An esophageal foreign body with an ICD-10 code is a deliberately or accidentally swallowed object or food particles lodged in the digestive lumen. A stuck foreign body is accompanied by spasms and pain, dysphagia, suffocation, vomiting with blood and swelling of the cervical tissues. A foreign body in the esophagus can be diagnosed using an x-ray, on the basis of which the patient is prescribed appropriate treatment.
Children are more susceptible to foreign substances entering the esophagus.
Causes of a foreign body
A foreign body may appear in the esophagus for a number of the following reasons:
- when rushing while eating, which leads to poor chewing of food;
- inattention during cooking results in foreign objects getting into the dishes;
- people with the habit of keeping all sorts of foreign things in their mouths, especially children;
- in elderly patients who have poorly fixed removable dentures;
- with special swallowing of things by mentally ill patients;
- foreign objects block the lumen of the esophagus due to burns, tumors and functional disorders;
- Specialists with the profession of a seamstress or carpenter have a habit of holding screws, bolts, needles, and clamps with their teeth.
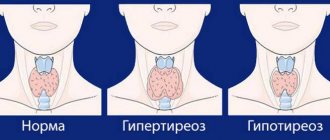
Thyroid pathologies
With diseases of the thyroid gland, its size increases, which leads to compression of the organs located next to it. There is a sensation as if there is a lump in the esophagus , which makes swallowing and breathing difficult. A lump in the throat and esophagus can occur with the following pathologies of the thyroid gland:
- Diffuse goiter , which may cause frequent dry cough, discomfort when eating, hoarse voice, difficulty breathing in tight clothing. The cough is observed when lying on your back. Therefore, the patient has to sleep on his side.
- Nodular goiter , with partial damage to the thyroid gland. A feature of the pathology is the constant presence of a lump in the throat, and not periodic, as is the case with diffuse damage to the gland.
So, with a disease of the thyroid gland, a lump in the esophagus, what it could be is diagnosed during an examination of the organ. In any case, if you experience discomfort in the throat or esophagus, you should definitely consult a specialist to rule out thyroid pathology. If a disturbance in the functioning of this organ is nevertheless detected, then it is not the symptom that is treated, but the thyroid gland - a very important organ in the human endocrine system.
Hitting methods
Foreign bodies of the esophagus (ICD-10 code) enter the organ through the oral cavity. Obstruction of a foreign object occurs due to a physiological narrowing of the esophagus, which results in difficulty swallowing, vomiting, coughing and a painful sensation in the chest. If a child swallows a sharp object, there is a risk of damage to the esophageal mucosa. Physical damage to the esophageal tissue can lead to the penetration of infections through damaged areas of the organ and contribute to the development of periesophagitis, which can develop into mediastinitis . Foreign objects can enter the esophagus due to various esophageal pathologies.
Features of the pathology
Foreign objects and difficult-to-swallow foods get stuck in the physiological narrowing of the esophageal tube. Delay of objects can be observed in the thoracic, diaphragmatic-cardiac, and cervical regions. This depends on the shape, volume of the object, and the elasticity of the muscles of the internal walls of the organ. Accumulations of undigested food in the area of chest constriction, observed in children and the elderly, are also considered foreign objects.
Ingestion of foreign bodies, depending on the organic or mechanical origin of the object, contributes to the occurrence of edema, inflammation, reflex muscle contraction, the formation of erosions and cicatricial deformities, as a result - obstruction of food into the stomach. Penetration of sharp objects leads to damage to the esophageal mucosa. Through irritated walls, infections and pathogenic bacteria enter, affecting the functioning of the body.
Symptoms
A foreign body (ICD-10 code) that has entered the esophagus has symptoms that are divided into late, early and immediate. The latter symptoms occur when foreign bodies are absorbed and affect the walls of the esophagus. The early ones follow the first ones and progress throughout further exacerbation. In the later stages of symptoms, complications occur in the form of infection and perforation.
Immediate symptoms are explained by the occurrence of a feeling of pain when swallowing a foreign object and is accompanied by increased salivation. Depending on the nature of the course and intensity of the pain syndrome, it is stated that a foreign object is stuck, damaging the mucous membrane and leading to perforations or ruptures of the walls of the esophagus. Symptoms manifest as pain in the upper esophageal sections.
Painful sensations can be constant or variable. Pain on a constant basis indicates the penetration of foreign bodies into the esophageal wall, damaging it and forming through holes. The pain can be localized behind the sternum, in the cervical region or between the shoulder blades.
Foreign objects entering the lower esophagus can cause compressive sensations in the sternum and heart. There is pain in the back, sacral region and lower back. Often, the symptoms are caused solely by the consequences on the walls of the esophagus from a foreign body that has already entered the stomach.
At the stage of early symptoms, there is difficulty in drinking liquid, which leads to severe thirst. Patients begin to rapidly lose body weight as a result of an imbalance in the body's water balance. If a foreign object stops at the entrance to the esophagus, the patient’s breathing is impaired, which is caused by spasm and compression of the larynx.
At the final stage of early symptoms, various signs of foreign body obstruction may form, which manifest themselves in the sudden onset of pain and its localization below the initial level of foreign object formation. In addition, compaction occurs in the soft tissues of the cricoid cartilage and neck. Foreign objects can cause a sharp increase in body temperature, which is accompanied by chills.
Secondary symptoms arise after the primary ones and manifest themselves exclusively during the meal of food that has a dense structure. At a late stage of symptoms, foreign objects manifest themselves as usual symptoms, which gradually develop into inflammation of the esophagus and the surrounding tissue.
In addition to the above symptoms, a patient with a foreign body may experience a feeling of constriction in the throat, as well as belching, increased salivation, regurgitation, vomiting, and tachycardia. The victim experiences pain when swallowing food, hoarseness, and an increase in body temperature.
Symptoms
Signs depend on the shape, volume, time spent, and location of the foreign object. Pronounced symptoms of a foreign body of the esophagus at different stages are:
- Immediate: acute pain when swallowing, spasms in the area where the object is located, excessive salivation, a feeling of constriction, asphyxia when the trachea is pressed, tachycardia, panic attack.
- Early: constant spasms radiating to the heart, adrenal glands when entering the thoracic region, dysphagia (vomiting, belching), severe thirst with difficulty absorbing liquid, water-salt imbalance, weight loss, elevated temperature.
- Late: hoarseness, difficulty breathing, hyperthermia, chills, fever.
The degree of strength of the pain syndrome indicates the location of the object: constant spasms occur when the object is in the area of the esophageal wall. Primary, immediate symptoms appear immediately after the body enters with partial or complete occlusion of the organ. Secondary signs are observed during the process of food absorption. Late symptoms indicate an inflammatory process.
Pronounced signs of a foreign object in children are severe crying, excessive drooling, lack of motor activity of the head, decreased appetite, and cough. Penetration of small objects that do not block the lumen of the esophagus is not accompanied by symptoms. Radiography allows identification of a foreign body.
First aid
To avoid complications from a foreign object entering the esophagus, the patient should immediately receive first aid. A foreign object in the esophagus with a code in the International Classification of Diseases - 10 requires urgent hospitalization in the surgical department, where the patient will undergo the necessary measures to remove the object. You should not try to help yourself and push the object into the stomach; doctors do not recommend pushing it with bread, meat and other solid foods, which can also get stuck in the esophagus and injure the mucous membrane.
Health care
If the methods described above do not help, you should go to the doctor. At the hospital, they will first induce vomiting to try to push the lump out. Next, the person is fully examined to understand why food is getting stuck in the esophagus.
Examination methods include radiography and endoscopy. The first method is needed to determine in which part of the esophagus the foreign body is located. Endoscopy allows the doctor to assess the condition of the mucous membrane. If food does not pass due to the presence of tumors, then using this device you can take tissue for a biopsy.
Note! Quite often, if food does not pass and causes pain, this may mean the presence of a pathology called achalasia cardia. That is, when the migration of food into the stomach is impaired.
And also if food regularly gets stuck in the esophagus, then there may be other pathological reasons for this:
- tumor formations in the esophagus;
- esophageal stenosis;
- atony;
- esophagitis of an infectious nature;
- chemical burn.
In such cases, a person needs serious treatment, since these pathologies can lead to negative consequences. In all these conditions there will be pain or discomfort behind the sternum. In some pathologies, pain spreads to the neck or arm.
Neuroses also lead to the sensation of a lump in the esophagus. When a person is stressed, blood pressure rises, and as a result, the mucous membrane swells. In this state, a person wants to eat, and food passes through a narrow hole. This is also characterized by food getting caught in loose tonsils and the walls of the esophagus. As a result, discomfort appears, which a person may mistake for a lump of food. For this reason, the person is fully examined, and it is especially important to prescribe a psychiatrist. These will be sedative medications.
Every person should know what to do if food is stuck in the esophagus, since such a situation can arise anywhere and anytime. But if food often gets stuck in the esophagus, then you should undergo an examination.
Diagnostics
A foreign object that has entered the esophagus requires diagnosis, which is based on a visual examination of the pharynx, neck, larynx, esophagoscopy and x-rays. Diagnosis allows you to examine the walls of the esophagus for the presence of damage and its depth, based on which the volume and urgency of the operation will be determined. The x-ray is carried out in two projections and allows you to easily examine radiopaque materials - meat bones, metal objects and large bones.
Foreign objects that have poor contrast and are X-ray negative are detected in the organ by radiography using barium or an iodine-containing substance, and, if necessary, by fistulography, computed tomography, and ultrasound. By diagnosing a foreign object in an organ by esophagoscopy, doctors are given the opportunity to study its location and assess the integrity of the walls of the esophagus.
If a patient has a peptic ulcer of the esophagus, esophagospasm, paralysis of the pharyngeal muscles, by diagnosing a foreign object, the doctor can detect the patient’s hernias, ulcers, tumors, diverticula and strictures.
Methods for diagnosing dysphagia
Dysphagia is not an independent disease, but a symptom of another disease.
Finding out the cause of dysphagia requires a careful doctor’s approach to the clinical examination of the patient, finding out the history of his life and the development of the disease, as well as dietary habits and lifestyle. After preliminary data collection, additional research methods may be prescribed:
- Endoscopic examination of the esophagus and stomach can help in most percent of cases. Using this method, the doctor is able to visually evaluate the esophagus and identify the causes of dysphagia. Using this examination, you can diagnose gastric ulcers and reflux esophagitis.
- If a tumor process is suspected in the esophagus, fibroesophagogastroscopy with biopsy is performed. A small piece of the mucous membrane of the organ is taken for a special morphological study, where the diagnosis of the tumor will be confirmed or not.
- If a diaphragmatic hernia is suspected with the esophagus and part of the stomach emerging into the chest cavity, an X-ray examination is performed using a contrast agent.
- In case of peptic ulcer, it is important to identify the bacterium Helicobacter pylori, which causes inflammation in the mucous membranes and peptic ulcer.
If using these methods it is not possible to establish the cause of dysphagia, then it is necessary to consult a neurologist, since the symptom most likely has a neurological cause. The accumulation of stuck food in this case is associated with neuro-reflex reactions.
Treatment
After an X-ray examination, made in two projections, of an object lodged in the esophagus, the doctor prescribes appropriate treatment, which can be surgical or conservative. The choice of treatment method depends on the obtained indicators and the need for emergency action. Treatment in any case is based on removing the body from the lumen of the esophagus.
Having studied the location and size of the trapped substance, the doctor can prescribe more gentle methods of therapy, which are based on removing the object with drugs with an enveloping effect, rinsing with furatsilin and diet. If conservative treatment is ineffective, the doctor may prescribe endoscopy, which is based on removing the body with a fibroesophagoscope. Endoscopy is performed under anesthesia, in adults - under local anesthesia, and in children - under general anesthesia. The patient is administered drugs that relax the skeletal muscles, which reduce motor activity, and then the foreign body is removed.
Causes
The reasons for the entry of a foreign body can be very unusual. However, in most cases, the culprit is a person’s carelessness and carelessness during certain manipulations. So, a foreign object in the esophagus may appear in the following case:
- Chewing and swallowing food quickly. This reason is the most common and frequently encountered. Constant rushing and swallowing virtually unchewed food leads to a person simply choking. In such cases, urgent help is necessary, otherwise asphyxia is likely to occur.
- The presence of foreign objects directly in prepared food. Chewing thoroughly will protect you from possible negligence of the people who sold you the food. In store-bought food, such as pizza, sushi, and hamburgers, you can find buttons, wood chips, and pieces of wire that can cause significant harm to your health. As for pizza, be especially careful when purchasing seafood mix, as it may contain whole shards of shellfish.
- Swallowing removable jaw. Usually seen in elderly patients. This absurdity occurs due to the unreliable fixation of the denture.
- Careless handling of small tools and parts. Failure to comply with safety standards for handling working tools can easily lead to ingestion of foreign objects, and then to suffocation.
Important: A foreign object getting stuck in the esophagus can occur not only through the fault of the person himself. In some cases, there may be diseases that provoke certain phenomena, which in turn prevent the normal passage of food through the esophagus.
Foreign body removal
A foreign object that has entered the esophagus needs urgent removal. Removal is carried out surgically and by endoscopy. Before removing the object that has entered the organ, you should study its nature and adherence to the walls, confirm or exclude damage to the esophagus. If the body does not pose a threat to the organ and the patient, and is small in size, it can be removed in a more gentle conservative way, which is based on the use of enveloping anesthetics, sulfonamides and antibiotics. The patient is given local rinsing with a solution of furatsilin and prescribed a diet.
The endoscopic method using an esophagoscope is based on the administration of a muscle relaxant and tracheal intubation. The procedure is carried out as follows: the doctor, visually examining what is happening, grabs the foreign object with forceps and carefully removes it separately or immediately with an endoscope. When the extraction is completed, the patient is prescribed a control contrast radiography, which will reveal signs of possible penetration of the walls of the organ.
If a minor organ injury is detected, the patient is prescribed antibiotics, a therapeutic diet, and rinsing of the perforation. When it is not possible to remove a foreign object with an esophagoscope, conservative treatment, deep perforation is not effective and the patient experiences bleeding, doctors resort to surgery. The surgical method is used depending on the height of the location of the body in the organ and includes laparotomy, esophagotomy, aspiration, mediastinotomy and sanitation of the source of inflammation.
When the operation is performed and the foreign body is removed, the patient is prescribed drug therapy, which includes anti-inflammatory drugs, detoxification drugs and eating through a tube. After stabilizing the patient's condition, he can switch to a gentle diet.
Throat bone (fish bone)
Among cases of foreign bodies of the upper respiratory tract in the practice of an otorhinolaryngologist, fish bones are the most common. The peak demand for removal of fish bones occurs in the summer months, when the diet contains a lot of freshly caught river fish. Samara is no exception, as it is located on the Volga River.
Removing and pushing through fish bones is done at home with a crust of bread. The most common bones that get stuck are small, thin bones—the ribs. The bone gets stuck in the upper respiratory and digestive tracts when swallowed. The most favorite places for bone fixation in the pharynx are the palatine tonsils, lingual tonsil, lateral ridges, posterior palatine arches, and pyriform sinuses.
The palatine tonsils become a target for fish bones, since they actively accompany the bolus of food at the moment of swallowing. The lingual tonsil suffers for the same reasons. The tissue of the palatine and lingual tonsils is represented by lymphadenoid tissue, which is very loose and easily threaded onto a thin fish bone. Concomitant pathology in the form of chronic tonsillitis with hypertrophy of the tonsils increases the risk of bone entering the tissue.
In the case where the bone is stuck in the upper parts of the pharynx and is in the line of sight, removing the fish bone in such a situation is not difficult. The situation with bone fixation in the lower parts of the pharynx requires the participation of a specialist. It is extremely difficult to remove such a bone without the help of an otolaryngologist.
Complications of pharyngeal trauma caused by fish bones are rare. This form of sore throat is classified as traumatic; if the bone remains in the tonsil tissue for a long time, paratonsillitis can develop, which will end in a peritonsillar abscess. Acute pharyngitis, lateropharyngeal abscess, mediastinitis, phlegmon of the pharynx, neck, sepsis, laryngeal stenosis as a complication are quite rare.
Removal of fish bones in Samara is performed by ENT doctors at Outpatient Center No. 1. First aid. During pharyngoscopy, you should carefully examine the palatine tonsils, moving away the palatine arches; with indirect laryngoscopy, you should carefully examine the root of the tongue, the vallecula of the tongue, and pear-shaped pouches. Finger examination is allowed.
The foreign body is removed with a forceps or tweezers under visual control, after which it is recommended to rinse the oropharynx with an antiseptic solution and adhere to a gentle diet. If the foreign bodies are located in a different location in the pharynx, the patient should be urgently hospitalized in the otorhinolaryngology department.
Specialized assistance. Foreign bodies of the lingual tonsil, vallecula of the tongue root and pyriform pouches are removed during indirect laryngoscopy in adults and direct hypopharyngoscopy in children using a laryngeal forceps or forceps. Anti-inflammatory therapy is prescribed. If a foreign body is not detected in the pharynx, and the pain syndrome persists, it is necessary to exclude a foreign body of the esophagus. For this purpose, fibrohypopharyngoscopy and esophagoscopy are performed.
Complication
A foreign object entering the esophagus can cause serious complications in the form of mediastinitis, paresis, perforation of an organ with damage to the heart, trachea and bronchi, periesophagitis, bleeding, pericardium and paralysis of the nerves in the lower larynx. The developing process of inflammation is accompanied by high body temperature, severe pain and swelling in the cervical region. When diagnosing a body lodged in the esophagus, the doctor sends the patient to an otolaryngologist, who will clarify the diagnosis and location of the stuck object, remove it from the organ and prescribe appropriate preventive measures that will prevent the patient’s condition from worsening.
Psychological cause of the symptom
When a symptom such as a lump in the esophagus appears, the causes, treatment and grounds for a thorough diagnosis of which are explained above, one cannot ignore any manifestations of diseases of the digestive, endocrine, lymphatic, cardiovascular and respiratory systems. And often modern research methods cannot identify a disease that can cause such a complaint. In this case, when serious diseases have been excluded, it makes sense to look for the cause of the lump in the throat in the patient’s psyche.
Chronic social stress, disturbances in the patient's adaptation to work and life conditions, as well as the loss of loved ones, failures in relationships or business - all this can, due to autonomic reactions, cause discomfort in the esophagus. The so-called lump in the throat, which comes in moments of strong disgust, resentment, irritation, when a person, feeling powerless, wants to burst into tears and give up, should be discussed with a psychologist. But this must be done either after excluding serious somatic diseases, or simultaneously with their diagnosis.
Prevention
To avoid foreign bodies entering the esophagus, people should be attentive to their health, namely: do not rush while eating and do not talk, chew food thoroughly and be careful when preparing food. If you have dentures, you should ensure they are securely fixed and do not leave dentures in the mouth overnight. You should not put small foreign objects in your mouth and supervise children so that they do not play or put small toys in their mouths.
Causes
Factors influencing the entry of foreign bodies and large pieces of food into the esophagus are internal diseases, household negligence, and non-compliance with food consumption rules. The reasons for the retention of foreign bodies include: internal and external.
Internal:
- strictures;
- burns of the mucous membrane;
- rachiocampsis;
- diverticula;
- decreased motor function;
- the presence of worms;
- benign and malignant tumors.
External:
- fast, hasty swallowing of food;
- poor quality of chewing food;
- conversation, laughter when eating foods;
- poor quality cooking.
A foreign body in the esophagus in children is observed quite often. This is due to the ability of a small child to experience the world through touch and taste. Therefore, if not properly supervised, children may swallow large or small parts. There are cases of poorly secured dentures getting into the pharynx in older people. Retention of objects is observed in people of certain professions due to the habit of constantly holding essential things in their mouths: seamstresses, tailors, shoemakers, hairdressers, carpenters. Special swallowing of difficult-to-pass objects is associated with mental and nervous disorders.
Health care
If the methods described above do not help, you should go to the doctor. At the hospital, they will first induce vomiting to try to push the lump out. Next, the person is fully examined to understand why food is getting stuck in the esophagus.
Examination methods include radiography and endoscopy. The first method is needed to determine in which part of the esophagus the foreign body is located. Endoscopy allows the doctor to assess the condition of the mucous membrane. If food does not pass due to the presence of tumors, then using this device you can take tissue for a biopsy.
Note! Quite often, if food does not pass and causes pain, this may mean the presence of a pathology called achalasia cardia. That is, when the migration of food into the stomach is impaired.
And also if food regularly gets stuck in the esophagus, then there may be other pathological reasons for this:
- tumor formations in the esophagus;
- esophageal stenosis;
- atony;
- esophagitis of an infectious nature;
- chemical burn.
In such cases, a person needs serious treatment, since these pathologies can lead to negative consequences. In all these conditions there will be pain or discomfort behind the sternum. In some pathologies, pain spreads to the neck or arm.
Neuroses also lead to the sensation of a lump in the esophagus. When a person is stressed, blood pressure rises, and as a result, the mucous membrane swells. In this state, a person wants to eat, and food passes through a narrow hole. This is also characterized by food getting caught in loose tonsils and the walls of the esophagus. As a result, discomfort appears, which a person may mistake for a lump of food. For this reason, the person is fully examined, and it is especially important to prescribe a psychiatrist. These will be sedative medications.
Treatment methods for dysphagia
The selection of treatment methods is carried out only by the attending physician after conducting the necessary examination.
Treatment of dysphagia is aimed at eliminating the underlying disease
Treatment of dysphagia should be aimed at eliminating the cause that causes disruption of the passage of the food bolus through the esophagus. For this, both therapeutic and surgical methods can be used. In cases of true dysphagia and reflux of food into the respiratory tract, emergency medical care is necessary, which consists of removing food particles from the trachea and bronchi, as well as their sanitation, and providing nutrition to the patient through a tube. It is very important to prevent aspiration pneumonia in such cases.
Every patient should be able to change their diet. You should eat soft, easily digestible foods, such as steamed or boiled vegetables, lean poultry or fish. It is necessary to completely exclude from the diet all fatty, spicy, hot foods, as well as any fast food that can cause irritation of the mucous membranes and their damage. Also, all patients are advised to stop drinking alcoholic beverages and smoking tobacco.
Patients with dysphagia are advised to give up bad habits
It is recommended to adhere to certain dietary recommendations:
- Small meals are required: small meals 5-6 times a day.
- Food should always be soft and chewed thoroughly.
- You need to wash down your food with one or two glasses of clean water.
- After eating, maintain an upright body position for 2 hours and during this period refrain from performing physical activity.
For dysphagia caused by peptic ulcer and reflux of gastric juice into the esophagus, it is recommended to use the following groups of drugs:
- Enveloping agents (Phosphalugel, Maalox), which create a protective film on the surface of the mucous membranes and neutralize hydrochloric acid, reducing the aggressiveness of the stomach contents.
- Drugs that reduce the secretion of hydrochloric acid (Rabeprazole, Omez, Ranitidine) reduce the acidity of gastric juice.
- Prokinetics accelerate the passage of the bolus of food through the esophagus and stomach, preventing the development of reflux.
Medicines that stimulate gastrointestinal motility
The correct selection of medications and their administration should be carried out under the supervision of the attending physician.
For some diseases, surgical treatment is indicated for patients with dysphagia. A similar approach is used to treat tumors such as squamous cell carcinoma of the esophagus and adenocarcinoma. Only radical removal of cancer can improve the prognosis of the patient's life expectancy and quality of life.
Surgery is also necessary for esophageal hernias, since medications can only hide the symptoms, but do not affect the very cause of their appearance. For this purpose, surgical treatment is carried out aimed at restoring the correct location of the abdominal organs and strengthening the esophageal opening of the diaphragm.
Dysphagia is a symptom that may appear periodically and not cause serious discomfort. However, everyone needs to remember that dangerous diseases such as tumors are sometimes hidden behind them. Therefore, if swallowing problems and heartburn occur, you should always seek professional medical help.
While eating, it may happen that a large piece gets stuck in the throat due to poor chewing, or swallowing foreign objects may occur accidentally. In such cases, if help is not provided, the person experiences discomfort, pain, etc. Everyone should know what to do in such a situation.
Medical care for a foreign body in a child’s digestive system
At the medical clinic, the child will be examined by experienced pediatricians and surgeons, and if necessary, an x-ray, additional ultrasound or endoscopic examination will be prescribed.
Based on the results of these studies, it is possible to establish an accurate diagnosis and determine the location of the foreign body.
- To remove it from the body, a laxative is used.
- If a foreign body that has entered the child’s body moves with difficulty, then the attending physician will prescribe an endoscopy.
- If endoscopy is not practical, surgery or laparoscopy is prescribed, but this is too traumatic for the baby and often causes complications.
Why children swallow foreign objects - the main reasons
Pediatric surgeons often discover foreign bodies in toddlers, and doctors add to the collections of their own museums by removing them. Statistics show that almost every fourth child from one to six years old has swallowed small objects, causing their parents to worry a lot.
Children between one and three years of age are more likely to swallow objects.
Exploring the world, the child goes through the “oral stage ,” and at this stage of development he studies various objects according to their shape, tastes, and properties. And parents need to monitor the safety of this knowledge, constantly watch the child’s play, what he picks up and then puts into his mouth. For your baby to play, you need to choose large objects that have a safe surface.
But there are situations when it is difficult to keep track of a child, or adults are distracted and forgetful.
While playing, the baby may become interested in some foreign object that catches his eye. But objects differ in shape, size, and surface type - this affects whether they pose a danger to children.
Causes of pain in the esophagus
Painful sensations can occur in the esophagus for various reasons. Different pathologies have their own characteristics, and therefore the treatment is different in each case. A comprehensive diagnosis will make it possible to find out what caused the patient’s discomfort.
Esophageal rupture
This pathology can be traumatic or spontaneous, but the latter type is rare (2-3% of cases). Traumatic injury may be caused by blunt trauma to the chest, neck, or abdomen, or as a result of surgery or an endoscopic procedure. Spontaneous rupture can be caused by the following factors:
- excess alcohol consumption;
- overeating;
- vomit;
- tense abdominal muscles;
- diaphragmatic contraction, compression of the muscular lining of the stomach.
Pressure increases in the esophagus, tearing its walls. Pain usually occurs after a traumatic event and manifests itself abruptly. Often irradiation into the lower back or shoulder girdle area. There are other signs of organ rupture:
- rapid pulse;
- difficulty and shallowness of breathing;
- skin cyanosis (blue discoloration);
- cold sweat.
With the progression of inflammation affecting the mediastinum with the abdominal cavity, the patient's condition worsens to a critical situation. This manifests itself in tachycardia, shortness of breath, fever, intoxication and shock.
The location of the esophageal rupture affects other organs. This leads to various diseases - pyothorax, mediastinitis, peritonitis, phlegmon.
Foreign body
A frequent source of pain in the esophagus is the entry of foreign bodies into it. It could be a bone, a coin, a button. Such objects enter the esophagus for various reasons. Sometimes it is the habit of holding small objects in the mouth, for example, pins, needles, nails. Foreign objects often get caught in food and are swallowed due to inattention, haste, or insufficient chewing. Another reason is childhood or mental problems.
Due to the entry of a foreign object, painful sensations are localized behind the sternum, increasing with swallowing. The pain is pressing. Salivation increases, the act of swallowing is disrupted (dysphagia). Over time, your general condition may worsen. If a foreign object remains in the organ, the mediastinum may become inflamed (mediastinitis).
Esophagitis
This pathology means inflammation of the esophageal mucosa. The disease can be acute or chronic. It is most often caused by gastrointestinal reflux, when stomach contents enter the esophagus. The disease can also cause chemical burns, physical injury, or infection.
Swallowing may be difficult or painful. The patient feels as if something is stuck in the throat. The mouth hurts, heartburn, nausea and vomiting begins.
Gastroesophageal reflux disease
This pathology is chronic and recurrent. It means the reflux of gastric or duodenal contents into the esophagus. This phenomenon is called gastroesophageal reflux.
The first manifestation of the disease is heartburn and sour regurgitation. Typically these symptoms appear after eating, bending the body forward and at night. Pain is in second place in terms of occurrence. Painful sensations can be transmitted to the area between the shoulder blades, neck, left side of the chest and lower jaw.
It is not uncommon for such a pathology to have additional symptoms that are extraesophageal. The disease is manifested by shortness of breath, cough, dry throat, hoarseness, and a white coating on the tongue. From the side of the stomach, rapid saturation indicates pathology. The patient becomes bloated, feels nauseous, and begins vomiting.
Diaphragmatic hernia
The transitional area from the chest cavity to the abdominal region for the esophagus is the diaphragm. When the esophageal opening is affected by the displacement of some organs into the sternum cavity, a hernia is diagnosed.
A diaphragmatic hiatal hernia occurs due to increased elasticity of the tissues, ligaments or pedicles necessary to limit the esophageal opening. The pathology can be congenital, but in most patients it is acquired during life. The provoking factor may lie in obesity, excessive physical labor, constant coughing, frequent vomiting and other factors that increase intra-abdominal pressure.
The onset of the disease is characterized by periodic displacement of organs, but then it becomes more frequent or becomes permanent. In addition to chest pain, the patient suffers from heartburn, which worsens during physical activity and in a horizontal position. After eating, shortness of breath begins and the heart rate increases. Symptoms depend on which organs are affected by the pathology.
Esophageal tumors
Neoplasms of this organ can be benign or malignant. In the second case, cancer is diagnosed.
The presence of a tumor is accompanied by moderately intense dull pain. It usually worsens with eating. Other symptoms also appear:
- The act of swallowing is impaired. As the tumor grows, the patient has difficulty swallowing solid food, and then even liquids have difficulty passing through. With benign neoplasms, the progress of dysphagia is slowed down.
- Sensation of a foreign object in the esophagus.
- Arrhythmia and increased heart rate. Such manifestations are characteristic of tumors localized in the thoracic part of the organ.
- Shortness of breath, cough.
- A bluish tint to the skin (cyanosis).
- Heartburn.
- Increased salivation.
- Belching. The patient may vomit both air and eaten food.
- Fatigue, weakness.
- Dizziness.
- Weight loss. The cause is usually dysphagia.
The main method of treatment is surgery. Radiation and chemotherapy are also important in the fight against cancer.
Diverticula
Pain in the esophagus can occur with diverticula - sac-like protrusions of its walls. The thoracic part of the organ is most often affected. At risk are people over 50 years of age who have pathologies of other organs of the digestive system. Mostly (90% of cases) diverticula are single.
Symptoms depend on the location of the process. Pain behind the sternum is characteristic of damage to the middle section of the esophagus. The patient suffers from dysphagia, nausea, night cough, and regurgitates undigested food.
Pathologies in the upper part of the organ are characterized by dysphagia, sensation of a foreign object in the throat or sore throat, nausea, and drooling. The voice often changes and a dry cough begins.
If the lower part of the esophagus is damaged, the pain radiates to the heart. The heart rate increases, shortness of breath and bronchospasms begin.
Bile reflux into the esophagus
Nature intends that food passes through the esophagus into the stomach and then into the intestines. Food, including its remains, does not return due to the sphincter. It can change pathologically when bile is released. As a result, bile refluxes into the esophagus.
There are several possible causes of the pathology. This could be a hernia, injury, neoplasm, pregnancy, poor diet or bad habits. Obesity, bloating, and ascites (abdominal dropsy) can provoke disorders.
The patient experiences pain while swallowing and passing food through the esophagus. There is often a feeling as if something is stuck in the throat, so a foreign body is suspected. The pathology also manifests itself with other symptoms:
- belching;
- heartburn;
- hiccups;
- nausea;
- dizziness.
The upward reflux of bile (reflux) can cause angina and disrupt the functioning of the heart. Reflux begins after eating and does not depend on stress or physical activity.
Chalasia and achalasia
Possible provocateurs of painful sensations are chalazia and achalasia of the esophagus. Both pathologies mean impaired functionality of the digestive system, but differ in their manifestations. Read more about the causes, symptoms and treatment of these diseases in this article.
Chalazia means that the sphincter's ability to close is impaired. Due to this pathology, the patient suffers from gastroesophageal reflux and esophagitis.
Achalasia is a neuromuscular disorder. The pathology is chronic and means a violation of the normal opening of the cardia during meals. Alahazia reduces the tone of the digestive organs, provoking a gag reflex and making it difficult to pass food of any hardness and consistency.
Symptoms of both diseases include severe heartburn leading to vomiting. The patient experiences a dull pain in the epigastric or solar plexus area.
Painful sensations are one of the main manifestations. They are caused by contractions of the muscles of the organ, which occur sharply during sleep, after overwork or stress. The pain can be controlled with medication or goes away when the patient eats or drinks water.
Another important sign is dysphagia. There is pain when swallowing food. It can be dull or sharp and is localized in the sternum. Dysphagia often appears after an emotional outburst - anxiety, stress, depression or apathy.
Regurgitation is also possible. The muscles of the esophagus contract painfully and abruptly, so the reflux of undigested contents occurs not only into the esophagus, but also into the mouth. This provokes heartburn, regurgitation or vomiting.
Portal hypertension
This disease can cause pain in the esophagus. The provocateur of this syndrome is a violation of blood flow in the portal vein basin with increased blood pressure. Subsequently, the normal functioning of the stomach is disrupted, varicose veins develop in the esophagus and stomach, ascites, splenomegaly (the spleen pathologically increases in size), and gastrointestinal bleeding begin.
A dangerous manifestation of the disease is bleeding from the veins of the esophagus, rectum and stomach. This occurs due to changes in varicose veins.
Pain with portal hypertension affects the epigastrium, iliac region and right hypochondrium. The patient loses his appetite, becomes weak, loses weight sharply, and feels sick. The stomach feels full and flatulence increases. The stool is unstable - this can manifest itself as both constipation and diarrhea. Possible jaundice and increased abdominal volume.
Hepatitis C and cirrhosis of the liver
Pain in the esophagus can be one of the complications of hepatitis C. They expand, and tortuosity begins. Due to the thinning of the vein walls, massive bleeding may occur.
Varicose veins of the esophagus do not appear immediately. Sometimes the disease has no symptoms for years. The main manifestations of pathology include:
- disturbances in swallowing food;
- heaviness in the chest;
- heartburn.
Typically, these symptoms indicate inflammation of the esophagus - esophagitis. It often accompanies varicose veins of this organ.
Important! In case of pathologies of any digestive organs, it is important not to ignore doctor’s consultations and prescribed diagnostic tests. Different elements of the digestive system interact closely, so some diseases can spread to other organs.
Cardiospasm
This pathology is typical for people 20-40 years old. It means a spasm of the cardia. The root cause of the disease is unclear, but it is caused by impaired functionality of the vagus nerve. It is he who is responsible for the opening of the sphincter and peristaltic activity.
Pain in the esophagus during cardiospasm can be constant or paroxysmal. It occurs in the area of the xiphoid process (sternum) and can radiate to the cervical spine or heart.
Pathology usually begins with dysphagia. It can develop gradually or occur suddenly. Most patients find it easier to swallow warm, liquid foods, although some people prefer solid foods.
With cardiospasm, swallowed food is delayed and does not immediately enter the stomach. As a result, the esophagus expands above the cardia. Stagnant food masses are regurgitated and can therefore enter the respiratory tract. The consequences are very serious - pneumonia, abscess. Due to a decrease in the volume of food and liquid entering the stomach, the patient may become severely exhausted.
Esophageal tuberculosis
Cutting in the esophagus with this pathology is usually provoked by ulceration of the mucous membrane of the organ. One of the clearest indicators of the disease is dysphagia.
Pain when swallowing appears due to ulcers, and a burning sensation may also occur during swallowing. There are no unpleasant sensations in the interval between swallowing food.
If tuberculosis occurs in a sclerotic form, then the patient’s general condition worsens, and dysphagia becomes more pronounced. The loss of strength is explained by the impossibility of proper nutrition.
Progressive ulceration of the organ sharply disrupts the swallowing act, and severe unexpected pain occurs. They often appear at night and are not relieved by conventional analgesics. The pain can radiate to the ear (sometimes to both at once), behind the sternum it is expressed in a burning sensation that intensifies when swallowing.
Dyskinesia
This pathology is another possible provoking factor for esophageal pain. Dyskinesia means impaired motor functionality of the esophagus, that is, food moves into the stomach differently, but there is no damage to the organ.
Painful sensations are caused by concomitant dysphagia. The patient, having finished eating, feels heaviness in the epigastrium, and gastroesophageal reflux occurs. The contents of the esophagus or stomach can penetrate the respiratory system, causing chronic bronchitis or pneumonia.
With hypermotor dyskinesia, pain may radiate to the shoulder blade, left arm, or left side of the chest. With such symptoms, diagnosis must be differentiated, since they resemble myocardial infarction or cardiac ischemia.
With neurosis or hysteria, a spasm occurs in the lower esophagus. This is a common cause of a lump in the throat.
Esophagospasm
This pathology is also called diffuse spasm. The disease refers to esophageal dyskinesia. The smooth muscles of the organ are subject to spasms, but the cardiac sphincter remains in normal tone and reflexively opens during swallowing.
Smooth muscle spasms cause chest pain. It can occur outside or during a meal. Even swallowing saliva can cause discomfort. Discomfort increases under stress.
Dysphagia occurs after meals of any consistency, although in some cases it is caused only by solid foods. In many patients, dysphagia is not a constant symptom.
Ulcer
An esophageal ulcer is usually accompanied by a similar pathology of the stomach or intestines. A single manifestation of such a disease is diagnosed tens of times less often.
The reason most often lies in the insufficiency of the cardiac sphincter accompanied by gastroesophageal reflux. The disease can also be caused by a tumor, radiation therapy, or certain medications.
Symptoms of an ulcer are usually quite striking. The disease is accompanied by:
- pain behind the sternum;
- dysphagia;
- heartburn;
- vomiting;
- weight loss.
Painful sensations occur after eating and are usually localized in the area of the xiphoid process or epigastrium (less commonly). Motility of the esophagus is inhibited, swelling occurs, causing swallowing problems.
If the disease is prolonged, the patient regurgitates the food he has just eaten. Due to weight loss, general exhaustion begins. Complications such as perforation into the pleural or abdominal cavity are possible.
What measures should be taken in this case?
If a bone is stuck in the esophagus, you can use age-old, proven methods for removing the bone at home:
- Ingest products with a viscous consistency, such as kefir , mashed potatoes or yogurt . These products can push bone into the esophagus, but only if the bone is not stuck too deep in the tissue. You can also use products with a soft texture (marshmallows, bananas), which will envelop the bone and it will not be able to continue to harm the integrity of the mucous membrane.
- Swallowing a piece of stale rye bread is perhaps the most common method for pushing bone down the esophagus. However, the danger of this method is that a piece of bread can break the bone and plunge it even deeper into the tissue.
- Slowly drink honey, preferably liquid consistency. In this case, it is necessary to be active with the swallowing muscles. This method is very effective if food is stuck in the esophagus.
- Ingest a couple of tablespoons of vegetable or olive oil , so that the bone can slip out and travel further along the digestive tract.
- Vomiting will help dislodge the stuck bone from the tissues of the larynx. You need to induce vomiting by gently pressing on the root of the tongue.
- You can try to remove the bone using a small piece of gauze wrapped around your finger. You need to carefully run your finger and gauze over the supposed place of the jam, as a result of which the foreign body can get caught in the fabric and get out.
- You can eliminate the feeling of food stuck in the esophagus by causing a severe sneezing attack. If you smell black pepper, the effect will not take long to appear. When sneezing, dynamic muscle contraction occurs, which promotes bone rejection.
- If the stuck bone is clearly visible, you can use a mechanical extraction method - tweezers . It must first be disinfected with an antimicrobial substance, such as alcohol. The procedure should be carried out in good lighting, gently pressing down on the tongue with a spoon. Can a pill get stuck in the esophagus? Such cases are not uncommon, and this is observed in the upper, cervical part of the esophagus, where it has a physiological narrowing. If a tablet gets stuck in the esophagus, what should you do? There is no need to panic, since any medicinal pill intended for oral administration tends to dissolve within 30 minutes. If the patient has impaired swallowing function and needs to take pills constantly, it is recommended to grind them to a powder consistency and wash them down with water before taking them.
What to do if the tablet is stuck in the esophageal tube and does not want to leave its confines?
- first of all, do not panic: during times of fear and fright, a spasm of the muscles of the larynx occurs, which will aggravate the situation;
- drink a few mugs of warm water or tea - plenty of warm drink will neutralize the spasm and soften the tablet;
- perform smooth, circular movements with your neck, while constantly swallowing saliva;
- take a small piece of boiled potato and swallow it, if possible;
- A gentle cough can also push the tablet through if it is not deep.
What to do if food is stuck in the esophagus and remains there for a long time?
In this case, severe complications may develop, such as necrosis of the mucous membrane, bedsores , ulcers and inflammatory processes (esophagitis). It is important to understand that the entry of a foreign object or food stagnation inside the esophageal tube is directly related to injury to the esophagus and the development of serious pathologies.
If you suspect the presence of a foreign body in the esophagus, it is recommended to immediately contact a specialized medical institution to make an accurate diagnosis and promptly remove the object from the body.