A common proctological disease, paraproctitis, after surgery requires special attention and long-term rehabilitation. If all the specialist’s recommendations are not followed, a relapse of the disease is possible, leading to repeated surgery. It is necessary to analyze in detail what paraproctitis is, the causes and mechanism of its formation, the main method of combating pathology, and treatment in the postoperative period.
The importance of rehabilitation measures after paraproctitis surgery
Surgery for paraproctitis is a method of radical treatment. It includes dissection of the skin and tissue to remove pus, fistulas, followed by plastic surgery and suturing. During the manipulation, tissue damage occurs, therefore, to obtain a favorable result, postoperative therapeutic measures are necessary. They pursue several goals:
- Preventing the development of an infectious process - damaged tissues are the entry gates for various pathogenic and conditionally pathogenic microorganisms.
- Creating conditions for rapid tissue healing.
- Reducing the severity of the inflammatory reaction - cells of the immune system rush to the site of tissue damage, producing prostaglandins and other biologically active compounds. They are responsible for the occurrence of pain, increased blood supply to tissues, as well as their swelling.
- Improving the functional state of the digestive system, as well as reducing the load on the intestines.
Carrying out therapeutic measures can improve a person’s general condition, reduce the severity of discomfort, and also speed up recovery.
Basic rules of nutrition during illness
Diet therapy prevents the development of abscesses, normalizes stool, and reduces the symptoms of the disease. List of recommendations:
- split meals: eat every day at the same time of day;
- drinking 5-7 glasses of plain purified water per day to soften stool and facilitate the emptying process;
- For lunch, be sure to eat hot soup or broth;
- inclusion of fresh fruits, vegetables, berries, salads rich in fiber;
- reduction of refined foods, sugar;
- exclude spicy, sour, fatty foods, smoked foods, alcohol.
Important! Citrus fruits are consumed with extreme caution; allergy sufferers are advised to abstain.
Products prohibited for paraproctitis
It is recommended to avoid smoked foods, canned foods, spicy, salty, spices, baked goods, flour foods, rich meat or fish broth. Avoid fried and fatty meats, alcohol, tea, coffee, and soda. It is not recommended to eat foods that may cause difficulty in bowel movements:
- red wine;
- bakery products made from premium flour;
- blueberries;
- cocoa beans;
- rice;
- spinach, sorrel;
- grapes;
- mushrooms;
- almonds;
- corn and pearl barley;
- fatty meat and fish;
- dairy products with a high percentage of fat, cream;
- garlic, onion;
- rutabaga;
- ice cream;
- chocolate;
- pastry cream;
- shortcrust pastry;
- legumes: chickpeas, beans, peas, lentils;
- dishes with a viscous consistency: slimy soups, pureed porridges;
- hot seasonings, sauces and dishes: horseradish, mustard, Tabasco, pepper, ketchup;
- You should not eat foods that can cause increased gas formation: white cabbage, radish.
The main methods of surgical treatment of fistulas
A fistula is a canal connecting the rectal cavity with the tissue around the organ. In this case, bacteria enter from the tissue, leading to inflammation, which is called paraproctitis. Surgical treatment includes removal of the pathological canal, purulent contents in the tissues, followed by plastic surgery. Techniques are used to preserve the integrity and functional state of the anal sphincter:
- blockage of the fistula lumen with biological sealing tampons;
- intersection of the canal in the intersphincteric space or in the submucosa;
- transplantation of adipose tissue cells into the fistula;
- laser ablation;
- introduction of chemical compounds that destroy the cells of the fistula with subsequent closure of the canal;
- closing the internal opening of the fistula with a displaced section of the mucous membrane of the large intestine.
Important! The duration of recovery after excision of a rectal fistula depends on the surgical technique.
Stages of excision of the fistula in a single block, a - oval incision of the external opening of the fistula, b - excision of the fistula in a single block using a probe. (From: Dultsev Yu.V., Sapamov K.N. Paraproctitis. - M., 1981.)
Advantages of performing an operation at Miracle Doctor
Advanced low-impact technologies
Microscopic punctures are made, and intervention is carried out through them. The second option is bloodless surgery using radio wave techniques.
Our specialists develop a fistula removal and rehabilitation scheme for each patient separately.
Hospital with constant supervision of medical staff
We offer comfortable rooms with an individually designed menu. Each postoperative patient is cared for by a nurse and also examined by a doctor.
Speed of the rehabilitation period
The highly qualified doctors of the Miracle Doctor clinic, extensive experience in performing operations in the anorectal area and modern technologies allow us to achieve the highest results and prevent the development of complications when removing a rectal fistula after surgery.
Convenient location of the clinic
The building is located a two-minute walk from the Rimskaya metro station in Moscow.
You can by phone or on our website
Leave your contact information in the online registration or call back form, we will definitely call you back.
Rules for the treatment of paraproctitis after excision
Therapeutic measures after surgery for the radical treatment of paraproctitis are carried out in 2 stages:
- treatment in a medical hospital;
- carrying out activities at home after discharge from the hospital.
To obtain a positive result, it is important for the patient to follow several important rules:
- For several days, therapy is carried out only in the department.
- Prevention of infection involves dressings in compliance with aseptic conditions aimed at preventing bacteria from entering the wound.
- Only sterile material should be used for dressing.
- If infection develops, antibiotics are prescribed.
- Reducing the functional load on the lower intestines is achieved through diet.
- The duration of the postoperative period depends on the extent of the surgical intervention.
- Quality control of therapy is carried out using laboratory tests and instrumental studies.
Based on a comprehensive examination, the attending physician decides whether to discharge the patient home.
Hospital
After the operation, the patient remains in a medical hospital. This is necessary to ensure quality treatment and prevent complications. The department is equipped with a manipulation room, where it is possible to carry out dressings. If the patient is in pain, non-steroidal anti-inflammatory drugs are used. Bleeding is a condition in which hemostatic agents are urgently prescribed.
Important! The length of a patient's stay in the hospital is determined individually. It depends on the type and volume of the operation performed and averages 5-10 days.
Follow-up outpatient treatment at home
Upon discharge from the hospital, the patient receives recommendations regarding further therapy. The emphasis is on diet and physical activity. The diet is designed to ensure normal bowel movements and prevent the development of constipation. Motor activity increases gradually.
It is recommended to perform special gymnastic exercises that involve the buttocks. With good blood supply and moderate physical activity, tissues will heal and recover faster. Walking in the fresh air for half an hour is also recommended. Following the recommendations helps prevent the recurrence of the pathology in the future.
Recovery methods
Surgery is an effective method of removing the rectal mucosa where the purulent abscess is located. You can eat after surgery only after several days. Immediately after surgery, you should drink plenty of clean water. When the operation takes place, in the first 2 days a gentle diet is prescribed, including ground porridge, light soups, broths, and steamed dishes. Expansion of the diet occurs with normalization of bowel movements. Food after surgery should be easily digestible, healthy, and rich in carbohydrates. Lotions and antiseptic dressings of the anus are additional therapeutic measures.
To avoid relapse of the disease it is necessary:
- undergo regular medical examinations;
- adhere to a healthy diet;
- make medicinal compresses;
- monitor the nature of the stool, if constipation occurs, use laxatives and enemas.
An effective method of recovery from paraproctitis is following the rules of a therapeutic diet: it is necessary to exclude from the diet foods that cause increased gas formation and constipation.
Main nuances of the postoperative period
Treatment in the postoperative period includes several important nuances:
- normalization of stool;
- compliance with dietary recommendations;
- treating wounds to speed up healing;
- use of antibiotics;
- preventing exacerbation.
Each nuance is of great importance to obtain an overall positive therapeutic result.
Normalization of stool
After surgery, which is performed with anesthesia, intestinal motility often decreases. This is accompanied by the development of constipation in the postoperative period, which increases the risk of sutures coming apart during defecation. Following a diet helps loosen stools and normalize intestinal motility, but in the first days the prescription of laxatives is often required. Several groups of drugs have become widespread:
- indigestible carbohydrates (Lactulose, Duphalac);
- emollients (Vaseline oil, Glycerin);
- irritant laxatives (rhubarb root, castor oil);
- salt products (magnesium sulfate).
A laxative that acts by increasing peristalsis. Helps with systematic constipation.
The choice of drug and duration of its use is based on the severity of constipation. Emollients in the form of suppositories and complex carbohydrates in capsules received good reviews. Laxatives that increase the volume of intestinal contents are not prescribed, as the risk of suture dehiscence increases.
Diet food
During the first day after surgery, diet 0 (therapeutic fasting) is prescribed, and a small amount of still mineral water is allowed. Then, within 2-3 days, the diet is expanded to include crushed food in the form of vegetable puree, dietary meat (diet 1 according to Pevzner). Then, in the absence of complications, a general diet is prescribed. All dishes are steamed or boiled. During the day, food is taken at least 5 times, while portions remain small. Dinner is allowed no later than 2 hours before expected bedtime.
The diet involves fractional meals and a fairly high caloric intake. The preferred food processing is boiling and steaming.
Healing: wound treatment
Treatment of a postoperative wound is carried out in a manipulation room once every 1-2 days. In this case, a sterile dressing material must be used, including bandages, medical cotton wool, and gauze wipes. At the same time, the surface of the postoperative wound is washed with antiseptic solutions. If a drainage is installed, then medications are injected through it into the fiber.
To stimulate tissue healing, Levomekol ointment is used, which is applied to the wound surface after treatment with an antiseptic solution. The drug destroys microorganisms and accelerates regeneration.
Antibiotic therapy
Antibiotics are not always prescribed. The indication for the use of drugs is the appearance of symptoms of acute inflammation in tissues. The skin around the stitches turns red, becomes hot, and body temperature rises, which indicates intoxication.
Important! In hospital settings, semisynthetic penicillins or cephalosporins are prescribed in the form of tablets or capsules. In case of severe infection, parenteral forms in the form of injections are used. The duration of antibiotic therapy is 5-10 days.
Prevention of relapse
To prevent exacerbation of the disease, bed rest is prescribed immediately after surgery. After 1-2 days you are allowed to get out of bed and walk a little. Then the motor mode expands. During the entire rehabilitation period, the patient is not recommended to sit, as this increases the load on the perineal area and there is a risk of sutures coming apart.
After discharge from the hospital, the motor mode expands. It is allowed to perform special gymnastic exercises and walk in the fresh air. Preventing relapses is impossible with proper care of the perineal area. After defecation, it is recommended to wash with clean warm water without adding detergents. Toilet paper cannot be used.
Diet for paraproctitis
An important point during the rehabilitation period is proper nutrition and restoration of normal stool. In the next 2-3 days after surgery, stool should normalize. Otherwise, cleansing enemas are done.
The first meal should take place a few hours after surgery. It is important that the food is gentle and easily digestible, capable of easy emptying. For rapid healing of the postoperative wound, there should be no strong straining, hard feces, or constipation. It is strictly forbidden to eat fried, sweet, salty, spicy, gas-forming foods and alcohol.
Dietary nutrition throughout the rehabilitation period should consist of viscous porridges in water, boiled meat, steamed fish, baked apples, and omelettes. Fresh vegetables and fruits are not allowed.
The list of products desirable for consumption must be approved by a doctor. Dried fruits (dried apricots, prunes), natural yoghurts, kefir, and fruit drinks will help fight constipation. You should establish the correct drinking regime, drink at least 1.5 liters of clean still water per day.
The recovery period, during which you should adhere to a strict diet, can last up to 3-4 months. After this, subject to successful wound healing and with the consent of the doctor, you can gradually switch to your usual diet.
It is easier to prevent the development of a disease than to treat it later. This statement fully applies to paraproctitis, an unpleasant proctological disease known for its relapses and complications.
Prevention of paraproctitis and prevention of relapses includes:
- strengthening the immune system;
- correction of vascular disorders (atherosclerosis, diabetes mellitus);
- elimination of foci of chronic infection;
- normalization of the gastrointestinal tract, excluding constipation and diarrhea;
- timely treatment of diseases of the rectum (hemorrhoids, anal fissures);
- proper nutrition;
- eliminating bad habits such as drinking alcohol and smoking.
You should be attentive to your health and, if the first signs of any disease occur, consult a specialist.
Possible postoperative complications and ways to treat them
With improper treatment or its absence in the postoperative period, the following complications develop:
- seam divergence;
- bleeding of varying severity;
- formation of intestinal fistula after surgery;
- infection of tissues with subsequent inflammation, which may subsequently lead to the formation of a purulent focus;
- narrowing of the rectal lumen, leading to chronic constipation;
- violation of the functional state of the intestine.
Prevention of the development of complications is achieved against the background of adequate treatment of paraproctitis after surgery.
Surgery is often required for radical treatment of paraproctitis. How long you will stay in the hospital after surgery and how long the rehabilitation will last is determined by your attending physician. He prescribes therapeutic measures depending on the severity of the pathology and the extent of the operation performed.
Bibliography
- An V.K., Rivkin V.L. Emergency proctology. M.: Medpraktika Publishing House. M., 2003. 144 p.
- Bogomazov Yu.K., Tumanov A.B. Advantages of hemorrhoidectomy using the UDO-38 device // Current issues in coloproctology: Mater. 2 congresses of coloproctologists of Russia with international participation. Ufa, 2007. pp. 138-139.
- Anakhosyan V.R., Bagdasarov G.A., Ostrin P.I., Kogan L.V. Some issues of surgical treatment of acute paraproctitis. Sov. Med., 1977, No. 12, p. 48-51.
- Aregvi M.E., Sakkier J. Minimally invasive coloproctology (translated from English) M., Medicine, 1999, p. 100.
- Dultsev Yu.V., Sapamov K.N. Paraproctitis. - M., 1981
Paraproctitis is an acute inflammatory process affecting the peri-rectal tissue. The most common cause of this disease is the penetration of pathogenic microorganisms through rectal fissures; less commonly, this pathology can occur when the infection is transferred from another focus by hematogenous or lymphogenous routes. The main treatment method for this disease is surgery.
Treatment of paraproctitis after surgery involves both non-medicinal (compliance with the regime and diet) and medicinal (use of antibacterial and antiseptic agents) methods. This and much more will be discussed in our article.
Rehabilitation period
After paraproctitis surgery, the patient requires recovery. At first, the patient is prescribed bed rest in the hospital for a week. Then treatment begins on an outpatient basis. Full recovery depends on the severity of the disease and the complexity of the surgical procedure.
What is done in case of chronic inflammation?
Complications in the postoperative period are rare. The patient is prescribed dressings, which must be performed every day. To ensure intensive healing, antibacterial ointments and creams are used.
Therapy for acute cases
The wound is dressed and treated with antiseptic and antibacterial medications. Doctors often use Methyluracil or other agents to speed up healing. At the same time, the patient is referred to physical therapy. For this purpose, prescriptions for ultraviolet irradiation are issued. Additionally, they are referred to therapy with ultra-high frequencies (40-70 W) or microwaves (20-60 W).
Treatment is selected to suit each case. The procedures are carried out for 10 minutes, and the course lasts from 7 to 14 days. Sometimes the period is increased if there was a complex operation.
Treatment in the postoperative period
Typically, paraproctitis after surgery is treated with daily wound treatment, dressings using antibacterial and anti-inflammatory ointments, vitamins and immunomodulators. Physiotherapeutic treatment is often prescribed. Various recovery methods are used - they will be discussed below.
Physiotherapy
The physiotherapeutic method of treatment is aimed at eliminating pain, accelerating tissue regeneration, and also preventing relapse of the disease. In the postoperative period, patients may be prescribed:
- ultraviolet irradiation;
- magnetic therapy;
- ultra high frequencies;
- microwave.
One of the above methods is carried out in a hospital for 10 minutes, the course of treatment is 5-14 days.
Physiotherapeutic procedures are carried out only after the acute inflammatory process has reduced.
Dressings
Dressings with ointments in the postoperative period relieve the inflammatory process in the tissues and prevent re-infection of the wound.
The first dressing is carried out 24 hours after the operation. Before applying a bandage, the wound is treated with antiseptic solutions such as Iodopirone, Chlorhexidine.
Next, a bandage is applied: for acute paraproctitis - a dry aseptic one, and for a chronic form of the disease - with the use of antibacterial ointments (Fuzimet, Levomekol). To speed up wound healing, use Methyluracil ointment.
Dressings are carried out daily, while the attending physician assesses the condition of the postoperative wound: with rationally performed procedures, there should be no signs of secondary infection (hyperemia, swelling, increased local temperature) and suture dehiscence.
Medicines
Acute paraproctitis is not an indication for the systemic use of antibacterial drugs. Usually, the chronic form of the disease is treated with antibiotics, but there may be other indications for their use:
- accompanying illnesses;
- signs of intoxication of the body;
- spread of infection to neighboring tissues;
- long-term non-healing wound;
- relapses of the disease.
Broad-spectrum penicillins (Ammoxicillin, Amoxiclav) are usually prescribed. In the presence of anaerobic infection, Metronidazole is used.
Vitamins A, E, C and immunomodulators (Imupret, Imudon) are also prescribed as general treatment. Painkillers (Analgin, Ketorolac) are used to relieve pain. Often, on the first day after surgery, patients may have a rise in body temperature - in this case, antipyretics are used (Fenbufen, Nurofen).
Rectal suppositories (Anuzol) and warm baths with anti-inflammatory and antiseptic herbs (chamomile, sage) are used as local treatment.
Active patient management plays an important role in the recovery of the body in the postoperative period. The regimen followed by the patient depends on the form of the disease:
- For acute paraproctitis, an active regimen is prescribed: you can get out of bed on the second day after surgery. To avoid an early urge to defecate, some restrictions are possible, but the patient is allowed to walk around the ward and corridor.
- After chronic paraproctitis, the regime is generally active, but depends on the volume of the operation: if surgery was performed with suturing of the anal sphincter, bed rest is extended to a week.
Early initiation of an active regimen normalizes hemodynamic parameters, prevents congestion in the lungs, increases body tone, and accelerates wound regeneration.
Symptoms of acute and chronic paraproctitis
Acute paraproctitis is characterized by a sudden and striking manifestation. The disease develops quickly, within 2-3 days. The abscess can occur subcutaneously or deep inside.
The first symptoms of the acute form of this disease are:
sharp, increasing pain in the anus, aggravated by movement, urination or defecation;
- redness of the skin near the anus;
- increased body temperature;
- chills;
- weakness;
- headache.
If you do not consult a doctor in a timely manner or if treatment is carried out incorrectly due to high intoxication of the body resulting from a widespread infection, the patient may die.
Chronic paraproctitis usually forms from an insufficiently well-treated acute form of the disease or from spontaneous opening of an abscess. A peculiarity of this form of the disease is the formation of an anal fistula due to incomplete scarring of the tissue. Other symptoms characterizing chronic paraproctitis are:
- dull pain that intensifies with straining;
- purulent discharge from the anus;
- itching in the perineal area;
- deformation of the anal area;
- moderate increase in body temperature;
- decreased appetite;
- general malaise.
There is an undulating course of the chronic form of the disease: periods of exacerbation are replaced by remission. It is important to note that anal fistula tracts cannot disappear on their own and require immediate treatment in order to prevent the development of dangerous complications.
If you do not contact a specialist in a timely manner, purulent inflammatory processes can spread widely in the patient’s pelvic area. A formidable complication of paraproctitis should be considered purulent melting of the walls of the rectum and urethra. Purulent contents can enter the abdominal cavity, retroperitoneum, and vagina in women. The patient experiences discharge of pus and blood from the rectum and vagina. In this case, there is a real threat to the patient’s life and urgent surgical intervention is required.
Nutritional Features
Diet for paraproctitis involves the following aspects:
- eating easily digestible food;
- consumption of foods that normalize stool;
- exclusion of products that increase gas formation;
- compliance with the drinking regime - drinking at least 2 liters of fluid per day;
- exclusion of spicy, salty, smoked dishes;
- meals should be provided at least 5 times a day in small portions;
- It is preferable to boil, bake, steam food;
- It is also recommended to reduce the amount of foods that are not fully digested in the intestines.
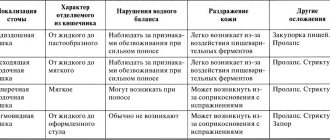
| Products | Allowed | Prohibited |
| Broths | Vegetable | Strong meat |
| Vegetables | Beets, carrots, spinach, cucumbers, radishes, green onions | Fresh cabbage, legumes (beans, peas) |
| Drink | Fruit and berry juices, dried fruit compotes, fermented milk drinks | Strong tea, coffee; alcoholic, carbonated drinks |
| Cereals | Buckwheat, wheat, barley, corn | Rice, semolina; cereals |
| Bread | Black bread | White flour bread and other flour products (buns, buns) |
| Meat | Chicken, rabbit, turkey | Pork |
| Fish | Cod, flounder, hake | Herring, salmon, tuna |
To avoid constipation, foods allowed for paraproctitis should be introduced into the diet gradually, starting with small quantities.
Basic rules of nutrition during illness
Diet therapy prevents the development of abscesses, normalizes stool, and reduces the symptoms of the disease. List of recommendations:
- split meals: eat every day at the same time of day;
- drinking 5-7 glasses of plain purified water per day to soften stool and facilitate the emptying process;
- For lunch, be sure to eat hot soup or broth;
- inclusion of fresh fruits, vegetables, berries, salads rich in fiber;
- reduction of refined foods, sugar;
- exclude spicy, sour, fatty foods, smoked foods, alcohol.
Important! Citrus fruits are consumed with extreme caution; allergy sufferers are advised to abstain.
Products prohibited for paraproctitis
It is recommended to avoid smoked foods, canned foods, spicy, salty, spices, baked goods, flour foods, rich meat or fish broth. Avoid fried and fatty meats, alcohol, tea, coffee, and soda. It is not recommended to eat foods that may cause difficulty in bowel movements:
- red wine;
- bakery products made from premium flour;
- blueberries;
- cocoa beans;
- rice;
- spinach, sorrel;
- grapes;
- mushrooms;
- almonds;
- corn and pearl barley;
- fatty meat and fish;
- dairy products with a high percentage of fat, cream;
- garlic, onion;
- rutabaga;
- ice cream;
- chocolate;
- pastry cream;
- shortcrust pastry;
- legumes: chickpeas, beans, peas, lentils;
- dishes with a viscous consistency: slimy soups, pureed porridges;
- hot seasonings, sauces and dishes: horseradish, mustard, Tabasco, pepper, ketchup;
- You should not eat foods that can cause increased gas formation: white cabbage, radish.
If any product causes increased flatulence, discomfort, or pain in the stomach, it must be immediately excluded from the diet. In case of exacerbation, it is necessary to remove the fistula.
What should be in the diet: allowed foods and dishes
The diet consists of sauerkraut, boiled beets, cabbage, carrots, tomatoes, cucumbers, radishes, dairy products, light soups, lean meat and fish dishes, black bread, whole grains (except white rice). The patient is advised to use herbal and fruit and berry infusions, rosehip infusion, and prunes.
| Allowed to use | |
| Vegetables |
|
| Dried fruits |
|
| Greenery |
|
| Fruits |
|
| Cereals |
|
| Bakery products |
|
| Eggs |
|
| Confectionery |
|
| Meat fish |
|
Diet
The duration of diet therapy depends on the patient’s well-being and the regenerative capacity of the affected tissue. The diet is varied - alternate whole grain foods, vegetables, berries, and protein-rich foods. Avoid foods that can cause constipation and increased gas formation. If you are prone to difficulty defecating, the menu is enriched with boiled beets, seaweed, vegetable oils, fiber, psyllium, and dried fruits. The use of flax seeds is indicated. To increase bioavailability, flax is ground in a coffee grinder and consumed within 15 minutes after grinding.
Sample menu for the week
Sample menu for a week for patients with paraproctitis:
| Breakfast | Dinner | Afternoon snack | Dinner | |
| Monday | buckwheat with boiled beets | baked turkey fillet, cream soup with broccoli | half a cup of fresh berries, apricot decoction | cottage cheese casserole with low-fat cottage cheese |
| Tuesday | oatmeal with a small piece of butter | steamed cutlets, vegetable broth soup, prune broth | stewed apples with raisins and cinnamon | boiled fish, carrot-beet puree |
| Wednesday | salad with vegetables, boiled chicken breast | pearl barley porridge, steamed cutlets | a handful of dried fruits, rosehip decoction | grilled zucchini, vegetable salad |
| Thursday | buckwheat porridge with vegetable milk, apricot decoction | vegetable soup, whole grain bread, large bowl of lettuce | baked apples | fish baked in tomato sauce, large portion of salad |
| Friday | pumpkin porridge with semolina, grated apples, cinnamon | boiled chicken breast, stewed vegetables | smoothie with berries, banana, flax seeds | mashed potatoes with steamed cutlets, a large portion of salad |
| Saturday | whole grain bread with mild, low-fat cheese, apricot broth | vegetable soup with buckwheat noodles, boiled vegetables, baked turkey fillet, prune broth | plum compote with biscuits | vegetable stew, fish cutlet, salad |
| Sunday | oatmeal with dried fruits, rosehip decoction | rassolnik with baked chicken and potatoes | berry smoothie | baked potatoes with herbs, steamed chicken cutlets |
How long does healing take?
Many patients are interested in how long it takes for the wound surface to heal after surgery. The timing depends on the volume of intervention and, on average, is 21-28 days. During this period, it is recommended to give up an active lifestyle, avoid lifting heavy objects, and going to the pool. Wound healing should be monitored by a doctor - surgeon or proctologist.
To prevent infection from entering the wound, which can increase its healing time, proper treatment is necessary: first, wash the wound surface with an antiseptic solution, then apply ointment and cover the wound with an aseptic bandage. After each act of defecation, it is also recommended to treat the postoperative scar.
After surgery, partial weakness of the anal sphincter is possible. This can lead to stool and gas incontinence. To eliminate this problem, special gymnastics are used.
Why diet?
Paraproctitis is a pathological condition in which the fatty tissue of the rectum becomes inflamed. This pathology is considered quite common; it is diagnosed in almost 30% of all visits to proctologists. The disease mainly affects the adult population. Paraproctitis in infants is diagnosed extremely rarely, although such cases are also possible.
The only effective treatment for paraproctitis is surgery. In case of acute symptoms of the disease, it is carried out on an emergency basis and cannot be postponed. If the disease was detected in the subacute period, when an inflammatory process occurs in the intestinal wall and there is compaction, conservative treatment can be carried out within 1-3 weeks.
If treatment of acute paraproctitis is not carried out in a timely manner, the disease becomes chronic. Periodically, the patient may experience exacerbation of symptoms.
In both acute and chronic paraproctitis, nutrition plays an important role. It is important for people diagnosed with the disease to have regular bowel movements. In addition, feces should have a soft consistency so that when they pass through the rectum, there is no injury to the mucous membrane of the affected organ. These problems can be solved by following a diet.
In the postoperative period, when rectal disease is eliminated surgically, adherence to diet is also very important. The main task of the diet in the recovery period is to improve stool and prevent the occurrence of dyspeptic symptoms: bloating, intestinal spasms, problems with appetite and digestion.
Why doesn't the wound heal?
If after a month the wound does not heal, you should immediately contact your doctor to correct the problem.
The main causes of this complication are:
- irrational wound treatment and application of bandages;
- permanent damage to the wound surface when it is treated too thoroughly;
- incorrect selection and irregular use of antibacterial drugs;
- secondary infection of the wound endogenously from foci of infection in the body (most often chronic forms of tonsillitis, sinusitis, cholecystitis);
Less commonly, there are cases when surgery does not have a positive effect. This usually occurs in the chronic form of paraproctitis with the presence of a non-healing fistula. With this outcome, the patient is advised to undergo repeat surgery, which is performed no less than a year later.
The relevance of dieting
Considering the need for urgent surgical treatment upon diagnosis, there is no special diet for paraproctitis.
Functional disorders of the gastrointestinal tract can manifest themselves in changes in the tone and peristalsis of hollow organs. A big role in this is given to habits and the nature of nutrition, since many pathological conditions can be aggravated if such banal recommendations as diet are not followed. Features of the regime and diet of food consumption can play a big role in the following conditions that can lead to paraproctitis:
- Exhaustion of the body, cachexia, exhausting methods of losing weight;
- Reducing local and general resistance of the body (immunity);
- Addiction to alcohol, smoking;
- Development of infectious and inflammatory diseases, including the digestive tract;
- Improper nutrition worsens the patient's condition in the presence of diabetes, which leads to the progression of damage to small vessels (it is thanks to them that gas exchange occurs in the tissues);
- Failure to comply with dietary recommendations in case of atherosclerosis;
- Functional constipation, prolonged diarrhea, intestinal obstruction, fecal incontinence;
- Hemorrhoids and anal fissures (constipation is one of the most common risk factors for the formation of nodes);
- Disruption of food digestion processes in the intestines - fermentation and rotting.
With paraproctitis, the functions of the final sections of the large intestine are primarily disrupted, and its emptying suffers. Considering the need for proper recovery after surgery, as well as during treatment, it turns out that diet is needed primarily to ensure an adequate bowel movement.
Regular stool passage is necessary both to prevent infectious and inflammatory complications and dyspepsia (flatulence, nausea, constipation, diarrhea), and to restore intestinal tone and motility.
In fact, patients should strive to ensure that there are not even prerequisites for the formation of fecal stagnation or frequent loose stools.
Prognosis and prevention
Prevention of paraproctitis is aimed at preventing recurrence of the disease and implies the following rules:
- prevention of digestive disorders (diarrhea, constipation);
- adherence to a specialized diet;
- timely treatment of chronic foci of infection;
- rational therapy of other diseases of the rectum and anus;
- maintaining an active lifestyle;
- eliminating bad habits.
In general, the prognosis for timely treatment of this pathology is favorable. But long-term fistulas often lead to the spread of the process to the sciatic nerve with the occurrence of ischiorectal paraproctitis, pelvic-rectal tissue (retrorectal form) and other organs and tissues. In such cases, treatment becomes more complicated and the prognosis becomes questionable.
Causes and symptoms of paraproctitis
Disease of the veins in the subcutaneous layers, mucous membrane, fatty tissue, perimuscular tissue or rectum develops against the background of provoking factors:
- frequent stress,
- abuse of bad habits (smoking, alcohol),
- sedentary sedentary lifestyle,
- intestinal diseases,
- digestive system disorders,
- unhealthy diet
- infection,
- gastrointestinal disorder,
- pathological manifestations in the rectum,
- wearing tight, tight underwear,
- hypothermia in the off-season.
What does paraproctitis look like?
More often, paraproctitis is diagnosed in older people, when treatment for diseases of the rectum was not carried out from a young age. The disease led to complications and surgery. Perhaps there are residual infectious phenomena in the body that transform into a fistula, or adhesions are observed in the pelvis and rectum. The main symptoms of paraproctitis:
- sharp burning pain in the lower abdomen, around the anus,
- low temperature,
- dizziness,
- prostration,
- loss of appetite,
- symptoms of poisoning,
- pain during defecation,
- hyperemia, sphincter pain,
- constant drowsiness, apathy.
Paraproctitis in chronic form acquires a relapsing course. Exacerbations are replaced by remission of the disease.
Only a timely radical operation to excise purulent, necrotic areas in the rectum will help stop the progression of paraproctitis and improve the general well-being of patients, so a visit to the clinic at the first suspicion is mandatory.
ethnoscience
The main ways to have regular bowel movements using simple ingredients are:
- juice from carrots, spinach, red rowan;
- boiled beets with the addition of vegetable oil;
- sauerkraut brine;
- prunes;
- brine of soaked lingonberries.
Medicinal decoctions of dried chamomile and sage have an antiseptic and anti-inflammatory effect. Herbal teas based on yarrow, plantain, St. John's wort, and celandine improve the functioning of the digestive system.
Prevention
Treatment of paraproctitis after surgery will pass without complications if you follow all the doctor’s recommendations. The main prevention of disease recurrence is careful wound care after surgery. Make dressings in a timely manner. Be sure to use antiseptics and antibacterial ointments, which will protect the operated area from infection. Personal hygiene is also of great importance. Remember to wash the anal area after each bowel movement, as well as in the morning and evening.
In addition, try to avoid constipation. To do this, watch your diet. Drink at least one and a half liters of water daily. Avoid foods that have fixing properties and cause intestinal irritation and flatulence. And, of course, to avoid relapses, contact your doctor immediately if you have any problems with the operated area.
Dietary recommendations for patients with paraproctitis
In chronic and acute paraproctitis, nutrition is certainly important. People suffering from this disease must, first of all, avoid the development of constipation and ensure that the stool has a soft consistency, since this will eliminate the risk of injury to the rectal mucosa. Nutrition will help achieve this effect. Your diet should include foods rich in fiber every day. These include a variety of vegetables and fruits - pumpkin, broccoli, apples, boiled beets, dried fruits, etc., whole grain bread, oatmeal, buckwheat and barley porridge are healthy. Food rich in plant fiber improves intestinal motility.