The abdominal cavity contains a number of vital organs, so if you are suffering from abdominal pain, this is an alarming signal.
The syndrome can affect not only the organs located in the abdomen, but also the systems adjacent to this area. The article will discuss a symptom that is leading in most clinics specializing in lesions of the abdominal cavity. If you are experiencing acute abdominal pain, this is a reason to consult a doctor without the slightest delay.
Etiology
The following signs accompany pain attacks in the abdomen are identified:
- Smooth muscle spasm. Affects the excretory ducts and hollow organs (stomach, esophagus, gall bladder, intestines, pancreatic duct and urinary tract).
- Wall stretching. Inherent in hollow organs located in the abdomen. Accompanied by simultaneous tension of the ligamentous apparatus.
- Circulatory disorders. Ischemic and congestive dysfunction of the blood vessels of the abdomen. These include stenosis of the branches of the abdominal aorta, spasm, embolism of mesenteric vessels, thrombosis, microcirculation disorders and other pathologies.
- Structural organ damage (tumor growth, inflammation, ulceration, necrosis).
- Penetration, perforation and peritoneal pain.
Classification
The presence of abdominal pain requires in-depth diagnosis and subsequent treatment. The classification system for the mentioned syndrome is quite complex.
Pathogenetic classification
- Spasmodic pain. Colloquially known as colic. The cause is a spasm of smooth muscles. They arise from organic abdominal pathologies (renal, gastric, liver, pancreatic), functional ailments (irritable bowel syndrome) and poisoning. Spastic pains flare up unexpectedly and can stop just as suddenly. The syndrome can be alleviated with antispastic drugs and heat. Concomitant symptoms sometimes include flatulence, vomiting, cardiac arrhythmia, and problems with coronary circulation.
- Pain associated with stretching of hollow organs. There is no clear localization, the character is pulling and cutting.
- A syndrome caused by problems of local circulation. There are two types: angiospastic (attacks) and stenotic (proceed slowly, but can become increasingly severe).
- Peritoneal pain. They are characterized by suddenness, duration and gradual subsidence. The localization is clear, the doctor can identify it through palpation. Mechanical impact (movement, coughing, palpation) may increase the degree of pain.
- Reflected syndrome. Abdominal pain that flares up in the digestive organs can radiate to the stomach.
Mechanism of occurrence
- Visceral syndrome. It is greatly facilitated by pathological processes occurring in the internal organs. The starting point can be, say, an increase in pressure in the cavity of the organ, as well as tension, stretching and vascular disorders in the abdomen.
- Somatic pain. They occur if the abdominal wall and the peritoneum itself are involved in the pathological process. They are clearly localized and acute in nature. It gets worse when coughing and moving.
- Referred pain. With visceral syndrome (passage of a stone), the impulse can radiate to the abdomen. The syndrome may also be based on an anatomical cause (strangulation of the intestine). Sometimes the pain radiates to the back, shoulder or right shoulder blade.
- Psychogenic syndrome. If there are no somatic and visceral causes, the triggering factor may be psychogenic. Depression plays a key role here. Abdominal pain is associated with depression through complex biochemical processes. The main features: monotony, duration and diffuse qualities. At the same time, pain may be felt in the back, head and throughout the body.
Localization
Depending on the damage to a particular organ, different parts of the abdomen may hurt.
- Right hypochondrium. Signals about ailments in the gall bladder, liver, duodenum, biliary tract, pleura, right lung, head of the pancreas.
- Left hypochondrium. Problems in the stomach, spleen, pancreas, ureter, left kidney, pleura and left lung.
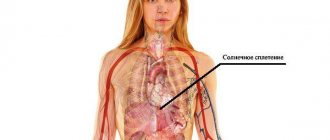
- Epigastrium. The disease is rooted in the bile ducts, liver, pancreas, lower esophagus, stomach, chest, celiac plexus.
- Right iliac region. The pathology crept into the ileum (terminal section), appendix, ureter, right kidney, right appendages of the uterus (in women).
- Left iliac region. The problem is in the colon, ureter, left kidney and left uterine appendages.
- Periumbilical part. The colon or small intestine (transverse), appendix, abdominal vessels or pancreas are affected.
- Groin and pubis. The violations affected the female genital organs, bladder, and rectum.
Etiological classification
This classification includes the main symptoms of abdominal pain.
Intra-abdominal causes
- inflammation of organs (cholecystitis, appendicitis, peptic ulcer, etc.);
- generalized peritonitis (primary and secondary);
- obstruction of a hollow organ (biliary, intestinal, urinary tract, aorta, uterine);
- ischemic disorders (organ torsion, intestinal infarction, etc.);
- others (retroperitoneal tumors, drug withdrawal, hysteria, hemolytic anemia).
Extra-abdominal causes
They mean radiating pain not in the abdomen - formed by pathologies of other organs. These include:
- pathologies of the thoracic cavity organs (myocardial ischemia, pneumonia, pneumothorax, diseases of the esophagus, pleurisy);
- neurogenic diseases (syphilis, spinal diseases, polyneuritis);
- exposure to toxins (poisons, insect bites);
- metabolic disorders (diabetes mellitus, for example).
"Non-surgical" reasons
It also happens that abdominal syndrome is of a non-surgical nature. The reasons lie in the area of the following systems:
- cardiovascular;
- respiratory organs;
- digestive organs;
- urogenital;
- hematopoietic;
- diseases of the musculoskeletal system;
- infectious diseases;
- endocrine and metabolic disorders.
Development speed
Depending on the progression, the syndrome in question is divided into:
- acute form;
- chronic form.
Causes of pain
Main causes of pain:
- Extra-abdominal. For myocardial infarction, pleurisy, pneumonia, anemia, endocrine and hormonal disorders, as well as osteochondrosis. Most of these painful sensations are referred.
- Intra-abdominal. These sensations indicate that an inflammatory process is occurring in the human body, spastic sensations, stretching, and problems with blood circulation are observed. Such sensations also occur with growths in the peritoneal cavity. Visceral pain may be due to stomach disease.
The causes of unpleasant sensations can be pathological or non-pathological processes.
Non-pathological include:
- Wrong diet. For example, there are too many spicy foods and carbohydrates in the diet.
- Taking medications. Some tablets have a negative effect on gastrointestinal motility and mucous membranes.
- Menstruation. Systematic pain is caused by temporary endometrial ischemia and myometrial spasm.
- Unpleasant sensations in the stomach in children. Up to a year, the sensations are due to the immaturity of the digestive system. Up to 3 years of age, processes of a psychological nature or pathology develop due to errors in the diet.
- Pain during pregnancy. Caused by sprained ligaments, divergence of the symphysis pubis, joint surfaces, or tension of the skin.
Pathological factors:
Dangerous symptoms
What symptoms are the most dangerous for abdominal pain? Let us briefly list the signs hinting at emergency surgery:
- tachycardia;
- arterial hypotension;
- weakness;
- apathy;
- dizziness;
- fever;
- visible bleeding;
- repeated vomiting;
- absence of peristaltic noise and gas discharge;
- increase in abdominal volume;
- muscle tension in the abdominal wall;
- increased pain syndrome;
- fainting during bowel movements;
- Shchetkin-Blumberg symptom (positive).
Diagnostics
For abdominal pain, the following types of diagnostics are recommended:
- Pregnancy test (biochemical) for women.
- Analysis of urine. Will help identify pyelonephritis, genitourinary tract infection, urolithiasis.
- Blood analysis. In case of inflammation (diverticulitis, appendicitis), leukocytosis is observed in the blood, but conventional analysis is not able to detect it.
- Liver function tests. Along with lipase and amylase studies, they may indicate pathologies of the gallbladder, liver, and pancreas.
- Ultrasound of the abdomen. It is done if there is a suspicion of an abdominal aortic aneurysm, lesions of the biliary tract, ascites or ectopic pregnancy.
- CT. This type of research is aimed at the abdominal organs and, in the presence of pain, allows identifying abdominal aortic aneurysm, nephrolithiasis, diverticulitis, mesenteric ischemia, appendicitis, and intestinal obstruction.
- Radiography. A survey examination of the abdominal area designed to diagnose two ailments - intestinal obstruction and perforation of a hollow organ.
- ECG. Required to exclude myocardial ischemia.
How to deal with abdominal ischemic syndrome
The pain usually appears about half an hour to an hour after eating and can last up to four hours. Sometimes it radiates to the back or to the left side of the chest and is accompanied by flatulence, belching, nausea, vomiting, regardless of the quality of food taken.
It can be provoked not only by food, but also by physical stress or fast walking, and the pain is relieved at rest on its own, although sometimes this requires additional nitroglycerin or (in case of increased intensity) analgesics.
When diagnosed with “abdominal ischemic syndrome,” treatment, as in other cases, is aimed at the underlying disease. The patient is prescribed antispasmodics, drugs that improve blood circulation, anticoagulants, and in the case of intestinal dysbiosis, drugs that improve its microflora.
Patients are usually recommended to eat fractional meals in small portions with the exception of coarse and gas-forming foods. And in severe cases of the disease, they may be indicated for surgical intervention to restore blood circulation in the abdominal branches of the aorta.
Differential diagnosis
In case of abdominal syndrome, it is necessary to differentiate the following ailments:
- Perforated ulcer (both duodenum and stomach). This disease is characterized by sharp and sudden pain in the epigastric region. Primary localization is the upper abdomen. Gradually, unpleasant sensations cover the entire abdomen, affecting its sections in turn.
- Acute cholecystitis. Repeated acute pain is observed in the right hypochondrium, accompanied by repeated vomiting, fever, and occasionally jaundice.
- Acute pancreatitis. This disease is caused by eating large amounts of fatty foods. Acute pain flares up suddenly and has a girdling character. The patient vomits bile and literally screams in pain. The muscles are tense, the stomach is swollen, peristalsis is weakened.
- Colic (renal and hepatic). The patient experiences cramping, acute pain, and there are also clinical manifestations of urolithiasis and cholelithiasis.
- Acute appendicitis. This pathology is easily confused with a perforated ulcer. In the second case, the syndrome is localized in the right iliac region, the peritoneum is irritated, and its anterior wall becomes tense.
- Thromboembolism. This disease affects the mesenteric vessels. There is no clear localization. The patient is tossing about in bed, he is worried, intoxication is rapidly turning into collapse. The patient suffers from loose bloody stools. The abdomen is distended and there is no peristalsis. The pulse is increased. Sometimes it is possible to identify a heart defect.
- Abdominal aortic aneurysm (dissecting). Typically, this disease affects older people. Occurs against the background of atherosclerosis. The pain flares up unexpectedly in the epigastrium. The abdominal muscles are tense, but the abdomen itself is not bloated. Blood pressure drops, pulse quickens. A tumor-like formation is palpable in the abdominal cavity. Limbs are weakened.
- Pleurisy and pneumonia (lower lobe). At first, the sensations are similar to abdominal syndrome, but examination reveals pneumonia.
Treatment
To suppress the syndrome, the following medications are used:
- Relaxers. They affect smooth muscles, reducing their contractile activity. Normal transit is restored, and the spasm is eliminated. Platyfillin (30-55 rubles), atropine (about 50 rubles), metacin (prices range from 15 to 253 rubles) have a good systemic effect.
- Myotropic antispasmodics. Designed to relieve abdominal pain. The most effective drugs are no-spa (cost - within 100 rubles), papaverine (up to 50 rubles).
- Mebeverine hydrochloride. It has a pronounced spasalytic effect and does not have an atropine-like effect on the body. Cost - 300-450 rubles.
- Selective blocker. Relieves abdominal pain at any level of the gastrointestinal tract. A typical example is pinaverium bromide (200-300 rubles).
- Prokinetics. Increase motor activity.
- NSAIDs. Regulate the mechanisms of pain perception. True, COX-2 inhibitors do not always achieve the desired analgesic effect.
Let us remind you that purchasing these substances in pharmacies on your own, without medical advice, is strictly not recommended.
https://www.youtube.com/watch?v=-2dtFRb0F_k
How is abdominal syndrome treated?
Due to the fact that the described condition is not a separate disease, but only a complex of symptoms, abdominal syndrome should be dealt with by eliminating, first of all, the cause that caused the disease. A significant role in this is also played by the elimination of motor disorders in the gastrointestinal tract and the normalization of the patient’s perception of pain.
To eliminate the discomfort that appears due to problems with the gastrointestinal tract, myotropic antispasmodics are usually prescribed. The most popular among them is the drug "Drotaverine", which has a highly selective effect and does not have a negative effect on the nervous and cardiovascular systems. This remedy not only has an antispasmodic effect, but also helps reduce blood viscosity, which makes it possible to use it not only for biliary dyskinesia, gastric or duodenal ulcers, but also for ischemic intestinal disease.
No less effective are drugs related to muscarinic receptor blockers (they create conditions for muscle relaxation and relief of spasms) or selective and non-selective anticholinergic blockers (Gastrocepin, Platifillin, Metacin, etc.).