Heart defects are anomalies and deformations of individual functional parts of the heart: valves, septa, openings between vessels and chambers. Due to their improper functioning, blood circulation is disrupted, and the heart ceases to fully perform its main function - supplying oxygen to all organs and tissues.
- Classification
- Kinds
- Mitral valve
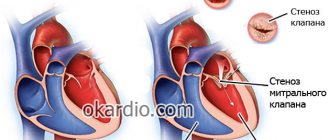
- Mitral stenosis
- Aortic defect
- Aortic stenosis
- Tricuspid area
- Heart defects in children
- Diagnostics
- Treatment
As a result, a condition develops, which in medicine is called “hypoxia” or “oxygen starvation.” Heart failure will gradually increase. If qualified medical care is not provided in a timely manner, this will lead to disability or even death. It is important to know the main causes and symptoms in order to notice the development of pathology in time.
In the majority of all clinical situations, heart defects are formed in humans due to deformations and anomalies of the aortic or mitral valve, which connect the largest vessels in the heart. Many people who hear such a terrible diagnosis immediately ask the question: “How many live with such vices?” There is no definite answer to this question, since all people are different and clinical situations are different. They live as long as their heart can work after conservative or surgical treatment.
Acquired heart disease: symptoms
Acquired heart defects are different. We will tell you more about this below. Here we list the main symptoms, since for all types of acquired heart defects the symptoms are almost the same:
- Fast fatiguability
- Discomfort or pain in the heart area
- Dizziness, less often – fainting
- Feeling short of breath (especially during exercise or lying down)
- Cardiopalmus
- Changes in skin color (pallor, bluishness)
- Heaviness in the right hypochondrium
- Swelling of the legs at the end of the day
- Dry cough, which indicates that heart failure is progressing
Acquired heart defects in adults differ in that they can produce specific symptoms. For example, hoarseness for no apparent reason (no diseases of the ENT organs), shaking of the head in rhythm with the pulse in aortic insufficiency and a number of others.
It is important to know:
acquired heart defects are dangerous. If one or another heart defect is not detected in time, sooner or later it will lead to serious consequences that can cost you your life.
If you have any of the symptoms we've outlined above, don't try to cure yourself or live with the expectation that "it will go away." It’s better to make an appointment with our cardiologist, who will thoroughly understand your situation, determine exactly whether you have a heart threshold, and tell you in detail what to do next.
Make an appointment now.
Mitral valve insufficiency
With this defect, the valve leaflets do not close completely, causing a backflow of blood from the left ventricle into the left atrium. The diseases that can lead to this type of defect are the same as with mitral stenosis. Mitral stenosis is much less common.
The reverse flow of blood that occurs with this type of defect stretches the left atrium, in which too much blood accumulates. For some time, the body uses protective mechanisms, but when its reserves are depleted, blood stagnates in the lungs, and the size of the right side of the heart increases slightly. In advanced cases, pronounced signs of heart failure appear.
Symptoms
As in the case of mitral stenosis, valve insufficiency may not make itself felt for a long time. Often such a diagnosis is an incidental finding during an annual medical examination or during a medical examination. As the defect progresses, shortness of breath appears during physical activity, and then at rest, a feeling of rapid heartbeat. A cough with scanty sputum may appear. Pains in the heart are often disturbing: aching, stabbing, pressing, and they are not necessarily associated with physical activity.
Diagnostics
The appearance of such patients has no peculiarities. Upon examination, the doctor may well suspect a defect, which is easily confirmed by instrumental examination methods (ECG, echocardiography).
Treatment
Surgical: restoration of normal dimensions of the valve ring.
The main cause of acquired heart defects
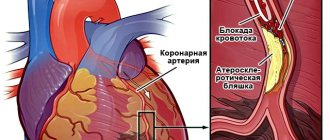
The main cause of acquired heart defects is rheumatism, atherosclerosis, and infective endocarditis. In addition to these diseases, acquired heart defects can develop due to other infectious and autoimmune pathologies.
- Infectious diseases
Bacteria, entering the blood, settle and multiply on the valves, gradually destroying them, resulting in valve insufficiency. As the body continues to fight the infection in an attempt to repair the diseased valve, the valve leaflets become hardened and subsequently fuse laterally, resulting in a narrowing of the valve (stenosis). - Autoimmune pathologies
With rheumatism and other autoimmune pathologies, the body, destroying itself, destroys, including the heart valves, as a result of which a defect usually develops (usually aortic or mitral).
Reasons for appearance
Changes in the structural structure of the valves, atria, ventricles or heart vessels, causing disturbances in the movement of blood in the large and small circles, as well as inside the heart, are defined as a defect. It is diagnosed in both adults and newborns. This is a dangerous pathological process that leads to the development of other myocardial disorders, from which the patient can die. Therefore, timely detection of defects ensures a positive outcome of the disease.
The etiology of the disease depends on the type of pathology: congenital, or arising in the process of life. The acquired type of disease is characterized by damage to the valve system. They arise due to:
- infectious lesion;
- systemic diseases;
- autoimmune pathologies;
- atherosclerosis;
- rheumatism;
- syphilis;
- cardiac ischemia.
In addition, this disease causes chronic pathologies of the heart and blood vessels, alcoholism, head injuries, dysfunction of the liver, joints (artosis, arthritis, rheumatism), as well as a hereditary factor.
The congenital form is diagnosed in 5-8 babies out of 1000. The defect develops due to viral diseases suffered by the woman during pregnancy, as well as:
- alcoholism;
- smoking;
- drugs.
Disorders can be diagnosed in infants if the woman has any degree of obesity.
Acquired heart defects: what are they?
Acquired heart defects can be different and they are divided according to different criteria. Let's talk about the main ones.
Depending on the type of lesion:
- Insufficiency is a pathology when the valve leaflets do not close completely, resulting in blood flowing back from the ventricle into the atrium during contraction.
- Narrowing (stenosis) - due to scars, the valve leaflets grow together and do not open completely, which is why not all the blood flows from the atrium to the ventricle.
Depending on the affected valve:
- Mitral valve disease
- Tricuspid valve disease
- Aortic valve disease
- Pulmonary valve disease
By the number of affected valves:
- Monovalvular defect - one valve is affected
- Simple defect - insufficiency or narrowing of one valve
- Combined defects - both insufficiency and narrowing of one valve
- Combined defects - two or more valves are affected
According to the state of blood circulation:
- Compensated defect – no circulatory failure
- Decompensated – there are signs of circulatory disorders
Types of birth defects
CHDs are characterized by a variety of heart and blood vessel defects. Some of them appear in childhood immediately after birth. Others occur hidden and are discovered in old age. There are many vices in various combinations. They can be isolated or combined. The severity of the pathology is related to the degree of hemodynamic impairment. Congenital defects are divided into the following clinical syndromes.
ASD
The most common defect is an atrial septal defect (ASD). The anomaly is a hole in the wall between the two chambers that did not close after birth. Oxygen-rich blood flows from the right atrium to the left side of the heart. This is a normal phenomenon during the prenatal period. Soon after birth the hole closes. The defect leads to increased pressure in the blood vessels of the lungs.
Attention! The most pronounced symptoms of the defect appear at a young age, when the heart rhythm is disturbed.
Since the hole does not close on its own, surgery is required, which is best done between the ages of 3 and 6 years.
VSD
A ventricular septal defect is found in 20% of children with heart defects. With a developmental anomaly, an incompletely closed hole remains in the septum. As a result, blood under increased pressure during contraction penetrates from the left to the right ventricle.
Attention! The defect threatens pulmonary hypertension. This complication makes the operation impossible. Therefore, parents of children with VSD need to promptly consult a cardiac surgeon. Children after valve correction lead a normal life.
Diagnosis of acquired heart defects
Diagnosis of acquired heart defects begins with detailed collection of information. At the initial appointment, the doctor will ask you in detail what exactly you are complaining about, what symptoms bother you, and whether you or your close relatives have other cardiovascular diseases.
After this, he will conduct a visual examination, including listening to your heart. If, in addition to your complaints, noises and displacement of the boundaries of the heart characteristic of defects are detected, the doctor will prescribe additional examinations to confirm the diagnosis, which may include:
- Electrocardiography (ECG)
will help identify various rhythm disturbances and metabolic processes in the myocardium, characteristic of heart defects. - Daily Holter ECG monitoring
will help to study the rhythmic picture in detail and identify myocardial ischemia, if any. - Echocardiography (EchoCG) with Dopplerography
is one of the most effective methods for diagnosing acquired heart defects: it will clearly show damage to the valves and help assess their severity and the degree of influence on blood flow inside the heart. - Chest X-ray
will help identify venous congestion in the lungs and determine whether there is a characteristic effusion in the pleural cavity. - Laboratory tests
will help identify changes in the blood that are characteristic of heart defects and other cardiovascular pathologies that accompany them. - and MRI of the heart
will help to study in detail the existing valve lesions and accurately formulate further treatment tactics.
Patent ductus arteriosus (PDA)
A vessel necessary in utero, it allows the fetal blood to be discharged from the pulmonary artery directly into the aorta, bypassing the non-functioning lungs. In utero, along with the oval window, it functions as a bypass in the pulmonary circulation. At the birth of a child, the ductus arteriosus loses its functional significance and normally begins to close after 15-20 hours. If its closure does not occur after 1-2 weeks of the baby’s life, this is considered a heart defect.
PDA occurs, according to cardiologists, in approximately 6-18% of cases of all heart defects, and in boys it is 2-3 times more common than in girls. In addition, there is a certain connection between the degree of prematurity and the frequency of a patent duct: the greater the degree of prematurity and the weight of the child, the later the duct closes, and special medications are used to stimulate its closure.
With PDA, blood is discharged from the aorta, where the pressure is higher, into the pulmonary trunk, and through it into the vessels and tissue of the lungs. Then the blood, without entering the systemic circulation, returns to the left half of the heart. Because of this, the blood supply to the child’s body organs decreases and blood pressure decreases. A circulatory disorder in the lungs gradually develops - pulmonary hypertension (increased pressure in the blood vessels of the lungs) and the formation of heart failure.
The manifestations of the defect depend on the width of the duct - with a narrow duct, children are almost indistinguishable from their peers, and their anomaly can be detected several years later. They usually suffer from ARVI and have a heart murmur somewhat more often than others. With a wide size, most children begin to lag behind in physical development from an early age, acute respiratory viral infections and pneumonia are common, and there are frequent complaints of fatigue, poor sucking, lethargy, shortness of breath on exertion, and paleness of the baby. Upon examination, the baby may exhibit pulse asymmetry and a decrease in diastolic (lower) pressure, and the lower the pressure, the larger the size of the duct. When listening with a phonendoscope, a special “machine” noise in the heart area is characteristic.
In diagnosing the defect, ECG, PCG and ultrasound of the heart help, in which the defect is detected, and it is possible to measure the size of the duct and estimate the amount of blood discharged through it per minute. In addition, X-rays show an increase in the size of the heart to the left. The danger of PDA lies in the early development of heart failure; in addition, children may be severely delayed in development.
When a diagnosis of PDA is made, ligation of the duct is indicated. The optimal time frame for performing this operation is 12 months - 3 years, but if complications develop, it is possible at any age. Usually, at the present stage, the operation is performed endoscopically - using small punctures at certain points of the chest, instruments and a camera are inserted into the pericardial region, under the control of a monitor, manipulations are carried out to ligate the duct and apply a staple to it, preventing it from opening again.
The second option is to insert a catheter with a special device inside, called an occluder, through one of the child’s large veins. Essentially, this is a plug that is placed inside the duct across the vessel and plugs it from the inside. The process of complete recovery after surgery takes about a year, and after that the child is no different from his peers.
Back to contents
Treatment of acquired heart defects
Treatment of acquired heart defects is a complex process that includes medication, a special diet and lifestyle adjustments, and in severe cases, surgery. Unfortunately, modern medicine is not yet able to completely remove already formed valve lesions and it may be necessary to replace them with prostheses. That is why it is important to identify acquired heart defects as early as possible and stop the development of the pathological process in time.
Conservative treatment
The main goal of conservative treatment of acquired heart defects is to choose the right medications and lifestyle, taking into account all important factors, in order to stop further progression of the disease.
This can only be ensured by an integrated approach to the treatment of acquired heart defects, with the involvement of other specialists - a rheumatologist, neurologist, therapist, cardiac surgeon and others. It is this comprehensive approach that we practice in our network of clinics.
Conservative treatment of acquired heart defects includes:
- Treatment of the underlying disease resulting in the development of heart disease
- Treatment of complications: for example, normalization of heart rhythm, treatment of heart failure and others
- Normalization of systemic circulation
- Prevention of recurrence of the underlying disease
- Prevention of thrombosis
Surgery
If our specialists diagnose you with a severe heart defect, you will definitely need to consult a cardiac surgeon, who will assess whether you need surgery.
Among the methods of surgical intervention for heart defects, the most effective are:
- Catheter balloon valvuloplasty
A balloon catheter is inserted into the valve area. The balloon inflates, expanding the narrowed hole. - Commissurotomy (valvotomy)
Dissection of adhesions, which is performed on the open heart during artificial circulation. - Valve replacement
The affected valve is excised. In its place, an artificial one is installed - mechanical or biological.
Classification
In medicine, all heart defects are divided based on the mechanism of their formation into: congenital and acquired .
An acquired defect can develop in a person from any age group. The main reason for its development today is rheumatism, hypertension, syphilis, ischemic heart disease, and cardiosclerosis. This disease occurs in people of working age and the elderly. More than 50% of all clinical cases involve damage to the mitral valve and only about 20% damage to the semilunar valve. The following types of anomalies also occur:
- prolapse. The valve protrudes or swells greatly, with the valves everting into the heart cavity;
- stenosis. Develops as a result of post-inflammatory cicatricial adhesions of the valve leaflets, which significantly reduce the lumen of the opening;
- failure. This condition develops due to sclerosis of the valves. They are shortened.
Congenital heart disease begins to form in the fetus during the period of its intrauterine development, due to improper formation of systems and organs at the stage of formation of groups of cells. In medicine, there are two large groups of reasons that lead to this:
- internal. All reasons are directly related to hormonal changes, as well as hereditary predisposition on the mother’s or father’s side;
- external. The development of heart defects can be caused by a poor environmental situation, maternal illness during the entire period of pregnancy, or taking synthetic medications.
Heart valves
Classification according to the number of affected valves and holes:
- simple or “clean”. In this case, abnormal changes are observed exclusively in one valve or narrowing of only 1 hole occurs;
- complex. In this case, a combination of two or more violations occurs. For example, insufficiency of 1 valve occurs along with a narrowing of 1 hole;
- combined heart defects. The most complex combination that poses a serious threat to health and life.
Classification by localization:
- valve defects;
- septal defects – upper, lower and middle.
Classification according to hemodynamic status:
- compensated heart defects;
- subcompensated. The course of the disease occurs with incoming decompensation;
- decompensated. They are characterized by the development of circulatory failure, which is fraught with disastrous consequences. People live with this disease for a short period of time. Only a cardiologist can tell approximately how much time is allocated for them, after diagnosis, conservative or surgical treatment.
Cardiotrophic diet
Cardiotrophic diet
– one of the key factors in the successful prevention of acquired heart defects. Her menu includes:
- Dairy products – milk, kefir, yogurt, cottage cheese, mild cheese
- Dishes made from dairy products - cottage cheese casseroles, puddings, cheesecakes, dumplings and others
- Boiled meat - lean beef or pork, veal, rabbit meat, chicken, liver
- Fish dishes
- Boiled or baked potatoes
- Stewed vegetables (beets, carrots, cauliflower)
- Fresh cucumbers, tomatoes, lettuce, green onions, dill, parsley
- Fresh fruits and berries
- Vegetable oil
- Butter
- Cereals – buckwheat, oatmeal, barley
- Eggs
- Vegetarian soups
- Veal broth soups
- Surrogate coffee with milk
- Weak tea
- Rosehip decoctions
- Dried fruit compotes (prunes, dried apricots or raisins)
- Kiseli
- Fruit and berry juices
Treatment with folk remedies
Traditional medicine offers many recipes that will help cure manifestations of heart disease.
Alternative methods of treating the defect are based on the use of the following medicinal herbs, vegetables and berries:
- Drops based on lily of the valley. Pour alcohol into the flowers, leave, strain and take 15 k/3 times a day.
- Potato diet. During the day (6 times), eat 1 kg of boiled unsalted potatoes in small portions.
- Mint infusion. Brew a teaspoon of leaves with boiling water (300 ml), leave. Drink the strained one-day infusion 3 times a day on an empty stomach.
- Beetroot juice with honey in a 2:1 ratio. Take in small portions to support cardiac function.
- Grape juice. Drink in the morning before meals. Especially recommended for older people.
- Tincture of calendula. 1 tbsp/1 l. vodka, leave for up to a week, strain. Take 20 ml/up to 3 times a day.
- Hawthorn tincture. 2 tsp/0.5 l. boiling water, leave for 24 hours, strain. Take 5 ml/2 times a day. The course of treatment is 1 month.
- Coltsfoot tincture. Infuse for 3 days 20 gr. leaves filled with 1 liter. boiling water Take the finished infusion 15 ml/2 times a day after meals.
- Motherwort tincture. Pour boiling water over the leaves (20 g/1 l). Drink the strained daily infusion 10 ml/3 times a day after meals.
Many tinctures can be bought ready-made at the pharmacy. They improve heart function, have a calming effect, and strengthen the blood vessels of the heart. Their use successfully answers the question of whether heart disease can be cured.
Heart disease is a disease that requires serious attention to health. Strengthening the immune system and prevention will give positive results.
Lifestyle
Prevention of acquired heart defects cannot be effective without lifestyle correction:
- Stop smoking and drinking alcohol forever, including weak beer and dry wines
- Eliminate too fatty foods and dishes from your diet
- Don't eat fast food
- Lead an active lifestyle, move more, play sports (for example, swimming), but do not overstrain your body with excessive physical activity, as this can lead to various complications
- Don't be nervous about trifles
- Cure any infectious diseases, including colds, in a timely manner
- Have annual check-ups with a cardiologist and the tests he prescribes for you, especially if you are over 50 years old
Note:
These are only general recommendations for the prevention of acquired heart defects. Our specialists will help you choose the right diet for you and adjust your lifestyle during the treatment process.
Most importantly, remember:
Acquired heart defects are dangerous pathologies that can develop for years without manifesting themselves. The earlier a particular defect is diagnosed, the easier it is to stop the development of the pathological process and normalize the normal functioning of the heart valves and the entire cardiovascular system as a whole.
Therefore, if you feel any discomfort in the heart area, do not self-medicate according to recommendations from the Internet. First of all, it won't help. Secondly, with improper treatment you can speed up the pathological process and worsen your condition.
Make an appointment with our specialists, who will thoroughly understand your situation, make an accurate diagnosis and provide safe treatment that will really help you.
Make a choice in favor of professional medicine!
Causes
In most cases, hereditary factors that cause congenital heart defects are considered. Also, the fetus can be affected by external factors, which are often combined with the same hereditary predispositions.
Genetic predisposition
Most often it is presented in the form of local mutations or chromosomal changes that lead to major or minor malformations. Today, trisomies of different pairs of chromosomes are distinguished, which cause congenital heart disease in almost 8% of cases. The most common, occurring against the background of gene mutations, are atrial septal defects, ventricular septal defects, electrical conduction disorders, and blood outflow disorders.
Etiological factors of influence
In the development of congenital heart defects, a significant role is played by unfavorable factors, most often directed externally to the organism developing in the womb. Under their influence, certain parts of the DNA are mutated, as a result of which the normal formation of the cardiovascular system is disrupted.
Unfavorable impact factors are:
- Physical phenomena, among which radioactive radiation has a particularly negative effect on the fetus.
- Chemical components found in various alcoholic beverages, cigarettes, some medications, and mutagens are also found in low-quality paints and varnishes.
- Biological influence can be carried out through various infectious diseases that occur in a pregnant woman. Most often, heart defects are caused by rubella; diabetes mellitus, systemic lupus erythematosus, and phenylketonuria can also lead to congenital changes.
Relationship between congenital heart disease and gender
In the 70s of the last century, studies were conducted that confirmed the connection between heart defects and gender. For this purpose, more than 30 thousand patients were examined for congenital heart defects, as a result of which congenital heart defects were divided into “neutral”, “female” and “male”. For example, girls are more likely to have Lautembacher's disease, patent ductus arteriosus, and are also more likely to develop a secondary atrial septal defect. Stenosis and coarctation of the aorta are more common in boys. The following are considered “neutral”: Ebstein's anomaly, complete atrioventricular septal defect, pulmonary stenosis, septal defect between the aorta and pulmonary artery, and ventricular septal defect.
Doctors in our clinics
KMN
Tartakovsky Lev Borisovich
Head of the Department of Cardiology and Deputy Chief Physician for Clinical Expertise at the Leninsky Clinic, functional diagnostics doctor, cardiologist, arrhythmologist, Candidate of Medical Sciences
Clinic on Arbat Clinic on Leninsky
Reviews Video
KMN
Vasyutina Ekaterina Ivanovna
cardiologist, functional diagnostics doctor, arrhythmologist, candidate of medical sciences, doctor of the highest category
Clinic on Arbat Clinic on Leninsky
Reviews
Kovaleva Anzhelika Aleksandrovna
cardiologist, functional diagnostics doctor, arrhythmologist, ultrasound diagnostics doctor, doctor of the highest category
Clinic on Arbat Clinic on Babushkinskaya
Kolesova Marina Borisovna
cardiologist, arrhythmologist, functional diagnostics doctor, doctor of the highest category
Clinic on Babushkinskaya
KMN
Sokolova Svetlana Olegovna
cardiologist, functional diagnostics doctor, arrhythmologist, candidate of medical sciences
Clinic on Arbat
DOCTORS
Diagnostics
Diagnosis of the disease includes the following types of medical measures:
- Echocardiography, which is performed fetally. With its help, signs of congenital heart disease are diagnosed even during pregnancy.
- Phonocardiography. Recording noise for subsequent evaluation.
- Carrying out an ultrasound of the heart after the birth of a child.
- Electrocardiography.
- Chest X-ray. X-rays make it possible to assess the size, contours and location of the heart.
- Pulse oximetry. An examination through which it is possible to obtain information about the oxygen content and its deficiency in peripheral tissues.
- Tomography. Used in cases of a rare type of birth defect.
- Blood test: general and biochemical. Thanks to the analysis, it is possible to assess the degree of blood saturation.
It is worth noting that not all of the above diagnostic measures are carried out for one case of the disease. The doctor himself decides what tests he needs to make an accurate diagnosis.
Prevention of complications
Tactics for preventing complications in adolescents and children include medications and changes in their diet (limiting salt and using high-calorie foods with relatively little fluid). These measures reduce the load on the heart.
Patients who have serious heart defects or have had surgery to repair cardiac abnormalities should follow the following recommendations:
- Take antibiotics before visiting the dentist and before certain surgeries (for example, bowel or bladder surgery). These antibiotics are used to prevent a serious heart disease called endocarditis.
- Taking good care of your teeth and gums will reduce the risk of infection spreading in your body, which can affect your heart.
Video Heart defect. Symptoms. Operation
4.50 Aug. rating ( 89 % score) - 2 votes - ratings
Normal fetal circulation
Blood circulation in the fetus is carried out differently than in children and adults.
Normally, all the blood going to the heart from the body (low-oxygen venous blood) passes through the right atrium and then through the right ventricle to the pulmonary artery and from there to the lungs. Here the blood is saturated with oxygen from the pulmonary alveoli, through which carbon dioxide is released. This blood, which is rich in oxygen and now called arterial blood, returns from the lungs to the left atrium and left ventricle, and from there it flows from the heart to the body through a large artery called the aorta. Then it spreads through smaller arteries to all tissues and organs.
The fetus is in the uterus, where there is no access to the air needed for breathing. Instead, it receives oxygenated blood from the mother's placenta through the umbilical cord while the lungs fill with fluid. Since the fetus does not breathe, only a small amount of blood must pass through the lungs to keep them alive. The path by which blood circulates through the heart and lungs differs between the fetus and the newborn.
Before birth, most of the venous blood entering the right side of the heart bypasses the fluid-filled lungs and passes through two different short paths, which are:
- Foramen ovale located between the two upper chambers of the heart, the right atrium and the left atrium
- The ductus arteriosus (ductus arteriosus), which is a blood vessel connecting two large arteries, the aorta and the pulmonary artery.
Such communication pathways change immediately after birth. As it passes through the birth canal, fluid is squeezed out of the newborn's lungs. With the first breath of a newborn, the lungs are filled with air that is saturated with oxygen. Next, the umbilical cord is cut and the newborn begins to receive oxygen through the lungs.
Thus, the foramen ovale and ductus botalli are no longer needed and they normally close within the first few days to a few weeks of life. As a result, the newborn's blood circulation becomes the same as that of an adult. Sometimes the foramen ovale does not close, but in most cases this condition does not cause any health problems.
Treatment methods
Acquired heart disease is a problem that can only be corrected through surgery. Medicines are also used. They prevent complications and relapses of primary pathology, help correct heart rhythm disturbances and avoid heart failure.
All patients should periodically visit a cardiologist to determine when surgical treatment is necessary. Among the surgical techniques used are:
- Mitral commissurotomy. During the operation, the valve leaflets are disconnected and the atrioventricular opening is widened. This leads to partial or complete elimination of stenosis and helps eliminate severe hemodynamic disturbances.
- Valve replacement. If insufficiency occurs, the damaged valve is replaced with an artificial one.
- Commissurotomy with prosthetics. This may be necessary for combined defects.
The duration of such procedures is determined by the attending physician. The sooner the violation is eliminated, the lower the likelihood of complications.
Hemodynamic disturbance
When these factors-causes are exposed and manifested in the fetus during development, characteristic disturbances occur in the form of incomplete or untimely closure of the membranes, underdevelopment of the ventricles and other anomalies.
Intrauterine development of the fetus is distinguished by the functioning of the ductus arteriosus and the oval window, which is in an open state. The defect is diagnosed when they still remain open.
The presented pathology is characterized by the absence of manifestations in intrauterine development. But after birth, characteristic disorders begin to appear.
Such phenomena are explained by the time of closure of the communication between the systemic and pulmonary circulation, individual characteristics and other defects. As a result, the pathology can make itself felt some time after birth.
Treatment methods for heart disease are described in this article.
Often, hemodynamic disorders are accompanied by respiratory infections and other concomitant diseases. For example, the presence of a pale type pathology, where arteriovenous discharge is noted, provokes the development of pulmonary hypertension, while a blue type pathology with a venoarterial shunt promotes hypoxemia.
The danger of the disease in question lies in the high mortality rate. Thus, a large discharge of blood from the pulmonary circulation, provoking heart failure, in half of the cases ends in the death of the baby before the age of one, which is preceded by the lack of timely surgical care.
The condition of a child over 1 year of age improves noticeably due to a decrease in the amount of blood entering the pulmonary circulation. But at this stage, sclerotic changes often develop in the vessels of the lungs, which gradually provokes pulmonary hypertension.
Symptoms appear depending on the type of anomaly, the nature and time of development of circulatory disorders. When the cyanotic form of the pathology develops in a sick child, a characteristic blueness of the skin and mucous membranes is noted, which increases its manifestation with each strain. The white defect is characterized by pallor, constantly cold hands and feet of the baby.
The baby himself with the presented disease differs from others in hyperexcitability. The baby refuses to breastfeed, and if he starts sucking, he quickly gets tired. Often, children with this pathology are diagnosed with tachycardia or arrhythmia; external manifestations include sweating, shortness of breath and pulsation of neck vessels.
In the case of a chronic disorder, the child lags behind his peers in weight, height, and there is a physical delay in development. As a rule, at the initial stage of diagnosis, a congenital heart defect is listened to, where heart rhythms are determined. In the further development of the pathology, edema, hepatomegaly and other characteristic symptoms are noted.
Complications include bacterial endocarditis, venous thrombosis, including cerebral thromboembolism, congestive pneumonia, angina syndrome and myocardial infarction.
Development mechanism
For full development, the fetus needs its own blood circulation, so the cardiovascular system develops earlier than others - formation begins already on the 14th day after conception. After 22 days, the heart begins to pulsate, and after a few more days the blood begins to circulate. And, although the cardiac system during this period is still only at the initial stage of formation, much depends on how the processes of fetal development proceed, the condition of the mother and external factors.
Congenital malformations of the cardiovascular system develop from 14 to 60 days from conception. With a normal pregnancy and proper development of the fetus, by the second month the baby’s heart should be formed:
- septa grow, the heart becomes four-chambered;
- the arterial trunk divides into the aorta and pulmonary artery;
- the ventricle is divided into two halves;
- heart valves are formed.
But the influence of negative factors leads to a failure in the development of the cardiac system - this is how congenital defects are formed.
From the 12th week of pregnancy, you can determine what pathologies may develop in the child. This allows parents to decide whether to terminate or continue the pregnancy. But, it should be borne in mind that there is a possibility of a medical error and the child may be born healthy. In any case, suspicion of congenital heart disease in a child allows you to prepare for possible operations that must be performed immediately after birth in order to save his life.
Prognosis and prevention
Acquired heart disease, in which changes in the structure and functions of the valve are insignificant, the heart muscle is not affected, can proceed for a long time in the compensation stage. In this case, the patient’s ability to work is not impaired, and he is not even aware of his condition.
The prognosis worsens significantly when compensatory mechanisms are exhausted. To predict possible consequences, consider:
- The presence of repeated rheumatic attacks, intoxications and infectious pathologies.
- Level of physical activity and emotional stress.
- Pregnancy and childbirth.
If the valve apparatus is severely damaged and the disorders continue to develop, heart failure occurs. In the acute period, the probability of death is very high.
Mitral stenosis has a poor prognosis. If there is a deviation, the heart muscle cannot maintain the compensation stage for a long time. With this diagnosis, congestion and circulatory failure develop very quickly.
Whether the patient will remain able to work depends on many factors. This is influenced by the amount of physical activity, the fitness of the body and the general health of the patient.
If there are no signs of decompensation, then no performance problems occur. If circulatory failure develops quickly, the patient is allowed to engage in light work or is recommended to completely abandon work.
Acquired heart disease in adults requires a responsible attitude towards one's health. The patient must observe moderation in physical activity, stop drinking alcohol and smoking, engage in physical therapy, and undergo preventive treatment in sanatoriums.
To avoid the development of defects, it is necessary to take measures that will prevent syphilis, rheumatism, and septic conditions. To do this, the body needs to be constantly trained, hardened, and sanitized foci of infection.
If the defect has already formed, then efforts must be made to prevent heart failure. To do this, all patients are recommended to:
- Regularly walk in the fresh air and do gymnastics.
- Eat nutritiously with a predominance of protein foods.
- Use as little salt as possible.
- Avoid sudden changes in climatic conditions. It is especially undesirable to climb mountains.
- Do any sports.
The patient should visit a cardiologist regularly. Routine examinations will help control the rheumatic process and promptly notice the prerequisites for heart failure.
In this article, we will look at the main signs of heart disease in adults.
Tetralogy of Fallot
Tetralogy of Fallot is the most severe and most common defect in newborns. Anatomically - combined, with a violation of the exit from the right ventricle of the pulmonary artery and its narrowing, a large hole in the interventricular septum, dextraposition (located on the right, and not on the left, as is normal) of the aorta.
Symptoms: cyanosis even after light exertion, attacks with severe shortness of breath and loss of consciousness develop. The functioning of the stomach and intestines is disrupted, there are nervous system disorders, and the child’s growth and development are slowed down.
Treatment: in not too severe cases - surgery to eliminate stenosis (narrowing) of the pulmonary artery.
Prognosis: unfavorable. Unfortunately, children with severe cyanosis and profound developmental disorders cannot live long.
Lifespan
The easier the pathological process is, the higher the life expectancy. Life expectancy is also influenced by the prescribed treatment. Conservative therapy should be present in the treatment process.
But usually conservative treatment is not enough. In this case, surgical intervention is required. However, only as prescribed by a doctor!
Only a specialist can decide on further treatment. Pay attention to the localization of the affected process, as well as the presence of acute symptoms. Therefore, a severe course of the disease requires adequate treatment, timely diagnosis and an integrated approach!
Acquired heart defects develop as a result of the negative influence of external factors. They appear in a person throughout life and lead to dysfunction of the valve apparatus and heart. Pathology requires treatment, which most often consists of surgical procedures. It is important to carry out therapy in a timely manner, since with this diagnosis there is a high probability of heart failure.
Types of congenital heart disease according to Fridley
The classification is based on the most severe syndromes characteristic of each group of congenital heart disease.
| Leading syndrome | Types of violations | Vice |
| Arterial hypoxemia, hypoxemic status | Mixing of arterial and venous blood | Fallot's disease |
| Decreased pulmonary blood flow | Pulmonary stenosis | |
| Complete separation of the pulmonary and systemic circulation | Aplasia, ventricular hypoplasia | |
| Closure of the ductus arteriosus | Atresia of the pulmonary trunk | |
| Heart failure (acute, congestive), cardiogenic shock | Overload with large volume of blood | Aortic stenosis |
| Increased resistance | Stenosis or atresia of the pericardial vessels | |
| Myocardial damage | Hypoplasia of the right ventricular myocardium | |
| Closure of patent ductus arteriosus | Underdevelopment of the heart chambers, three-chambered heart | |
| Arrhythmia | Atrioventricular blocks | Fallot's defects, Eisenmenger's syndrome |
| Paroxysms of tachycardia | Arteriovenous aneurysm | |
| Fibrillation | The only ventricle of the heart | |
| Flutter | Cardiac inversion, venous sinus defect |
How is congenital heart disease treated?
Treatment of congenital heart disease depends on the severity of the pathology, the age of the child and concomitant diseases. In most people, congenital heart disease is in the compensation stage and does not pose a threat to health throughout life. To maintain this condition, monitor your health and adhere to several rules:
- Get your heart checked in a timely manner.
- Avoid heavy physical activities and limit yourself to light sports: gymnastics, swimming or physical therapy.
- Maintain a daily routine and get enough sleep.
- Eat right, limit consumption of foods high in cholesterol. Control the amount of salt consumed and maintain a drinking regime.
- Avoid nervous tension, protect yourself from stressful situations.
Drug therapy is aimed at reducing symptoms of the disease. To do this, medications are prescribed aimed at normalizing breathing, reducing blood pressure, and eliminating tachycardia. Defects of the “white” type can be permanently maintained with drug therapy without surgical intervention.
“Blue” anomalies in 90% of cases require surgery in early childhood. The success of the operation depends on its timeliness. More than 70% of operations guarantee a complete recovery of the child. There are cases where operations on a child’s heart were performed in the womb. But these very complex manipulations are not used as often as necessary, since most hospitals do not have the necessary equipment and highly qualified specialists.
There are ways to perform operations for congenital heart disease:
- closed - the intervention is performed on the vessels without affecting the heart;
- open – abdominal heart surgery is performed.
If the patient's life is in danger, emergency operations are performed. In most cases, they are performed at an early age or immediately after birth. Emergency interventions are also carried out in severe conditions, but at the same time it is possible to prepare for the operation and conduct all the necessary examinations.
Planned interventions are carried out if there is no direct threat to life, but surgery is necessary so that the child’s condition does not worsen. In some cases, one surgical intervention is sufficient, but in complex situations, repeated operations may be required.
After surgery, a recurrence of the defect may occur - vascular stenosis, valve insufficiency, coarction of the aorta. According to statistics, less than half of children with relapses live more than 10 years. When using prosthetics, the following problems arise: the child grows out of the prostheses and the need for repeated intervention arises, therefore, if it is possible to delay the operation, it is performed as late as possible.