How to determine that it is the ovary that hurts. Causes of pain in the ovaries and advice from doctors. It is extremely rare that a woman herself can determine where (which organ in the pelvis) pain occurs, the ovaries are located in the lower abdomen on the right and left (lateral areas), but in these areas there are also the intestines and fallopian tubes, so most often a woman turns to a gynecologist with complaints for pain in the lower abdomen.
In order for a doctor to make a diagnosis, it is important when pain appears in the middle of the cycle, does not depend on the menstrual cycle, appears suddenly or constantly. The doctor is also interested in the nature of the pain:
- acute pain – characterizes an acute condition, for example, with ovarian apoplexy, appendicitis;
- dull, aching pain - characteristic of inflammatory diseases in the pelvis, can also occur after ovarian stimulation;
- cramping pain is more common when there is a threat of miscarriage.
And the most important thing is to make a correct diagnosis and not self-medicate, but to visit a gynecologist.
Moreover, for each period of a woman, pain in the ovarian area should always be alarming.
Thus, in women of reproductive age, pain in the area of the projection of the ovaries is often associated with inflammation, ovulation, less often with cysts in the ovaries, and in the menopause it is always necessary to exclude neoplastic processes.
How to understand that the right or left ovary hurts?
Before talking about the pathology of the uterine appendages, you need to understand one simple thing: if a woman says that her ovaries hurt, this does not always mean that the organ really needs treatment. Often completely different conditions are mistaken for discomfort in the projection of the gonads:
- Intestinal pathology. Pain in diseases of the colon can be localized on the right and left in the groin area, and at home it is impossible to distinguish one problem from another. Associated symptoms speak in favor of problems in the intestines: constipation or diarrhea, flatulence, bloating, heaviness in the epigastrium, etc.
- Osteochondrosis. The exacerbation of this disease occurs at an increasingly earlier age, and rarely do any women boast of the absence of problems. With osteochondrosis, there is pain in the lower back, sacrum, coccyx, unpleasant sensations arise in the perineum, on the thigh, in the groin area. When some nerve fibers are pinched, the sensations that arise can imitate the pain characteristic of the pathology of the pelvic organs.
- Vegetovascular dystonia. This disease causes pain in the chest, neck, lower back, stomach, and legs. The symptoms of VSD are different, and sometimes it is quite difficult for a doctor to identify the source of the problem in the variety of complaints. Often, women suffering from vegetative-vascular dystonia report rapid heartbeat, changes in blood pressure, and numbness in the arms and legs. Discomfort can also be felt in the projection of the ovaries.
How to understand whether it is the left or right ovary that hurts? There are no specific symptoms of gonadal pathology. The following signs speak in favor of diseases of the appendages:
- Unpleasant sensations are associated with the phases of the menstrual cycle.
- Pain occurs against the background of previously identified pathology of the appendages (using ultrasound).
- Severe symptoms are accompanied by infertility.
- Natural mucous discharge changes: it intensifies, and admixtures of blood or pus appear.
Expert opinion
Svirid Nadezhda
Obstetrician-gynecologist
expert
It is important to know: the ovaries hurt when their capsule is stretched. This happens with large formations of the appendages (tumors and cysts), as well as against the background of an active inflammatory process. In other situations, you should look for another source of discomfort.
Yesterday evening there was not too severe pain in the right lower abdomen. I didn’t go to the doctor. There is an ovarian cyst. By morning the pain intensified and my stomach became swollen. I called my doctor, he says that not only the cyst, but also the appendix can hurt on the right. How to understand that it is an ovarian cyst that hurts and how to distinguish it from appendicitis? Elena, 21 years old.
Appendicitis and complications due to ovarian cysts are very similar. In both situations, pain is noted in the lower abdomen on the right. It is recommended to do an ultrasound of the pelvic and abdominal organs. You need to urgently consult a doctor - without consulting a surgeon and gynecologist, it will not be possible to make a diagnosis.
Pathological causes
If the ovaries begin to hurt, unfortunately, there can be many pathological reasons. Soreness is caused by inflammatory processes occurring in the appendages, disruption of tissue structure, malfunctions, and neoplasms localized in the glands. All possible reasons are discussed in detail below.
We recommend watching a video about inflammation of the appendages in women.
Watch the full episode here:
https://youtu.be/RSJ_31GJanU
Ectopic pregnancy
Normally, the fertilized egg should be in the uterus, but in some cases it remains in the fallopian tube and begins to develop and grow there. The tube gradually stretches, which is accompanied by pain localized closer to one of the ovaries. The pain is one-sided, at first weak and almost imperceptible, but as the ovum enlarges, it intensifies.
An ectopic pregnancy in the fallopian tube, which unfortunately cannot be preserved under any conditions.
With an ectopic pregnancy, all the signs of conception occurring are observed: delayed menstruation, swelling, enlargement and increased sensitivity of the mammary glands, possible nagging pain in the lower abdomen, general malaise, nausea. But the fertilized egg is not visualized in the uterine cavity during ultrasound.
Ectopic pregnancy. Interesting video from the best gynecologist!
An ectopic pregnancy lasts about 6-9 weeks, after which it is inevitably interrupted due to rupture of the fallopian tube. In this case, acute pain occurs in the abdominal cavity, internal bleeding begins, which, with significant blood loss, leads to fainting and shock.
Inflammatory diseases
Often the ovaries begin to ache due to inflammatory processes localized in them, caused by the following gynecological diseases:
- Adnexitis is also called salpingoophoritis. This disease is characterized by inflammation affecting the uterine appendages: the ovaries and fallopian tubes. The inflammatory process can be unilateral or bilateral. The main reason is infections that penetrate from the uterus, intestines, with the flow of lymph or blood. Symptoms: disruption of the menstrual cycle, serous or purulent vaginal discharge, pain in the lower abdomen on the side, increased body temperature.
- Oophoritis is an inflammation of the ovaries, which is much less common than adnexitis. The reasons are the same, the symptoms are similar, but usually less pronounced.
Since the main cause of inflammatory diseases is infections, and their frequent causative agents are bacteria, treatment will necessarily include taking antibiotics , selected individually after analysis to identify microorganisms and determine their sensitivity to drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed to relieve pain. After eliminating acute symptoms, physiotherapeutic procedures are prescribed to speed up recovery: electrophoresis, paraffin and UHF therapy.
Cysts
A cyst is a fluid-filled cavity that can develop in the ovary from a follicle. Cystic neoplasms that are small in size do not make themselves felt. But as the ovaries increase in size, they begin to hurt: the sensations are usually aching or pulling, occur on one side, and intensify after sexual intercourse or physical activity. Heaviness and discomfort often occur at the site of the cyst. Disruptions of the menstrual cycle are possible: amenorrhea (absence of menstruation), an increase or decrease in the duration of menstruation, scanty or, on the contrary, heavy discharge, the so-called “daub” in the intervals between critical days.
Cysts can lead to some complications:
- Torsion. If the cyst on the ovary is secured with a pedicle, it may become twisted. This phenomenon provokes an acute circulatory disorder and is accompanied by symptoms: severe and sharp pain (sometimes spreading to the entire peritoneum or radiating to the rectum, lower back), weakness and malaise, lightheadedness or fainting, severe nausea and vomiting.
- Break. If the cavity is filled with fluid, stretched and thinned, the cyst may rupture with the inevitable spillage of the contents into the abdominal cavity, which threatens peritonitis. A rupture may have symptoms such as abdominal pain, weakness, and nausea.
We recommend the video!
What is an ovarian cyst? Should it be removed? Cysts are often formed due to hormonal imbalances and ovarian dysfunction. Sometimes normalization of hormonal levels leads to regression of the neoplasm - independent resorption. For small sizes, wait-and-see tactics are used. If the cyst begins to grow rapidly, surgical removal is indicated. But cystic neoplasms often recur and become multiple, so it is important to find and eliminate the cause.
With a significant size of the cyst, a noticeable increase in the volume of the woman’s abdomen is likely.
Polycystic
Polycystic disease, in medical practice called polycystic ovary syndrome, is a condition in which the functioning of the ovaries is disrupted (usually due to endocrine disruptions, chronic inflammation, problems in the functioning of the hypothalamic-pituitary system).
On the left is a healthy ovary, on the right is polycystic ovary syndrome.
With the disease, multiple cluster-like cysts form on the appendages, ovulation becomes irregular and rare or absent.
Due to hormonal disorders, weight gain, hirsutism (male-pattern hair growth in women), changes in figure, problems with conception, and depression are observed. How to treat polycystic ovary syndrome?
Video from the channel © EXPERT Speaks The treatment is complex, prescribed by a doctor after a full examination and establishment of the exact reasons why the ovaries began to hurt and their polycystic disease developed. Therapy includes weight stabilization, normalization of hormonal levels, taking vitamin supplements and physiotherapeutic procedures.
Ovarian apoplexy
Ovarian apoplexy is hemorrhage into its cavity as a result of vascular damage. The condition occurs due to injury, surgery, cysts and tumors, rough sexual intercourse or intense physical activity (especially during ovulation).
Hemorrhage into the ovarian cavity (apoplexy) requires emergency care. At the first symptoms, consult a doctor immediately! The picture shows a hemorrhage in the left ovary.
With apoplexy, there is a sudden sharp pain in the side of the abdominal cavity, dizziness and weakness, attacks of nausea, decreased blood pressure, lightheadedness or complete loss of consciousness. Symptoms and their severity depend on the volume of blood lost.
The professor tells interesting facts about ovarian apoplexy... We recommend viewing!
Apoplexy requires urgent hospitalization. If the hemorrhage is minor, complete rest and bed rest, hemostatic drugs, cold to stop bleeding (ice on the stomach), and antispasmodics to relieve spasms are prescribed. Once the condition has stabilized, the doctor may recommend a course of physiotherapeutic procedures. And in case of severe hemorrhages, surgical intervention is indicated to open the cyst that provoked the hemorrhage or resection of the ovary.
Tumors
Ovarian tumors can be benign or malignant. But in both cases, in the early stages of development they are asymptomatic; the first signs begin to appear as the volume of tumors increases.
Typically, tumors disrupt the functioning of the appendages and provoke disruptions in the menstrual cycle, often leading to infertility due to the absence or decrease in the number of ovulations.
A large neoplasm compresses not only the ovary with the fallopian tube and the uterus, but also neighboring organs: kidneys, intestines, bladder. In such cases, numerous symptoms are observed: stool disorders, rare or frequent acts of urination, pain when emptying the bladder or intestines, spontaneous miscarriages during pregnancy, an increase in the size of the abdomen, and deterioration in general condition. In the video, a leading gynecologist will tell you what to do with a problem such as ovarian tumor .
All tumors require surgery. The removed tumor is sent to the laboratory for histological examination for identification, that is, to determine its nature. In case of frequent relapses and oncological diseases, resection of the appendage or hysterectomy can be performed - complete removal of all reproductive organs. For cancer, chemotherapy is prescribed to destroy lesions and prevent metastases.
Hormonal disorders, taking certain medications
The functioning of the ovaries is disrupted due to hormonal imbalances, and in some cases the appendages may hurt. Violations are possible with endocrine diseases, ovarian dysfunction, taking hormonal drugs, ovarian hyperstimulation during the IVF protocol.
Surgical interventions
The ovaries may hurt after surgical interventions: laparoscopy, biopsy or puncture of the appendages, surgical removal of cysts. During operations, the tissues of the paired sex glands are injured, which is accompanied by pain. But if everything went well, and the woman follows the surgeon’s recommendations, the sensations will soon pass.
In some cases, surgical interventions lead to complications such as bleeding, infections, adhesions, and inflammation. Then the pain intensifies, accompanied by an increase in body temperature and malaise. Antibiotics will be required. In case of suppuration, a repeat operation is performed to remove the pathological contents.
Pathologies of other organs
Often, when the lower abdomen begins to hurt on one side or both sides at once, a woman thinks that the reason lies in the ovaries. But pain can be caused by pathologies of other internal organs, such as:
- appendicitis;
- colitis (inflammation of the mucous membranes of the colon);
- cystitis;
- twisting of intestinal loops;
- intestinal obstruction.
How to understand that it is the ovaries that hurt: timely diagnosis
It is almost impossible to determine on your own that it is the ovaries that have started to hurt, since sensations can be deceptive and subjective, and it is difficult to accurately determine their location. Therefore, if you have any suspicions, contact a gynecologist, who will conduct an examination in a chair, prescribe an ultrasound of the pelvic organs and, most likely, blood tests for hormones. Sometimes ovarian puncture or biopsy and diagnostic laparoscopy are indicated.
Timely diagnosis of the ovaries can save you from many problems in the future.
If there are no gynecological diseases, go to a therapist. He will give referrals to specialized specialists involved in the examination and treatment of nearby organs (intestines, bladder): urologist, proctologist, oncologist. For diagnosis, ultrasound, CT or MRI, blood tests, and abdominal punctures are performed.
When your ovaries hurt, consult a doctor immediately. A comprehensive examination will help determine the causes of the symptom. Treatment depends on the specific problem, but should be timely and prescribed by a specialist after diagnosis.
(voted: 1, rating: 5.00 out of 5)
Share the news on social networks
Ask a Question! You have questions? Feel free to ask any questions! And our staff specialist will help you. Go>>
Tags: ovaries
- Recommended Articles
- Therapeutic tampons to improve women's health
- Vaginal acidity: when to sound the alarm
- Treatment of vulvovaginitis
« Previous entry
Why do the ovaries hurt on different days of the cycle (in the middle, in the first or second phase)?
A normal menstrual cycle for a healthy woman lasts 21-35 days. There are several phases in it:
- The follicular phase is from the first day of menstruation until ovulation. At this time, the follicles are maturing and the dominant one, the carrier of the egg, is being isolated from among them.
- The ovulatory phase lasts 24 hours. At this time, the egg leaves the ovary and prepares to meet the sperm.
- The luteal phase is from the completion of ovulation to the first day of the next menstruation. During this period, the corpus luteum is produced, and the body is preparing for a possible pregnancy.
In the first phase of the cycle
Pain in the projection of the ovaries in the first phase of the cycle occurs when a follicular cyst appears. This benign formation, filled with serous fluid, arises from a follicle that has failed to complete the full development cycle. Ovulation does not happen, the cyst grows, reaching a size of 4-5 cm - and characteristic pain appears on the right or left side. Unpleasant sensations occur against the background of a long (up to 30 days) delay in menstruation and subsequent heavy periods. The development of uterine bleeding is possible.
A follicular cyst is considered functional and usually does not pose a danger to a woman. After a month, it resolves spontaneously, less often it persists for 2-3 cycles. A control ultrasound to assess the size of the cyst is prescribed 3 months after the disease is detected. If the cyst does not resolve on its own, its removal is indicated. To accelerate the regression of education, it is possible to use hormonal drugs and physiotherapy.
In the middle of the cycle
A nagging pain in the lower abdomen in the very middle of the menstrual cycle is usually associated with ovulation. The egg matures, reaching a size of 2-3 cm, the ovarian capsule stretches, and characteristic symptoms appear. Nausea is observed, vomiting, flatulence and bloating are possible. Unpleasant sensations persist for 1-2 days, after which they disappear without a trace. No anesthesia is required.
It is important to know: the Graafian vesicle containing the egg does not always reach a large size. Its rapid growth is observed against the background of stimulation with drugs (including after discontinuation of OCs or before IVF).
In the second phase of the cycle
Pain on the 15-28th day of the cycle (with a standard 28-day cycle) can be caused by the formation of a luteal cyst. This formation grows from the corpus luteum and reaches a size of 3-8 cm. Against the background of pain, other symptoms arise:
- Delay of menstruation up to 14 days.
- Soreness and engorgement of the mammary glands.
- Nausea, often vomiting.
- Change in taste preferences.
- Aversion to strong odors.
- Emotional lability, etc.
Such symptoms are similar to signs of early pregnancy, and this is not surprising. The corpus luteum cyst is a full-fledged gland, and it produces progesterone. This hormone is also synthesized during pregnancy, so the symptoms will be similar.
Expert opinion
Svirid Nadezhda
Obstetrician-gynecologist
expert
A blood test for hCG helps to distinguish a luteal cyst from the first weeks of gestation. During pregnancy, human chorionic gonadotropin will increase, but with a cyst, it will remain within normal limits. Ultrasound helps confirm the diagnosis.
A luteal cyst is considered a functional condition. Observation for 3 months is indicated. During this period, the formation should resolve. Progestins, synthetic analogues of the hormone progesterone, help speed up the regression of the cyst. When taking Duphaston or Utrozhestan, the cavity resolves in 1-2 cycles. If the pathology does not go away, surgery is indicated.
Pain syndrome during periods of natural hormonal imbalances
Nagging pain in the ovary can be avoided, but to do this you need to know how they arise. Pain in the ovarian area appears in many patients after 30 years. For the most part, it can be associated with the onset of ovulatory syndrome. This is a very common occurrence. After a girl has her next period, a corpus luteum forms in place of the follicle in the ovary. It is a collection of cells that is responsible for the production of progesterone.
Can the ovaries hurt with this condition? In order to exclude any pathologies, consult a specialist. Most often, the ovary hurts after ovulation. In this case, severe pain occurs in the second part of the cycle, after two weeks. It is part of the ovulatory syndrome. In this case, aching pain in the ovaries in women is especially noticeable.
If the corpus luteum has not formed, the ovary and follicle will secrete a small amount of progesterone. As a result, damage and rejection of the uterine mucosa may occur. As a result of this, the woman’s ovaries hurt a lot, sometimes they pull, and her lower back also ache.
This manifestation of ovulatory syndrome has the following symptoms: periodic sharp pain in either the right or left ovary, weak vaginal discharge, elevated temperature, pain during discharge.
Please note: What can cause ovarian pain in women during ovulation? The ovary is pulled at the moment when the egg leaves its limits. Minimal rupture occurs and some blood spills into the abdominal cavity. The spilled blood irritates the nerve endings of the peritoneum, so aching pain in the ovary is normal.
Since it occurs in the middle of the cycle, it is easy to calculate the moment of its occurrence. For example, if your cycle is twenty-eight days long, then pain in the ovaries appears on the thirteenth to fourteenth day. Most women at this time note a shooting pain that lasts for several hours.
A woman may also feel discomfort if the ovary ruptures. This condition leads to heavy bleeding into the peritoneum, resulting in peritonitis - a severe inflammatory process. In order to restore the integrity of the ovary, urgent surgical intervention is necessary.
During menstruation, pain in the ovarian area under normal conditions cannot bother a girl. What many patients write off as pain in the ovary is actually pain in the uterus. When the uterine lining is shed, it must get rid of its contents, so it begins to rapidly contract.
My ovary hurts, what should I do, many women ask. If this phenomenon occurred after menstruation, then such a picture is not characteristic of ovulatory syndrome. The girl should not lift weights or engage in physical activity. Contact your gynecologist to rule out the possibility of complications.
We recommend you find out: Why
Colitis of the ovary after ovulation
Pain in the left ovary can be present with a natural hormonal imbalance. These periods include adolescence, postpartum and premenopausal. Discomfort experienced during this time rarely requires treatment and usually goes away on its own.
Puberty
During adolescence, the formation of the menstrual cycle occurs. This may be accompanied by pain in the lower abdomen. The left and right appendages gradually increase in size and begin to produce the first follicles, which results in minor discomfort.
Pain can persist until the menstrual cycle reaches full regularity. For prevention, it is recommended to show the girl to a doctor. Pathologies discovered at this stage are easily treatable and do not cause complications in the future.
Postpartum period
The main process of recovery of a woman’s body after childbirth takes place within six months. During this time, the ovary begins to function fully, and the menstrual cycle is restored. Pain in the left ovary can be throbbing or dull and is physiological in nature. It indicates the normalization of reproductive function and the process of preparing the body for a new conception.
If you are breastfeeding, pain in the ovaries may occur only after the end of lactation. In some women it occurs earlier, in others the menstrual cycle is absent throughout the entire period of feeding the baby. This is explained by the fact that prolactin, produced during lactation, stops the functioning of the appendages, protecting against a new pregnancy. However, women who are breastfeeding need additional contraception.
Menopause
Closer to 40-50 years, a woman’s menstrual cycle is disrupted. This is facilitated by low follicle maturation and lack of ovulation. The functionality of the left ovary decreases, which leads to a decrease in its size and the appearance of pain in the organ. The onset of menopause is accompanied by other symptoms - hot flashes, mood swings, changes in blood pressure, and deterioration in well-being. Some women tolerate this process easily and feel almost no changes in the body.
At the onset of menopause, the ovaries reach their minimum size. The menstrual cycle stops. All unpleasant symptoms, including pain in the lower abdomen, also disappear.
Why do women's ovaries hurt during pregnancy?
The reasons for the appearance of unpleasant sensations in the projection of the gonads are different:
- Threat of miscarriage. The pain is localized in the ovaries, lower abdomen, goes to the lower back and perineum. The appearance of brown discharge may be a sign of chorionic detachment (placenta) and an incipient miscarriage.
- Ectopic pregnancy. The pain is felt in the projection of the appendages on the left or right, and intensifies when walking or running. When an abortion begins or the fallopian tube ruptures, bloody discharge from the genital tract appears.
- Ovarian cyst. During pregnancy, a corpus luteum cyst is usually detected. As the tumor grows, pain occurs on one side. When the cyst is twisted or ruptured, the pain increases sharply.
- Pathology of the digestive tract. Increased production of progesterone leads to relaxation of the intestinal muscles, decreased peristalsis and the appearance of constipation. Pain in the groin area that occurs with this condition is not associated with the ovaries, but can be taken as a sign of damage to the uterine appendages.
Painful sensations in the projection of the ovaries can be caused by physiological stretching of the pelvic ligaments. This is a normal condition and does not require treatment.
Pain in the ovary during ovulation (ovulatory pain)
With a high sensitivity threshold, some women feel ovulation.
What is this connected with? Before ovulation, the follicle increases to 20-24 mm, the ovarian capsule stretches and ruptures above the follicle. The process of releasing an egg into the abdominal cavity is painless, but when the follicular fluid flows into the abdominal cavity, it irritates the peritoneum - and this is a very sensitive space, pain occurs. But since there is approximately 3 ml of liquid in the follicle, not all women feel this.
If the ovarian capsule is dense and when it ruptures the vessel is damaged, then blood drips from the vessel along with the follicular fluid into the abdominal cavity - this condition is called ovarian apoplexy and requires immediate medical attention and requires immediate hospitalization.
In order to understand what caused the pain - ectopic pregnancy, intestinal diseases, etc. A consultation with a gynecologist, an ultrasound examination of the pelvis, and a blood test are required. If the cause of the pain is not clear, an MRI is performed, and, if indicated, laparoscopy.
Many women begin to take antispasmodics and analgesics on their own and come to the doctor after the pain has stopped, which makes it difficult to determine its cause.
Prolonged monthly pain in the area of the ovarian projection can also be associated with pathological neoplasms. It is timely treatment that will help avoid surgical treatment, because many ovarian cysts can be treated without surgical treatment, and when the cyst occupies the entire ovary, the tissue that contains the eggs may no longer exist.
Why do the ovaries hurt after an abortion, miscarriage, or childbirth?
Pregnancy, regardless of its outcome, leads to serious hormonal changes in the female body. The menstrual cycle is disrupted, the follicles do not develop, and the corpus luteum does not regress in due time. Functional formations arise - follicular and luteal cysts - the direct cause of pain in the ovaries.
Unpleasant sensations in the groin area after an abortion or miscarriage do not occur immediately. It takes at least a month for the cyst to appear and grow to a clinically significant size - 3-5 cm. The pain from ovarian formations is pulling and aching, radiating to the lower back, sacrum, and leg. There is a delay of menstruation for up to a month, followed by heavy periods or bleeding.
It is important to remember: not every ovarian formation is functional. Abortion or miscarriage can provoke the growth of true tumors that are not amenable to hormonal therapy and do not resolve on their own.
Pain in the ovaries after childbirth requires special attention. Such symptoms may indicate the development of an inflammatory process in the pelvic organs. If both ovaries hurt, you should think about bilateral salpingo-oophoritis. The predominant localization of pain in the lower abdomen with irradiation to the groin area indicates postpartum endometritis. In both cases, urgent assistance from a gynecologist is required.
Adnexit
Adnexitis is an inflammatory process in the ovaries. It is accompanied by cutting and stabbing pain. The patient experiences pain periodically. They are localized in the lower abdomen.
The intensity of pain varies. Sometimes the pain spreads to the back and legs. Adnexitis is treatable, but subject to adequate and timely treatment. Otherwise, the pathology may become chronic, and pain in the ovaries will bother the woman throughout her life.
In the ovaries, sharp pain in women is caused by adnexitis, an inflammatory disease that is caused by infections. Young ladies over 20 years of age are at risk.
Why do women’s ovaries hurt when taking and after stopping contraceptives?
Contraceptives containing estrogen and progesterone block the ovaries. The production of your own hormones changes, ovulation does not occur, and the corpus luteum does not form. Against this background, there cannot be functional cysts in the ovary, and the appearance of pain when taking OCs is an alarming sign. If a girl taking estrogen-progestin drugs experiences pain in the lower abdomen or groin area, you should consult a doctor. When taking contraceptives, it is possible that a true ovarian tumor may develop, requiring surgical treatment.
The appearance of pain after stopping contraceptives is associated with completely different reasons. Unpleasant sensations are caused by the rebound effect. Cancellation of OC leads to active stimulation of the ovaries and increased production of follicles. The Graafian vesicle, which carries the egg, can reach a size of 3 cm. This formation stretches the ovarian capsule and leads to pain on one side. A similar symptom may also indicate the maturation of several eggs - and a high probability of multiple pregnancy.
Tell me, can you get ovarian cancer at the age of 35? For what other reasons do the ovaries hurt at this age in women? Zhanna, 35 years old.
The cause of pain in the ovaries can be various diseases - inflammatory processes, cysts, and tumors, including malignant ones. Cancer cannot be ruled out. In order not to miss a dangerous pathology, it is important to be regularly examined by a gynecologist. If you have complaints of pain, you need to visit a doctor as soon as possible.
Treatment
If the cause of pain in a woman is infectious and inflammatory diseases, then antibacterial therapy (you can use tablets or injections), anti-inflammatory drugs, and immunomodulators is prescribed. Upon completion, physiotherapy is indicated.
Hormonal imbalances (polycystic disease, hormonal cysts) are corrected with appropriate medications. They are usually prescribed for a long term, at least 4 months. After this time, repeated studies are carried out and, depending on the results, a decision is made to continue hormonal therapy or to discontinue it.
If there are any formations on the right ovary that require surgical intervention, the patient is hospitalized and undergoes surgery to remove them.
The adhesive process (especially if it is extensive) is difficult to treat with medications. Therefore, laparoscopic surgery is performed to cut the adhesions.
If the cause of pain is psycho-emotional factors, then antidepressants, tranquilizers or antipsychotics may be prescribed. Calming sedatives are also used.
Ovulatory syndrome does not require specific treatment. However, taking complex vitamins, magnesium, and maintaining a healthy lifestyle will help reduce its intensity.
Purely female diseases, characterized by pain in the ovaries, often occur in women of all ages. Physiological, mild pain does not cause much concern. Others may be the result of serious pathologies of the reproductive or organs located in the pelvis. Therefore, every woman needs to know where the ovaries are located, when and why they can hurt, and what to do if certain symptoms occur.
Why do the ovaries hurt when taking hormonal medications (Duphaston, Utrozhestan)?
In the instructions for many progestin drugs, pain in the lower abdomen is indicated as a common side effect. Unpleasant sensations are localized on the left or right in the groin area, above the pubis, and less often in the lower back. Other undesirable effects may also occur:
- Nausea, vomiting, bloating.
- Headaches, dizziness.
- Peripheral edema.
- Skin itching and rashes.
- Breakthrough vaginal bleeding.
If such symptoms appear, you should stop taking the drug and consult a doctor.
Dependence on the menstrual cycle
Pain localized in the right ovary, provided that it does not cause acute discomfort to the woman, may indicate the onset of a specific menstrual phase.
During ovulation
Ovulation is the process of the release of an egg from a rupturing follicle. In most cases, it is accompanied by slight bleeding that irritates receptors located in the abdominal area.
Other causes of discomfort in the lower abdomen during this period may include:
- high pain threshold;
- adhesions located in the pelvic organs (are a consequence of the woman’s previous infectious diseases);
- leakage of follicular fluid, provoking uterine contractions.
Ovulatory pain occurs in the middle of the cycle and can be:
- cramping;
- cutting;
- piercing.
Provided there are no secondary pathologies in the pelvic organs, pain during ovulation will be localized only on one side. This is due to the alternate maturation of eggs in different ovaries. To minimize discomfort, gynecologists recommend that girls suffering from ovulatory pain get more rest and follow a drinking regime.
During menstruation
It is a misconception that women experience pain in their ovaries during menstruation. During this period, the functional organ is the uterus, whose active contractions cause discomfort in the lower abdomen.
Gynecologists, assessing a woman’s condition, classify painful periods (dysmenorrhea) into:
- primary;
- secondary.
The reasons that provoke the persistence of dysmenorrhea for a long time (more than 1 year) are:
- instability of the emotional background;
- deviations in the functioning of the autonomic and nervous systems of the body;
- hormonal imbalance.
Modern gynecologists do not recommend that women take painkillers to get rid of painful sensations during menstruation. This approach will not solve the problem, but will only mask its manifestations. To normalize the functioning of the body, regardless of the phase of the cycle, women's doctors advise taking natural vitamin and mineral complexes, for example, Cyclovita.
Menopause
During menopause, a radical restructuring of all body systems occurs, including the reproductive system. During this period, the production of hormones decreases significantly, which leads to reorganization of the uterine tissue, as well as “drying out” of the ovaries. Despite the actual difficulty of overcoming age-related changes in the female body, pain during this period is not physiological.
Discomfort in the lower abdomen during menopause in most cases indicates the presence of:
- endometriosis;
- fibroids of the uterine tissue (it causes pain during hormonal changes);
- progressive adhesive process;
- inflammatory processes in the pelvic organs;
- salpingitis;
- malignant neoplasms;
- urethritis;
- cystitis;
- cystic neoplasms.
Pain during menopause can be different: acute, pulling, aching. Discomfort in the abdomen “radiates” to the lumbar region, and sometimes to the shoulder, bladder or limbs. With a timely examination of the body during age-related changes to identify pathologies, a woman will be able to avoid complications, some of which require exclusively surgical intervention.
Why do the ovaries hurt after IVF and embryo transfer?
In vitro fertilization involves conception outside the female body and often requires prior stimulation of the ovaries. Medications are used that lead to the maturation of a large number of follicles - 10 or more. This process is accompanied by stretching of the ovarian capsule and the appearance of characteristic pain. Other symptoms are also noted:
- Nausea and vomiting.
- Disturbance of stool and urination.
- Bloating and flatulence.
- Headache.
- Marked weakness.
- Swelling of the limbs.
With a mild form of ovarian hyperstimulation, the woman does not need to be treated. Sexual and physical rest and observation by a gynecologist are indicated. In severe situations, ovarian puncture is performed.
After IVF and embryo transfer, the ovaries should not hurt. Residual discomfort may persist after puncture and stimulation, but within 1-2 weeks all discomfort should go away. If the pain does not go away, you should consult a doctor. The development of complications cannot be ruled out:
- The appearance of ovarian cysts against the background of stimulation of ovulation.
- Development of the inflammatory process in the appendages after puncture.
- Increased uterine tone and threat of miscarriage.
Yesterday pain appeared near the ovary, only on the left. Today the pain has gone lower - to the hip and leg, radiating to the knee. Gradually intensifies, profuse mucous discharge from the vagina appears. What it is? Which doctor should I go to? Natalya, 27 years old.
Similar symptoms occur with partial torsion of an ovarian cyst or tumor, diseases of the spine, and neurological disorders. As the pain intensifies, you cannot hesitate. You should consult a gynecologist as soon as possible to rule out pathology of the pelvic organs. Next, you may need to consult a therapist.
Pain whose causes require treatment
If you experience severe, prolonged, sharp pain, you should not self-medicate; you should definitely consult a doctor. The following diseases require competent medical treatment:
- inflammatory diseases of female organs;
- benign or malignant tumors;
- cysts, endometriosis;
- miscarriages, ectopic pregnancy;
- concomitant diseases that cause pain in the gonads.
With an ovarian cyst
The pain, depending on the type of cyst and its progression, is of a different nature and appears at different times. May occur during sexual intercourse or physical activity. When the leg is twisted or an ovarian cyst ruptures, paroxysmal, severe pain occurs.
- heaviness, feeling of fullness;
- aching pain in the lower abdomen, perineum, radiating to the lower back, sacrum, rectum;
- menstrual irregularities;
- bloody, spotting discharge;
- difficulty urinating, with frequent urge;
- nausea, fever, fainting.
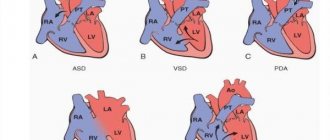
Painful symptoms are caused by gynecological diseases such as adnexitis, salpingoophoritis (simultaneous inflammation of the ovaries and fallopian tubes), apoplexy (rupture of ovarian tissue), polycystic disease, and ovarian endometriosis.
Untreated, neglected cysts lead to serious complications - their ruptures, pedicle torsion, development of tumors, infertility, adhesions. Women undergoing IVF may develop ovarian hyperstimulation syndrome, associated with an excessive amount of medications that increase ovulation.
To avoid these complications, doctors, based on the type of cyst or cystic formation, prescribe medication or surgical treatment. One of the treatment methods that is not often used is puncture, which removes aspirate (contents) from the cystic ovarian cavity.
Related to the menstrual cycle
Ovulatory syndrome - pain in the ovaries before menstruation, after ovulation, is often associated with an insufficiently mature corpus luteum. In this case, partial detachment of the uterine epithelium occurs, which causes discomfort.
The period during which the egg leaves the follicle is characterized by micro-tears of the membrane and micro-hemorrhages. This period occurs during ovulation in the middle of the monthly cycle and is also characterized by a slight pain syndrome. Pain usually occurs on the side on which the egg matures. The occurrence of severe, sudden pain may be a signal of ovarian rupture. And in this case, immediate medical assistance cannot be avoided.
Pain during menstruation, according to doctors, occurs in the uterus itself, which vigorously rejects the mucous layer if pregnancy has not occurred. The ovaries can also hurt, but this is due to pathological processes in them, stressful conditions or nervous strain.
If pain begins to bother you after menstruation or during menopause, you need to pay attention to the possibility of gynecological pathology.
During pregnancy
Pain during pregnancy can be caused by non-obstetric (non-gynecological), pathological or natural, physiological causes.
Symptoms and causes of non-gynecological pain are associated with exacerbation of chronic pathologies, such as:
- cystitis - inflammation of the bladder;
- exacerbation of cholecystitis;
- pyelonephritis;
- appendicitis.
Physiological pain, aching, not severe, is caused by sprained ligaments, muscle tissue, displacement of internal organs by the uterus, which gradually increases its size. They are temporary and not dangerous to the body.
Pathological - the most unpleasant, can occur at different stages of pregnancy, caused by the following reasons:
- inflammation of one or both ovaries;
- cyst or its rupture (apoplexy);
- spontaneous miscarriage (abortion);
- consequences of IVF (in vitro fertilization).
Ovarian pain before childbirth is associated with increased activity of hormones that cause softening of cartilage tissue, ligaments, and separation of the pelvic bones. These processes cause uncomfortable pain, which doctors call false.
During and after sex
One of the main causes of pain during sex may be an uncomfortable body position (posture) or a rude attitude of a partner. Pain after sex can be associated with the onset of ovulation or psychological problems in a woman. These problems, with respect and mutual understanding between partners, are resolved positively.
Burning, tingling, nagging pain appear after sex with inflammation of the ovaries, endometriosis, and tumors of the appendages. Sharp, unbearable pain occurs with apoplexy.
Important: High-quality sex is an important component for maintaining a woman’s health. Without good emotional and physiological release, venous stagnation occurs in the pelvic organs. This leads not only to pain, but also to neuropsychiatric disorders.
After surgery
It is clear that with any surgical intervention, discomfort is almost inevitable. After puncture of the ovaries, nagging, aching pain and slight bleeding appear, but after five days or a week these phenomena usually subside.
Minor pain is a natural consequence of surgical interventions to remove a cyst and other operations on the organ. They may intensify with the development of complications - postoperative bleeding, pelvioperitonitis, adhesions.
Neoplasms
Benign or malignant tumors occur for a long time without obvious symptoms. In the later stages, women begin to experience aching pain in the pelvic organs. Malignant tumors reduce a woman’s vitality, worsen her health, and increase feelings of discomfort.
Ovarian pain has different origins and is caused by different reasons. Therefore, during preventive or unscheduled gynecological examinations, it is necessary to more accurately explain to the doctor how and when the pain syndrome manifests itself. To be more accurate in describing symptoms, it is advisable to keep a calendar that indicates the timing of the female cycle and the time of occurrence of uncomfortable conditions. These records help the doctor make a more correct diagnosis and prescribe treatment.
The causes of pain in the ovarian area can be physiological or provoked by some disease. More often than not, this is just a symptom, so if it appears, you should consult a gynecologist. Read on to learn why your right ovary hurts.
What it is?
The ovaries are paired organs of the female reproductive sphere located in the pelvis. Eggs mature in them and sex hormones are synthesized.
If the right ovary hurts and pulls, the first thing to suspect is a gynecological disease. The inflammatory process often affects the entire uterine appendages on one or both sides - the pain becomes constant, and in this case they speak of chronic pelvic pain.
Where does the right ovary hurt?
Pain in the ovarian area is the most common complaint of women who come to the gynecologist, since this symptom accompanies many pathologies of the genital area. Where are the painful sensations localized? When the ovary on the right hurts, pain can be felt:
- in the lower abdomen;
- in the right iliac region;
- in the right side;
- above the pubis;
- pain can radiate to the lower back, rectum and hypochondrium.
Why do the ovaries hurt after surgery: laparoscopy or laparotomy?
To find the cause of the discomfort, you need to know for what reason the operation was performed and what organs were damaged in the process.
After removal of an ovarian cyst or tumor
Unpleasant sensations in the groin area after removal of an ovarian cyst or tumor is a natural process. It does not matter which way the operation was performed. Both after minimally invasive laparoscopy and after classical laparotomy, the ovaries require time to recover.
The damaged tissues must heal, but until this time pain may be felt in the projection of the appendages. Normally, discomfort gradually decreases and finally subsides 5-10 days after surgery. If the pain does not go away or intensifies, you need to inform your doctor about this - the development of complications is possible.
Expert opinion
Svirid Nadezhda
Obstetrician-gynecologist
expert
Pain in the ovaries a month after laparoscopy may be associated with the appearance of new cysts or tumors. Pathology can be determined by ultrasound.
After oophorectomy
Unpleasant sensations in the lower abdomen on the left or right can also occur after an oophorectomy - removal of the entire ovary. This pain is not associated with damage to the pelvic organs, but is caused by the natural processes of tissue healing. Discomfort persists for up to 2 weeks, after which it disappears. Analgesics and antispasmodics are used in treatment.
After hysterectomy
Pain in the lower abdomen and groin area also occurs after a hysterectomy. After removal of the uterus, cysts may form in the intact ovaries - the result of stress and hormonal changes. The type of cyst can be determined by ultrasound, diagnostic laparoscopy and histological examination.
It is important to know: discomfort after removal of the uterus may be associated with the formation of adhesions in the pelvis. Without treatment, this condition can lead to chronic pain and a deterioration in overall quality of life.
Physiological reasons
In the ovaries, follicles with eggs mature and the female sex hormones estrogen and progesterone are produced. The condition of these organs determines a woman’s reproductive ability, her general health and age-related characteristics of the body. The maturation of the egg and related processes most often occur alternately in the left and then in the right organ. The causes of pain in the ovaries are both ongoing physiological processes and various pathologies.
Natural reasons for pain in the groin area are:
- Menstruation. If the left ovary begins to hurt, this means that it is the one that is active in this cycle. Nagging pain is observed in most women, even without any pathologies in the condition of the genital organs. The regular occurrence of such ailment a few days before menstruation allows many women to predict their onset. Painful sensations continue during menstruation and even after it ends. The reason is changes in hormonal levels during the cycle.
- Ovulation. Around the middle of the cycle, a mature egg breaks the follicle membrane and leaves it, moving into the fallopian tube. In this case, the nerve endings are irritated, resulting in pain. Their intensity depends on the sensitivity of the body.
- Pregnancy during its normal course. The cause of mild pain in the left groin may be a natural hormonal shift that changes the structure of the ovaries and endometrium.
- Postoperative healing of the left ovary.
- During sexual intercourse, there may be an impact on the lower abdomen, which sometimes causes an aching sensation of mild pain and tingling. However, pain in the groin after sexual intercourse in most cases is a sign of serious illness. You should pay attention to how often it occurs and what other symptoms appear. An examination by a gynecologist helps to determine the nature of the pathology.
- Emotional experiences, heavy physical exertion.
Cyclically occurring pain in the lower abdomen, not associated with pathologies, is called ovulatory syndrome. It occurs in approximately 60% of women. The pain is not intense against the background of general malaise associated with menstruation; it does not cause any particular discomfort in the woman. But it is necessary to pay special attention to the appearance of other symptoms (cycle disruption, the presence of unusual discharge between periods, changes in the nature of menstruation), since there are many ovarian diseases that are characterized by the occurrence of such a manifestation.
Why do the ovaries hurt during menopause?
With the onset of menopause, the functioning of the gonads ceases. The ovaries decrease in size. Menstruation ends, and a new stage in a woman’s life begins. The appearance of pain in the projection of the ovaries in women over 40 years of age may be associated with the following conditions:
- A paraovarian cyst is a benign formation that occurs near the ovaries. It grows slowly and does not bother you for many years. The likelihood of malignancy has not been fully studied.
- Cystadenoma is a benign ovarian tumor. It is characterized by an asymptomatic course and begins to cause concern only with active growth. It can develop into a malignant tumor.
- Ovarian cancer is a dangerous malignant tumor. Pain occurs at a late stage of pathology, when treatment is not always effective. In the early stages, the disease is asymptomatic and usually becomes an incidental finding during ultrasound.
During menopause, any ovarian neoplasm should be considered as a potential malignant tumor, requiring a special approach to diagnosis and treatment.
I am 40 years old and recently noticed the first signs of menopause. I began to feel hot, I began to have trouble sleeping, and I worry all the time. A week ago I had abdominal pain on both sides. I can’t figure out what hurts – either the intestines or the ovaries. Tell me, how do ovaries hurt in women after 40 years of age, and are there any special symptoms? Svetlana, 40 years old.
Unfortunately, there are no specific symptoms. At 40 years old, the ovaries hurt in the same way as at a younger age. Without an examination, it will not be possible to find the cause of the pain. You should not delay your visit to the doctor - when you enter menopause, the risk of developing malignant ovarian tumors increases significantly, and they can also cause similar pain.
Female sex hormones
Regardless of where the ovaries are located in women, the organ is capable of producing sex hormones necessary for the normal functioning of the entire body of the fair sex. These are progesterone and estrogen. A woman’s appearance, her attractiveness and the ability to conceive healthy offspring depend on the amount of these hormones. The true female hormone is estrogen. This element is absent in the normal male body. There are several types of estrogens. Depending on the size of the ovaries, women can produce a certain amount of hormones. This happens from the moment of puberty until the onset of menopause.
The growth of the mammary glands may indicate that the girl’s body has begun to produce sex hormones. In addition, the teenager begins to grow quickly. Subsequently, growth stops abruptly, and this is also due to the production of estrogen by the egg. Scientists have found that the formation of the female body ends by the age of 18, while in a man this process lasts up to 22 years.
Progesterone, which is also produced by the ovaries, is usually classified as a male hormone. It is the representatives of the stronger sex who produce this substance in greater quantities. Regardless of the size of the ovaries in women, the male sex hormone is also produced in their bodies. True, this happens only after the follicle has matured to the required stage and the egg is released.
Why do the ovaries hurt when urinating?
Unpleasant sensations in the groin area when urinating are not associated with pathology of the appendages. Such symptoms occur when the organs of the urinary system are affected: the urethra and bladder. Other signs of pathology also appear:
- Stinging and burning when urinating.
- Drawing pain over the womb.
- Frequent urination.
Bacteriological urine culture, ultrasound and cystoscopy help to make the correct diagnosis. After treatment of the underlying pathology, pain when urinating goes away.
Why does the right ovary hurt and radiate to the lower back? The pain has been bothering me for a week now, then subsides, then intensifies. Walking is uncomfortable, my back hurts and it hurts my legs. What happened with me? Alevtina, 43 years old.
Probably, such pain is associated not with the ovary, but with spinal pathology. Such symptoms occur during exacerbation of lumbar osteochondrosis. You need to see a therapist to find out the exact cause of the pain. It wouldn't hurt to consult a gynecologist.
What should I do and which doctor should I contact?
If you have pain in the ovary on the right side, you should first see a gynecologist. Based on the examination, ultrasound, smear results and other tests, the doctor will determine the cause and prescribe the necessary treatment. Treatment methods for pain in the ovary depend on the disease:
- Oophoritis, adnexitis - anti-inflammatory drugs, antibiotics, strengthening the immune system, vitamin therapy, physiotherapy;
- Cyst - oral contraceptives, painkillers or surgical removal;
- Tumor - radiation and chemotherapy, hormonal agents (if the tumor is sensitive to them), if large - removal surgery;
- Polycystic disease - elimination of the underlying cause, diet, restoration of the menstrual cycle and stimulation of ovulation, laparoscopy.
Ovarian and premenstrual pain can be overcome by taking painkillers - No-shpa, Drotaverine, Spazgana. It is also recommended to eliminate stress and physical activity, eat well, and take vitamins.
- If the pain in the area of the right ovary is not caused by gynecological pathologies, the help of a neurologist, psychotherapist or urologist may be required.
Why do the ovaries hurt when walking, running, or pressing?
Pain in the projection of the appendages during fast walking or running, coughing and sneezing, pressing and during sex can be associated with the following conditions:
- Cysts and tumors of the ovaries, including those with a risk of torsion.
- Inflammation of the uterine appendages.
- Condition after stimulation of ovulation (during COC withdrawal or during IVF).
- Intestinal diseases leading to the development of constipation.
- Pathology of the bladder, including stones and tumors.
It is possible to find out the exact diagnosis and begin treatment only after examination by a specialist.
The left ovary has been hurting for two days. Yesterday, mucous discharge appeared - abundant and thick, but odorless. There is no pain or itching. I had my period almost two weeks ago. What could it be? Christina, 19 years old.
The appearance of pain in the projection of the ovaries against the background of abundant mucous discharge from the vagina in the middle of the cycle indicates probable ovulation. During this period, the chances of conceiving a child are very high.
Causes of pain
Without instrumental and laboratory tests, it is difficult to identify the cause of organ pain. There are two types of pain in the left ovary - physiological and pathological. The first ones can be distinguished independently; to do this, just listen carefully to your own body.
Physiological
The symptom occurs on certain days of the cycle. It is not very intense and causes virtually no discomfort to the woman. Possible causes of pain in the left ovary:
| Cycle day | Causes |
| 1-3 | The course of menstruation. Due to temporarily increased blood circulation during menstruation, there is pain in the left ovary. The symptom is especially acute in the presence of functional cysts. |
| 8-13 | Stage of follicle maturation. Their increase may be accompanied by slight nagging pain in the woman’s left ovary. |
| 14-15 | Ovulation. When the Graafian vesicle ruptures and the egg is released, there is sometimes a short-term acute pain of low intensity in the left lower abdomen. The duration of the symptom is from several hours to 1-2 days. |
| 26-28 | Preparing for the start of menstruation. |
The ovary on the left most often hurts during ovulation; discomfort is least often noted in the second half of the cycle.
A physiological symptom may be completely absent. Its presence is determined by the individual characteristics of the body. Often women who feel such pain in the left ovary experience severe discomfort in the lower abdomen during menstruation.
Pregnancy
Pain of natural origin includes pain during pregnancy. Successful conception may be manifested by unpleasant sensations in the left lower abdomen. The sign appears from the first days of a missed period. Its absence cannot exclude pregnancy, since its occurrence is individual.
The symptom is caused by the growth of the corpus luteum, which produces progesterone. This is explained by the body’s increased need for this hormone during gestation. Pain in the left ovary is often accompanied by nausea, dizziness, weakness and drowsiness. All these signs are a consequence of increased progesterone levels.
Functions of the ovaries
The production of sex hormones and eggs begins in women from the time of their first menstruation. These processes continue throughout reproductive age.
The main functions of the gonads can be distinguished:
- Hormonal – the production of female sex hormones.
- Generative – the formation of eggs.
- Vegetative – the formation of primary and secondary sexual characteristics.
Important! The production of sex hormones continues throughout the menstrual period.
The development of these organs begins in the second month of pregnancy and continues until the start of the menstrual period. The work of the glands is to prepare the woman’s body for conception and gestation. If fertilization does not occur, the cycle is repeated again. This continues throughout the menstrual period.
Clinical picture
If the appendage is enlarged, the symptoms are not specific enough. When the ovaries have enlarged, the signs are as follows:
- intense pain in the lower abdomen, in the suprapubic and pubic areas. Discomfort increases before menstruation.
- discomfort during urination. The symptom is nonspecific, since problems with the urinary system are possible.
- acyclic bleeding. When the menstrual cycle is normal and blood is released between two cycles.
- Discharge during menstruation becomes purulent. The symptom is alarming and indicates severe inflammation of the ovaries.
- pain syndrome during sexual intercourse. It is observed with significant growth of appendages and surrounding structures.
- in severe cases, female infertility is possible.
Manifestations may not be sufficiently expressed. In this case, you need to listen carefully to your own well-being. If the above symptoms are present, we may be talking about a number of gynecological diseases. Diagnostics is intended to put an end to the question.
Normal ovarian size for age
The standard size of the ovary in a healthy woman is between 3.5-4 cm in length, 2-2.5 cm in width, 1-1.5 cm in thickness. It weighs 5-6 g. The right ovary is usually larger than the left. With the onset of menopause, their size decreases. The activity of the follicular apparatus fades and the ovaries gradually dry out.
| Duration of postmenopause, years | Ovarian volume, cm3 | Follicular apparatus |
| 1 | 8-10 | saved |
| 2-3 | 5-7 | single follicles |
| 4-15 | 3-6 | individual liquid inclusions |
| Over 15 | 3-4 | not expressed |
Talitsa. The normal pattern of changes in ovarian size in postmenopausal women.
Recommended therapy for enlarged appendages
Pathology must be treated in a comprehensive manner. Among the stages of therapy are the following:
- Treatment at the first stage consists of normalizing the woman’s hormonal levels. It is necessary to prescribe synthetic estrogen hormone replacements. If the measures do not have a sufficient effect, the treatment should be reconsidered: increase the dosage of the drugs, but this can only be done under the supervision of a doctor and with his consent.
- Treatment at the second stage requires stabilization of the menstrual cycle. Surgery may be required. The same hormonal therapy is enough.
- Treatment in the third stage consists of restoring normal fertility. The effect is achieved independently with systematic and correct therapy.
- Finally, treatment in the fourth stage is stabilization of metabolism.
Surgery is a last resort. If the ovary is unable to perform its functions, it is resected. In other clinical situations, conservative hormonal therapy at all described stages is sufficient. Changing your diet is of great importance. Be sure to follow a fortified diet with a large amount of plant components and a minimum of animal foods, fatty, fried, smoked, salted.
Important! Treatment is carried out only by a specialist. Self-medication is a road to nowhere. At a minimum, there will be no improvement, at a maximum, severe changes will occur in all body systems. Is it dangerous.
Causes of the phenomenon
After a routine ultrasound, almost every woman hears a diagnosis - an enlargement of the right ovary. What could be the reason for the development of this pathology? Probably every woman is concerned about the causes of this pathology. Enlarged ovaries can be the result of certain disturbances in the body's functioning or a consequence of illness.
Why the ovary is enlarged - the reasons are:
- long-term use of hormonal drugs;
- period of breastfeeding - prolactin is significantly increased;
- stressful and depressive states, psycho-emotional tension;
- sudden weight loss;
- period of adolescence;
- different degrees of obesity;
- disturbances in the functioning of the endocrine system.
To establish why enlarged ovaries in women, the reasons are determined with the help of a specially designed examination by a specialist. Sometimes certain types of microorganisms are to blame for changes in the size of the ovaries. This reason why the ovary could become enlarged can be discussed if the disease is infectious in nature.
Enlarged ovaries can be due to thrush, gonorrhea, under the influence of staphylococci, enterococci and other pathogens. If the cause is one of the diseases mentioned, then you first need to address the root cause.
One ovary may be larger in size during certain phases of the menstrual cycle. Such changes in the reproductive system are temporary and are not considered a dangerous pathology. Sometimes there are cases when, due to the formation of several cysts on the appendages, they increase in size. With this disease, it is important to accurately determine the type of cyst and choose an effective treatment method.
When a woman’s right ovary is larger than the left or vice versa, she is often given a referral to take hormone tests. It is important to do this, because often disorders of the thyroid gland lead to unwanted enlargement of the female appendages.
Another reason may be a very dangerous and fear-inducing diagnosis - the formation of a malignant tumor. In this case, treatment will bring positive results only if the diagnosis is made correctly and at an early stage.
Enlarged ovary - what does it mean?
Gynecologists emphasize that organ enlargement is not a rare pathology. In some cases, the increase is physiological in nature and does not indicate a disease.
An enlarged ovary can be determined during an ultrasound examination and gynecological examination. Sometimes the organ is enlarged 2 or more times, which requires searching for the cause.
Enlargement of the appendages can occur at any age. Often the organ increases in size in women of the reproductive cycle, which is associated with hormonal function. However, pathology can also be detected in menopausal women and girls.
Treatment of the disease
Treatment tactics are determined after an accurate diagnosis has been established. The choice of treatment option depends on several factors:
- stages of the disease;
- causes of pathology;
- symptoms.
Only the acute form of oophoritis is treated in a hospital setting. The remaining stages of ovarian inflammation with mild symptoms can be treated at home.
Antibiotic therapy
When ovarian inflammation is detected in women with acute symptoms, treatment with these drugs is mandatory. During diagnosis, it is only necessary to identify the type of pathogen and its sensitivity to the drug. The dosage is selected individually to ensure the required concentration of the antimicrobial component. In severe cases of the pathology, several medications may be prescribed at once.
You cannot self-medicate, as there are several groups of antibiotics with their own characteristics. A doctor can figure them out; he prescribes medications, taking into account diagnostic data.
For inflammation of the ovaries in women with pronounced symptoms, prescribe treatment at home, and a quick recovery can only be achieved with the help of properly selected antibiotics. The table presents the main medications for the treatment of ovarian inflammation.
| Antibiotic group | Medications | Description |
| Sulfonamides | Streptocide, Sulfasalazine, Co-Trimoxazole | Strong drugs with a wide spectrum of action. Used as injections. |
| Aminoglycosides | Kanamycin, Gentamicin | They show high efficiency and are used in the form of injections and tablets. |
| Penicillins | Oxacillin, Ampicillin | They have few side effects, but are low in effectiveness. |
| Cephalosporins | Cephalexin, Cefazolin | Has many side effects. |
| Tetracyclines | Tetracycline, Doxycycline | Often prescribed and well tolerated. |
To achieve maximum antimicrobial effect, antibiotics are often combined.
Application of candles
For severe inflammation of the ovaries in women with complex symptoms, treatment with antibiotics is supplemented with suppositories. Vaginal suppositories that contain:
- oak bark;
- walnut extract;
- propolis.
A positive result is shown by the use of Clindamycin suppositories. They are administered at night. Metronidazole suppositories are used morning and evening. Voltaren suppositories have a calming effect and are recommended for complex treatment.
For chronic inflammation of the ovaries in women with mild symptoms, treatment with suppositories is recommended to be carried out regularly in courses for the purpose of prevention.
Effective Treatments
Therapy for adnexitis must be carried out necessarily. It is good if treatment begins in the acute stage. However, medical practice shows that inflammation emanating from the vagina and affecting the appendages is already chronic.
Treating ovarian inflammation at home can be done with over-the-counter medications or alternative medicine. Often, patients are able to buy effective medications prescribed by doctors without a prescription. When taking such drugs on your own, you must be aware of responsibility for your own health, evaluate the consequences of treatment and strictly follow the instructions for use. Good results, according to reviews from women, are shown by an integrated approach when therapy is carried out with the help of medications and traditional recipes.
Treatment with medications
Inflammation of the tissues of the ovaries and fallopian tubes is caused in 90% by chlamydia. Microorganisms cannot be classified as bacteria or viruses. For this reason, it can be very difficult to find an effective medicine for chlamydia. It is necessary to use antiprotozoal agents to which the infectious agent will be sensitive. For self-treatment of adnexitis, women use antibiotics.
They will be effective if the disease is caused by bacteria: streptococci, gonococci, E. coli, peptococci and other pathogens.
- Metronidazole and drugs based on it have been used for many years to treat adnexitis. The medicine is prescribed in the form of tablets for a course of treatment. If necessary, you can use suppositories or vaginal gel. Combining several forms of antiprotozoal antibiotic will achieve the best effect. Metronidazole appears to be effective even when other antibacterial drugs do not show good results.
- Azithromycin (Sumamed, Aditrus) is used in a short course of 3-5 days. The medicine is used in tablet form. Despite the fact that it is included in the list of prescription products, you can buy it yourself if you wish. The drug has a wide spectrum of action and is effective against gram-positive and gram-negative microorganisms.
- Doxycycline (Unidox, Vibramycin) is widely used in venereology. The drug is effective against most bacteria that cause inflammation in women. In severe cases, an injection form can be used, but at home patients prefer to take tablets.
- Ceftriaxone (injectable drug) is used to treat the appendages and uterus. The use of this antibiotic shows good results. It is effective against many pathogens, with the exception of viruses.
Local medications
To quickly relieve the symptoms of inflammation of the appendages, it is necessary to use local remedies. Their action can be:
- antiseptic;
- antimicrobial;
- regenerating;
- anti-inflammatory;
- painkillers;
- immunomodulatory.
Many suppositories (rectal and vaginal) for inflammation are sold without a prescription. The average course duration is 5-7 days. For effective treatment at home, they should be combined with systemic medications for adnexitis.
- Voltaren, Movalis - painkillers and anti-inflammatory drugs, eliminate the symptoms of inflammation of the appendages for 8-12 hours. The medicine is contraindicated in certain vascular diseases and bleeding disorders.
- Floumizin, Hexicon, Chlorhexidine are antiseptic suppositories for vaginal use. They act directly on the source of infection and disinfect the mucous membrane.
- Polygynax, Terzhinan, Betadine, Macmiror Complex - are used to treat inflammation caused by the colonization of pathogenic flora.
When choosing how to treat ovarian inflammation at home, you must give preference to one particular drug. Do not use all medications that may be effective at once.
Alternative medicine
Folk remedies for inflammation of the appendages and ovaries are treated quite well. Alternative medicine shows a positive result if the disease is old and has long become chronic. After a few days of using the available recipes, a noticeable improvement in well-being is observed. There is a lot of debate about how to treat inflammation on your own. Alternative medicine offers many recipes that have been proven over the years.
Caution must be exercised when using natural medicinal formulations. Any herbs are contraindicated for pregnant and lactating women. Also, non-traditional drugs are more likely to cause an allergic reaction than traditional drugs.
Recipes for internal use
For inflammatory diseases, plants of medicinal origin are used in the form of decoctions and tinctures. It is important to consider that a separate form of the disease requires the use of individual formulations. Thus, for acute inflammation of the ovaries, treatment with folk remedies is carried out using boron uterus, field grass, oak, linden, coltsfoot, and raspberries. The chronic form of the disease is well eliminated by cinquefoil, chamomile, sage, and daisy flowers. The preparations are prepared on a water basis or with the addition of alcohol-containing substances. The latter are prohibited for use by women driving cars and patients engaged in hazardous activities.
- A decoction of nettle, centaury, oak bark and knotweed is prepared over low heat for an hour (200g of raw material per 1 liter of water). After this, the medicine is infused for another 4-5 hours and filtered. You need to take 100 ml half an hour before meals. After 10-15 days, the symptoms of inflammation will disappear.
- A water infusion of chamomile, immortelle and calendula is prepared in a thermos. This remedy will be effective for purulent vaginal discharge. The medicine is taken 50-80 ml after meals for a long time.
- Goose cinquefoil in the amount of 2 tablespoons is brewed with 400 ml of water. After an hour of infusion, strain and take half a glass every 6 hours. The course of treatment is 2 weeks.
- Borovaya uterus (1 tablespoon) is poured with a glass of boiling water and left for 2 hours. Take the strained infusion in a third of a glass 4 times a day at equal intervals.
Any raw material can be prepared on an alcohol basis. It is believed that such treatment of the ovaries in women will be more effective, since ethanol promotes vasodilation and rapid penetration of the active component into the bloodstream. However, you should not chase the best result, harming your health. It must be remembered that alcohol-containing medications are not suitable for everyone.
Douching
The question of the effectiveness of douching for inflammation remains open to this day. It is believed that herbs when used in this way penetrate directly into the area affected by the pathogen and act on it. At the same time, vaginal microflora, which may be pathogenic, can spread to the uterus. This process is fraught with additional infection. A woman who wants to perform vaginal irrigation should definitely consult a doctor.
If the patient is adamant in her decision, then the following recipes should be used:
- aloe and plantain (plantain decoction is mixed with fresh aloe);
- water infusion of eucalyptus (raw materials are brewed in a thermos);
- chamomile decoction (dried flowers are boiled over low heat).
Alcohol-containing douching products are not used. It is necessary to treat the syringe in order to douche with adnexitis. The mucous membranes become inflamed from douching (with inflammation of the appendages) if the instrument is unsterile. In this case, harmful microorganisms enter the vagina in an additional portion, and this is fraught with complications.
Tampons
There are many ways to cure ovarian inflammation at home. One of the most effective methods is the use of tampons. Unlike douching, this method does not contribute to the spread of infection and can be safely used independently. It is important to choose the appropriate ingredients for the medicine, since all substances have individual effects.
- propolis – has an anti-inflammatory and regenerating effect (beeswax is melted in a water bath, then a sterile tampon is soaked in it and, after hardening, it is inserted into the vagina);
- Celandine and garlic are natural antibiotics that have a pronounced antimicrobial effect (the juice obtained from the raw material is mixed with 200 ml of warm water, after which a tampon is soaked in this solution and inserted into the vagina before bed).
To make tampons, medications in the form of ointments are often used, for example, Levomekol and Methyluracil. The substances are applied to sterile gauze and inserted into the vagina. You can only use a freshly prepared tampon. The course of treatment with such compresses lasts from 5 to 14 days and depends on the severity of the clinical manifestations of the disease.
Diagnostic measures for enlarged gonads
Diagnosis of problems of this type is carried out by gynecologists. Additional consultation with an endocrinologist may be required.
During the initial appointment, the doctor interviews the patient and clarifies the nature and duration of the complaints. Anamnesis is also collected. This procedure is necessary to identify diseases that the patient has suffered during her life. The following facts play a special diagnostic role: the presence of gynecological problems, diseases of the paired organs themselves, the uterus, a history of infertility, and menstrual irregularities. Subsequently, the doctor carries out a bimanual examination, palpates the appendages and records the data obtained.
What is the peculiarity of the location of the appendages?
It is important to emphasize that the location of the ovaries has its own nuances. To accurately determine them, you will need the help of reliable sources. According to information presented in the anatomical literature, these paired organs are located deep in the pelvis.
Normally, the right ovary differs from the left one in size, and in addition they are located at slightly different levels. This is explained by the fact that, under the weight of its own weight, one ovary is slightly lowered down. The uterus has a broad ligament with it, which holds it in the required position and prevents it from descending. The ovaries, in turn, articulate with it through the mesentery, and in the pelvic cavity the genitals are tightly held precisely thanks to the ligaments.
During pregnancy, the appendages can change their normal anatomical position. This is very important, because during such a difficult period, the uterus gradually begins to take up more and more space. In this case, the distance between the uterus and the appendages is reduced, and one of the ovaries is closer to it. Nature has foreseen everything, and if from an anatomical point of view the internal genital organs do not have deviations, a change in the localization of the ovaries does not pose any danger.
Not only the period of gestation, but also various pathological conditions can lead to changes in the position and shape of these glands. The main thing is to identify them in time, and having identified the symptoms and causes of the disease, begin adequate treatment as soon as possible. If you visualize the appendages, that is, imagine them along the anterior abdominal wall, they will be located in the lower abdomen, just above the inguinal folds. The pain often begins to bother the right or left side above the pubis.
Ovarian diseases
Pathological conditions of the female reproductive system organs bring many unpleasant sensations. If left untreated and careless about your health, such situations threaten to lead to infertility. Among the common women's problems are the following diseases:
Apoplexy
Hemorrhage in the ovary, provoked by the rupture of a cyst, connective tissue (stroma) or follicle with an egg. Any bleeding that occurs inside the body is life-threatening, ovarian apoplexy is no exception.
According to statistics, bleeding is most often observed at the age of 20-35 years and in teenage girls during puberty. Follicular apoplexy is a recurrent pathology and in 60% of cases it recurs.
The disease has a complex development mechanism. To understand the process, you need to remember the cyclical nature of the female reproductive system:
- Every month, an egg matures in the follicle (graphic vesicle).
- The follicle bursts, and the egg waits for a possible meeting of the sperm.
- In the absence of a “date,” the egg dies and menstruation occurs, renewing the mucous membranes of the uterine tissue.
In this most complex process, there are phases of increased risk for the integrity of the ovary - this is the middle of the cycle and its second decade. During such periods, the blood vessels that feed the uterine appendages become overfilled with blood, making them vulnerable.
The right ovary bursts more often - blood circulation in this organ (compared to the left) is more intense. And the artery that supplies blood to the right ovary originates directly from the aorta - the artery of the left ovary branches off from the bloodstream of the kidney.
Gynecologists divide the disease into two groups:
- Painful (with no internal bleeding). With painful apoplexy, hemorrhage occurs, but the blood does not enter the retroperitoneal space - it is limited to the corpus luteum or follicle.
- Hemorrhagic (with bleeding). This form of the disease is divided into three groups (depending on the amount of blood loss).
Causes. For an ovarian rupture to occur, a combination of certain conditions is necessary: a time when a woman’s ovary is most vulnerable and a simultaneous increase in pressure from the walls of the abdominal cavity. This can happen when:
- Severe abdominal injury.
- Too intense sex.
- Rough examination by a gynecologist.
- Incorrect action when douching.
- Long-term horse riding lessons.
- Increased physical activity (workouts in the gym with weight lifting, walking with weights).
But pathological conditions and chronic diseases of the body can also provoke ovarian rupture. Apoplexy occurs in the following cases:
- Varicose veins of the ovary.
- Growing tumors pressing on the ovary.
- Congenital malposition of the uterus.
- The presence of postoperative adhesions in the pelvic organs.
- Vascular changes (sclerosis, varicose veins).
- Chronic inflammation of the female reproductive system.
- Thrombocytopenia (blood clotting problems due to current illnesses or after long-term use of anticoagulant drugs).
Symptoms. The main symptom of apoplexy is sudden, very sharp pain in the lower abdomen. After 2-3 minutes, the pain syndrome is accompanied by weakness and a feeling of nausea (they come as a result of blood loss). As hemorrhage increases, the following symptoms are added to the symptoms:
- Vomit.
- Tachycardia.
- Dry mouth.
- Blurred consciousness.
- Appearance of sticky sweat.
- Paleness of the skin and mucous membranes.
- Drop in blood pressure.
- Temperature rises to +38-39⁰ C.
The woman notes the appearance of bloody discharge, and upon examination the doctor diagnoses bloating and a tense state of the peritoneum. Touching the stomach during this period is extremely painful.
Polycystic
An endocrine disease that provokes destabilization of the reproductive work of the ovaries. This disease, which affects 15% of women, leads to infertility in 70% of cases. Often the disease begins in adolescents and manifests itself with the onset of menstruation.
Polycystic disease “blooms” by the age of 30-35. At this time, the disease manifests itself most clearly. And after 40 years, women no longer get polycystic disease.
With the disease, multiple proliferation of follicles with immature eggs is observed. Such abnormal activity leads to pathological changes in the menstrual cycle, disruption of the normal course of pregnancy and deterioration in the overall health of the woman.
It is important to diagnose the disease in time and begin treatment in the early stages of the disease. Polycystic disease provokes the development of diabetes, cardiovascular diseases and obesity.
Causes. Doctors were unable to determine the exact culprits for the development of abnormal polycystic follicles. It was revealed that the disease is associated with disturbances in the level of hormones (androgens, progesterone and estrogen). Hormonal changes stop the normal release of the egg from the follicle, which leads to a lack of ovulation.
In the process of studying the disease, doctors identified six factors that lead to the occurrence of pathology:
- Imbalance of the glands, organs responsible for the production of hormones. This includes problems with the thyroid gland, pituitary gland, hypothalamus, and adrenal glands.
- Excessive production of insulin (a hormone produced by the pancreas). Excessive amounts of insulin provoke active production of androgens. An increase in male hormones in women has a detrimental effect on follicular development and interferes with the normal maturation and release of the egg.
- Excess weight, which becomes the culprit for the active creation of insulin in the female body.
- Hormonal imbalance. When the amount of prolactin (the hormone responsible for the production of breast milk) increases, follicles begin to grow rapidly. Polycystic disease also causes an increased amount of testosterone and androgen (male hormones).
- Chronic inflammatory diseases. When inflammation occurs, there is a high level of leukocytes (white blood cells) in the blood. They are produced by the body to stop infection. But the activity of leukocytes leads to an increase in insulin and the development of polycystic disease.
- Heredity. If there are cases of the disease in the family, the risk of developing the disease increases 3 times.
Symptoms. The symptoms of the pathology vary and depend on the severity of the disease, its duration and the general health of the woman. To diagnose polycystic disease, you need a combination of the following signs (at least two):
Menstrual irregularities. The monthly cycle becomes abnormal in the following situations:
- Absence of menstruation for more than 4 months.
- The monthly cycle lasts more than 35 days.
- Up to 7-8 menstruation periods per year are noted.
- Abnormality of discharge (too scanty or too abundant).
Male pattern hair growth. An increase in androgens – male hormones – leads to the growth of hair on the body and face. Activation of androgen causes other symptoms:
- Deepening of the voice.
- Enlargement of the clitoris.
- Noticeable breast reduction.
- Thinning scalp hair and baldness.
Deterioration of skin condition. With polycystic disease, women note increased pigmentation of the skin, their roughness, and darkening. Acne appears and actively manifests itself. The functioning of the sebaceous glands is disrupted, which leads to a change in the structure of the hair (it looks shiny, constantly dirty, unkempt).
Weight gain. The patient may suddenly (within a month) gain fat. Body weight increases by 10-15 kg, the distribution of fat follows the male scenario: it is deposited in the abdominal cavity.
All these troubles are accompanied by nagging pain in the ovaries. A woman with polycystic disease is unable to become pregnant and carry a child to term.
Thrush
The human body is a haven for a huge number of microorganisms. In small quantities, such microflora does not harm the body and is normal. But under certain conditions, microorganisms begin to multiply rapidly, leading to the appearance of diseases. These creatures include yeast-like fungi called Candida.
Thrush or candidiasis is an inflammatory disease caused by abnormal activity of yeast fungi.
What causes the disease. The development of thrush indicates that the body’s defenses have decreased to critical levels: there has been a sharp drop in immunity or a relapse of chronic diseases. The following conditions lead to the activity of pathogenic microflora:
Unbalanced diet. A diet containing large quantities of sugar, flour, smoked meats and other high-carbohydrate foods has a detrimental effect on the functioning of the gastrointestinal tract. As a result, the acidity of the microflora changes and dysbiosis develops, which leads to the appearance of candidiasis.
Changes in hormonal levels. Often candidiasis develops after ovulation - in this case the disease is explained by an increase in progesterone. This phenomenon is observed during pregnancy, when a woman’s hormonal background changes dramatically. Long-term use of contraceptives also affects hormone levels. Thrush is caused by various endocrine disorders.
Taking antibiotics. Antimicrobial therapy is a double-edged sword. By destroying viruses, anti-inflammatory drugs also kill beneficial microflora, giving the green light to the growth and reproduction of candida.
The activity of yeast fungi is caused by sexually transmitted diseases, severe hypothermia, poor personal hygiene, and tight underwear. The disease is provoked by previous colds (sore throat, flu, ARVI), prolonged wearing of tampons and nervous stress.
Symptoms. The disease manifests itself 6-7 days before the arrival of the next period. In pregnant women, candidiasis occurs at any stage of pregnancy. Signs of the disease:
- Burning, itching, unpleasant odor in the genital area.
- Urination occurs with a burning sensation and pain.
- Redness and inflammation of the external genitalia and mucous membranes.
- Increased pain when coughing, sexual intercourse, at night, after using the toilet (when the woman sits down) and a warm bath.
- The appearance of white discharge with a cheesy consistency. Their color can change - a woman may observe brown, yellow, greenish discharge.
Pain in the ovaries with a cyst
An ovarian cyst is a cavity filled with fluid. With the accumulation of internal secretions, the cystic benign formation increases in volume and puts pressure on nearby tissues, causing pain. Doctors divide cystic formations into six types:
- Endometrioid. Neoplasm on the superficial tissue of the ovaries. The tumor affects both organs and reaches a size of 20 cm. There is a high risk of the endometrioid cyst degenerating into a cancerous tumor.
- Dermoid. A cyst developing from connective tissue. The process of its creation involves the embryonic sheets of the embryo (the rudiments of cartilage, hair, teeth, fat cells). These are slow-growing, thick-walled formations.
- Paraovarian. Formation growing from appendages. A single-chamber cavity filled with transparent liquid and densely entwined with a network of capillary vessels. Paraorvial cysts are more often diagnosed in women 20-40 years old.
- Mucinous. Multilocular cyst filled with mucous contents. This type of formation is predisposed to developing into a cancerous tumor.
- Corpus luteum cyst. Thickening of the walls of one of the ovaries, containing yellow liquid with bloody inclusions. This tumor is formed due to excessive growth of the follicle. Instead of corpus luteum cells, the follicle is filled with fluid.
- Follicular. A single-chamber cyst with elastic thin walls and transparent contents. It is formed after ovulation, when the follicle does not fill itself with cells of the corpus luteum, but, stretching, is filled with liquid.
Causes. The exact culprits for the abnormal growth of tumors have not been identified. Doctors note the presence of general patterns leading to the appearance of cysts:
- Hormonal imbalance.
- Regular surgical interventions (abortions).
- The arrival of the first menstruation too early (before 10 years).
- Diseases of the thyroid gland and other endocrine pathologies.
- The presence of chronic inflammation of the appendages (adnexitis, salpingo-oophoritis, endometriosis).
The risk group includes women who actively smoke, have had a cesarean section, or suffer from dysmenorrhea (painful periods). Prolonged wearing of an intrauterine device provokes the development of neoplasms.
Symptoms. In most cases, the cyst does not manifest itself; it is detected by chance, during routine examinations of the gynecologist. But with excessive growth, large size and long existence of neoplasms, they announce their presence with the following signs:
- Sudden increase in abdominal volume.
- Dull pain in the lower part of the peritoneum.
- Weakness, feeling of nausea, causeless fatigue.
- Increased pain after sexual intercourse, when lifting weights and during defecation.
- Disturbance of the monthly cycle with a change in the volume of discharge (they become too abundant or scanty).
When complications develop (when the cyst twists on the stem or bursts), the woman feels sharp pain. The pain impulse radiates to the intestinal area, the temperature rises, vomiting and tachycardia begin.
Cancer
Common cancer holds the second position in popularity after uterine cancer. Most often, pathology is detected in older women (50-70 years). Ovarian cancer is fatal in 30% of cases. Doctors classify ovarian cancers into three groups (based on origin):
- Primary. An incipient tumor initially has signs of malignancy.
- Secondary. A benign neoplasm gradually develops into cancer.
- Metastatic. The beginning of a tumor is given by cancer cells from other organs carried in the blood or lymph flow.
Causes. Cancer is an insidious and mysterious pathology. The true causes of the appearance of malignant cells have not been found. Doctors have established a relationship between the occurrence of ovarian cancer and the following factors:
- Heredity. In 10-12% of cases, heredity becomes the culprit for the appearance of a cancerous tumor.
- Age. It has been established that the risk of developing cancer depends on age. Most often, ovarian cancer is diagnosed in women after 45 years of age (with the onset of menopause).
- Hormonal disbalance. An excess amount of male hormones in a woman’s body becomes the culprit for the development of malignant neoplasms.
- Obesity. Excess weight is one of the common causes of pathology. Doctors have noticed that the mortality rate of patients from ovarian cancer with large body weight is much higher.
- Early puberty.
- Violations of the rules for taking oral contraceptives.
- Promiscuity, abortion, sexually transmitted diseases.
- Current infections of the female reproductive system that develop into chronic ones.
- Exposure to radiation.
Symptoms. The insidiousness of ovarian cancer lies in its asymptomatic character in the first stages. There are a number of features that may indicate the development of a fatal disease (every woman needs to know them):
- Abdominal discomfort, similar to indigestion.
- Constant malaise, unexplained weakness and fatigue. Such sensations do not go away after proper rest.
- Sensation of a foreign body in the lower abdomen. This feeling intensifies after visiting the toilet and eating.
Such signs are nonspecific. They also appear in a number of other pathological situations. As the tumor grows, the following signs are added to the primary symptoms:
- Urinary disorders.
- Increase in peritoneal volume.
- Increasing weakness, exhaustion.
- Constant dull abdominal pain.
- Decreased menstrual flow.
- Temperature rises to +37⁰ C in the evenings.
- Complete loss of appetite, depression.
For what reasons does an inflamed ovary hurt?
Why is the right ovary enlarged and painful? When oophoritis occurs, the paired sex glands and fallopian tubes become inflamed. The inflammatory process can be either unilateral or bilateral. Inflammation can occur due to the introduction of pathogenic microorganisms into the body:
- chlamydia;
- Trichomonas;
- gonorrhea;
- streptococci;
- staphylococci;
- coli.
Main signs of the disease
The disease is characterized by numerous manifestations. They are not specific, they are similar to the symptoms of other pathologies, and they are easy to confuse. Only a specialist can make a correct diagnosis using diagnostics.
Pain in the lower abdomen
This symptom indicates the onset of an acute inflammatory process. Due to swelling, the size of the ovaries increases. Often the pain is localized in the suprapubic region and radiates to the lumbar spine.
Increased body temperature
An increase in temperature is a general reaction to the presence of foreign protein compounds in the body. Fever helps stimulate immune forces, creating unfavorable conditions for pathogenic agents.
Digestive system dysfunction
Inflammation of the ovaries may be accompanied by a disorder of the gastrointestinal tract. Characteristic manifestations:
- nausea, vomiting, as a reflex reaction to pain;
- diarrhea is caused by irritation and intoxication of the inflamed ovaries located nearby.
Such symptoms blur the true picture of the disease. A person thinks that he has poisoning, he begins to treat himself, and does not see a doctor.
Unpleasant discharge from the genital tract
Normally, discharge from the genital tract should be clear and odorless. If inflammation or infection occurs, the discharge changes.
Pathological discharge can be:
- With pus. This is an indicator of bacterial infection. The volume of excretion depends on the type of pathogen. There is often a smell of spoiled fish. The presence of foam indicates the presence of anaerobic microflora.
- Serous. This is an indicator of viral inflammation that affects the body and cervix.
- Mixed with blood. This indicates a violation of the integrity of the blood vessels.
Such signs should be a reason to immediately seek medical help.
Menstrual irregularities
This is one of the common signs of ovarian inflammation. Violations are expressed as follows:
- complete absence of bleeding;
- strong or scanty discharge;
- long breaks between menstruation;
- severe pain.
The causes of such disorders are disruptions in the functioning of the ovaries due to inflammation, a decrease in the amount of sex hormones that they produce.
Pain during sexual intercourse
Due to inflammation in the reproductive system, pain occurs during sex. This is often caused by a lack of vaginal lubrication, a lack of the hormone progesterone, or damage to the vaginal mucosa. As a result, female frigidity develops. Sexual dissatisfaction becomes the cause of depression.
Hormonal disorders
This is not a necessary symptom. It is caused by a lack of the hormones estrogen and progesterone. Symptoms of hormonal disorders:
- infertility;
- decreased sexual desire;
- frequent mood changes;
- increased blood pressure;
- increase in body weight.
Such disorders occur only with bilateral inflammation of the ovaries, when the disease lasts for a long time.
Infertility
If inflammation of the ovaries is accompanied by impaired maturation of the egg, then there will be problems with conception. Typically, pregnancy does not occur if inflammation of the oviduct is associated with oophoritis. In this case, the lumen of the fallopian tubes decreases, resulting in their obstruction, which is the cause of infertility.
Inflammation of the ovaries during pregnancy
Inflammation of the ovaries significantly reduces the chances of getting pregnant. The formation of adhesions during a chronic inflammatory process makes the union of sperm and egg impossible. Before planning a pregnancy, the disease or its consequences must be eliminated. To preserve reproductive function, it is better to prevent oophoritis by taking measures to prevent infection with pathogenic microflora.
If pregnancy occurs against the background of inflamed ovaries, then there is a high risk of miscarriage due to placental insufficiency or intrauterine infection of the fetus.
Inflammation of the ovaries during menopause
This disease can also affect the ovaries during menopause. The mucous layer of the vagina becomes thinner during this period and cannot provide a protective function. Infections can enter through the vagina or through the pelvic organs.
Types of disease
The ovaries have a very infection-resistant outer shell. But the pathology can be transmitted through nearby organs, for example, the fallopian tubes. This is how inflammation of the ovaries or oophoritis develops. A viral infection can spread through blood or lymph. Oophoritis can become a complication after tonsillitis, appendicitis or chronic caries.
There are three types of ovarian inflammation:
- acute;
- subacute;
- chronic.
In the acute form of oophoritis, the symptoms appear sharply, the woman is forced to immediately seek medical help, there is no way to endure it. The subacute condition occurs in women with tuberculosis.
Without treatment, the pathology becomes chronic, in which periods of exacerbation and remission alternate. Pronounced symptoms are absent or they are confused with other pathologies.