Sometimes growths form on the mucous membrane of the lower intestine - polyps in the rectum. Difficult early diagnosis due to the asymptomatic course of the pathology leads to the risk of malignant degeneration of polyps. Treatment of rectal growths is usually surgical. Therapeutic measures in the form of ointments and suppositories are used as preoperative preparation and during the recovery period after surgery.
Photo of polyps in the intestines
Classification of neoplasms
Depending on the predominance of a particular type of cell in the tissues, formations in the rectum are of several types:
- Villous. They were named so because of the large number of small, seemingly easily bendable fibers collected together in the form of a sponge.
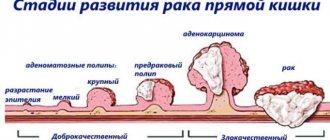
- Adenomatous. They consist predominantly of secretory cell tissues. Such formations more often than others turn into a malignant form, therefore, if an adenomatous polyp is suspected, they often talk about a condition when cancer may begin to develop.
- Fibrous. Such neoplasms consist of connective tissue cells that can easily replace the epithelial cover of the intestinal wall. Fibrous neoplasms become malignant extremely rarely; more often they provoke the development of various inflammations.
- Juvenile. These polyps are of the mixed type in their structure, which is characteristic of multiple rectal polyposis.
Polyps come in different types, but the discomfort they always cause is almost the same
There is also another classification based on the causes of their occurrence. According to this principle of division of education there are:
- inflammatory – formed due to a long inflammatory process in the tissues and cells of the rectum;
- neoplastic – resulting from an uncontrolled increase in the number of intestinal cells;
- hyperplastic - due to an increase in the number of abnormal cells.
Fibrous type of polyps
Such outgrowths are often called “false” due to the fact that their structure is represented by connective tissue and they are covered on top with epithelial cells. This is how to distinguish them from all other formations in the rectum. Another unique feature is that they never degenerate into malignant tumors. Such polyps appear in humans in response to inflammation in the rectum that remains untreated for a long time. Due to the force of the process, empty hemorrhoids and hypertrophied anal papillae degenerate into polyps in the form of pears or human fingers. As a result, these formations only make the course and diagnosis of diseases such as hemorrhoids, cryptitis, internal fistula and so on more difficult.
Adenomatous type of polyps
The formation of such a rectal polyp is considered a condition when cancer cells begin to develop. The cause of its occurrence is a disruption in the renewal process of epithelial cells in the rectal mucosa.
Due to the fact that cell division occurs without any control, entire colonies of polyps develop on the surface of the mucous membrane in the intestine. They begin to grow quickly and over time completely block the anal passage.
When their size and number increase greatly, a person begins to experience severe discomfort, unbearable itching and periodic pain in the anus. This is due to the fact that with each act of bowel movement, the neoplasms are injured and bleed. Pedicled adenomatous polyps in the rectum may prolapse from the anus.
Important: the main danger of increasing the number of polyps lies in the high risk of transition to a precancerous state and the occurrence of acute rectal obstruction.
To eliminate this type of tumor, a complex surgical operation is required, after which the patient faces a long recovery period.
Villous type of polyps
Such formations have a round or less often elongated shape and a velvety surface. They are prone to malignancy (transition to a malignant form).
In the initial stages of tumor growth, as a rule, they develop in two directions: either inside the intestine or along the mucosa. Over time, in the absence of proper treatment, the nature and speed of their growth changes. They begin to sink more and more into the intestinal wall and increase in size (can reach 7-10 centimeters).
Unlike other varieties, the first symptoms of such rectal polyps have their own characteristics. They are characterized as follows:
- Constant discharge from the anus of a viscous secretion, which looks like white from a raw chicken egg. Because of this very large amount of mucus, the rectum begins to become congested and the patient experiences frequent urge to defecate. The entire contents of the stool consists of this secretion alone.
- There are traces of blood in the stool. This is due to chronic damage to the villi.
- The patient feels heaviness and strong pressure in the rectum.
- Due to the strong growth of the polyp, obstruction and, as a result, constipation may occur.
- Those polyps that are close to the anus may fall out of it, thereby causing a strong feeling of discomfort.
Hyperplastic type of polyps
Such polyps are small in size and develop as a result of abnormally rapid division of epithelial cells of the rectal mucosa.
New growths are considered to be the most diverse in their shape: you can find ordinary spherical, mushroom-shaped, and branched ones. Their color also varies greatly and ranges from dark red to yellow.
Important: the cause of these tumors is often gastritis caused by the bacteria Helicobacter pylori. This must be taken into account when visiting a doctor.
If left untreated in the later stages, this form of polyps leads to the development of the following symptoms:
- severe pain in the anal area;
- bleeding and discharge of a small amount of mucus during bowel movements;
- nagging pain in the lower back.
Hyperplastic polyps often grow in colonies. The danger of delaying treatment of such formations lies in the fact that over time they begin to grow greatly and can lead to rupture of the intestinal walls.
Classification
In medicine, polyps are classified according to their morphological structure or the number and prevalence of tumors. In the first case they can be:
- villous, glandular or glandular-villous;
- fibrous;
- hyperplastic;
- cystic-granulating.
In the second case, the following types of pathology are distinguished:
- single neoplasm;
- a group of neoplasms (polyps can be detected in several parts of the intestine at once);
- familial polyposis;
- pseudopolyposis.
With familial polyposis, people most often suffer from numerous adenomatous neoplasms located in the large intestine. Usually the clinical picture in all relatives is the same, so at the first signs of the disease you should immediately visit a proctologist. The main danger of diffuse (familial) polyposis is the high probability of malignancy of the polyps.
With pseudopolyposis, there is a proliferation of the intestinal mucosa, which ultimately leads to the formation of nodes that look like polyps. An experienced doctor can easily recognize this type of pathology, but if there is doubt, a biopsy is performed to clarify the diagnosis.
Reasons for the development of polyps
Predisposing factors for the occurrence of formations include:
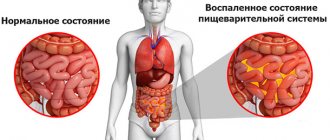
- proctitis, chronic enteritis, colitis and other inflammatory bowel diseases;
- haemorrhoids;
- anal sphincter fissures;
- infectious diseases of the gastrointestinal tract;
- chronic constipation;
- hereditary predisposition (familial polyposis);
- malformations of the fetus inside the womb;
- poor diet, which contains excess amounts of animal fats and does not include plant fiber;
- unfavorable ecology of the city;
- sedentary lifestyle.
What are polyps
Polyp is a descriptive term that refers to a growth of mucosal tissue (not skin). The formations have intraluminal growth and can be found in many cavitary organs, for example, in the uterus, vagina, throughout the intestine, in the urinary, gall bladder, etc.
Polyps in the anus can be single or multiple
Polyps look like raised growths and are attached in two ways: with a thin stalk or a wide base. Can be single or multiple. The presence of polyposis (multiple forms) in a family history increases the risk of their malignant transformation.
The pathology occurs in almost all age groups of the population. Men are 1.5 times more likely to suffer from intestinal polyposis. This pathology is diagnosed in 10% of people over the age of 40, of which in 1% of cases degeneration into a malignant form is eventually observed.
The disease is found in 30% of patients with chronic anal fissure and in 10% with prolapse of the rectal mucosa.
Symptoms characterizing rectal polyps
With rectal polyposis, people experience a number of symptoms typical for this disease. The main one is irregular bowel movements - alternating diarrhea and constipation. This symptom appears at the very first stages of the disease. This is due to primary irritation of the intestinal walls by the tissues of the developing polyp.
Subsequently, due to the steadily narrowing lumen of the intestine, the clinical picture begins to change. The patient is increasingly worried about long-term constipation, and their duration directly depends on how narrow the lumen has become. Such complaints often become the reason for going to the doctor.
Another symptom indicating the presence of neoplasms is severe discomfort in the rectal area and the feeling that there is something foreign in it. This sign makes itself felt when the formation grows to a large size.
A person feels small growths relatively rarely, and then only during contractions of the intestinal walls (during defecation). In this case, discomfort appears either from the pubic region or in the rectum itself.
Development and forms of formations
With polyposis, which has not been treated for a long time, the patient constantly experiences a feeling of fullness in the intestine. This feeling is only intensified by chronic constipation.
Pain in the lower abdomen is another characteristic sign of the presence of polyps in the rectum. It appears due to stagnation of digested food in the depths of the large intestine. As mentioned above, an overgrown tumor almost completely closes the lumen of the rectum and thereby provokes defecation disorders and the formation of chronic constipation. Due to excessive accumulation of waste food, the walls of the colon are stretched. As a result, this content puts pressure on nerve cells, which are found in abundance in the intestinal mucosa, and causes nagging pain. The situation becomes more serious if there is an accumulation of gases.
When mucous cells - obligatory companions of polyps - work more actively, the presence of a large amount of mucus in a person’s feces becomes noticeable. Normally, it is necessary to moisturize the organ cavity and facilitate the separation of feces. And in the case of a constantly growing tumor, the glands have to work in a tighter mode.
Excess mucus is not completely removed from the body. Most of it accumulates in the anal sinuses and serves as an excellent breeding ground for pathogens. Mucopurulent discharge will indicate an advanced disease process and infection.
The most obvious symptom indicating the neglect of the disease process is the presence of blood in the stool or bleeding from the sphincter. The cause of this alarming sign may be pinching of the tumor, damage to the vessels located in the submucosal layer of the intestine, or tissue necrosis.
Types of polyps
Based on the type of tissue that forms the structure, several types of intestinal outgrowths are distinguished:
- villous polyp of the rectum - often occurs in the elderly. Outgrowths on a broad base can cover the intestinal walls like a carpet. The surface of the villous polyp is densely penetrated with blood vessels. They often manifest themselves by bleeding from the anal canal. They have a high risk of oncogenic degeneration;
- fibrous polyp - formed from connective tissue, covered with epithelium. The formation of a fibrous growth is preceded by an inflammatory process of the rectum - hemorrhoids, cryptitis, proctitis. This is the most harmless type of growth in terms of turning into a cancerous tumor;
- adenomatous polyp of the rectum - grow to large sizes, over 1 cm in diameter. They have 2 types of fibers in their structure - tubular and villous. The higher the proportion of villous structures, the greater the likelihood of malignant growths and the occurrence of rectal cancer;
- juvenile or cystic polyp of the rectum in children, looks like small clusters covered with a large amount of mucus. Usually these are single formations, ranging in size from 5 to 20 mm.
Many polypoid formations in the anal canal are inherited. The outgrowths are grouped, forming numerous islands. The number of shoots ranges from hundreds to thousands. Such polyps are called familial, and with a high degree of probability they become malignant.
Diagnosis of polyps
How to identify polyps in the intestines? Today this is far from a problem, since modern medicine is literally replete with a variety of techniques. Among them are:
- Digital examination is the easiest and safest method of diagnosis. With its help, you can determine the size, number of polyps, whether they have legs and the nature of the consistency of the formations.
- Sigmoidoscopy is a method based on the introduction into the rectal cavity of a metal tube, which is equipped with a video camera at one end.
- Colonoscopy is an identical method that allows you to examine the condition of not only the rectum, but also the colon.
- Irrigoscopy is an X-ray examination with the introduction of a contrast agent. This diagnostic method is one of the most accurate, since with its help the doctor can accurately determine the location of polyps, their number and size.
- CT (computed tomography) is a method that has no contraindications and does not require any special preparation from the patient.
Using a colonoscope, the doctor will be able to examine everything in detail and detail.
Symptoms
The symptoms of rectal polyps are not particularly specific, which makes it difficult to differentiate them from other diseases. Among the main signs of pathology are the following manifestations:
discomfort inside the rectum (in the area of the anus). A person feels as if a foreign body is stuck inside him. Such discomfort is not constant, but is paroxysmal in nature. Constant discomfort with pain indicates that the polyp has reached a significant size;
- as polyposis develops, pain in the lower abdomen appears;
- bowel dysfunction, in which at the initial stage of the disease constipation alternates with diarrhea. With large polyps, chronic constipation appears. The frequency of bowel movements does not exceed 2 times in 7 days;
- impurities in feces. A constant symptom of rectal polyps is mucus in the stool, because... These benign formations have increased excretory capacity. The most dangerous manifestation is blood impurities. This may indicate pinching of the growth, its damage or necrosis.
What diseases can polyposis be confused with?
Rectal polyposis is usually differentiated from pelvic diseases such as:
- Lipomas are benign neoplasms localized in the submucosal layer of the colon. They, like polyps, can reach large sizes. Most often they are found in the right part of the intestine, less often along its entire length.
- Large fibroids.
- Angiomas are vascular-type tumors that bleed heavily as they increase in size.
- Actinomycosis of the colon is an infectious disease caused by radiant fungi.
- Crohn's disease is a chronic granulomatous inflammation that affects various segments of the digestive tract.
Prevention of occurrence
Prevention of rectal polyps is the prevention or reduction of the causes that contribute to the formation and growth of polyps. It is necessary to perform simple preventive actions to avoid cancerous tumors. These include:
- Treatment of diseases that become chronic;
- Replenishing the lack of vitamins and nutrients in the body;
- Eating the right nutritious food;
- Elimination of constipation;
- Visiting medical institutions for tests.
Diseases that contribute to the development of polyp-like growth include colitis, proctitis, Crohn's disease, colon dyskinesia, enteritis, and hemorrhoids. In case of inflammatory processes of these diseases, it is necessary to consult a specialist in a timely manner. This will favorably facilitate the correct diagnosis and treatment in the early stages of the disease.
- An important role is played by replenishing missing elements in the human body, such as vitamins A, C, D, E, folic acid, calcium, selenium and others.
- Eating whole grains (brown rice) and high fiber content (white cabbage) will be good for your health. Lean varieties of meat products (turkey) are more valuable than the abuse of “red meat” (smoked products). Vegetable fats (linseed oil) should replace animal fats.
- To avoid constipation, avoid fast food, play sports, do not use enemas, eat prunes and dried apricots, they contain potassium.
- After 40 years, it is recommended to periodically examine the colon and take a test for occult blood in the stool. The risks increase in males, those with a hereditary predisposition, and those living in large cities and industrial areas.
If you have already had surgery to remove the tumor, to avoid a recurrence, you must be monitored by a doctor. It is advisable to conduct a full examination once a year.
Treatment of polyps in children and adults
In children, these neoplasms never become malignant, so treatment of polyps in the rectum in them is based only on eliminating the source of bleeding. Surgical removal of growths in adults, on the contrary, is carried out to prevent the risk of their becoming malignant.
Polyps are removed exclusively surgically, but there are several methods of surgical excision. Each of them has its own characteristics:
- Transanal excision. This method is relevant for removing polyps located close to the anus. The canal is stretched with special hooks, after which the stem of the tumor is clamped with a clamp and bandaged. Next, the polyp is simply cut off.
- Electrocoagulation. Otherwise - cauterization. With this method, a special device is inserted into the anus, which is a source of alternating current and electrodes. Thanks to the gradually applied voltage, the leg of the polyp begins to char. After it has completely thinned out, the neoplasm is removed and the remaining wound is cauterized. The wound surface with this method is quite extensive, so several additional operations are performed.
Electrocoagulation is one of the most effective, but time-consuming methods
- Colotomy. This method involves isolating a segment of the intestine from the polyps and creating protection from gauze pads for the abdominal cavity. In this case, the polyp is simply cut off, after which sutures are placed on the wound.
- Resection of the rectum. This method is the only one possible when malignant tumors appear. During this procedure, a whole piece of tissue is cut out, while the patient is under general anesthesia.
Drug therapy
To treat polyps with medications, a special device is often used - a sigmoidoscope. It allows you to insert suppositories into the rectum.
Important: treatment with medications can only be carried out in the early stages, otherwise no effect will be achieved.
The suppositories must be administered twice a day: in the morning and in the evening (necessarily after an enema). Such treatment should be started immediately after the recommendation of a specialist, and carried out only by an experienced doctor.
Traditional medicine
Treatment of polyps in the rectum with folk remedies is quite common and can rightfully be considered very effective. One of the most popular methods is a celandine enema. The bioactive substances included in it directly affect benign formations on the legs and reject them without harm to the mucous membrane. After this, they are eliminated from the body naturally.
In order to achieve the desired effect, it is advisable to repeat the procedures every other day for 1-1.5 months.
Important: an enema with celandine is strictly prohibited for patients with hemorrhoids, ulcerative colitis, sphincter fissures and malignant tumors.
The article provides information for informational purposes only. It is the responsibility of the doctor to make a diagnosis and prescribe treatment.
Modern medicine uses the term “polyp” to define peculiar growths that form on the surface layer of the mucous membrane. These growths (polyps) look like spherical or mushroom-shaped growths, attached to an organ of the body with the help of a “leg”, or a dense base. The color range of polyps varies from gray-reddish to dark red, sometimes they are yellow.
Consequences of polyposis
If the identification and removal of a rectal polyp occurs at an early stage, then we can talk about the patient’s complete recovery. Relapses do occur; they occur after several years as a result of incompletely removed and residual effects of polyposis. To avoid relapses, a control colonoscopy is performed a year after the removal of large polyps, and the patient regularly undergoes endoscopic examination every 3-4 years.
The development of malignant polyposis is directly related to the number of tumors and their size. If there are many polyps and they are all large, then the risk of becoming malignant increases to 20%. Mostly patients suffering from hereditary polyposis are susceptible to cancer.
Polyp, what is it?
Polyps in the intestines
The size of the resulting polyps ranges from microscopic to solid, noticeable upon slight examination. On the outer surface of such formations there is a small layer of mucus; the consistency of the entire polyp is quite soft. Typically, polyps are harbingers of a benign or malignant tumor. Any fleshy growth or polyp very often causes various precancerous diseases. An old polyp can develop into a certain stage of a malignant tumor, such as colorectal cancer. Polyps can occur in both children and adults at any age.
The nature of the growth of polyps is associated with a tumor-like process occurring in the tissue lining the intestinal wall. As such growths on the walls increase, the lumen of the intestine itself decreases. The location or location of polyps in most cases refers to the rectal area or lower part of the large intestine.
The danger of the formation of fleshy growths or polyps in the body lies in the occurrence of causes that lead to the development of more serious complications in the organs. Often, due to a large accumulation of such growths in the lumens of the intestines, an obstruction through their lumen is formed. In the worst case, these polyps develop into malignant tumors, leading to cancer. In this regard, you should take care of the condition of your internal organs, especially the intestines.
Treatment
After the diagnosis is confirmed, the doctor decides whether the polyp needs to be removed. The volume, access and type of surgical intervention depend on the characteristics of the disease and the qualifications of the surgeon. Conservative therapy is ineffective, so it is used as an additional method or palliative care in seriously ill patients.
You can try to treat polyps without surgery, but it is important to consider that the risk of worsening the condition, recurrence, or developing colorectal cancer is too high.
To prevent surgical intervention, the patient may be prescribed symptomatic medications. It should be remembered that they do not have a direct therapeutic effect, so the advisability of conservative therapy for polyps is questionable.
Principles of surgery
The only method of treatment remains surgical intervention. In some cases, the diagnosis is confirmed after obtaining data on the morphological characteristics of the polyp (tissue origin).
Rectal polyps are resected taking into account the possibility of preserving all somatic functions. The following types of interventions are performed:
- Electrocoagulation;
- Polyp removal during colonoscopy;
- Transabdominal tissue excision;
- Radical removal of the rectum. The operation is mutilating, therefore it is carried out strictly in accordance with the indications (multiple lesions, suspicion of malignancy).
If the process spreads to the overlying sections, resection of a large part of the colon with the formation of a temporary or permanent colostomy may be required.
Principles of conservative therapy
As such, there are no conservative methods to combat polyps. As supportive and symptomatic therapy, it is possible to prescribe various medications (laxatives, painkillers, iron supplements, infusion solutions) in the pre- and postoperative period, taking into account the patient’s condition.
Rectal polyps cannot be cured without surgery!
There is evidence that Chistobilin suppositories are used to treat polyps, avoiding surgery. They contain natural ingredients (extracts from hemlock and burdock root), which have the following effects:
- Anti-inflammatory;
- Anesthetic;
- Antitumor;
- Immunostimulating.
These suppositories are considered more of a hygienic product, used to prevent various neoplasms in the pelvic organs. To date, there is no reliable data that would allow us to judge their effectiveness.
Signs of rectal polyp
The rectum, which is susceptible to the appearance of such growths, is responsible for removing undigested residues from the body, so polyps in its lumen will significantly worsen this process, leading to pain. Excessive concern for the condition of the intestines will help prevent the development of polyps in the body. How can you determine whether there are polyps in the rectum?
The presence of polyps in the area of the rectum, their number and size can be detected during an endoscopic examination of this organ. There are cases when these formations are detected by chance, during an examination of the body for the presence of other pathologies. Large polyps may manifest themselves by defecation. In the stool, if there are polyps in the rectum, a small amount of blood or mucus is detected. The blood discharge accompanied by feces is usually red, less often scarlet in color. If you find such feces in yourself, you should visit a medical facility as soon as possible to obtain medical advice.
Sometimes, when polyps form on the walls of the rectum, the patient feels an increase in body temperature, which indicates the beginning of an inflammatory process in the body that occurs in the area of the polyp. The growths can also cause corresponding pain in the abdominal area, as well as symptoms of diarrhea and characteristic constipation. In most cases, the patient feels constipation during bowel movements, caused by blockage of the lumen of the rectum and obstruction of feces from the body.
Large polyps often lead to blockage of the lumen of the rectum, while the patient feels the presence of a foreign object in the anus. In cases where the resulting polyps are attached to the intestinal wall with the help of a pedicle, the patient may observe its prolapse from the anus during defecation. If several polyps have formed on the walls of the rectum, then polyposis of this organ is diagnosed.
Causes
The mechanism of polyp formation, as well as the main pathogenetic factor leading to primary changes in the rectal mucosa, have not been fully studied. But there is a clear relationship between the growth of tumors and chronic inflammatory diseases of the gastrointestinal tract. So, the people most susceptible to rectal polyposis are:
- not following the basic principles of a healthy diet;
- abusing carbonated and alcoholic drinks;
- those suffering from obesity due to systematic overeating;
- prone to severe allergic reactions, especially to gluten.
Vascular atherosclerosis or thrombophlebitis of the rectum can lead to the formation of polyps. These pathologies are often a consequence of smoking. Other reasons for the development of polyposis include:
- infectious diseases of the gastrointestinal tract (rotavirus, dysentery, salmonellosis, etc.);
- intoxication of the body due to prolonged use of certain medications or other chemicals;
- physical inactivity, in which blood stagnates in the pelvis and lymph flow is disrupted, which leads to dilation of the rectal veins and tissue swelling;
- regular constipation;
- ulcerative colitis, enteritis, hemorrhoids;
- age-related changes.
Sometimes polyps are found in absolutely healthy people, but a thorough study of the issue most often reveals the patient’s genetic predisposition to polyposis. In other cases, a mutation may be diagnosed - incorrectly formed intestinal loops as a result of various disorders of fetal development in the antenatal period.
Why do polyps appear in the rectum?
Symptoms can be completely different
Today, scientists consider the following to be the main causes of polyps on the walls of the rectum:
- Hereditary predisposition of a person to the occurrence of a disease.
- Inflammatory processes in the rectum.
- Poor nutrition.
- Excessive drinking.
- Low human mobility.
- Bad ecology
Let's consider these reasons in more detail. Most scientists, based on the results of the study, came to the conclusion that it is human heredity that contributes to the appearance of these formations on the intestinal walls. At birth, a person’s genetic material may carry the makings of the development of polyps on his organs, including the rectum.
Polyps can develop in the human body even if there are inflammatory processes of various natures in the rectum that can cause the development of fleshy growths on the inner walls of the intestine. Most often, enteritis or colitis, as well as the development of dysentery in the body, lead to the appearance of polyps. An irrational and unbalanced human diet is often also the cause of polyps in the body. Especially often, growths on the intestinal walls occur when eating food that is oversaturated with fats of animal origin. Lack of plant fiber in food also contributes to the growth of the internal walls of the rectum.
The negative effects of the surrounding environment, excessive consumption of alcoholic beverages, and a sedentary lifestyle often have a beneficial effect on the development of polyps on the walls of the rectum. Taking into account the above reasons, it is possible to prevent the occurrence and significantly slow down the further development of polyp growths in the body.
Complications
If the detected tumors are not removed in time, the following complications may develop:
- malignancy of formation (degeneration into a cancerous tumor);
- inflammatory process in the intestines (enterocolitis);
- formation of fecal stones;
- anemia;
- intestinal obstruction.
Polyps in the rectum are a fairly serious pathology, so if you suspect their presence, you should first consult a doctor.
Diagnosis of polyps in the rectum
Take care of your health - save the VKontakte link
Variety of polypous formations
The presence of polyp formations on the walls of the rectum can be diagnosed if the patient regularly undergoes appropriate examinations. When confirming the presence of polyps, the doctor can determine their size, number, and the degree of risk of precancerous complications. The easiest way to determine polyps in the rectum is based on a digital examination of the patient's anus. Such a study allows not only to confirm, but also to refute the presence of these pathologies in the organ under study.
Another method to detect the presence of polyps in the intestine is sigmoidoscopy. This method allows you to examine in detail the inner wall of the rectum at a distance of up to twenty-five centimeters from the anus. Since polyps in most cases form at a given height of the rectum, the rectoscope can easily detect them.
Colonoscopy is also one of the reliable methods that can detect polyps in the lumen of the rectum. The method of such an examination is based on comprehensive visualization of the entire intestine, which makes it possible to determine the area in which the growths have formed. Both described methods, when special equipment is used, quickly and correctly determine the presence of polyps in the body, and also provide a lot of necessary information about them related to their structure, quantity, etc.
Sometimes, by examining the rectal cavity using these methods, the doctor has the opportunity to quickly remove polyp growths that are sessile on a stalk from the organ. This is achieved by introducing into the body a special electrode with a loop-shaped end, capable of cutting off the polyp from the intestinal wall. After this operation, the doctor cauterizes the area where the polyp was located. The growth removed from the body is subject to detailed study.
Modern medicine offers another method for diagnosing polyp growths in the body, this is irrigoscopy. This method allows you to detect polyps on the walls of the rectum if their size reaches one centimeter or more. Irrigoscopy is based on an X-ray examination of the entire rectum and intestines as a whole. When using irrigoscopy, a special contrast agent is injected into the organ.
Diagnostics
Procedures that help diagnose pathology are:
A colonoscopy may be required to examine the patient.
- Finger examination. The doctor palpates the rectum and anus from the outside. This method allows you to identify pathological changes in the mucosa and the presence of growths.
- Sigmoidoscopy. A thin tube is inserted into the intestine, the tip of which is equipped with a microvideo camera. Thanks to this study, the doctor will see ulcerations, diverticula, polyps and other pathologies on the mucous membrane.
- Colonoscopy. Helps examine the entire length of the intestine. But if the polyposis is bleeding and complicated, this type of diagnosis is contraindicated.
- Irrigoscopy. A contrast liquid is injected into the colon, after which a series of photographs are taken in which the proctologist identifies the slightest pathological changes.
- MRI or CT. These are modern diagnostic methods that will show the presence of the disease, even if it develops at the initial stage.
- Biopsy. A mandatory diagnostic procedure, during which a tissue sample is taken from the affected area and examined for the presence of cancer cells.
Treatment methods for anal polyps
Why suffer from discomfort and pain in the anus when you can easily get rid of the disease in the shortest possible time?
Based on the diagnostic results, the following treatment methods for the anus can be prescribed:
It is advisable to remove neoplasms, especially in places of constant irritation and injury (perianal areas, groin, etc.). After the procedure, the patient calmly leaves the clinic.
Symptoms and causes
The exact reasons why anal polyps occur have not yet been established. There are many theories explaining the appearance of these defects. It is believed that chronic inflammatory diseases can provoke the formation of such neoplasms. Such pathologies lead to rapid aging of the epithelial layer and disruptions in cell division. Inflammatory diseases that often cause polyps include:
- enteritis;
- typhoid fever;
- dysentery;
- ulcerative colitis;
- ulcerative proctosigmoiditis;
- haemorrhoids.
Forecast and preventive measures
If polyps are removed in a timely manner, the prognosis is favorable. With multiple formations against the background of intestinal inflammation, it worsens. When there is a predisposition to cancer, after removal of polyps you need to undergo regular preventive examinations with a proctologist.
The main preventive measure is a healthy diet with a predominance of plant fiber in the diet. Doctors note that in people with unchanged rectal mucosa, the likelihood of polyps appearing is virtually eliminated. This suggests that for prevention it is important to undergo examination by a proctologist when complaints arise for early treatment of inflammatory diseases of the gastrointestinal tract.
A polyp in the anus occurs as a result of pathological proliferation of tissue of the epithelial layer. This formation is the result of a violation of the regenerative ability of the cellular apparatus. This defect is often encountered in proctology. Despite the fact that such formations can appear in patients of any age, they are more often diagnosed in people over 45 years of age. Such defects cannot be left without treatment, because they can become the basis for the development of malignant tumors.
Definition of disease. Causes of the disease
Anal polyps (AP) are a collective concept used to refer to neoplasms within the anal canal. This is not the most common proctological disease, but it joins other chronic inflammatory conditions of the terminal colon. When diagnosed with anal polyp, patients are often afraid of the consequences in the form of cancerous tumors. This is completely justified. Therefore, the disease requires careful diagnosis and timely treatment.
Anal canal polyps are usually called all kinds of volumetric formations within the anal canal that protrude into the lumen of the intestine. The sources of polyp formation can be any cells from tissues located in the anal area.
The reasons for the formation of AP are quite a few factors, which is explained by the great diversity of their origin and histological structure. We can definitely say that these polyps accompany (or complicate) the course of chronic inflammatory diseases both in the anorectal area and in the intestinal tract as a whole.
To clarify the boundaries of the anal canal, the Russian Society of Coloproctologists recommends the wording: “The anal canal is the terminal part of the digestive tract, starting from the place of the anorectal junction at the upper border of the pelvic floor and ending with the external opening - the anus, the boundary of which is the place of transition of the non-pigmented anoderm into the pigmented (true) one. skin." [eleven]
Causes of AP:
- long-term inflammatory processes in the intestines and anorectal area (chronic fissures, chronic hemorrhoids, colitis, including Crohn's disease, ulcerative colitis);
- regular trauma to the rectal mucosa (chronic constipation, prolonged diarrhea, practice of unconventional types of sex, abuse of strong alcohol, spicy foods);
- genetic predisposition to tumor formation (familial polyposis, etc.).
Complications of anal polyp
With large polyps, as well as with multiple formations, complications may occur in the form of bleeding, constipation, and irritable bowel syndrome. The most serious consequence is intestinal obstruction, which requires immediate assistance with surgical intervention.
Other possible complications of polyposis:
- degeneration into a cancerous process;
- anemic syndrome;
- prolapse and necrosis of the polyp.
Intestinal obstruction
Intestinal obstruction can occur against the background of chronic constipation, which often accompanies polyposis. This disease is manifested by severe pain, nausea, vomiting, increased abdominal volume, and lack of bowel movements. The pain syndrome is the most pronounced, manifested by cramping severe pain, when a person takes a forced squatting position, distorts, and groans.
During the attack, pale skin, cold sweat, tachycardia, and hypotension are observed. Without timely medical care, there is a high probability of death from intestinal rupture and poisoning of the body with toxins.
Complications and dangers of pathology
In the vast majority of cases, the disorder is successfully treated by surgical removal of nodes from the intestinal mucosa.
Complications can arise only in cases where the disease, without being promptly noticed and identified, develops to the stage at which the transformation of a benign polyp into a malignant neoplasm begins.
However, even if the polyps are successfully removed, the disease may return in the form of relapses.
Etiology
No one can still say reliably where polyps in the sigmoid colon come from. There are a number of theories suggesting the probable causes of these neoplasms. It was noted that people suffering from chronic intestinal inflammation are most susceptible to the appearance of polyps. In addition, a number of factors have been discovered that increase the risk of developing this pathology:
- Errors in diet and consumption of foods that contribute to the appearance of inflammatory reactions in the intestines;
- Chronic constipation caused by stagnation in the intestines;
- Permanent injuries to the mucous membrane with hard feces;
- Acute infection.
All of the above factors are to one degree or another associated with poor nutrition. Frequent consumption of low-quality and fatty foods, as well as the lack of foods containing fiber in the diet, can lead to improper formation of feces. Due to its anatomical features, the sigmoid colon is very vulnerable to such damage. The density of feces in the left parts of the colon is higher compared to the left, while the sigmoid colon has two bends that increase the likelihood of injury.
There is an embryonic theory, which suggests that polyps form in humans in the womb. During the formation of the intestine, improper formation of epithelial tissue occurs, which subsequently leads to the appearance of polyps on the mucous membranes. A relationship was noted between the formation of polyps and other gastrointestinal disorders (diverticulosis, circulatory failure). There is a family predisposition to the formation of polyps. The most common pathologies are Peutz-Jeghers syndrome and Gardner syndrome.
Treatment of polyps in the intestines with folk remedies
It is impossible to completely recover from the causes of polyposis using folk remedies without traditional medicine, but herbal decoctions are perfect for normalizing digestion and relieving symptoms of the disease. Herbal medicine is good for prevention: it will prevent the development of cancer. The main thing is to coordinate the treatment of intestinal polyps with folk remedies with your doctor.
Here are some of the most popular recipes for treating symptoms:
- Pour boiling water over yarrow, celandine, St. John's wort and chaga in an amount of 1 teaspoon each and let it brew for 20 minutes. Take half a glass before meals.
- Pour boiling water over 3 tablespoons of viburnum berries and let cool. The drink can be drunk instead of tea and before meals.
- Mix honey and grated horseradish root in equal parts. Take 1 teaspoon on an empty stomach every day.
Find out more about how chaga is used for oncology.
Treatment of rectal polyps with celandine
Medicinal plants become a preventive measure for a whole range of diseases, and polyposis in this case is no exception. Treatment of intestinal polyps with celandine (especially in the rectum and large intestine) is best done using an enema. The simplest and most effective recipe is as follows: 2 parts of yarrow, 1 part of celandine and calendula flowers are poured with boiling water and allowed to cool, the broth is filtered, corn oil is added and shaken well. How to treat: administer into an empty intestine 2 times a day in 50 ml portions.
How to treat polyps?
The main method of treating polyposis is surgical removal of even the smallest growths detected. Both in the situation with single formations and with multiple ones, therapeutic treatment does not make sense. If the diagnosis reveals polyps, you need to get rid of them without delay, and then conduct histology of the removed formations.
Polyp removal
More often, the procedure for removing polyps is performed using endoscopic equipment and may not even require general anesthesia. An endoscope with a lighting device, at the end of which there is a loop electrode, is inserted through the patient's anus. The doctor places a loop over the polyp, grasping it at the base, tightens it and cuts it off at the base, along with the stem.
There is also a method of electrocoagulation - cauterization or excision of polyps with a laser. This intervention is suitable for removing small polyps, since working with a laser on space-occupying formations risks unintentional perforation of the rectal wall. The good thing about the procedure is that, in parallel with the removal of the polyp, the laser seals and seals the vessels and mucous membrane, eliminating bleeding and complications after surgery. Laser exposure also has a disinfecting effect, and the risk of infection entering wounds is significantly reduced. The only condition is that electrocoagulation is applied only to polyps located no deeper than eight centimeters from the anus.
The two above-mentioned methods are minimally traumatic; after the intervention, patients can walk independently and the next day continue to live in a normal rhythm, without unnecessary stress.
Endoscopic polyp removal process
If the polyps affect a significant part of the intestine, are located too close to each other, or there are a large number of them, the surgeon performs abdominal surgery and excises part of the intestine. This procedure requires a long recovery period. After the operation, the excised part of the organ along with the polyps is sent for examination, based on the results of which it becomes clear whether malignant transformation has occurred in the formations.
After the polyps have been removed by any means (or they have “gone away” on their own during conservative treatment of the underlying disease), a year later the patient must undergo a routine colonoscopy to ensure that there are no new formations. If no polyps are found during diagnosis, the procedure can be performed every three years. According to statistics, in 14% of patients, formations may recur at the site of removal, and in 7%, relapse occurs in other, previously unaffected areas of the epithelium. Therefore, you need to be understanding of the need for preventive diagnostics.
More detailed information about polyp removal can be found in our special article.
Video - Consultation with a proctologist: intestinal polyps
Consequences of polyps
The most common consequence of polyps is constipation, since their presence in the lumen causes partial intestinal obstruction. A dangerous sign that requires immediate consultation with a doctor is bleeding, because it may be caused by oncological pathology, the detection of which at an early stage will contribute to more successful treatment. The occurrence of an inflammatory process with polyps is most often indicated by abdominal pain. How to identify an anal polyp? More on this later.
Diagnosis of polyposis
A proctologist is a specialist who should be contacted if a person has discovered primary symptoms of polyposis or simply wants to know about the state of his own health. The doctor will first ask about complaints and symptoms, then conduct a manual examination, palpating the rectum at its entrance and as deep as possible. Polyps are sometimes located several centimeters from the anus, then upon palpation they are detected.
Polyposis can only be detected visually using modern diagnostic methods.
If this research method shows the presence of polyposis, more detailed information can be obtained by sigmoidoscopy. Diagnostics is possible using a special tube-shaped device that pumps air into the rectum and thereby straightens its walls. When inspection is possible, the doctor turns off the air supply, turns on the miniature light at the end of the tube, and adjusts the eyepiece. A sigmoidoscopy allows not only to detect the presence of polyps, but also to find out in what quantity they are, what size they are and where they are located.
Also, formations are diagnosed using x-rays of the colon and even the stomach, since polyps often affect the higher segments of the gastrointestinal tract. An X-ray examination, like sigmoidoscopy, provides complete information about polyps; in addition, the doctor can obtain data on the benignity or malignancy of the formations. In the case of the rectum, this method is called irrigoscopy - through the anus, in the form of an enema, the patient is sprayed with a contrast agent, which is distributed along the walls and shows very clearly their contours and all foreign formations.
Irrigoscopy of the intestine
Colonoscopy is considered the classic method for examining the rectum. With colonoscopy, the doctor can examine up to a meter of intestine by inserting an endoscopic tube through the anus. The device has a very small diameter, so it easily passes through all the narrowing of the intestines and clearly shows how things are with the patient’s health. This procedure is required to be completed annually by all citizens over fifty years of age.
Diet before colonoscopy
Prevention
To reduce the risk of developing anal polyps, you need to eat right. You should regularly consume foods containing plant fiber. In addition, to improve intestinal motility, it is necessary to maintain normal physical activity.
To prevent the appearance of such neoplasms, it is recommended to stop smoking and drinking alcohol. People over 45 years of age should undergo regular preventive examinations to timely identify existing defects and begin their treatment.
Manifestations of polyposis
The disease does not have specific symptoms that would accurately indicate the presence of pathology. Polyposis in most cases is combined with other intestinal diseases, so their manifestations can be observed.
Some symptoms may still indicate the presence of formations. Their severity will depend on the form of the disease, the size of the polyps and associated disorders.
Polyps are often discovered accidentally during a routine examination or diagnosis for another disease.
What manifestations can be observed with polyposis:
- feeling of discomfort;
- discharge from the anus;
- bleeding from the rectum;
- dyspeptic symptoms;
- frequent urge to defecate without subsequent bowel movements.
Unpleasant sensations arise due to the movement of the free part of the formation, which leads to irritation of the intestinal walls. In rare cases, pain may be bothersome. Symptoms are more pronounced during walking, and subside at rest.
The causes of pain are destruction of the formation and injury to the already inflamed intestinal mucosa. In the first case, we are talking about the transition of the disease to cancer, in the second case, about pathology against the background of paraproctitis.
Symptoms
Only a coloproctologist can accurately determine whether a patient has polyps in the intestines
Symptoms indicating that there are polyps in the anus are often vague and unreliable.
Symptoms rarely appear fully, and their severity depends on which anal polyps have developed in a particular case.
Often, anal polyps are discovered completely by accident when conducting any research about other diseases; it is often possible to detect a polyp on an endoscopic photo.
However, although symptoms may not be noticeable, people over 40 years of age are advised to undergo annual examinations to diagnose the disease in its early stages and begin its treatment.
Timely treatment of polyposis can prevent complications such as the degeneration of a benign neoplasm into a malignant one, as well as the development of obstruction.
Symptoms that may manifest as polyps growing in the anus may be as follows:
- the presence of bloody or mucous discharge that appears during defecation;
- increased body temperature if there are symptoms of inflammation;
- frequent congestion in the rectum or, on the contrary, diarrhea, for which it is not possible to find a treatment;
- pain in the lower abdomen;
- loss of lumps resembling hemorrhoids, which can be seen even in the photo.
The similarity of polyps to hemorrhoids complicates diagnosis and selection of treatment methods. The symptoms that appear in both cases are identical, so it is impossible to accurately diagnose the disease based on the clinical picture.
Treatment methods
Treatment of polyps cannot be carried out using conservative therapy, that is, treatment with folk remedies and medications is unacceptable.
The only true treatment is removal using endoscopic or surgical techniques.
If the anal polyp is located low enough, treatment involves removal through the anus.
If the polyp is small and found high in the colon, then treatment includes removal using endoscopic electroexcision (exposure to current). Treatment of large polyps is carried out by removing them from the intestines in parts.
As soon as the polyp is removed, it must be sent for histological examination.
Treatment of diffuse polyposis is carried out by removing the affected part of the intestine.