If you have recently been diagnosed Crohn's disease, most likely, you have not thought about the impact it can have on other body systems besides the intestines. The main symptoms of this disease are abdominal pain and diarrhea. Crohn's disease most often affects the ileum, which is the lower part of the small intestine, coming after the jejunum and before the upper part of the large intestine. But the inflammation can subsequently spread to other places, including the eyes, skin and joints.
Types of Crohn's disease
The disease was described by BB Crohn and GD Oppenheimer in 1932. Nonspecific inflammation occurs in the submucosa and subsequently spreads to the mucous membrane and the entire intestinal wall. The inflammatory process is segmental in nature - the affected segments alternate with unaffected ones.
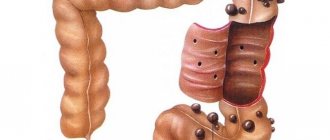
Depending on the location of the pathological process, two types of Crohn's disease are distinguished:
Type 1:
- the lesion is limited to one segment of the small intestine;
- the ileocecal region is affected;
- the lesion is limited to a segment of the colon.
Type 2:
- segments of both the small and large intestines are affected;
- there is a combination of intestinal damage to the stomach, esophagus or oral mucosa,
- granulomatous inflammation of the appendix (appendix) is also possible.
Mouth ulcers
People with Crohn's disease may develop mouth ulcers, also known as canker sores. These sores can appear on the gums and lower lip, as well as on the sides of the mouth and at the base of the tongue. Dr. Chang says patients sometimes experience ulcer flare-ups during a flare-up. “The best way to treat these symptoms is with Crohn's disease treatment because other treatments for ulcers only provide short-term relief,” says Dr. Chang. Some doctors prescribe mouthwash to suppress infection and multivitamins to help correct nutritional deficiencies.
Causes
The cause of the disease is unknown. At different times, several hypotheses were put forward, including immunological and infectious. The role of viruses, chlamydia and bacteria, especially mycobacteria, has been suggested.
Observations show that dietary supplements and lack of fiber in foods play a role in the increased incidence of Crohn's disease.
However, none of these hypotheses have been proven. A family predisposition to the disease is observed in approximately 20% of patients, which suggests the influence of genetic factors.
The first stage of diagnosis is questioning the patient
People meet with a specialist at a doctor’s appointment; they come with their health complaints, suspicions, doubts, “secrets” that are impossible to talk about with others. Since Crohn's disease is part of the class of inflammatory bowel diseases, there are common symptoms. They will have to be clarified when interviewing the patient.
Meaning:
- loss of appetite;
- the appearance of stomatitis with mouth ulcers;
- skin rashes;
- weight loss;
- acute and dull abdominal pain associated with food or stress;
- diarrhea or constipation, the presence of visible mucus, pus, and blood in the stool.
It is necessary to find out whether among blood relatives there were cases of diseases similar to Crohn's disease, possibly with a fatal outcome. These signs are not accurate criteria for Crohn's disease, but help in developing a differential diagnosis plan.
Development of the disease
The earliest microscopic sign of damage in Crohn's disease is a tiny ulceration of the mucous membrane (aphtha). The inflammatory process gradually spreads to all layers of the intestinal wall and is especially pronounced in the submucosa, where infiltrates (granulomas) are formed.
Granulomas consist of clusters of lymphocytes, in the center of which single giant cells of the Pirogov-Langhans type can be found. Unlike tuberculous granulomas, Crohn's disease never develops foci of caseous necrosis.
Infiltration extends to both the mucous and serous membranes of the intestinal wall. As a result, the intestinal wall becomes dense, the mucous membrane acquires relief, and multiple erosions and ulcers like cracks are formed on its surface, penetrating the entire intestinal wall. Sometimes ulcers perforate, which leads to the formation of intestinal fistulas. Scar changes in the wall can lead to a narrowing of the intestinal lumen, the development of partial and even complete intestinal obstruction.
The relief of the mucous membrane often takes on a peculiar cobblestone appearance due to infiltration of the intestinal wall with lymphoid cells and its intersection with deep cracks and linear ulcers.
The main feature of the histological picture of Crohn's disease is a typical transmural lesion of the intestinal wall. Inflammation can spread to the serosa and adjacent tissues and organs, forming fistulas and adhesions.
Another characteristic feature of the disease is the formation of non-caseating sarcoid-like epithelioid granulomas with Pirogov-Langhans cells.
Granulomas are found in approximately 30-40% of cases during histological examination of biopsy material. When examining surgical material, granulomas are found much more often, including in the mesenteric lymph nodes.
The presence of granulomas is characteristic of Crohn's disease, but their absence does not provide grounds for its exclusion. Histological examination allows us to see pronounced infiltration of the lamina propria of the mucous membrane and submucosa with lymphoid cells, thick-walled vessels with symptoms of vasculitis.
The process may involve the mesentery, which becomes swollen and thickened. The mesenteric lymph nodes are enlarged and contain large numbers of inflammatory cells, indicating chronic inflammation. Transmural inflammation, deep ulcers, edema and fibrotic changes in the intestinal wall create conditions for obstruction, fistulas and abscesses.
The affected segments of the small intestine are sharply demarcated from adjacent normal intestinal loops, corresponding to the concept of “regional enteritis.”
The pathological process in Crohn's disease is most often located in the terminal part of the small intestine (ileocecal region), although it can be located in any part of the digestive tract - from the oral cavity to the anus.
Isolated damage to the ileum is observed in approximately 35% of cases, the ileum and colon - in 45%; Crohn's disease of the colon occurs in approximately 20%.
Isolated damage to the anorectal area is observed in only 3% of patients.
Symptoms
Symptoms of Crohn's disease in adults and children are very diverse. There is no single evidence-based set of clinical signs. Patients visit different specialists to treat their symptoms.
Regarding aphthous stomatitis - see a dentist, a therapist with unknown abdominal pain, or a proctologist with a lesion in the anal area (fistula, fissures, abscess formation). There are intestinal and extraintestinal symptoms. It depends on the localization of the process, the severity of the course, the frequency of relapses, and the form of inflammation.
Intestinal signs include:
- prolonged diarrhea (considered chronic if it lasts more than 6 weeks);
- abdominal pain - worse after eating;
- nausea, vomiting;
- flatulence;
- weight loss - first supported by refusal to eat due to fear of pain, then by malabsorption syndrome against the background of a widespread process.
Pain can be disguised as acute appendicitis if localized in the iliac region on the right
Symptoms of the general condition:
- lack of appetite;
- increased fatigue, constant fatigue;
- temperature rise of a wave-like nature.
The fistula form is manifested by: non-healing anal fissures, rectal fistulas. The correct diagnosis is made after unsuccessful use of medications and surgery for another reason.
Symptoms of Crohn's disease of the colon are often accompanied by high body temperature. Damage to the small intestine is indicated by the patient's sudden weight loss, impaired absorption of proteins, fats and carbohydrates, loss of vitamins (especially A, D, B12) with signs of hypovitaminosis, severe steatorrhea (fatty feces).
Extraintestinal signs
The course of the disease is characterized by the involvement of various organs and systems in the pathological process. How inflammation is transmitted from the intestine is unknown.
In the oral cavity, aphthous stomatitis is detected with painful bleeding ulcers, pain when eating
The eyes react with diseases of the membranes: conjunctivitis, uveitis, keratitis. Damage to the joints is characterized by inflammation of one (monoarthritis) with pain, redness, swelling, ankylosing spondylitis of the spine with severe pain during body movements, and the development of stiffness.
The skin reveals erythema nodosum, multiple pustules, gangrenous pyoderma, and angiitis of superficial vessels are possible.
Fatty degeneration forms in the liver, subsequently cirrhosis, sclerosing cholangitis develops in the biliary tract, stagnation of bile causes the formation of stones (cholelithiasis), which can subsequently lead to a malignant tumor, cholangiocarcinoma. For kidney and urinary tract tissues, typical manifestations are: cystitis, chronic pyelonephritis, nephrolithiasis, amyloidosis, hydronephrosis.
Manifestations of varying degrees of process activity
In practice, doctors use a combination of signs of the disease to determine the degree of activity of the process.
A mild degree is characterized by:
- diarrhea no more than four times a day;
- rare presence of blood in the stool;
- temperature not higher than 37.5 degrees;
- normal pulse.
In case of moderate activity:
- diarrhea recurs more than six times a day;
- there is always blood in the stool;
- moderate tachycardia (pulse 90);
- complications are likely.
Severe degree is different:
- severe diarrhea, stool more than 10 times a day;
- massive discharge of blood in feces;
- temperature within 38 degrees;
- tachycardia above 90 per minute;
- addition of complications.
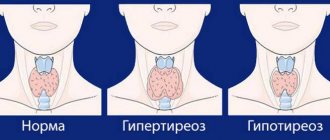
Hyperthermia is one of the signs of an acute process
Symptoms in children
Features of symptoms in children for a long time do not allow making a correct diagnosis and prescribing optimal treatment for Crohn's disease. The clinical picture is blurred, poorly expressed, diarrhea is inconsistent, and primarily extraintestinal signs are detected. Cases of illness in children are severe and are accompanied by numerous complications.
Parents and attending physicians are advised to pay attention to the following signs:
Intestinal atresia in newborns
- pain in the abdomen - a child may have different types of pain from strong cramping to dull, aching;
- nausea, vomiting - observed when the gastric mucosa is damaged;
- bloating;
- diarrhea - the more intense, the higher the prevalence of intestinal inflammation, blood clots, impurities of pus and mucus, a fatty film are possible in the stool, the color of the stool becomes lighter;
- lack of appetite, weight loss;
- an unclear elevated temperature is determined;
- in a blood test, with good nutrition, a reduced hemoglobin level is found;
- teenage girls stop having periods;
- in half of the cases, inflammation occurs in the ileocolic area, symptoms manifest themselves in the form of an “acute abdomen”, urgent observation by a surgeon is required;
- extraintestinal symptoms do not differ from those in adult patients (stomatitis, congestion in the biliary tract, perianal abscess, fissures and fistulas of the anus, joint pain).
Symptoms
The manifestations of Crohn's disease depend on the part of the intestine in which the inflammatory process develops and its severity.
General symptoms that are characteristic of all types of Crohn's disease:
- diarrhea;
- stomach ache;
- fever;
- weight loss;
- anal fissure.
Diarrhea
Diarrhea is common in all patients, but it varies.
At the height of the disease, persistent diarrhea is most typical (stools 2-3 times a day, copious, semi-formed, less often liquid, watery).
When the ileum is damaged, the absorption of bile salts is impaired, which causes increased secretion of ions and water in the colon and leads to hologenic diarrhea. If more than 100 cm of the ileum is affected, steatorrhea develops. Some patients may experience miasmas (false urge to defecate), but unlike ulcerative colitis, there may be no blood in the stool.
Abdominal pain with CD
- Most often the right lower abdomen hurts, pain occurs immediately after eating.
- In case of obstruction, the pain is strong and cramping.
- The formation of an abscess (abscess) is indicated by constant pain with fever and an increase in white blood cells.
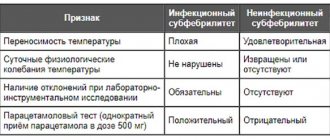
Low-grade fever and general malaise in Crohn's disease
These manifestations are characteristic of inflammatory bowel disease. A high temperature indicates an exacerbation of the process, the formation of an abscess.
Weight loss
This symptom can be very pronounced, up to extreme exhaustion of the body, general weakness, sudden weight loss, and a decrease in the activity of physiological processes.
Anal fissure
Examination of the anus and rectum often reveals
- anal fissure;
- proctitis;
- paraproctitis.
Sometimes anal fissure and paraproctitis can precede Crohn's disease or be its main manifestation. In this case, conservative treatment of these manifestations does not bring any positive results. Therefore, every case of persistent fistula or anal fissure of the rectum should be checked for the presence of Crohn's disease in the patient, including in another part of the intestine.
Joint pain
Crohn's disease is likely to cause vitamin D and calcium deficiencies, so many people with the disease may also develop osteoporosis . “When the ileum is inflamed, your body has a hard time absorbing vitamin D, and vitamin D malabsorption interferes with the absorption of calcium into the bones,” explains Ellen Scherl, MD, director of the Jill Roberts IBD Center at New York Presbyterian Hospital/Weill Cornell Medicine.
“Joint pain can be migratory, meaning it moves from one part of the body to another,” says Dr. Scherl. For example, back pain is a common complaint, but patients with Crohn's disease may also complain of stiffness in the wrists, hips, and knees. Dr. Chang recommends treating joint pain with heat, ice, and stretching, but avoiding nonsteroidal anti-inflammatory drugs, as they may affect the development of Crohn's disease in the intestines. Dr. Scherl and Dr. Chang say doctors also order x-rays to rule out the possibility of stress fractures and rheumatic diseases, which are common in patients with Crohn's disease.
Forms of the disease
Crohn's disease, which affects the intestines, has the following forms:
- acute ileitis (ileotiphlitis);
- jejunoileitis with small bowel obstruction syndrome;
- chronic jejunoileitis with malabsorption syndrome;
- granulomatous colitis;
- granulomatous proctitis.
Acute form of the disease
When acute inflammation occurs, the symptoms are similar to an exacerbation of appendicitis. Sharp pain in the right lower abdomen, fever. During laparotomy, inflammation of the ileum is detected.
If there is perforation or necrosis of the intestine, part of it is removed. In other cases, the entire intestine is inspected and the mesentery of the small intestine is infiltrated with a solution of novocaine with an antibiotic.
Stenosing form (jejunoileitis with small bowel obstruction syndrome)
Crohn's disease can last a long time with vague abdominal pain and extraintestinal symptoms (episodes of causeless fever, joint pain, erythema nodosum, etc.). The disease may remain unidentified for many years. If it begins in childhood, the child lags behind in physical and sexual development.
Over time, as intestinal obstruction increases, attacks of pain appear, more often in the right iliac region (lower right abdomen), vomiting, bloating, loud rumbling and sounds of fluid transfusion, stool and gas retention.
Visible peristalsis appears on the abdominal wall in the form of periodically rising “shafts”.
Crohn's disease with a primarily chronic course
Chronic jejunoileitis with malabsorption syndrome is manifested by symptoms of intestinal malabsorption:
- frequently recurring diarrhea;
- anemia (low hemoglobin in the blood);
- decreased protein in the blood (hypoproteinemia);
- swelling;
- fever.
The severity of pain and severity of fever depend on the degree of inflammation and intestinal obstruction.
Granulomatous colitis
This type of disease exhibits symptoms such as:
- stomach ache;
- fever;
- unshaped chair;
- mucus in stool;
- blood in stool.
Granulomatous proctitis
The main manifestations are:
- long-term non-healing anal fissures;
- anal fistulas.
If inflammation affects only the colon, then the symptoms of granulomatous colitis and proctitis may be no different from ulcerative colitis.
Crohn's disease of the appendix
Usually this disease manifests itself as an attack of acute appendicitis. The symptoms differ from appendicitis in that they are less acute and sometimes form a dense infiltrate in the lower right abdomen.
Fatigue
Another classic example of how malabsorption of nutrients can lead to Crohn's disease, fatigue and anemia is iron deficiency. “Iron deficiency can also be the result of blood loss due to active bleeding associated with colitis and anal fistulas, which are small holes or tunnels that form inside the anus and in the skin around the anus,” explains Dr. Scherl. Dr. Scherl also says that celiac disease is common in the setting of Crohn's disease, so having celiac disease may also affect how your body absorbs iron and vitamin C, which helps the body absorb iron.
Extraintestinal manifestations of Crohn's disease
Quite often this disease manifests itself with symptoms that seem to have nothing to do with intestinal inflammation. Conventionally, all manifestations can be divided into three groups.
First group: combination of extraintestinal symptoms with intestinal ones
In approximately 1/3 of patients, the intestinal symptoms described above are combined with
- joint damage (arthritis),
- inflammatory eye disease (episcleritis),
- stomatitis (inflammation of the oral mucosa),
- inflammation of the skin and subcutaneous vessels (erythema nodosum),
- skin lesions (pyoderma gangrenosum).
These same symptoms may accompany ulcerative colitis.
These diseases are related to the condition of the intestines and do not require separate treatment. Sometimes extraintestinal manifestations are the first signs of Crohn's disease and ulcerative colitis.
Second group: extraintestinal manifestations requiring special treatment
This group includes the development of Crohn's disease when, in addition to the intestines, other organs and systems are affected. For example,
- spinal lesions (ankolosing spondylitis and sacroiliitis),
- inflammation of various parts of the uvea (uveitis),
- inflammation of the bile ducts (cholangitis).
In this case, special treatment of the affected organs and systems is necessary.
Third group: malabsorption
As described above, damage to the small intestine in Crohn's disease causes disruption of absorption processes. This leads to the development of diseases such as:
- urolithiasis disease;
- cholelithiasis;
- anemia;
- blood clotting disorders.
In addition, hydronephrosis may develop as a result of compression of the urethra and urinary tract by infiltrates in the pelvis and retroperitoneum.
Dry eyes
People with Crohn's disease may be deficient in vitamin A, which is important for maintaining good vision. Because of this, many patients experience blurred vision and dry eyes, which can lead to redness, irritation and burning.
Two other common vision complications in patients with Crohn's disease are uveitis and episcleritis, according to Dr. Chang. Uveitis is an inflammation of the choroid of the eyeball - the middle layer of the eye located directly under the sclera, and episcleritis is an inflammation of the superficial layers of the eye white, or episclera.
“They [uveitis and episcleritis] can cause eye pain and inflammation, so it is important that patients see an ophthalmologist immediately if they experience these symptoms,” she says.
Extraintestinal manifestations of CD
| Related to process activity | Arthritis, osteoporosis, conjunctivitis, episcleritis, iritis, aphthous ulcers, erythema nodosum, pyoderma gangrenosum |
| Not related to process activity | Arthralgia, sacroiliitis, ankylosing spondylitis, osteomalacia, maldigestion, cholelithiasis, fatty liver, primary sclerosing cholangitis, urolithiasis, ureteral strictures, right-sided hydronephrosis, amyloidosis |
Degrees
Depending on how intense the symptoms of the disease are and how they affect the functioning of the body in general, different degrees are distinguished:
- mild Crohn's disease;
- moderate Crohn's disease;
- severe Crohn's disease.
To determine it, the following criteria are described:
- degree of diarrhea - number of trips to the toilet, presence of blood or mucus in the stool;
- Body temperature;
- weight loss;
- pulse and organ condition in blood tests;
- general state.
A mild degree is characterized by stool less than 4 times a day, in which there is no blood or mucus, body temperature is normal, and there is no loss of body weight or changes in the blood.
Moderate severity is manifested by diarrhea 4-6 times a day mixed with blood, which often prevents the patient from sleeping at night. Body temperature rises, signs of intoxication syndrome appear:
- headache;
- weakness;
- mild tachycardia;
- muscle cramps;
- changes in general blood test;
- signs of anemia appear as a result of blood loss;
- leukocytosis with a shift of the leukocyte formula to the left due to the progression of intestinal inflammation.
Severe: diarrhea with blood and mucus more than six times a day. Often there is only blood in the stool. The patient is weakened and requires urgent hospitalization. Body temperature above 38ºC degrees, tachycardia above 100 beats per minute, signs of organ failure and weight loss greater than 10%. A severe degree requires initiation of urgent resuscitation of the patient with the prescription of blood transfusions and infusion therapy, in order to avoid hypovolemic shock.
A mild degree does not require hospitalization and home therapy with oral medications is possible. Moderate and severe degrees require intravenous injections and therefore require hospitalization and treatment in a medical facility.
Can Crohn's disease be cured?
In an acute attack of Crohn's disease, recovery occurs in 95% of patients; in the rest, the disease takes a chronic form.
It is impossible to completely recover from the chronic form of Crohn's disease. Even removing part of the intestine does not guarantee a complete cure.
It is believed that the risk of cancer in patients with CD is quite high. Both domestic and foreign doctors do not have a definite opinion on this matter.
Some researchers provide evidence of a high incidence of cancer in patients with Crohn's disease.
However, most doctors argue that if such statistics exist, then the percentage of such cases is very low compared to the general statics of cancer development among the population, and life expectancy with Crohn's disease usually does not decrease.
What is Crohn's disease
Malaise, intestinal upset, stomach pain, discomfort, all this can be the cause of a rather serious disease called Crohn's disease, which can take a chronic form.
This disease also has the following synonyms: granulomatous enteritis, regional enteritis, transmural ileitis, regional terminal ileitis.
This is an inflammatory disease of a granulomatous (small nodules) nature that affects the entire digestive system, mostly partially. It develops more often in the lower parts of the small intestine, but inflammation can spread throughout all parts of the gastrointestinal tract, including the oral cavity.
In 50% of cases, damage to the large intestine is observed, as well as all the walls and layers of the esophagus, the lymph nodes become inflamed, ulcers and scars form throughout the digestive system, narrowing and deformation of internal organs occurs.
- Stomach ulcer.
Diagnostics
When making a diagnosis, a number of diseases whose symptoms and examination results are similar to CD should be excluded:
- appendicitis,
- diverticulitis,
- yersiniosis,
- intestinal tuberculosis,
- all types of infectious inflammation (salmonellosis, pseudomembranous colitis),
- ulcerative colitis,
- AIDS.
The correct diagnosis is usually established during laparotomy, X-ray examination, and irrigoscopy.
What does X-ray examination reveal?
With fluoroscopy (irrigoscopy), three stages of the disease can be established:
- Stage I (early changes). Characteristic signs are thickening and straightening of the walls due to edema; the presence of multiple superficial ulcers with a diameter of 0.1-0.2 cm, surrounded by an inflammatory shaft, unevenness, in some places, vagueness of the intestinal wall, the elasticity of the wall is preserved.
- Stage II (intermediate changes). The intestinal wall is significantly thickened, the width of the intestinal lumen is within normal limits, ulcerations, rigidity of the mesenteric edge, and nodular defects with a diameter of less than 1 cm are observed.
- Stage III (pronounced changes). As the process progresses, the leading radiological symptom becomes a narrowing of the affected area of the intestine, which takes on the appearance of a cord. Characteristic spicule-like (needle-like) projections are often found. An important sign is the shortening of the affected areas of the small and large intestine, the walls are thickened and rigid.
Other types of CD research
In recent years, multidetector CT (computed tomography) and MRI (magnetic resonance imaging) have been increasingly used to diagnose Crohn's disease. These methods allow visualization of all parts of the intestine.
The new paradigm of patient examination includes its safety as a very important aspect when assessing the role of any diagnostic method. MRI, unlike CT, does not expose the human body to ionizing radiation, and therefore is the preferred method for assessing small intestinal disease, especially in young people.
Colonoscopy is used to examine the colon and terminal ileum, extending from 10 to 30 cm.
Diagnosis and treatment of Crohn's disease
To confirm the diagnosis, blood and feces are examined, colonoscopy, computed tomography, ultrasound, endoscopy with biopsy, intestinal MRI, video capsule endoscopy, irrigoscopy, sigmoidoscopy are performed.
Uncomplicated granulosa enteritis is treated with:
- glucocorticoids – methylprednisolone, prednisolone. With long-term use of these drugs, the development of hypercortisolism and hormone dependence cannot be ruled out;
- salicylates – mesalazaline, sulfasalazine. Possible oral administration or local application (in the form of suppositories, rectal foam, suspension);
- topical steroids (budesonide);
- immunosuppressants - methotrexate, azathioprine, mercaptopurine;
- antibiotics - metronidazole, rifaximin, ciprofloxacin;
- genetically engineered drugs – adalimubab, infliximab, etanercept, golimubab.
Alternative methods include:
- oxygen treatment,
- transplantation of live bacteria from a donor,
- plasmapheresis,
- introduction of stem cells.
Severe disease requires surgical intervention. The operation does not lead to a complete recovery; its purpose is to eliminate the complications that have arisen.
Diagnosis according to the Montreal classification
Sometimes the diagnosis of Crohn's disease is recorded by doctors using the Montreal classification. In this case it looks like this:
Crohn's disease: A2; L3; IN 1.
Below is a table of these designations.
| Age at diagnosis | A1-under 16 years old, A2-from 17 to 40 years old, A3-over 40 years old |
| Localization | L1-in the ileum L2-in the colon, L3-in the ileum and colon, L4-isolated lesion of the upper gastrointestinal tract |
| Nature of the lesion | B1-non-stenotic, B2-stenotic, B3-penetrating, p-modifier, reflecting the presence of changes in the perianal area. |
Diagnostic methods
If symptoms of pathology are detected, it is necessary to consult a therapist and gastroenterologist. When it comes to a disorder such as Crohn's disease, diagnosis begins with a history and careful analysis of the patient's symptoms. An external examination reveals an increase in the volume of the abdomen. Your doctor may immediately palpate your abdomen to identify areas of tenderness or tenderness.
In addition, the specialist examines the skin and eyes. If there are symptoms of their damage, a consultation with other highly specialized specialists, including a dermatologist and ophthalmologist, is often prescribed. Blood tests are of great importance in making a diagnosis. Their implementation is scheduled first. In a blood test, in the presence of an exacerbation of the disease, an increase in ESR and the number of leukocytes is determined. A reduced hemoglobin level may also be detected.
Performing a biochemical blood test allows you to determine the presence of C-reactive protein, an increase in the level of gamma globulins and an increase in the amount of fibrinogen, since in Crohn's disease these indicators in most cases do not remain normal. Laboratory diagnostics is complemented by immunological testing. It allows you to determine the presence of specific cytoplasmic antineutrophil antibodies in the blood.
Diagnosis of this disease also involves examining the affected intestinal walls. Most often, fibrogastroduodenoscopy or colonoscopy is used to visualize the organs of the digestive tract. These studies allow tissue sampling during the intestinal examination procedure, i.e., a biopsy for further histology. The endoscopic picture for this disease is characteristic. Criteria of this type include:
- defects on the intestinal walls;
- lumpy surface relief;
- the presence of mucus and pus on the walls;
- narrowing of the lumen;
- lack of vascular pattern;
- pronounced longitudinal ulcers.
To make an accurate diagnosis, an X-ray of the abdomen is often performed to exclude the presence of complications, including perforation and toxic expansion of the colon. Irrigoscopy is often performed. This is an x-ray method for examining the intestine, which involves the use of a contrast agent. A coprogram is used to detect hidden blood in the stool in Crohn's disease.
Calculation of IABK
| Index | Number of points | Coefficient |
| Number of bowel movements with loose or soft stools within 7 days | 0-70 | x2 |
| Severity of abdominal pain over 7 days | 0-21 | x6 |
| Well-being within 7 days | 0-28 | x6 |
| number of extraintestinal manifestations | 0-3 | x30 |
| Use of opiates for diarrhea | 0-1 | x4 |
| Volumetric formations in the abdominal cavity | 0-5 | x10 |
| Severity of blood loss: Ht men - 47, women - 42 | — | 6 |
| Degree of weight loss | — | 1 |
For symptomatic assessment of the activity of the inflammatory process in CD, the Best index is used.
Treatment
Since the pathogenetic causes of the development of the pathology have not yet been clarified, the answer to the question of whether it can be cured forever still remains negative. This is a chronic disease, so it cannot be completely eliminated, but using the developed treatment protocols it is possible to achieve stable remission and reduce the risk of severe disorders and exhaustion of the body.
Pathology therapy is primarily aimed at eliminating existing symptomatic manifestations and the inflammatory process. Comprehensive treatment can make life with Crohn's disease as normal as possible.
Therapy can be carried out using both conservative and surgical methods. Pharmacological treatment involves the selection of drugs that help normalize the immune system, eliminate the inflammatory process, restore digestion and relieve existing symptomatic manifestations.
Medicines for this disease should be introduced into the treatment regimen only by the attending physician. Surgical methods are used in the presence of complications. When it comes to a disorder such as Crohn's disease, treatment is always complemented by a special diet, which must be followed strictly, since ignoring the prescribed nutritional rules often causes an exacerbation.
Drug therapy
Drugs for the treatment of the disease are selected taking into account the activity of the pathology. The treatment regimen includes drugs belonging to the following groups:
- antibiotics;
- immunosuppressants;
- antibodies to tumor necrosis factor;
- probiotics;
- corticosteroids;
- antidiarrheal;
- vitamin complexes.
First of all, corticosteroids are selected to eliminate the inflammatory process, suppress the growth of pathogenic microflora and unwanted immune activity. Among the drugs belonging to this group, Prednisolone is most often used to treat the disease. This drug is used for severe forms of the pathology and to relieve symptoms.
When the acute period is over, Azathioprine or Budesonide may be prescribed. These drugs provide the necessary immunosuppressive and anti-inflammatory effects, but have fewer side effects. Additional drugs belonging to the category of corticosteroids should be used in short courses, because over time they become less effective.
When treating Crohn's disease, immunosuppressants are often used to reduce the activity of the immune system and eliminate the inflammatory process. For the described pathological condition, a combination of two drugs belonging to this group is most often used. This makes it possible to increase the effectiveness of drugs of this type. To eliminate the disease, the following types of immunosuppressants and tumor necrosis factor antibody inhibitors are most often used:
- Tysabri.
- Humira.
- Methotrexate.
- Stelara.
- Ismigen.
Most drugs that have an immunosuppressive effect have many side effects, so they should be used strictly following the recommendations of the attending physician. If there are infectious complications of the disease or a high risk of their occurrence, antibiotics are prescribed. The most commonly used drugs in this group include:
- Ciprofloxacin.
- Metronidazole.
- Klion.
- Flagyl.
- Trichopolum.
Medicines are selected to stop the manifestations of this disease. In the presence of severe pain, non-steroidal anti-inflammatory drugs are used. In most cases, drugs such as Ibuprofen and Naproxen are used, which come in tablet form.
In addition, antidiarrheal drugs are necessarily introduced into the treatment regimen. For mild cases, Citrucel, including methylcellulose, is prescribed. In severe forms of the disease, Loperamide and Imodium are prescribed to eliminate frequent attacks of diarrhea. These drugs also have contraindications, for example, they are not recommended for use in the presence of blood in the stool.
To restore normal intestinal function, probiotics are prescribed. Drugs in this group include:
- Linux.
- Bifidumbacterin.
- Bifiform.
Considering that immunosuppressants and corticosteroids are used in the treatment of pathology, which predispose to the development of osteoporosis, patients with Crohn's disease are prescribed vitamin D and calcium supplements.
In the presence of pronounced manifestations of anemia, it is recommended to use iron supplements to replenish the existing deficiency and normalize the general condition. In addition, patients with severe signs of exhaustion are often prescribed intravenous nutrition and vitamin complexes. They allow you to achieve stable remission faster.
Surgery
Using various medications, doctors try to delay the need for surgical interventions, since for people suffering from this pathology, they are associated with the risk of developing complications. The absolute indications for surgical treatment of the disease are:
- peritonitis;
- abscess;
- perforation of the intestinal wall;
- intestinal obstruction;
- extensive bleeding;
- inflammation of the bladder.
Relative indications for surgery include: active pathology, the presence of fistula tracts, obstructions and stenoses. There are several types of surgical interventions that are performed to treat the disease. For intestinal stenosis that is not accompanied by the formation of abscesses or fistulous tracts, endoscopic intestinal dilatation is often performed. In most cases, it gives a short-term effect that lasts no more than 1 year.
If fistulas are present, they are excised to close the existing defect. When treating such a complication of Crohn's disease, minimally invasive interventions are often performed that do not involve a large incision in the abdominal wall. If bleeding is present, economical resection is most often performed, which involves removing only the most affected part of the intestine or cauterizing it.
In the presence of various types of abscesses, a minimally invasive drainage procedure is performed. If this is not enough, after the procedure a resection of the section of the intestine in which the fistulous tract is present is performed. In case of intestinal perforation and the development of peritonitis, the affected area of the organ is removed. This operation is traumatic and is performed under general anesthesia. After its implementation, long-term rehabilitation is required.
Duration and effectiveness of treatment
Treatment of the acute stage with an anti-inflammatory complex of drugs lasts 2-3 months, followed by maintenance therapy. The specific period depends on the choice of drug and the patient’s condition. For example, corticosteroids cannot be used for a long time; the negative effect is the appearance of osteoporosis, diabetes mellitus, hypertension, and intestinal bleeding.
Antibiotic therapy is allowed for no longer than two weeks. In severe cases, 2 drugs with different directions of action are prescribed to enhance the effect. Other medications are used in a minimal dose for several months or years. Replacement with drugs of the same group is carried out.
The best positive outcome of treatment is the achievement of long-term remission, when exacerbations occur 1-2 times every 20 years. Doctors note that, unfortunately, relapses occur more often in 50-78% of cases. Surgical removal of an irreversibly altered section of the intestine is a way to extend the period between relapses. 65% of patients require re-intervention in the next 5 years.
How long does it take to treat Crohn's disease?
Patients have to undergo treatment for the rest of their lives. Doses and medications are changed, but the threat of exacerbation is not removed. The main cause of death is emergency conditions that arise when ulcers break into the abdominal cavity, peritonitis, and bleeding. The risk of degeneration into a malignant tumor increases sharply.
Is it possible to completely cure the disease?
The disease cannot yet be cured. Doctors insist that patients follow a healthy regimen, stop smoking, and completely abstain from alcohol. If patients do not want to take care of their health, the frequency of relapses increases almost 3 times. And lethal outcomes are 3.5-4.8 times.
The undulating course of the disease alternates between exacerbations and remissions. In mild and moderate forms, patients do not experience signs of pathology for several months and years.
Diet
Everything a person eats passes through the intestines. If the digestive tract is inflamed and its function of absorption and digestion is impaired, it is necessary to make its work easier. The diet for Crohn's disease includes foods that are easy to digest, mostly liquid and soft foods to reduce bowel irritation.
What can you do if you have Crohn's disease?
Foods and dishes that are healthy and can be eaten with Crohn's disease, both during remission and exacerbation:
- boiled eggs, 2-3 pieces per day, you can steam an omelet;
- vegetable soups, you can use chicken or beef broth, you can add only chopped, pureed meat, with slimy porridges;
- meat cutlets, steamed only, the meat is first minced several times in a meat grinder;
- bread only in the form of crackers, slightly dried;
- liquids, like an ordinary person, 2-3 liters per day, you can have weak tea or coffee, compotes from berries or dried fruits;
- butter maximum 20 g per day;
- low-fat grated cottage cheese, without sugar;
- fruits and berries in any quantity;
- fruit jellies or jelly;
- All types of cereals are ground and well cooked.
Sometimes, about once a week, it is not forbidden to treat yourself to noodles, weak coffee, low-fat stewed or baked fish, kefir or yogurt, and stewed vegetables.
What not to do with Crohn's disease
The range of products that are strictly prohibited for Crohn's disease and that can lead to complications:
- fast food;
- fried foods;
- highly salted or peppered dishes;
- hard foods;
- strong tea or coffee;
- tobacco and alcohol.
During an exacerbation, the following are prohibited:
- dairy products;
- vegetables such as sorrel, cabbage, radishes, onions, mushrooms, spinach;
- confectionery, spices.
All prohibited products can damage the intestinal wall when passing and lead to the onset of exacerbation, perforation of ulcers, perforation and peritonitis.
Approximate menu for Crohn's disease
The diet of a patient with Crohn's disease should consist of warm liquid meals and ground foods every day. For breakfast, for example, combinations such as:
- porridge from pre-ground cereals with the addition of 10-20 grams of butter with cocoa in water;
- pureed low-fat cottage cheese with the addition of berries or dried fruits and weak green tea;
- steamed omelette and fruit jelly.
For lunch, be sure to have vegetable soup, perhaps with the addition of meat minced several times in a meat grinder; for the second course, stewed vegetables or steamed fish and, for example, fruit jelly.
Dinner is preferably light, so as not to burden the intestines at night - unsweetened yogurt with fruit or crackers and weak tea.
It is important in maintaining a diet to maintain a certain number of calories per day, not to eat large portions, but to eat small portions and often.
Anatomical changes
Most often, changes in Crohn's disease are found in the final (terminal) section of the ileum and the initial sections of the large intestine. Areas of inflammation have segmental divisions with clear boundaries. The intestinal wall thickens. Due to this, the lumen is narrowed. The diameter of the upstream section has been expanded.
Multiple ulcers in the form of longitudinal and transverse slits or cracks are visible on the mucous membrane. Anatomists call this surface “cobblestone pavement” because of the abundance of bumps. A picture of perforation of the muscle layer with the formation of abscesses and fistula tracts into the peritoneum is possible.
Fistulas connect with intestinal loops, penetrate into the bladder, in women into the uterus and vagina, and extend onto the skin of the abdomen. Histological examination reveals inflammatory infiltration throughout the entire thickness of the intestine. Lymphocytes, eosinophils, and plasma cells accumulate here.
In the photo, a sign of Crohn's disease is a granuloma of epithelioid and giant multinucleated cells, recorded during microscopy of an intestinal biopsy. There is no curdled necrosis in the central part of the granulomas. In this way they resemble sarcoidosis changes.
The result of chronic inflammation is the formation of scars from connective tissue, stenosis of the intestinal lumen. Crohn's disease affects the lymph nodes. Their tissue is filled with epithelioid granulomas and inflammatory elements.
Literature
- Adler G. Crohn's disease and ulcerative colitis, M.: GEOTAR-MED, 2001
- Belousova E. A. Ulcerative colitis and Crohn's disease. - Tver: Triada Publishing House LLC, 2002.
- Grigorieva G. A., Meshalkina N. Yu. Crohn's disease. - M.: Medicine, 2007.
- Khalif I. L., Loranskaya I. D., Ultrabedikyan H. A. Inflammatory bowel diseases (nonspecific ulcerative colitis and Crohn's disease): clinical picture, diagnosis and treatment. - M.: Miklos, 2004.
- Mayevskaya M.V. Gastroenterology, M., 1998.
- English Harrison's Principles of Internal Medicine, 14th Edition, McGraw-Hill, Health Professions Division
- English The National Medical Series for Independent Study, Allen R. Myers, MD Harwal Publishing
- Pathological anatomy, Strukov
- Pathological anatomy of diseases of the fetus and child, T. E. Ivankovskaya, L. V. Leonova
How to diagnose the disease
Due to the nonspecificity and variety of symptoms, diagnosis can be difficult.
That is why doctors prescribe a whole range of laboratory tests. An important role in calculating the disease is played by:
- blood test (general and biochemical);
- laboratory research;
- stool test for occult blood;
- tomography;
- histological examination;
- pathology activity index.
The doctor carefully listens to the patient’s complaints and examines him. When palpating the abdomen, intestinal tension can be noted.
You may be interested in an article about treating food poisoning at home.
And this article is about treatment for parasites in the human body.
We also recommend that you read the article about the treatment of ulcerative colitis.
Complications
Over a long period of time during the course of the disease and its treatment, the body can weaken, compensatory mechanisms are disrupted, leading to cachexia, enzyme deficiency, liver cirrhosis with liver failure, chronic pancreatitis and many other metabolic disorders.
Compared to other chronic diseases of the gastrointestinal tract, Crohn's disease can quickly develop complications that sometimes threaten the patient's life and can only be treated with surgery. The following complications are possible:
- Inflammation leads to the formation of ulcers.
- Fistulas. Transmural inflammation (inflammation of the entire intestinal wall) leads to perforation of the resulting ulcer into the peritoneal cavity. Fistulas can connect the intestinal lumen with other organs, such as the bladder, or with the external environment.
- Incomplete fistulas can lead to the development of peritonitis.
- Stagnation in the intestines creates a favorable environment for the proliferation of anaerobic bacteria, which contributes to the appearance of toxic megacolon.
Complications can arise for several reasons. The course of the disease is difficult due to a genetically programmed severe case of inflammation; in this case, it is almost impossible to avoid complications. Incorrectly selected treatment, the patient’s frivolous attitude towards the prescribed diet and life.
When diagnosing complications, urgent surgical intervention is necessary, because infectious pathologies leading to peritonitis reduce the patient’s chances of survival every minute.
Answers to frequently asked questions
Many people are interested in whether Crohn's disease can be cured. Doctors believe that complete healing is possible only if the cause is completely eliminated. This is very difficult to do, since first of all it requires an impact on the immune system. Therefore, it will take years for a full recovery. Please note that the disease is chronic and relapsing.
Another question is whether the disease is contagious. The inflammatory processes occurring in the gastrointestinal tract with this disease are not contagious. Therefore, you don’t have to limit yourself in communication when interacting with other people.
And the last question that patients often ask is whether the disease is inherited. Yes, the probability of occurrence is quite high. If one of the parents had this disease, the probability of its occurrence in the child is 20%.
What are the consequences that require surgical intervention?
The most pronounced negative manifestations complicate Crohn's disease and require surgical intervention. These include the formation of fistulous tracts from the intestine to the bladder, uterus in women with infection, the release of feces and air from the bladder, vagina.
Perforation (perforation) of the intestinal wall is possible with the development of abscesses in the abdominal cavity, severe peritonitis, external and internal fistulas, adhesions, and cicatricial changes. A chronic inflammatory process appears, accompanied by massive cicatricial constrictions of the intestinal lumen, this is the cause of intestinal obstruction.
Ulcers on the mucous membrane damage blood vessels and cause massive internal bleeding. The formation of megacolon with symptoms of intoxication is possible.
The formation of different fistulous tracts in the anorectal zone is shown schematically
To make a correct diagnosis, intestinal diseases of various etiologies are excluded. First of all, it is necessary to identify chronic infectious diseases, to distinguish Crohn's disease from nonspecific ulcerative colitis, congenital anomalies in children and hereditary pathologies.
You can read more about methods for identifying the disease and differential diagnosis of Crohn's disease in this article.
Symptoms of Crohn's disease in children
The danger of Crohn's disease in children lies in the peculiarities of the development of the pathology and the resulting symptoms. Slowly occurring inflammatory processes can form lesions on the intestinal mucosa for up to three years before the child’s parents notice the signs of IBD. Asymptomatic progression virtually eliminates the possibility of detecting pathology in the early stages. As a result, treatment of Crohn's disease in the future becomes more difficult.
Infiltration is the first phase of the onset of the inflammatory process, during which the structure of the vascular surface changes, and a large number of cells are observed in the submucosal layer. The intestinal walls are gradually covered with erosions, which, upon the onset of the ulceration stage (the next phase), deepen in the muscle layer and take on the appearance of ulcers.
Symptoms of Crohn's disease in children:
- Frequent urge (diarrhea, disturbing the child up to 10 times a day).
The volume and frequency of stool are indicators that directly depend on the location of the affected area. Signs of the disorder are more pronounced the deeper the pathogenic changes occur in the intestines. Blood and clots in bowel movements in IBD are not uncommon. Due to granulomatous processes in the small intestine, the absorption of nutrients and microelements in the body is disrupted. Against this background, the child rapidly loses weight. When diagnosing Crohn's disease in infants, it is also important to pay attention to the composition of the stool, which contains purulent signs and mucus in IBD.
- Pain and bloating.
In the early stages of intestinal dysfunction, abdominal cramps and pain are not intense and acute. As the pain progresses, the patient's sensations change - the pain intensifies, and the intestinal lumen shrinks.
- Nausea and vomiting.
Patients with IBD complain of a feeling of heaviness in the abdomen, causing vomiting. Against this background, loss of appetite occurs. Body temperature rises.
With “acute abdomen” syndrome, children are hospitalized for care in a hospital setting. The consequences of Crohn's disease are difficult to predict. The prognosis depends on the severity of the lesion, timely diagnosis and therapy.
In addition to intestinal manifestations, there are other symptoms that indicate IBD:
- Pain in the joints;
- Inflammation of the mucous membranes of the mouth and eyes;
- Ulcers, eczema, skin dermatitis.
Note: if a child gets sick in infancy, extraintestinal signs of Crohn's disease will not appear immediately, but later.
Causes
Predisposing factors for the development of the disease are:
- previous viral infection (measles);
- food allergies;
- stress and mental strain;
- smoking;
- hereditary predisposition.
To date, the causative agent of Crohn's disease has not been identified. However, the infectious theory is the main version of the origin of the disease. This is explained by the positive effect of treatment with antibacterial drugs. In addition, disorders of the immune system play an important role in the development of the disease. Autoimmune processes, in which antibodies are produced against one’s own intestinal tissues, and the insufficiency of the protective function of the immune system are an important link in the origin of the disease.
Reasons for development
There is no reliable and single cause for the development of Crohn's disease. The development of the pathological process is provoked by the influence of a significant number of different factors, which include:
- Hereditary predisposition is the main reason, which is realized at the genetic level. Today, more than 20 genes are known, the presence of which significantly increases the likelihood of developing Crohn's disease. They are inherited from parents to children. Such genes are more often found in the indigenous inhabitants of Northern Europe and America.
- A primary change in the functional state of the immune system, which leads to excessive cell activity. They begin to “erroneously” produce antibodies to the body’s own tissues. In this case, Crohn's disease often develops in combination with other autoimmune pathological processes (glomerulonephritis, rheumatism, rheumatoid arthritis).
- Infectious diseases - reliable data on the role of infectious pathogens in the development of Crohn's disease are currently missing. It is believed that some bacterial and viral infections in the intestines can be a trigger for the development of the pathological process. They lead to damage to the mucous membrane, followed by the production of antibodies to their own tissues by cells of the immune system.
Poor nutrition, dysbacteriosis that persists for a long period of time, bad habits (systematic consumption of alcohol, smoking), excessive physical and psycho-emotional stress can accelerate the development of pathology. Knowledge of the causes and provoking factors that increase the likelihood of developing Crohn's disease in BP makes it possible to carry out adequate preventive measures.
Characteristics of the disease
Crohn's disease occurs with remissions or exacerbations. Most often it affects the final section of the small intestine or the large intestine. At the moment, statistics show 60 per 100 thousand people with an autoimmune disease.
The pathology acquired its name in honor of its discoverer, American gastroenterologist Barril Crohn. He first reported the identification of a new type of disease in 1932 at a scientific meeting.
The disease develops in the place where water is absorbed and feces are formed. Segmental inflammation mainly affects the distal part of the intestine. Crohn's disease is common in the age range from 13 to 37 years. Signs can appear even in the healthiest person.
Sometimes it is difficult to determine the inflammatory process, since it is similar to pathologies such as dysentery, non-ulcerative colitis, salmonellosis and others. At any age, starting from 13 years old, both boys and girls are susceptible to inflammatory processes. Diagnosis in children is carried out in the same way as in adults.
Forecast
Crohn's disease is incurable, disabling, with severe complications, constant treatment with hormonal or immunosuppressive drugs, which causes a lot of unpleasant consequences.
Such patients quickly lose the ability to work and become disabled. Due to unpleasant symptoms, operations, therapy, it is difficult for them to go out in public and build a personal life. Despite the favorable prognosis for life expectancy, the prognosis for work and personal life is always relative.
If Crohn's disease occurs in a mild form, with rare exacerbations, then perhaps such a patient will not differ from a healthy person during the period of remission. And for him the prognosis will be favorable for all aspects of life.
Unfortunately, Crohn's disease tends to progress, and any mild form over the years can develop into a severe one, with all possible complications.
Difference from ulcerative colitis
Crohn's disease and nonspecific colitis are included in the group of inflammatory bowel pathologies. It is difficult to determine the difference in symptoms. Often expressed by the same symptoms. Differential diagnosis requires additional research and includes the distinctive features shown in the table.
| Signs | Crohn's disease | UC |
| Localization of the outbreak | In 66% of cases at the border of the small and large intestine, other parts are affected less frequently. | In the rectum and colon. |
| Endoscopic picture | An alternation of healthy and inflamed areas is observed, fistulous tracts, ulcers, erosions, and narrowing of the lumen are detected. | The mucous membrane is loose, swollen, there is a large ulcer with a bleeding surface, the edges are inflamed, at the bottom of the granulation, polyps are possible. |
| Conclusion of X-ray diagnostics | The affected areas are asymmetrical in localization, alternating with normal ones, with signs of narrowing. | The entire intestine is changed, the ulcers are larger in size, granulations are visible. |
Differential diagnosis of the disease
Practice shows that with all the desire and capabilities of medicine, every tenth case is registered as “unspecified colitis”. In order to identify a disease, it is necessary to exclude many diseases with a similar picture. Let us note only the main differences:
- sarcoidosis - damage to the lung tissue, liver, eyes, skin is detected, the result of the biopsy is important;
- intestinal tuberculosis - positive tuberculin tests, an effective treatment regimen with anti-tuberculosis drugs, more often there is a primary pulmonary focus;
- Behcet's disease - basis - vascular pathology (systemic vasculitis with ulceration);
- cholelithiasis - detected by examining the patency of the ducts, damage to the pancreas disrupts digestion;
- intestinal cancer - the tumor is visible during colonoscopy and confirmed by biopsy;
- Radiation colitis - the dose of radiation is important, the connection with the previous radiation therapy;
- lupus erythematosus, scleroderma - characterized by systemic vasculitis, clinical signs of abdominal crises;
- contagious intestinal infections - diagnosed by bacteriological examination, serological tests.
Prevention
It is impossible to prevent the onset of Crohn's disease, but it is possible to prevent exacerbation and improve remission. To do this you need:
- closely monitor the condition of the body as a whole;
- come to your doctor's appointment at the appointed time;
- take all prescribed pills;
- adhere to the prescribed diet;
- take additional vitamin complexes;
- quit smoking and alcohol;
- perform physical activity regularly.
It is very important to monitor your nervous condition, since stress is a very common reason for the return or exacerbation of Crohn's disease. If you fulfill all the requirements in good faith, you can achieve excellent results and the disease will be defeated.
Project consultant, co-author of the article: Ovchinnikova Natalya Ivanovna | Gastroenterologist, Hepatologist, Infectious disease specialist 30 years of experience / Doctor of the highest category, Candidate of Medical Sciences
Education:
Diploma in General Medicine, Novosibirsk State Medical Institute (1988), Residency in Gastroenterology, Russian Medical Academy of Postgraduate Education (1997)