Classification according to ICD
The bicornuate uterus, like other malformations of the pelvic organs, is also included in the list of malformations of the reproductive organs, which the 10th revision of the International Classification of Diseases combined into a group of congenital pathologies of the development of the reproductive organ - its body and cervix, while the bicornuate uterus has its own code.
Bicornuate uterus - ICD 10 code Q51.3, which is included in the 17th class of diseases - congenital anomalies, deformations and chromosomal disorders, block of congenital malformations of the reproductive organs, subclause - congenital anomalies of the body and cervix, subclause Q51.3 - bicornuate uterus.
https://youtu.be/RqGmqY4zCLE
Causes
Bicornuate uterus: the reasons for its formation in women depend on the influence of certain factors on the intrauterine development of the fetus during the period of organogenesis. First of all, these are the adverse effects of various intoxications, a woman’s bad habits - smoking, alcoholism and nicotine addiction, insufficient intake into the mother’s body for the development of the unborn child, the adverse effects of stress and mental trauma, the presence of endocrinopathies in women and malformations of the cardiac system. The course of pregnancy, complicated by hypoxia, toxicosis or the presence of infection (measles, rubella, mumps, toxoplasmosis or syphilis) also has an adverse effect on the formation of organs.
Causes of pathology
The causes of abnormal uterine duplication lie in the field of embryology. In the fourth month of obstetric pregnancy, this organ is formed in the fetus. Often its underdevelopment is coupled with abnormalities of the kidneys or urinary tract. If a newborn or adult woman has a bicornuate uterus, then the reasons for its occurrence are unfavorable intrauterine conditions:
- intoxication of the body (alcohol, drugs, medications, harmful working or living conditions);
- severe toxicosis during pregnancy;
- infectious diseases in the early stages of embryo formation;
- endocrine disorders (diabetes mellitus, ovarian diseases, hyperfunction of the thyroid gland);
- fetal hypoxia.
Genetic factors should not be underestimated. Heredity is a reason for suspicion and further examination.
We recommend watching a video about what you need to know about the bicornuate uterus.
Ultrasound
To reliably confirm the presence of such a pathology in a woman, a number of additional studies are required, among which ultrasound takes a leading place in its availability, safety and low cost. We’ll talk about what a bicornuate uterus looks like on an ultrasound a little lower. With a complete bicornuate uterus, the cavity is divided into two horns on each side, while the distance between them is minimal and each horn resembles a mature uterus of normal size. If a woman is diagnosed with an incomplete version of a bicornuate uterus, in which the horns are the same size and have a small distance between each other in the upper third, and in the middle and lower third of the uterus they form one cavity
And finally, the saddle-shaped form of a bicornuate uterus has a depression in the fundus in the form of a saddle and then the shape of the uterus resembles a heart. This form of pathology is not always seen by ultrasound doctors, unlike the complete or incomplete form of a bicornuate uterus, since its diagnosis requires qualifications and experience. Bicornuate uterus: Ultrasound photo You can look a little lower, where there are descriptions of all varieties of this pathology.
Abortion
Abortion with a bicornuate uterus is a very dangerous manipulation, since the risk of bleeding and injury is maximum, which is a further cause of infertility for a woman, especially since the bicornuate uterus itself is the leading cause of infertility among women. If pregnancy develops in the smaller horn of the uterus, then this is a direct indication for its termination. Every woman should understand that an abortion with a bicornuate uterus is technically very difficult and entails a number of complications, which is associated with its abnormal shape, so it is not advisable to carry out an abortion with a bicornuate uterus, especially if the woman subsequently performs reproductive functions.
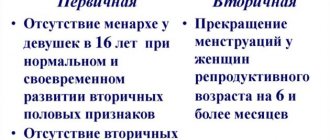
Diagnostics
Women most often find out about the anomaly during an examination after a number of unsuccessful attempts to conceive or during screening during pregnancy. Also, patients with a deviation in the structure of the organ may experience nonspecific symptoms:
- menstrual irregularities;
- intermenstrual bleeding;
- painful menstruation;
- amenorrhea;
- miscarriages;
- infertility.
If there is a closed horn, menstrual blood does not flow outward from it. Therefore, it accumulates inside, which leads to the appearance of characteristic bursting pain in the lower abdomen, intensifying during menstruation.
Is it possible to use the IUD for a bicornuate uterus in women?
Can an intrauterine device in a bicornuate uterus protect against unwanted pregnancy? This is a question that many women with this diagnosis face. If we talk about a regular IUD that does not produce hormones, then its use in a bicornuate uterus is ineffective, because if it is in one horn, pregnancy can occur in the other. As for the Mirena hormonal IUD, it is the only IUD in the modern world that is effective for any form of bicornuate uterus, since due to the release of the hormone it suppresses ovulation and changes the properties of cervical mucus.
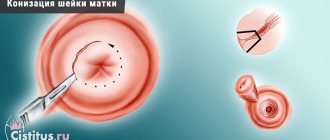
Surgical methods for correcting a bicornuate uterus
Surgical treatment of a bicornuate uterus is prescribed only if a woman is diagnosed with infertility or has more than 2-3 miscarriages in a row.
The operation in this case is carried out to restore a single uterine cavity, for which the septum that separates the uterine cavity is removed, or the rudimentary horn is extirpated.
Strassmann's operation is considered a completely common surgical intervention for this pathology , during which a laparotomy is performed, the uterine fundus is dissected with a transverse incision, the median septum is excised, and then the membranes of the organ are sutured.
In addition, surgical correction of a bicornuate uterus can be performed using the hysteroscopic method. Since after surgical correction the uterus needs some time to heal, the woman is fitted with an intrauterine device for at least six months.
Hormonal imbalance in a woman is difficult; find out the causes of ovarian dysfunction that need to be eliminated in order to prevent serious complications.
We invite you to familiarize yourself with the treatment options for bacterial vaginosis using folk remedies - read.
If you notice chest pain before menstruation, we offer you an article that discusses in detail the menstrual cycle and the symptoms associated with it.
Are there any chances of getting pregnant for a woman with a bicornuate uterus?
A woman, if she has a bicornuate uterus, often does not know about it until she becomes pregnant, but in most cases women learn about its existence at the stage of pregnancy planning, because this is often the cause of infertility or menstrual irregularities. Having learned about the presence of such a pathology, each of them, first of all, asks the question: “Is it possible to give birth with a bicornuate uterus? How does it affect the course of pregnancy? Let's try to figure this out a little.
So, a bicornuate uterus: every woman has a chance of getting pregnant, but not always to carry it to term. This is due to the fact that pregnancy can occur in different places and if implantation occurs in a non-functioning horn, then it is considered ectopic and must be removed, and if pregnancy occurs in one of the full-fledged uterine horns, then the likelihood of a successful pregnancy increases, but the risks that may arise remain. Such pregnant women are subject to careful monitoring by a doctor for timely assistance in the event of a threat of miscarriage, bleeding, or a frozen pregnancy.
Bleeding in a bicornuate uterus occurs when placenta previa occurs, since it is attached low due to the septum in the body of the uterus. And if its implantation occurred precisely on the uterine septum, then due to its poor blood supply, the development of the fetus does not occur and the embryo dies.
Bicornuate uterus - is it possible to get pregnant without the use of modern reproductive technologies? In most cases, there is a possibility of natural fertilization, but it does not always end favorably or is impossible, since bicornus is often combined with other malformations of the reproductive organs. We should not forget about the various variants of a bicornuate uterus, despite the fact that a saddle-shaped uterus in most cases does not prevent pregnancy, but a bicornuate uterus with an incomplete septum due to the presence of a rudimentary horn has an adverse effect on the onset of a long-awaited pregnancy.
A bicornuate uterus during pregnancy is diagnosed in 3% of all pregnancies and has characteristics of the course of pregnancy and its monitoring. Let's dwell on them a little. First of all, given the high risk of complications during pregnancy, the woman is subject to dynamic monitoring.
A woman has been diagnosed with a bicornuate uterus, what does this mean during pregnancy? This means that such a pregnancy is subject to strict observation and control by the attending physician, because it can cause the development of such serious complications as:
- termination of pregnancy at any stage due to the irregular shape of the reproductive organ and the inability to stretch all its muscle fibers and proper implantation
- placenta previa occurs due to implantation of the fertilized egg very low
- leakage or rupture of amniotic fluid also occurs quite often if a woman has such a pathology
- malpresentation of the fetus also depends on the shape of the uterus and the presence in it of insufficient space for its development compared to a normal-shaped uterus
- cervical insufficiency is very common and is associated with the inability of the internal os to hold the fetus
- when pregnancy develops in the rudimentary horn, urgent delivery is required, since this is dangerous not only due to interruption or missed abortion, but also to the possibility of rupture of the uterine horn and the development of heavy uterine bleeding
- Due to poor blood supply, premature placental abruption often occurs at any stage of pregnancy, which has a disappointing prognosis not only for the life of the child, but also for the life of the mother.
A bicornuate uterus and pregnancy in the right horn or a bicornuate uterus and pregnancy in the left horn does not have a significant impact on the development of pregnancy, because the outcome of the implantation of the fertilized egg does not depend on which uterine horn the implantation of the fertilized egg occurs, the main thing is that the blood supply to this horn, namely his placental site was very good. And if the horns are located far from each other, which indicates its underdevelopment, then problems during pregnancy are much more common. Implantation in one or another horn without ultrasound observation can be suspected by the load on the uterine ligaments, because on the side where the embryo develops, they will be stretched more strongly.
We will discuss below how to get pregnant with a bicornuate uterus and positions for conception, because this shape of the uterus cannot hold sperm and then pregnancy does not occur. Therefore, for conception, positions are used during and after sexual intercourse such that the sperm lingers in the woman for as long as possible and enters the uterine cavity. Doctors advise placing a pillow under the pelvis, lying on your back or lying on your stomach, place a pillow under the buttocks so that the pelvic end is raised. If the uterus is saddle-shaped, then it is better to use the knee-elbow position during intercourse.
So, a bicornuate uterus with a septum and pregnancy are often combined, but have a number of complications, which the doctor should always remember and warn the woman about their first symptoms, which require immediate seeking help from a medical institution in order to maintain the pregnancy and prolong it. Do not self-medicate, as this can cause infertility and loss of an existing pregnancy.
Treatment of bicornuate uterus
As a rule, no intervention or treatment is required for saddle anomaly.
A bicornuate uterus is treated surgically only in cases of infertility or habitual miscarriages, since the inferiority of the anatomical structure of the organ can affect the development of pregnancy. If the fertilized egg finds a place in one of the horns, then the second one may also respond to the changes that have occurred in the body and begin to grow in parallel with the first. In addition, the cavity that has received the fertilized egg is not always able to stretch as much as is possible for a full-fledged organ. And this jeopardizes the normal course of pregnancy. The extent of surgical intervention depends on the degree of pathology, but the goal of surgery for a bicornuate uterus is always to create a normal (single) cavity capable of implanting a fertilized egg and subsequently carrying a pregnancy.
The horn, if vestigial, must be removed. If there is complete bicornuity with two cavities separated by a septum, then the task of surgical intervention is reconstruction and plastic surgery. To carry out reconstructive plastic surgery, otherwise called metroplasty of the bicornuate uterus, a transverse incision of the uterine fundus is performed and the septum in the uterus located between the two cavities is removed, and then the uterine walls are sutured layer-by-layer. It should be noted that modern technologies allow metroplasty to be performed laparoscopically, however, subject to the availability of the necessary equipment and equipment.
After surgical treatment, to fully restore the usefulness of the organ, an intrauterine device is installed in its cavity, which must remain there for at least six months. By the way, with a bicornuate uterus that has not been operated on, no spirals, including the therapeutic Mirena, can be installed.
Causes of formation and methods of removal of Bartholin gland cysts and bartholinitis. The principle of the modern surgical method of fallopian tube laparoscopy is outlined in this article
Read more about follicular or functional ovarian cysts below
Twins
A bicornuate uterus and twin pregnancy can also occur, because a woman can simultaneously mature several follicles that undergo fertilization. Most often, when the uterine cavity is completely divided into two halves, twins, both identical and fraternal, can occur. Such a pregnancy is considered quite dangerous among doctors and has a high risk of termination at any stage, and sometimes there is a threat of uterine rupture. In almost 99% of cases, twin pregnancies with a bicornuate uterus end prematurely
A bicornuate uterus and twins do not always end sadly. It should be understood that if a woman has a bicornuate uterus at the stage of pregnancy planning or in the early stages of pregnancy with twins, then such a woman is subject to constant medical supervision and monitoring throughout the pregnancy. The very first danger occurs at the beginning of pregnancy, so a woman needs hospital treatment and round-the-clock medical supervision. There are cases when the mother’s life is in danger, then surgical delivery is performed by caesarean section.
A bicornuate uterus and multiple pregnancy have certain difficulties, but the likelihood of its occurrence is much higher than with a normal uterus. There is a very high risk of complications and miscarriage at any stage, and the risk during childbirth is also significant
Regardless of which horn the pregnancy occurs in, in most cases it ends in premature birth. To improve and have a favorable outcome of multiple pregnancy with uterine anomaly, a woman needs to completely change her lifestyle, completely eliminate physical activity and the effects of mental trauma and stress.
If there are twins in a bicornuate uterus and one miscarriage occurs before 12 weeks of pregnancy, then the fetus may disappear until the end of pregnancy and not be clinically manifested. If the fetus froze after 12 weeks of pregnancy, then a “paper” fetus is detected in the cavity, followed by its mummification. Due to the development of the second embryo and the development of the amniotic sac, it compresses the dead embryo, and the components of the amnion of the dead embryo are partially absorbed, which has a negative impact on the development of the remaining embryo. Clinically, it does not manifest itself in any way and only an ultrasound examination can detect a frozen pregnancy in one of the horns of the uterus.
Why is a bicornuate uterus dangerous for a woman?
Bicornus is not included in the group of diseases that negatively affect the quality of life. The pathology does not affect the viability of the fetus and the further development of the baby.
Important! A weakly expressed anomaly does not make itself felt in any way. The patient is not aware of the existing deviation, especially if reproductive function is not impaired.
The danger of deviation is as follows:
- Fusion (partial or complete) of the entrance to a separate uterine cavity.
- Hematometra. It may occur as a result of a violation of the outflow of menstrual blood due to the physiologically incorrect position of the horn. Infection of the contents causes the formation of pyometra (suppuration followed by the development of peritonitis and septic blood poisoning).
- Bleeding. Provoke anemia.
A bicornuate uterus is not a death sentence. With sufficient capacity, bearing a child takes place without problems. With severe bifurcation, the likelihood of spontaneous abortion or premature birth increases. Having such a pathology, the expectant mother should be observed by a specialist throughout her pregnancy.
ECO
A bicornuate uterus and IVF are often complicated by low placentation and presentation, leakage or early rupture of amniotic fluid, the development of ICI and placental abruption, which causes miscarriage at different stages of pregnancy. Carrying out the in vitro fertilization procedure if a woman has a bicornuate uterus is not a contraindication, but if there is a septum in the uterine cavity, it must be removed or dissected at the stage of pregnancy planning, which will significantly increase the likelihood of favorable implantation and pregnancy development. According to the standards for assisted reproductive technologies, in the presence of a bicornuate uterus, no more than one embryo is transferred, since the chances of a favorable outcome are much higher than with a multiple pregnancy.
Intrauterine insemination for a bicornuate uterus is carried out if a couple has male infertility, when the most active sperm are isolated from the man’s semen and placed in the uterine cavity or in the cervical canal, which significantly increases the likelihood of fertilization naturally, and not in vitro. This procedure is performed only if there is reliable patency of the fallopian tubes.
Dangers of a bicornuate uterus and its symptoms
Is a bicornuate uterus bad, what dangers does this anomaly pose and what consequences can it lead to?
First , this diagnosis can cause infertility and the inability to bear a baby, that is, miscarriages . However, this is not always the case; it all depends on the degree of development of the horn or horns of the uterus. The more pronounced the septum of the uterine cavity, the higher the chance of losing the child.
Secondly, this feature often causes abnormal spontaneous uterine bleeding.
And although a bicornuate uterus causes infertility in about half of the cases, its detection is not as obvious as it seems. During a routine gynecological examination, it is detected extremely rarely. Most often, a woman learns about this structural feature in one of three cases:
- diagnosis in connection with the problem of infertility or miscarriage;
- thorough diagnosis at the stage of pregnancy planning;
- directly during pregnancy.
In connection with the above, a woman may not even be aware of her illness. However, there are still some signs that may suggest something is wrong:
From the side of gynecology:
- uterine bleeding;
- pain in the lower abdomen as during menstruation;
- algodismenorrhea;
From the side of reproductive function:
- miscarriages (especially in the 1st trimester of pregnancy);
- premature birth;
- infertility;
- frozen pregnancy;
From the placenta:
- location anomalies;
- premature detachment;
- placental bleeding;
On the fetal side:
- breech presentation;
- transverse or oblique position;
- oxygen starvation and lack of nutrition in general;
From the side of labor:
- isthmic-cervical insufficiency;
- premature birth;
- violation of contractile function of the uterine muscles;
- postpartum bleeding.
It must be remembered that these symptoms do not appear in everyone and not always, as well as the fact that a bicornuate uterus and pregnancy is possible and quite often it is successful. If any symptom or several are noticed, you should immediately seek qualified help from a gynecologist for diagnostic measures.
Childbirth
Bicornuate uterus: childbirth can be either through the natural birth canal or operatively. This depends, first of all, on the obstetric situation and the intrauterine state of the fetus.
Birth with a bicornuate uterus is in most cases premature. This is due, first of all, to the inability of the uterus to fully stretch. Childbirth through the natural birth canal always occurs with weakness of labor, which is dangerous for the development of birth injuries in both mother and child.
The postpartum period often threatens the development of complications such as bleeding, poor contractility of the uterus, leading to the development of hematometra, and the development of inflammation in the uterine cavity. In obstetrics, a bicornuate uterus is not an indication for a cesarean section, and only based on the obstetric situation does the doctor assess the likelihood of performing it at different times in order to reduce complications for the mother and child. It is possible that the birth will end with a cesarean section, which happens in most cases, because bicornus complicates the course of labor and at the same time labor activity is disrupted, which can cause injury to the child. We should not forget about the postpartum period, which requires careful monitoring of the postpartum woman to exclude complications that threaten her life.
Reviews
Bicornuate uterus and pregnancy: reviews from women with this pathology are different, because the bicornuate uterus itself comes in several forms - from saddle-shaped to complete doubling, and there may also be forms of bicornuity with an incomplete septum, which significantly affects the process of conception and gestation. Many women learned about the presence of this pathology already during pregnancy, while others have been trying to get pregnant for years, undergoing several surgical interventions to remove or cut the septum, but the effect is negative. Everything depends not only on the bicornuate uterus, but also on the presence or absence of other pathologies of the reproductive system, therefore, you should not immediately panic when you learn that you have a bicornuate uterus.
Bicornuate uterus: reviews from those who gave birth are also ambiguous, because some of them gave birth through the vaginal birth canal without any complications, while others underwent a cesarean section. This is due, first of all, to the fact that the presence of pathology is due to the development of certain complications: placenta previa, abnormal position of the fetus, weakness of labor forces that are not subject to drug correction, and others that make childbirth through the natural birth canal impossible.
Malformation and pregnancy
A bicornuate uterus does not always manifest itself as problems with conception. However, infertility occurs with this malformation, which any doctor should remember.
The likelihood of impaired conception depends on the degree of bicornuity. The more pronounced the cleavage, the more likely problems are when trying to get pregnant. The saddle uterus is considered the most favorable option in this regard.
But even if pregnancy has occurred, with a bicornuate uterus the risk of miscarriage in the early stages increases. In addition, this defect is often accompanied by the following complications:
- Placenta previa.
- Violation of the position and presentation of the fetus.
- Isthmic-cervical insufficiency.
- Pathological uteroplacental blood flow.
- Spontaneous termination of pregnancy.
How to get pregnant with a bicornuate uterus? Today, gynecologists agree that every effort should be made to conceive naturally. And only if prolonged attempts are ineffective to seek help from surgeons. However, most often a bicornuate uterus and pregnancy are not mutually exclusive concepts.
Malformations of the genital organs can also affect labor.
Childbirth
Childbirth with a bicornuate uterus may be accompanied by certain problems. With pronounced splitting of the organ, the fetus is located in one of its halves. This means that the uterine muscles are overstretched and the risk of labor weakness and incoordination increases.
Also, with this defect, premature rupture of amniotic fluid is often observed.
The likelihood of trauma to the child and mother during childbirth in the case of a bicornuate uterus increases. This is why many obstetricians offer a woman a planned caesarean section. However, in some situations, natural childbirth without serious complications is possible.
Photo
What is a bicornuate uterus in women, photos of its varieties and a video of its treatment can be seen a little lower. Now let’s dwell a little on what a bicornuate uterus is, what it is, a photo of it and its shape. So, a bicornuate uterus is a congenital pathology of the reproductive system that occurs in girls in the prenatal period and exists until the end of life if reconstructive surgery has not been performed. Most women do not even suspect that they have this congenital pathology; some find out about it only when they become pregnant or, sometimes, during a cesarean section. Others, on the contrary, learn about the presence of this pathology even at the stage of preconception preparation, since pregnancy does not occur on its own and the woman has a number of clinical manifestations: from pain to recurrent miscarriage
We will post a photo of a bicornuate uterus and a regular one below, where it is clearly visible that the bicornuate uterus comes in several forms: saddle-shaped, with an incomplete and complete septum. The most favorable is the saddle-shaped uterus, where pregnancy often occurs spontaneously and proceeds relatively normally. But as for bicornus with a septum, it has its own characteristics. If the septum is complete, then the uterine cavity is divided into two separate cavities, which have one cervical canal. If the septum is incomplete, then, most often, the uterine cavity in the upper third is reported, which has a very adverse effect on implantation and the gestation period, because when the fertilized egg is implanted near the septum or on it, the pregnancy is interrupted or freezes, since its blood supply is insufficient and distensibility There are almost no fibers.
What a bicornuate uterus looks like: photos and pregnancy with it can be seen below, because a bicornuate uterus can have different development of the horns: they can be the same, different, one horn is rudimentary, or closed, or with atresia of one of the horns. We will provide all these features in the photo below, each of which will be signed and deciphered.
Bicornuate uterus: a close-up photo can be obtained either on the screen of an ultrasound machine, or during surgery or on a preparation for hysterectomy. Only cases where a woman has a history of recurrent miscarriage or infertility associated only with an abnormal development of the organ after excluding other causes of infertility are subject to treatment. The essence of surgery is to completely restore the integrity of the uterus. To do this, an operation is performed that involves dissecting the fundus of the uterus with a transverse incision, removing the septum in it, and then suturing its walls layer by layer. In order to restore the uterine cavity in the postoperative period, an intrauterine device is installed for a period of at least six months, which will not allow the walls of the cavity to close, but, on the contrary, will restore its cavity for successful implantation and pregnancy.
What a bicornuate uterus looks like during pregnancy, we can see a photo of it at the end of the article. Photos taken during an ultrasound examination can confirm the presence or absence of a second horn, whether it is functioning or not. Each woman suffering from this pathology must be aware that this pathology is not a sentence to infertility, and if you follow the doctor’s prescriptions and his recommendations regarding treatment and conception, then the likelihood of pregnancy and the birth of a child increases in a number of cases. There are cases when the chances of natural fertilization are minimal or absent, then it is also necessary to follow the recommendations of doctors: either surgical treatment, or the help of assisted reproductive technologies, which allow you to find the happiness of motherhood and give birth.
Bicornuate uterus: the video below once again confirms that it is not always the cause of infertility, and that there is a chance of having a child if you strictly follow the doctor’s instructions and seek help in a timely manner. Plan your pregnancy and be happy! After all, acquiring the status of motherhood for every woman is the most important task in life, and sometimes this requires determination and perseverance, so no self-medication, but only qualified assistance from specialists will help you with this.
https://youtu.be/ZP8JNyAvgxg