficiency, minimal side effects and good tolerability.
Ozone therapy can be used:
- externally - the use of ozonated oils, ointments and antiseptic solutions, balneotherapy, flow aeration in special plastic chambers;
- parenterally - ozonated blood for minor and major autohemotherapy, ozone injection into biologically active points, intra-articular administration, intravenous administration of ozonated saline solution, intramuscular and subcutaneous administration.
A set of ozone therapy measures is selected individually for each patient. Parenteral administration of ozone has a more pronounced effect and has a number of therapeutic effects:
- anesthetic;
- anti-inflammatory;
- bactericidal;
- normalizing blood microcirculation;
- stimulating the restoration of joint tissue.
Glucocorticosteroid drugs and chondroprotectors can be used in parallel with ozone. This combination enhances the healing properties of these drugs and reduces their negative effects on cartilage.
To relieve pain, gas is injected into the area around the pathological focus or directly into the pain points, as well as inside the joint. The number of points for subcutaneous ozone injection may vary depending on the condition of the knee joint; From 2 to 12 ml of ozone is injected into one point.
In parallel with the intra-articular administration of ozone, patients are prescribed intravenous infusions of ozonized 0.9% sodium chloride solution (about 400 ml daily). As a rule, a course of ozone therapy consists of 10-12 intravenous injections and 5-7 intra-articular injections. After just 3-4 procedures, the patient’s mobility of the affected joint improves and pain is significantly reduced. The clinical effect of ozone therapy can last for 4-9 months.
Postoperative course
Immediately after total knee replacement surgery, the patient will be admitted to the recovery room. Most patients can be admitted to a regular ward within a few hours when sensation returns in their legs. A pain pump connected to the epidural catheter will be given to control when pain medication is given. Most people are quite comfortable with a pain pump.
On the day of surgery, you can do some exercises as directed by your physical therapist, including quadriceps contractions and moving your legs up and down. Depending on your surgeon's preference, you may begin bending your new knee immediately after surgery or on the first day of surgery. The patient will be allowed to take ice after surgery to wet their mouth, but drinking liquids or eating may cause nausea. The patient will have a catheter in the bladder so there is no need to worry about urinating. Once movement in the legs is restored, you will be allowed to sit, stand, and take a few steps with the help of a walker and a therapist.
The first day after surgery will be an active day, designed to help you become more mobile.
The patient will meet with physical therapists who will provide instruction in additional exercises. They will also help you get on your feet and take a few steps with the walker. Typically, the patient will be allowed to drink clear liquids.
It will be easier and easier to move in the next few days. The patient will be relieved of pain and urinary catheters. Treatment for pain will be given in the form of tablets. On the second day after surgery, if signs of recovery are found in the intestines, you will be allowed to eat regular food.
Depending on your age, preoperative physical condition, and insurance coverage, the patient may be a candidate for short-term placement in a rehabilitation facility. Otherwise, the patient will be discharged home and a physical therapist will come to their home to continue rehabilitation. The dispatcher will discuss these options with the patient and help them plan their return home.
Return to activity will be guided by your surgeon and physicians. Typically, patients can walk as much as they want for 6 weeks after surgery. Patients can resume movement after 6 weeks. After 8 weeks, patients can resume golfing and swimming; at 12 weeks they can play tennis. Your surgeon will help you decide what activities you can resume.
Surgery
When the functioning of the joint is clearly impaired and conservative treatment does not help, surgical intervention is used. But it comes to this extremely rarely. The affected joint can be replaced with an artificial one (endoprosthetics). But more often it is used at stage III.
The axis of the limb is restored or bone changes are removed (osteotomy). Arthroscopic intervention is performed through skin punctures. Through punctures in the knee, destroyed cartilage is removed from the joints. Then medications are administered.
Nonsteroidal anti-inflammatory drugs
They will help relieve pain and eliminate pain due to arthritis of the knee joint in a short period of time. Go to the article on this topic. During exacerbation of the disease, medications that suppress the inflammatory process are indispensable.
The following are recognized as the most effective medications for relieving pain in arthrosis: Nimesulide, Nise, Xecofam, Nurofen, Movalis, Rofecoxib, Piroxicam, Aceclofenac.
Be careful: all strong anti-inflammatory drugs have a negative effect on the gastrointestinal tract. Therefore, it is worth taking any anti-inflammatory drug under the cover of stomach-coating agents (for example, Omez, Phosphalugel, etc.). The opinion that anti-inflammatory drugs administered intramuscularly do not have a negative effect on the gastrointestinal tract is considered erroneous.
In addition to taking anti-inflammatory drugs for inflammation of the knee joint, you need to relieve the load on it. To do this, a tight bandage and reduced physical activity will be enough.
When taking non-steroidal drugs, remember that their main purpose is to relieve acute pain, and not to treat. Their mechanism of action is simply not aimed at stopping the process of destruction of joint cartilage tissue.
Gymnastics for arthrosis of the knee joint
Any treatment option for arthrosis of the knee joint should only be carried out as prescribed by a doctor. Therapeutic gymnastics involves slow, measured exercises that exclude squats, twisting of the joint, and jumping. It is best to do gymnastics in the morning, sitting or lying down, for 20 minutes, repeating each exercise 10 times.
- Lying on your back, you can perform the bicycle exercise, but you need to straighten your legs parallel to the floor, make circular movements with your feet, move your legs to the sides, alternately sliding them along the floor, strain your feet for a count of 10.
- Sitting on a chair with your legs down, straighten your legs, simultaneously bending your feet, and hold this position, counting to 10, alternately pull each knee to your stomach with your hands and slowly return to the starting position.
- Focusing on the wall, standing on the floor, alternately swing your legs back and forth.
- Putting your straightened leg on a chair, perform inclined movements of a springy nature, while leaning your hands on your thigh, as if trying to straighten your leg more.
- Lying on your stomach, alternately lift your straightened leg and hold it for up to 3 counts.
- Sitting on the floor, spread your legs to the sides, moving them along the floor, pull your knees to your stomach as you inhale and return them to their starting position as you exhale.
Video on the topic:
The main objectives of therapeutic exercises are to relax muscle spasms that cause pain, increase blood supply to the joint, slow down the progression of the disease, and prevent further destruction of cartilage. During the period of exacerbation of the disease, physical exercise is prohibited.
A blow to the disease: intra-articular injections
Chronic arthrosis with periodic exacerbation is best not treated with corticosteroid injections (Medrol, Prednisolone, Kenalog), oxygen therapy (enrichment of joints with oxygen cells) and injections of hyaluronic acid, but only during a period of stable remission.
Injections into the joint are recommended no more than once every 2 weeks.
When resorting to injections, remember the following important rules:
- They contain hormones, so it is advisable to use them for joint swelling.
- It is strictly unacceptable to inject them without a history of symptoms of synovitis.
- They have a large number of side effects. For example, consuming them in large quantities without justifiable reasons leads to increased bone resorption.
- Corticosteroid injections are allowed only once every 2 weeks. Otherwise, the risk of joint injury, infection, ligament or muscle damage increases.
- Administration of the drug for prophylactic purposes is strictly prohibited.
How to treat arthrosis with massage?
Using the method of blows (through the palm, fingers, slaps) at home, you can work on a sore knee joint. It is important to know how certain movements affect the deforming joint:
- Massage in the form of spanking affects the nerve endings and promotes better blood circulation in the sore joint.
- Thanks to the blows through the pressed fingers, there is a positive effect on the tendons, muscles and all joint components. Due to the fact that the blows are softened, circulatory activity occurs without damaging the capillaries.
- The palm is pressed against the joint, and the blows are applied to the periarticular areas. Thus, the functionality of the internal parts of the joint increases.
- Initially, fingers lightly and carefully tap on the sore joint. As the condition improves, the force of the blows increases slightly. This procedure is accompanied by tolerable pain.
Treatment prognosis and prevention
It seems feasible to completely get rid of arthrosis if signs of the disease are found at stages I-II. When deforming processes are observed in the joint, and the patient constantly feels pain, motor activity is reduced to a minimum, then prosthetics will help restore maximum functions. But there will be no complete recovery.
Those who take up the treatment of a knee joint affected by arthrosis on their own should not hope for a successful fight against the disease. Without an accurate diagnosis, you can treat another disease without suspecting that you have arthrosis. This is fraught with serious consequences.
Among the positive aspects of treating knee arthrosis at home, it is worth highlighting the moral support of relatives. A good mood and a psychologically healthy background contribute to successful resistance to the disease.
The following measures are used to prevent arthrosis:
- moderate loads on the knee joints;
- morning exercises;
- going to the pool at least 2 times a week;
- eliminating problems associated with excess weight;
- for knee injuries, treatment until complete recovery;
- walking in the fresh air;
- balance in the diet.
Prevention will help, if not to avoid the disease, then to push its development as far into the future as possible. Arthrosis is a disease that requires a lot of attention and timely treatment over a long period of time.
Diet
Complex treatment of this disease includes, in addition to the methods described above, also a strict diet. It requires an adequate approach. There is no need to go to extremes. But there are a number of restrictions that will have to be taken into account:
- Various pickles and fermented foods also need to be minimized.
- Remove animal fats from your diet.
- Avoid bread and rolls (you can eat brown bread, but in moderation), as well as chocolate and sugar. People with osteoarthritis do not need carbohydrates. Their use has an impact on weight gain. And this is a risk factor.
- At least exclude fatty meats. Avoid eating duck, goose, lamb, and pork.
- Limit salt intake. It’s not for nothing that arthrosis is also called “salt arthrosis.” Doctors advise only adding a little salt to dishes before eating and not during cooking.
- Minimize the use of spices, especially hot ones. They contribute to the feeling of thirst and whet the appetite.
- Alcoholic drinks and smoking are strictly prohibited. At least during therapy.
Sample menu:
- Breakfast: oatmeal with water without butter or sugar, fruit juice, boiled egg
- Second breakfast: a glass of low-fat natural yogurt
- Lunch: steamed meat or fish, stewed vegetables, tea without sugar
- Afternoon snack: cottage cheese casserole with nuts, glass of fruit juice
- Dinner: vegetable salad, apple, tea without sugar
- Second dinner: a glass of low-fat kefir
A dietitian will help you balance your diet. For example, here are a number of foods that you can eat, and this is even welcome with such a diagnosis. First of all, these are products containing chondoprotectors and collagen; they are the building blocks for bones, cartilage, and ligaments. Your diet should include broth made from beef, especially bones. The presence of jelly, aspic, and jellied meat in the menu is welcome.
Symptoms
Individuals who develop knee OA may experience a wide range of symptoms and limitations based on the progression of the disease. Pain occurs when the cartilage covering the bones of the knee joint wears away. Areas where cartilage wears or becomes damaged exposes the underlying bone. The impact of the bone allows for increased stress and compression of the cartilage and sometimes bone contact during movement, which can cause pain. Because the knee is a weight-bearing joint, the level of activity and the type and duration of activities tend to have a direct impact on symptoms. Symptoms may worsen with weight-bearing activity, such as walking with a heavy object.
Knee symptoms may include:
- Worsening of pain during or after surgery, especially when walking, climbing, descending stairs, or moving from a sitting to a standing position.
- Pain or stiffness after sitting with a bent or straight knee for an extended period of time. Pain is the most common symptom of osteoarthritis. As the disease progresses and inflammation occurs, the pain may become constant.
- Feeling of popping, cracking, or grinding when moving the knee.
- Swelling after action.
- Stiffness in the affected joint is often noticed first thing in the morning and after rest.
- Swelling, which is sometimes warm to the touch, may be noticeable in an arthritic joint.
- Deformity can occur with osteoarthritis due to bone growth and cartilage loss. Bone growths at the end joints of the fingers are called Heberden's nodes. Bouchard's nodes are bone growths in the middle joints of the fingers. Degeneration of the knee joint cartilage can lead to outward curvature of the knees (bow-toe).
- A cracking sound or grating sensation may be noticed when moving the arthritic joint. It is caused by bone rubbing against bony or rough cartilage.
Typically, these symptoms do not occur suddenly and all at once, but gradually develop over time. Sometimes people don't recognize that they have osteoarthritis because they can't remember a specific time or injury that caused their symptoms. If your knee pain has gotten worse over several months and does not respond to rest or changes in activity, it is best to seek advice from a healthcare professional.
Compresses
In the initial stages of arthrosis of the knee joint, homeopathy has proven itself to be effective.
It is recommended to use compresses for arthrosis of the knee joint only in special cases:
- in the presence of edema and fluid accumulation;
- to improve joint mobility (in chronic form).
Compresses made from “Bishofite”, “Dimexide” and “Medical Bile” help relieve pain, swelling and inflammation most effectively.
Compresses will be much more effective than anti-inflammatory or warming ointments, due to their ability to penetrate into tissues. It is strictly forbidden to use medical bile in the presence of pustular skin rashes. Often, instead of saline solution, Novocaine is used together with Dimexide or Bischofite, which has not only a resolving and anti-inflammatory effect, but also pain relief. Very often, both drugs improve metabolism in joint tissues.
It is worth considering that during an exacerbation of the disease, it is undesirable to make compresses, since they only “warm up” the inflammation process.
The effectiveness of the compress directly depends on whether it was prepared correctly. To prepare compresses, you need to mix a one to four solution of Dimexide or Bischofite with saline. Soak a sterile bandage or gauze in the resulting mixture and apply to the site of inflammation. Cover the compress with cotton wool and secure with cling film. It is recommended to carry out the procedure once a day for 20-30 minutes for about two weeks.
Don't miss: Treating ligamentitis of the knee joint and patellar ligament
Please remember to take special precautions:
- You cannot prepare a compress in advance, because due to a chemical reaction with saline solution, the active substance loses its properties;
- For the compress, only sterile materials should be used, since the main active substance penetrates deep into the layers of the dermis, attracting with it all the elements dissolved in it. Therefore, in order not to provoke an allergic reaction, use only sterile materials.
- to prevent chemical burns, apply the drug “Dimexide” or “Bishofite” for no more than 20-30 minutes;
- for acute pain in the knee joint, replace the saline solution with Novocain. The drug will have an analgesic effect on the joint.
Chondroprotectors
Chondroprotectors - strong and effective drugs
Unlike anti-inflammatory drugs, which can only fight the symptoms of the disease, representatives of this group are used to directly treat the disease. They significantly reduce the manifestations of gonarthrosis, allowing you to restore joint function, remove excess fluid and heal damaged tissue.
Chondroprotectors are considered relatively safe because they are free of serious side effects.
Therefore, they are often called the best drugs for arthrosis of the knee joint. However, they should only be taken after consulting a doctor. Drugs in this group represent the basis for the treatment of arthrosis.
The principle of action of such drugs is based on the activation of restoration processes in the body. These drugs allow you to achieve the following effects:
- Improving blood circulation in the affected joint. This allows for the transport of nutrients to damaged tissues and accelerates their healing. Also, decay products and pathogenic microflora that destroy joints are removed with the blood.
- Normalization of joint fluid production. With a lack of this substance, the abrasion of the joint increases, as a result of which it becomes unusable, and the person becomes disabled.
- The lubricating effect of the joint fluid returns to normal. The load on the joint tissue is reduced, and it begins to function normally.
When treating arthrosis with chondroprotectors, it is necessary to take into account the following features of these drugs:
- You should not count on a quick effect. Drugs in this group have a slow action. The first results will appear only after 3-4 months. Therefore, the standard course of treatment with chondroprotectors is about a year. In some cases, taking drugs from this group extends up to two years. Therefore, if you want to get a truly effective medicine for arthrosis of the knee joints, you will have to be patient.
- The effectiveness of these medications is limited. Chondroprotectors will do their job perfectly if the disease is at stage 1-2. If arthrosis is advanced, then there will be no point in taking these medications. This is explained by the fact that if the cartilage tissue is significantly destroyed, there will simply be nothing left to restore.
- There are two types of chondroprotectors: glucosamine and chondroitin sulfate. And there is no consensus among specialists regarding their use. While some doctors advise taking them in combination, others argue that these drugs weaken each other’s actions.
Indications and contraindications for the use of drugs
There are a number of indications for the use of tablets for arthrosis:
- relieving inflammation;
- reduction of swelling;
- restoration of motor activity due to the restoration of cartilage tissue;
- reduction or removal of pain;
- strengthening metabolic processes and blood circulation.
As a rule, several courses of drugs are used to enhance and consolidate the effect. For each individual group of drugs, there are a number of contraindications and restrictions on use.
The general list of contraindications looks like this:
- diseases of the cardiovascular system;
- endocrine disorders;
- oncological diseases;
- pregnancy and lactation (limited drugs);
- children's age (limited drugs);
- individual intolerance to components;
- mental disorders.
Basic precautions for use:
- timely reception;
- correct dosage;
- selection of drugs from different groups, taking into account possible cross-reactions.
When taking, you should take into account possible allergic reactions. If they occur, you must again seek help from a doctor to prescribe other medications.
What is arthrosis?
Arthrosis is a degenerative-dystrophic disease of the joints that occurs as a result of damage to the cartilage tissue of the articular surfaces. An entire section of our website is dedicated to this disease. The development of the disease can occur in any joint: knee, hip (coxarthrosis), shoulder joint, hands and feet. Causes of the disease:
This is what healthy joints and joints affected by arthrosis look like
- Diseases or injuries of the joints.
- Disorders of metabolic processes.
- Nutritional errors, excess weight.
- Excessive physical activity.
- Chronic infection with frequent relapses.
- Long-term arthritis.
- Hormonal disorders in women during menopause.
- Congenital joint dysplasia.
Symptoms indicate the need for treatment:
- Soreness and cracking of the joints.
- The disappearance of pain when a person “disperses” and an increase in intensity after sleep and rest.
- Stiffness in movements.
- Limited range of motion of the limbs.
Nutrition
Calcium salts enter the human body with the wrong foods and unfiltered water. A balanced diet stimulates the cleansing of the body from harmful deposits and stops bone deformation. The diet is also recommended for overweight patients. Extra pounds are an additional burden on sore knees.
Nutrition for arthrosis performs two functions: restores cartilage tissue and normalizes body weight. A person will have to adhere to several rules:
- Eat low-calorie foods.
- Never skip breakfast.
- Have a snack if you feel hungry.
- Divide food into small portions.
- Products are not fried. Just boil, bake and steam.
- Strict diets and therapeutic fasting are prohibited.
- Don't go to bed with a full stomach.
- Eat food 4 to 7 times a day.
- Drink water, jelly and decoctions.
The main goal of a diet for arthrosis is to normalize weight. Pork and beef can be consumed twice a week. Cutlets, meatballs and other meat dishes are prepared from chicken breast or turkey; rabbit is also suitable. Sausages, lard, ham and smoked meats are prohibited, as are butter and sour cream.
You need to prepare poultry jelly or jelly weekly. Use legs, wings, breast. The meat is cleaned of fat and skin to reduce its calorie content. A little gelatin is added to the dish. The additive is classified as a chondroprotector. The substances trigger the renewal of cartilage tissue and stop bone deformation.
Joint function improves thanks to fatty fish: mackerel, salmon and trout. Seafood is prepared twice a week. Calcium sources that are useful for a patient with arthrosis are:
- lettuce leaves;
- parsley root and stems;
- cottage cheese;
- yoghurts without sweeteners and flavors;
- fermented baked milk;
- dill;
- kefir;
- milk serum.
Bone deformation is stopped by foods containing B vitamins. These include black and grain bread, egg yolk, seafood and peas, hard cheese, bananas and baked potatoes.
The body needs tocopherol. Vitamin E removes inflammation, increases the elasticity of cartilage tissue and joint mobility. The disease is slowed down by sprouted wheat, walnuts and pine nuts, hazelnuts and flaxseed oil.
A patient with knee arthrosis is recommended to include fresh fruits and vegetables in his diet. Allowed to use:
- zucchini;
- pineapples;
- carrots and Chinese cabbage;
- broccoli, pumpkin and apples;
- grenades;
- lentils, beans;
- raspberries, black and red currants.
Metabolic processes in the body are restored with porridge. Only polished rice and semolina are prohibited. Vegetable oils are useful, but more than 1 tbsp. l. in a day. It is recommended to drink a decoction of rose hips, raspberry twigs and leaves, as well as green tea.
Cartilage tissue is restored with desserts made from cottage cheese and dried fruits, seasoned with yogurt. Only gelatin must be added to the dish.
If you have arthrosis and are overweight, you should avoid processed foods, marinades, white cabbage, chips and crackers, buns and cakes. Marshmallows and halva, canned meat and fish, pates, and offal dishes are contraindicated.
You should not get carried away with hot spices: mustard, paprika, black pepper and chili. The amount of salt is reduced to 5 g per day. Seasoning is added to dishes after cooking, not during.
how to get rid of crunchy knees
Hyaluronic acid
Hyaluronic acid has a beneficial effect on the surface of the joint, forming a protective film on it. Preparations based on hyaluronic acid are prescribed by a doctor to a patient for acute deficiency of synovial fluid.
In this case, the hyaluronic acid will act as a lubricant for the knee joint. Injections with hyaluronic acid significantly increase the firmness and elasticity of the joint. It has virtually no contraindications - it all depends on the individual’s tolerance to the drug. Injections with hyaluronic acid should be carried out as a course of treatment: once every six months, only 3 - 4 injections with a short interval (1 - 2 weeks).
It is used together with Ostenil, Sinvix, Duralan and other drugs. Its main drawback is the price, which is completely justified by its effectiveness. Among the cheap analogues of hyaluronic acid is the drug "Giastat", the price of which is 30-40% lower than imported analogues.
Don't miss: What is prepatellar bursitis of the knee and how is it treated?
Injections of hyaluronic acid in case of synovitis and acute inflammatory processes are strictly prohibited, since in these cases it turns out to be completely useless and can harm the joints. It is best to inject acid during a period of stable remission.
Oxygen therapy allows you to normalize the metabolism of nutrients in the joint and achieve stable remission. The essence of this treatment is that ozone irradiated by a laser beam is injected into the joint. Oxygen therapy is quite effective in the early stages of knee arthrosis.
Injections are carried out in a course - no more than four times with an interval of two days.
FIND OUT MORE:
How to eat with arthrosis: the best advice from foreign orthopedists and nutritionists
Training on an exercise bike for the treatment of arthrosis of the knee and hip joint
Deforming arthrosis of the knee joint: etiology, clinical picture, diagnosis and treatment
Treatment of deforming arthrosis of the hip joint grades 1, 2 and 3
Diet for arthrosis
Intra-articular injections of corticosteroids for gonarthrosis
Burdock, honey and juices
Arthrosis begins with poor circulation in small vessels located next to the knee cartilage. For pain and destruction of bone tissue, massage is recommended. One of the most common is honey.
The muscles and cartilage tissue are heated with salt or a heating pad for 10 minutes. Apply a little liquid honey to the skin and rub in the bee product using stroking and patting movements. The procedure lasts 20 minutes. The remains of the sweet product are washed off with warm water, and a compress is applied to the sore knee.
Blood circulation in the cartilage is restored with burdock leaves. Take 5-7 fresh specimens, stack them and place a kettle of hot water on top. The skin is treated with vegetable oil, for example, sunflower or olive. Badger or bear fat will also work. Warm leaves are applied to the sore leg, wrapped in cling film and an elastic bandage. Cover with a woolen scarf.
Instead of heating the burdock, you can wash and mash it. When the juice comes out, apply triple cologne to the fluffy side. Apply to the deformed joint and secure with a plastic bag, with a warm scarf on top. On the second day, the leaf is smeared with honey and then cologne. On the third day, the bee product is replaced with garlic pulp. On the fourth day, use Vishnevsky ointment instead of honey and cologne. Compresses are alternated for 2 months. Break – 4–6 weeks. Burdock leaves restore mobility to joints, reduce swelling and discomfort.
Arthrosis is treated with tincture of black radish, cranberries and beets. 500 g of berries and root vegetables are passed through a meat grinder and the mixture is poured into a bottle. Pour 0.5 liters of cognac and leave in a closed container for 10 days. The medicine is taken in the morning before breakfast. Take 30 ml of liquid. The break between courses is 2–3 months.
Severe pain and swelling of the knee can be relieved with celery. The whole plant, along with the stems and roots, is washed and crushed. Squeeze the juice out of the mass and store it in a glass jar. Drink 60 ml three times a day. Food is consumed after 40 minutes. The cake is applied to the knee overnight. Before the procedure, the skin is moisturized with vegetable oil.
A medicine for arthrosis is prepared from celery root. The workpiece is cleaned, washed, and crushed. Measure out 1 kg of mass and mix with 1 liter of vodka. The jar with the preparation is placed in a dark place for 10 days. The strained celery product is stored in a bottle. The cake is left in the jar and 1 liter of water is added. The resulting water infusion is mixed in equal proportions with vodka. Drink 60 ml of medication half an hour before eating. The course lasts from 5 to 6 months. Celery infusion stops the destruction of cartilage tissue and relieves pain.
how to get rid of knee pain
Efficacy and principles of drug treatment
Drug treatment is based on the principle of increasing the duration of remission and reducing the exacerbation phase.
A correctly selected regimen allows you to quickly achieve a shift in balance towards restoration and reduce inflammatory processes. To begin with, the patient is removed from the state of acute inflammation of the joints and the pain syndrome is relieved using analgesics and non-steroidal drugs, then the disease is managed comprehensively.
For positive dynamics of drug therapy, it is necessary to follow the principles of treatment:
- Stimulating blood supply to the joints.
- Increased blood flow.
- Restoration of tissue innervation.
- Operational load reduction.
Each group of drugs has its own application characteristics. General principles of treatment:
- Long course of treatment (with periodic breaks).
- If there is no effect after the first course, change the drug.
- The regimen is prescribed individually (dose, time and method of administration).
- Control of general tests and x-ray control at least once every six months.
- For concomitant diseases, the dose is set individually.
Only the attending physician can draw up a medication treatment regimen and prescribe pills and medications after conducting instrumental and laboratory diagnostics and making a diagnosis.
Effective drugs
After consultation with a specialist, it is necessary to purchase medications for painful gonarthrosis. The cost of drugs varies depending on the manufacturer, the quality of the substances in the composition, and the pharmacy. There are products both at a high price and their inexpensive analogues, differing only in name. Let's consider the best effective non-steroidal anti-inflammatory drugs and chondroprotectors.
Diclofenac
- Ingredients: active ingredient – diclofenac sodium + excipients.
- Indications: helps with inflammatory, degenerative pathological changes in the musculoskeletal system. The drug is effective for arthrosis and arthritis. It has a pronounced anti-inflammatory effect, produces an analgesic effect, and relieves fever.
- Application: dosage is prescribed individually depending on the course of the disease. For adults, 25-50 mg of the drug is prescribed when taken orally 2-3 times a day.
- Price: 40-100 rubles.
Artra
- Ingredients: chondroitin sulfate + glucosamine hydrochloride.
- Indications: the medicine is an indispensable tool in the fight against gonarthrosis; it is prescribed for osteochondrosis of the spine and other diseases associated with dysfunction of cartilage tissue. Available in tablets.
- Application: in tablets of 250 milligrams - 2 pieces 2 times a day, 500 mg - 1 twice a day, 750 mg - 1-2 pieces.
- Price: 670-1600 rubles.
Don
- Ingredients: glucosamine sulfate + excipients.
- Indications: helps in the treatment of gonarthrosis and other diseases of cartilage tissue. The active substance of the medicine restores normal metabolic work in the cartilage, promotes its better nutrition and good “lubrication”. Reduces pain by inhibiting degenerative processes.
- Application: powder (in a sachet) - one packet once a day for one and a half months, injections - 1 ampoule 3 times a week.
- Price: 1100-1200 rubles.
Elbona
- Ingredients: glucosamine + auxiliary elements.
- Indications: for negative processes in cartilage tissue. The medicine helps to cope with arthrosis of the knee joint, producing an anti-inflammatory and analgesic effect. Stimulates restoration processes in cartilage tissues.
- Application: the drug is administered intramuscularly. Two milliliters of Elbona with a solvent are used, administered once a day three times a week. Course duration is 1-1.5 months.
- Price: 1200-1400 rubles.
Structum
- Ingredients: sodium chondroitin + sodium salt.
- Indications: this chondroprotective medicine helps the patient to quickly cope with arthrosis of the knee joint, restoring cartilage tissue and improving its nutrition. Has an antioxidant effect and helps cope with inflammation.
- Application: the drug is used in capsules, the recommended dose is 1000 milligrams.
- Price: 1400-1500 rubles.
Teraflex
- Ingredients: chondroitin sodium + glucosamine hydrochloride.
- Indications: a combined medicine that helps slow down the destructive processes affecting human cartilage tissue, which helps to more quickly treat arthrosis of the knee joint. Reduces discomfort, relieves inflammation.
- Application: for the first 20 days, 1 tablet 3 times a day, then two. The course lasts 2-3 months.
- Price: 1000-1500 rubles.
Chondrolone
- Ingredients: chondroitin sulfate + auxiliary elements.
- Indications: the medicine is indicated for people suffering from arthrosis of the knee joint of the first and second degree. The drug helps get rid of inflammation, pain, promotes restoration processes that return cartilage tissue to health, and improves metabolic processes.
- Application: every other day, 1 ampoule of the drug intramuscularly.
- Price: 1200-1300 rubles.
Chondroxide
- Ingredients: chondroitin sulfate + excipients.
- Indications: the medicine promotes the regeneration of damaged tissues, helps cope with inflammation, and reduces pain symptoms. Improves metabolic processes occurring inside fibrous and hyaline cartilage.
- Application: 2 tablets (0.5 grams) 2 times a day.
- Price: 300-500 rubles.
Chondroitin AKOS
- Ingredients: chondroitin sulfate sodium + auxiliary elements.
- Indications: used for osteochondrosis, cartilage damage, arthrosis of the knee joint. Helps reduce inflammation, relieve severe pain, improves metabolism occurring in cartilage tissues. Stops degenerative processes.
- Application: 1000 mg per day (2 tablets 2 times per day).
- Price: 60-300 rubles.
General Treatment Approaches
In the treatment of arthrosis, a complex of drugs and procedures is used
As mentioned above, arthrosis therapy should involve an integrated approach. Competent treatment should include the following procedures:
- Taking medications. Modern medications can reduce swelling and pain, and also effectively combat inflammatory processes.
- Physiotherapeutic procedures. These techniques allow you to achieve greater effect from taking medications, reduce pain and improve the mobility of the affected joints.
- Folk remedies. Used as auxiliary procedures. Doctors often prescribe baths, compresses and rubbing to their patients to reduce discomfort and increase the effectiveness of treatment.
- Diet. Proper nutrition is the key to recovery from arthrosis. Without eliminating harmful foods and including vitamin-rich foods in the diet, it is impossible to achieve truly high treatment results.
Thus, in addition to taking medications, the patient receives from a specialist a number of recommendations that he must follow impeccably. The course of treatment in each specific case is purely individual.
Surgical treatment of arthrosis
With the help of surgical intervention, you can not only eliminate the painful symptoms of a deformed knee, but also influence the cause that caused the development of the pathology. There are 4 different operations to get rid of arthrosis:
- Puncture. The therapeutic procedure allows you to quickly eliminate excess joint fluid, relieve the inflammatory process and restore mobility to the joint.
- Arthroscopy. The modern method is used for stage 2 arthrosis. The purpose of the operation is to eliminate the remnants of destroyed cartilage tissue. The intervention is carried out using the endoscopic method using thin surgical instruments and a microcamera inserted into the joint.
- Periarticular osteotomy. The operation involves sawing the patient's bone and fixing it at a different angle to redistribute the load. The method is recommended for diagnosed arthrosis of degrees 1 and 2.
- Endoprosthetics. A complex operation prescribed to patients if grade 3 gonarthrosis is diagnosed. During the operation, a prosthesis that simulates the knee joint is installed.
With the help of a prosthesis, it is possible to restore the patient’s motor functions, but such an operation requires a long rehabilitation period.
Folk remedies
Traditional medicine combined with traditional medicine gives excellent results. A separate article https://revmatolog.net/artroz/lechenie-kolennogo-sustava-narodnymi-sredstvami is devoted to treatment with folk remedies.
Rubs and baths
Rubbing is a mixture of medicinal solutions that is rubbed into the skin in the affected area. The purpose is to improve blood flow, helping to warm up the sore spot and distract the patient from pain. It is recommended to use this method in combination with a sauna or hot bath. First you need to warm up the body with hot water or a steam room in a bathhouse, and then apply a mixture of medicinal solutions to the sore area.
Infusions and decoctions
Infusions and decoctions will help relieve pain and improve the patient’s condition in the initial stages of gonarthrosis. To relieve symptoms, the following folk remedies are used: black bean herb tea, infusion of lemon, garlic and nettle, and decoction of beef hooves.
Compresses
You can make compresses based on natural ingredients yourself. They are performed in the same way as wrapping with ointments and solutions. You can use natural honey, clay, camphor oil, and young dandelion leaves as a basis. This compress can be left overnight.
There are three degrees of the disease
- Arthrosis of the 1st degree is the mildest of them. It begins gradually, very slowly, so it is difficult to name the time when the first signs appear. The changes in cartilage are minor and manifest as pain when walking up stairs. Sometimes the joint begins to ache constantly and swells a little, but everything goes away on its own and usually does not attract much attention.
- Arthrosis of the 2nd degree is manifested by an increase in the intensity and duration of pain, you have to take medications to get rid of it. Inflammation has already set in, so morning stiffness occurs and the joint increases in size. Some people notice a crunching sound when moving.
- Arthrosis of the 3rd degree is accompanied by the maximum severity of all symptoms. The pain bothers me not only when walking, but also at rest. The joint is enlarged, deformed, range of motion is narrowed.