Appendicitis is a common disease associated with a huge risk for humans. An untimely visit to a medical facility can lead to irreparable consequences. If your appendix bursts, you could die. Seeing a doctor at the first symptoms of inflammation of the appendix will relieve possible complications and save your life.
All age groups suffer from appendicitis: children, adults, the elderly. Inflammation of the appendiceal process is especially difficult to diagnose in women, since the symptoms are similar to many gynecological diseases. Calling an ambulance in a timely manner is the only solution. Inflammation of the appendix cannot be treated; it can only be excised (the surgical process lasts no more than 1-2 hours in the first stages of the disease).
A ruptured appendix is called peritonitis and will lead to infection of the abdominal cavity, circulatory system and even death.
Appendix rupture
Pathological processes during inflammation of the appendix last two to three days. Before rupture, catarrhal changes are observed. Later, purulent and gangrenous ones occur. If surgical treatment is not performed during this period, appendicitis ruptures.
The moment of rupture can be determined by the patient's complaints. He says that the lower abdomen becomes warm. There is a feeling that it is spreading inside. A serious consequence occurs, which is called “diffuse peritonitis.”
How to tell if your appendix has burst
Inflammation of the appendix of the cecum is called appendicitis.
Among abdominal diseases that require surgical intervention, acute appendicitis ranks first. The disease appears at any age. Moreover, women suffer from it more often than men.
If the disease is not diagnosed in time and appropriate treatment is not carried out, if appendicitis bursts, then the consequences can be not only severe. High probability of death .
Symptoms of a burst appendix
The initial stage is characterized by the fact that the patient experiences pain in the abdomen, in the navel area, which spreads to the right side of the lower abdomen.
Other signs:
- Temperature increase. Often it reaches 38-40 ˚С.
- Nausea.
- Vomit.
- Chills.
- Trembling in arms and legs.
- Diarrhea.
- Pain in the back.
- False urge to defecate.
- Temporary subsidence of pain due to paralysis of nerve endings.
- Very rapid return of pain and its intensification.
- The appearance of signs of intoxication.
The occurrence of such symptoms requires immediate treatment. The patient is indicated for surgical intervention.
Symptoms of peritonitis after acute appendicitis
The symptoms of acute inflammation of the appendix are generally familiar to each of us. This is pain, first in all parts of the abdomen, then localized in most cases in the lower right quadrant. There are symptoms of intoxication - tachycardia, fever, weakness, dyspeptic disorders. All these signs indicate the clinical picture of acute appendicitis. If the appendix bursts, then the clinical picture changes; some symptoms should alert even a person far from medicine.
Stages of peritonitis
In the development of diffuse peritonitis, it is customary to distinguish three stages, each of these stages is characterized by certain symptoms.
- The irritation stage occurs at the moment of rupture of the process. The functioning of the abdominal organs at this moment is not yet impaired. Signs of a ruptured appendix at this stage include the appearance of not limited, but diffuse pain. That is, pain from the right iliac region spreads to all parts of the abdomen. Nausea intensifies, there may be repeated vomiting, and there is not tension in the muscles of the abdominal wall, but rather bloating.
- The second stage of diffuse peritonitis is the stage of imaginary well-being. Due to the fact that at this stage there is paralysis of the endings of the nerves located in the peritoneum, the pain may completely disappear. And therefore the patient believes that everything has returned to normal. At this stage, severe tachycardia, clammy sweat, and rapid pulse are noted. Intestinal obstruction occurs.
- Heat stage. Symptoms of intoxication quickly increase, peritoneal signs and dyspeptic disorders develop. Body temperature is elevated, all signs of extensive inflammation are recorded. The pain is insignificant; palpation reveals bloating. Gases practically do not escape.
- The terminal stage is usually manifested by repeated vomiting, increasing signs of intoxication, and intestinal obstruction. Cardiac activity suffers, the functions of the respiratory system, liver and kidneys are deeply impaired. At this stage, death is most often expected.
Diagnostics
Ultrasound techniques are used to make a correct diagnosis.
The presence of the disease is determined by a blood test, which will show an increased number of leukocytes.
Research is carried out to differentiate appendicitis from diseases such as:
- Gastritis.
- Intestinal obstruction.
- Stomach or duodenal ulcer.
- Acute pancreatitis.
- Pyelonephritis.
- Women's diseases are in the acute stage.
- Pneumonia.
- Acute cholecystitis.
- Urolithiasis disease.
History and medicine
For a long time it was believed that it was necessary to wait as long as possible and operate on the patient only in case of complications. In 1993, they finally determined the need for urgent hospitalization and removal of the inflamed organ before complications began. In the 40s, antibiotics began to be used, which made operations safer and more effective. True, this became the reason for a rather long period of unjustified operations for everyone. Up to 60% of the removed organs had no traces of inflammation. Most often young women were operated on. This increased the likelihood of adhesions in the peritoneum.
In the 60s of the twentieth century, laparoscopy, previously used only by gastroenterologists, became available. Gradually we learned to use this method both to diagnose the condition and to remove inflamed areas.
Features of diagnosing appendicitis in children
How to understand that a child is having an attack of appendicitis, and what will happen if complaints of abdominal pain are ignored?
The first signs of rupture in a child are similar to the symptoms that occur in adults. But children are afraid of doctors and often say that nothing hurts them. Therefore, parents should know what the symptoms of a ruptured appendix in a child are and how to identify the disease.
The cecum in children becomes inflamed unexpectedly. Their sleep becomes restless. Children are capricious, cry, refuse to eat. Vomiting begins, the temperature rises, and bowel movements become more frequent.
The child pulls his right leg towards his body and tries to relieve pain. Pain in the abdomen intensifies during movement, lying on the right side . When turning on the left side, the pain decreases.
To prevent a ruptured appendix, the child needs urgent medical attention. Otherwise, a complication in the form of peritonitis will arise.
Complications
When peritonitis develops from appendicitis rupture, it is very important to take all therapeutic measures correctly so as not to provoke additional complications. If surgical care was provided late, the patient dies from the spread of pus throughout the body. Therefore, the sooner and more effectively help is provided, the greater the chances of recovery.
If doctors quickly responded to the problem, but the patient’s health is unsatisfactory, then he may experience some consequences:
- sepsis;
- abscess;
- gangrene of organs;
- adhesions;
- liver failure.
Complications of peritonitis are very serious, so about 20% of patients die from them.
Consequences of a breakup
If the appendix perforates, its contents enter the abdominal cavity. Purulent fluid with a huge number of bacteria penetrates the blood and covers the peritoneal organs.
Infection occurs, which is called “peritonitis.” It is this condition that is fatal to humans.
It provokes the occurrence of diseases such as:
- Bacteremia. Characterized by the presence of bacteria in the blood. The infection spreads throughout the body. Metastatic foci form. The consequence of this is meningitis - inflammation of the lining of the brain, pericarditis - an inflammatory process in the outer lining of the heart, endocarditis - inflammation of the inner lining, osteomyelitis - inflammation of bone tissue. An abscess occurs, which leads to death.
- Pylephlebitis. Purulent inflammation of the portal vein and its branches occurs. The disease develops at lightning speed and can be fatal.
- Appendicular infiltrate. The inflamed tissues of the appendix and omentum, small and large intestine are soldered together.
- Thrombophlebitis.
- Sepsis.
Course of the disease
The first period of illness lasts 2-24 hours, and its symptoms are similar to many acute diseases of the abdominal organs. It is characterized by acute pain in the epigastric region or throughout the abdomen (less often, pain appears immediately on the lower right), nausea, single vomiting, and a moist tongue with a coating.
In the appendix, blood circulation and lymph movement are disrupted, dystrophic changes occur in the intramural nervous system, the appendix flows away, and siderophages accumulate in it. In the second appendicular period, one can already suspect the development of appendicitis. In a person, acute pain moves to the right iliac region, the heart rate is up to 90-100 beats per minute, the abdomen is soft, the temperature is elevated, intestinal motor activity is preserved, and there is moderate leukocytosis in the blood.
A preliminary diagnosis can be made based on positive symptoms:
- Rovzinga (pushing pressure in the left iliac region when the descending segment of the large intestine is compressed leads to increased pain on the right side);
- Voskresensky (if you run your palm over the stomach from the right ribs downwards, pain will appear on the right in the groin area);
- Obraztsova (when palpating the right iliac region with the right leg raised straight, the pain becomes stronger).
If surgical intervention was not performed in the initial stages of the disease, then the inflammation extends beyond the appendix and the terminal period begins. It is characterized by pain in the right half of the abdomen, which can pass, sharply intensify, or remain approximately the same.
The patient may also experience repeated vomiting, increased heart rate (over 100 beats per minute), the tongue becomes dry, plaque is visible on it, intestinal motility is reduced or absent, body temperature is above 38 C, the temperature in the axillary and rectal area differs by one degree.
At this stage, the Shchetkin-Blumberg symptom is positive (the pain intensifies when the hand is quickly removed from the anterior abdominal wall). Sharp pain and tension in the abdominal muscles is a sign of peritonitis (the entry of purulent contents into the abdominal cavity).
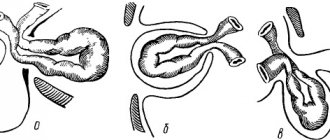
The changes that occur with superficial appendicitis are reversible, however, if the inflammatory process develops, then acute destructive appendicitis occurs. One day after the onset of the disease, the leukocyte infiltrate affects the entire wall of the appendix (phlegmonous appendicitis).
The process enlarges, a fibrinous coating appears on its surface, the wall becomes thicker and pus is released through it. If small pustules join diffuse purulent inflammation, then apostematous appendicitis is diagnosed, and if manifestations appear, then they speak of phlegmonous-ulcerative appendicitis.
Gangrenous appendicitis develops as a result of the spread of a purulent process to adjacent tissues, which will lead to thrombosis of the appendicular artery. Due to necrosis of the wall, a perforated hole appears through which pus flows out (perforated appendicitis), which leads to local peritonitis, which can develop into diffuse peritonitis.
6-12 hours after the onset of the disease, a simple one (catarrhal appendicitis) is usually diagnosed, after 12-24 hours the phlegmonous form already develops, after 24-48 hours the gangrenous form begins. After 48 hours, the appendix ruptures. However, the disease does not always proceed this way: in some cases, appendicitis remains catarrhal for several days, and in others, the appendix becomes gangrenous just a couple of hours after the onset of the inflammatory process.
Treatment
Surgery is the only treatment for a ruptured appendix. The vermiform appendix is removed open or laparoscopically.
- The operation to remove appendicitis with open access lasts about 1 hour. An incision is made with a length of 4 cm to 15 cm, depending on the thickness of the abdominal wall.
- When performing the operation using laparoscopy, 4 incisions are made on the abdomen, into which special tubes are inserted. They are called trocars. A monitor is inserted into one incision, which transmits information to a computer. The rest are filled with instruments. With their help, the surgeon removes the appendix.
Timely seeking qualified help ensures a favorable prognosis.
If a patient's appendix has burst, a thorough examination is necessary to determine the extent of damage to the abdominal cavity. After this, the doctor will be able to understand what to do. During the operation, purulent contents are removed, then drainage is installed. It helps remove any remaining pus.
What happens when the appendix is perforated?
The pathological process during inflammation of appendicitis takes from two to three days; in some people this period may lengthen slightly or, on the contrary, shorten. At this time, inflammation is limited only to the organ itself; gradual changes occur in it, which is first characterized by catarrhal phenomena, and then purulent and gangrenous. If the operation is not performed during this period, then the appendix ruptures. That is, all the purulent contents of the organ and dead tissue exit into the abdominal cavity. What to do in this case must always be decided several hours in advance, since pyogenic microbes lead to inflammation of the entire abdominal cavity and general poisoning of the body.
Acute appendicitis can stop on its own, but this happens rarely, only in exceptional cases. No one can predict how an inflamed appendix will behave, so doctors, after making a diagnosis, prefer to perform surgery in the next few hours. Only during surgery can it be determined what changes the organ has undergone, and it is after the operation that the stage of appendicitis is determined.
Postoperative period
After surgery you can and should:
- Carry out physical activity from the second day after surgery.
- Follow the diet for two days. It is allowed to consume kefir, tea, and rosehip drink. After intestinal motility is restored, pureed soups, mashed potatoes, and porridge are included in the diet. After 7 days, you are allowed to return to your normal diet.
- Take painkillers.
- Carry out detoxification therapy.
- Take antibiotics. The duration of the course is 3–5 days.
- Removal of postoperative sutures after 4–6 days.
The patient must adhere to a diet for several weeks after surgery. It is necessary to limit physical activity and exercise.
Otherwise, there is a risk of improper healing of the suture, adhesive disease and inguinal hernia develop.
Negative consequences arise for reasons such as:
- Poor nutrition.
- Refusal to wear a bandage belt.
- Weakness of the abdominal muscles.
- Lifting heavy objects.
- The presence of inflammatory processes in the peritoneum.
Europe and Asia
In the Greek lands, in recent decades there has been a decrease in the incidence of inflammation of the appendix by 75% compared to the previously known standard. If earlier per hundred thousand people acute appendicitis was diagnosed in 652, this number has changed to 164 patients on average. If in the period from 1970 to the end of the last century there were more women than men, the ratio was estimated at 1.27, then this gradually changed to the opposite state of male predominance. The mortality rate in Greece is stable, with at least 0.09 deaths among hundreds of patients.
Spanish doctors found that in the millennium there were 132 patients per hundred thousand men, and three years later - approximately 117.5 cases. Women tend to experience a more significant decrease in the incidence rate. The risk of perforation was estimated at 12.1%. Mortality after surgery is 0.38%.
In South Korea, the probability of acute appendicitis reaches 13.56 cases per 10 thousand people, with the risk of perforation being about 2.91. This country is more characterized by stability of average medical indicators.
Appendicitis and mortality
According to statistics, death from appendicitis occurs due to complications arising from ignoring symptoms and delays in seeking medical help.
Statistics on appendicitis in Russia and around the world confirm that if a patient’s death occurred under the supervision of a doctor, then he is held accountable for a medical error. For example, in the Republic of Tatarstan, due to the negligence of a surgeon during an operation, a young man whose artery was damaged died.
Mortality from appendicitis according to statistics is approximately 0.1% of the total.
Today, thanks to modern technologies, the danger during operations is minimal. In the USA in 2020, 1.5 million removals were carried out, in Russia - about 700 thousand. There were not a single deaths.
Unnecessary removal of appendicitis
In the last century, in some countries, doctors believed that the small appendage of the rectum was not particularly functional in the body. In order not to endanger the occurrence of appendicitis, they eliminated it in childhood.
After a while, consequences appeared due to unnecessary surgical intervention. Children who survived such an operation, in comparison with their peers, had a significantly worse moral and physical development.
Removal of appendicitis after the occurrence of “false” symptoms in adults results in disruption of the functionality of many systems in the body. After detailed studies, it turned out that this inconspicuous process takes an active part in the following functions:
- endocrine;
- secretory;
- lymphocytic;
- digestive;
- promotes regular bowel movements;
- has a positive effect on the microbial background;
- reacts to the slightest purulent processes in the colon.