C1. Diagnostic criteria* src
| Recurrent abdominal pain or discomfort** on at least 3 days per month over the past 3 months, associated with two or more of the following: • improvement after defecation; • onset is associated with a change in stool frequency; • the onset is associated with a change in the shape of the stool. Additional symptoms are:• abnormal stool frequency ( {amp}lt;3 times a week or {amp}gt; 3 times a day); • abnormal stool shape ([c] lumpy/hard stool or [d] loose/watery stool); • [e] straining during defecation; • [f] urgency or feeling of incomplete evacuation, mucus and bloating |
| Note: *Criteria present within the last 3 months with onset of symptoms at least 6 months prior. **Discomfort means an unpleasant sensation not described as pain. |
Table 3.
Lactase deficiency in adults
This is a fairly rare pathology, which is characterized by a lack of enzymes responsible for the breakdown of milk sugar molecules (hypolactasia). The main group of patients with this disease are children of the first year of life, as well as children of the younger age group (up to 3 years). In adults, the incidence of hypolactasia diagnosis is approximately 8.9%. With lactase deficiency, the human body cannot digest not only whole milk, but also any products that contain milk sugar (lactose): cheeses, cottage cheese, kefir, yogurt.
It is impossible to recognize the disease in an adult without laboratory diagnostics, but you can independently identify pathological symptoms, especially if they occur after consuming milk and milk-based products. Symptoms of hypolactasia include:
- stool liquefaction and diarrhea, provoked by an increase in osmotic pressure and the influx of water into the intestinal cavity;
- pain in the lower abdomen, which becomes spasmodic when intensified;
- bloating (mostly without flatulence syndrome - involuntary passage of gases);
- appearance of milk flakes in feces.
In some patients, hypolactasia manifests itself as chronic constipation. There may be no stool for three days or more, and the feces come out in separate dense lumps mixed with white particles.
Important! In rare cases, vomiting may be a symptom of lactose intolerance. It has a white or milky color, a sharp sour milk smell and may contain undigested particles of curd consistency. This symptom always appears after eating.
Comparison of normal digestion and lactose intolerance
https://youtu.be/by51jLluA1w
Color
Types of stool vary in color. It can be brown (healthy color), red, green, yellow, white, black:
- Red color. This color may result from ingesting food coloring or beets. In other cases, the stool becomes red due to bleeding in the lower intestine. Everyone's biggest fear is cancer, but this can often be associated with diverticulitis or hemorrhoids.
- Green color. A sign of the presence of bile. Stool moving too quickly through the intestines does not have time to turn brown. A green tint is a consequence of taking iron supplements or antibiotics, eating large amounts of greens rich in chlorophyll, or supplements such as wheatgrass, chlorella, spirulina. Dangerous causes of green stool are Crohn's disease, celiac disease, or irritable bowel syndrome.
- Yellow. Yellow feces are a sign of infection. This also indicates gallbladder dysfunction, when there is not enough bile and excess fat appears.
- White stool is a sign of diseases such as hepatitis, bacterial infection, cirrhosis, pancreatitis, and cancer. The cause may be gallstones. Stool does not stain due to bile obstruction. The white color of feces can be considered harmless if the day before you took barium before an x-ray examination.
- Black or dark green indicates possible bleeding in the upper intestine. A sign is considered harmless if it is a consequence of consuming certain foods (lots of meat, dark vegetables) or iron.
How to treat?
The establishment of creatorrhea is not an independent disease, but merely a symptom that indicates dyspepsia (functional digestive disorders) or serious gastrointestinal pathologies. Therefore, there is no need to treat creatorrhea if the analysis showed the presence of undigested protein fibers; it is necessary to look for the primary cause through a thorough examination.
In severe cases, antibiotic therapy or even surgery may be necessary. However, the first thing to start with when dealing with creatorrhoea and indigestion is diet.
You will have to forget about buns, cakes, fast food and other foods that are difficult to digest. A gastroenterologist can prescribe enzymes, the intake of which will reduce the load on the pancreas and help digest food. Enzymatic preparations for creatorrhoea can be taken for a long time without harm to the body, but even such simple treatment should be agreed with a doctor.
When creative rhea is detected in young children, sometimes it is enough just to adjust the diet and reduce the protein (specifically meat) load on the gastrointestinal tract. Until the age of three, it is better to give preference to dairy and fermented milk products, as well as low-fat fish, from the protein diet.
Separation of IBS according to the predominant form of stool
| 1. Constipation-predominant IBS (IBS-C) – hard or lumpy stools* 25% and loose or watery stools** {amp}lt;25% of bowel movements***. 2. IBS with diarrhea (IBS-D) – loose or watery stools** 25% and hard or lumpy stools* {amp}lt;25% of bowel movements***. 3. Mixed IBS (IBS-M) – hard or lumpy stools* 25% and loose or watery stools** 25% of bowel movements***. 4. Unclassified IBS - abnormal stool consistency that meets the criteria of IBS-C, D, or M***. |
| Note: *Bristol Stool Shape Scale, Type 1–2. **Bristol Stool Shape Scale, type 6–7. ***No use of antidiarrheals or laxatives. |
When should you see a doctor?
The consistency of stool varies depending on diet and amount of water consumed. If a person consumes refined foods - white bread, ground steamed meat, soft cereals, canned food - then there will definitely be a tendency to constipation. On the contrary, during the season of fresh fruits and vegetables, the overwhelming majority of the population tends to loose stools.
The rate of bowel movements is from 3 times a day to 1 time in 3 days. Everything that does not fit into these frameworks is a consequence of either errors in food or illness.
Constipation that occurs once - if there are obvious reasons - can be eliminated with the help of medications (Picolax, Microlax microenema) or an enema. Diarrhea caused by malnutrition lasts about a day and does not cause a change in the general condition.
You should see a doctor if:
- constipation recurs despite normal nutrition and sufficient water;
- I have a stomachache;
- gases stopped separating;
- body temperature rises;
- dryness and an unpleasant taste in the mouth are added;
- dizzy;
- worries about weakness;
- diarrhea does not stop for more than a day;
- the stool has changed its normal color (instead of brown it becomes white, gray or greenish);
- impurities appeared - undigested pieces of food, mucus, blood;
- Foam and a foul odor appeared in the stool.
Any of these reasons is a sign of a disease that needs to be addressed urgently.
Other characteristics
According to its characteristics, feces in an adult are directly related to lifestyle and nutrition. What causes an unpleasant odor? Pay attention to what you've been eating more frequently lately. A foul odor is also associated with taking certain medications and can manifest itself as a symptom of some kind of inflammatory process. In cases of food absorption disorders (Crohn's disease, cystic fibrosis, celiac disease), this symptom also appears.
Floating stool in itself should not be a cause for concern. If the floating stool has a very unpleasant odor or contains a lot of fat, this is a symptom of poor absorption of nutrients in the intestine. In this case, body weight is quickly lost.
Predisposing factors for creatorrhea
If the condition persists for a long time and is accompanied by other symptoms, you should consult a specialist.
Creatorrhea is not a separate disease, but refers to the symptomatic manifestation of certain diseases and damage to the organs of the epigastric space of various natures:
- Putrid dyspepsia. The condition occurs when the protein components of food are partially or completely undigested. In this environment, the pathogenic activity of bacterial microflora rapidly increases, provoking inflammation of various parts of the intestine.
- Gastric resection. Postoperative complication after removal of part or all of the organ cavity, resulting in disruption of all digestive processes. The condition is often associated with the development of achylia (complete absence of gastric juice) and achlorhydria (lack of chlorine and hydrogen ions in hydrochloric acid).
- Accelerated expulsion of chyme. A condition in which semi-liquid contents leave the intestines quite quickly.
- Pancreatitis. A long-term disease that occurs predominantly in a chronic form. Accompanied by impaired pancreatic function and slow pancreatic secretion. Against the background of chronic pancreatitis, a violation of the external secretion of the pancreas often occurs.
- Development of hypoacid gastritis. The disease is characterized by reduced secretion of gastric juice and hydrochloric acid simultaneously with an intense inflammatory process. Hypoacid gastritis often reduces the functionality of all epigastric organs.
Prognosis for MS
The prognosis of the disease is favorable. The course of the disease is chronic, recurrent, but not progressive. IBS is not complicated by bleeding, perforation, strictures, fistulas, intestinal obstruction, or malabsorption syndrome. The risk of developing inflammatory bowel disease and colorectal cancer in patients with IBS is the same as in the general population.
The opposite situation arises with regard to the individual prognosis of “patients” with IBS, which is often unfavorable. The ability of patients to work is impaired. As a cause of temporary disability, the diagnosis of IBS has now taken second place after colds. In patients with IBS, the number of visits to the doctor and the duration of temporary disability per year are 3.5 times higher than in healthy individuals.
Possible complications of creatorrhea
What causes the appearance of indigestible protein food in feces if you do not pay attention to it? Since creatorrhea is usually associated with some kind of gastrointestinal disease, it can become chronic without adequate treatment. And this, in turn, is fraught with unpleasant complications:
- With chronic gastritis, the risk of developing appendicitis increases many times over.
- Prolonged and severe pancreatitis can provoke catastrophic thinning of the walls of organs, subsequent reflux of gastrointestinal contents into the abdominal cavity and the development of acute inflammation.
- Advanced gastrointestinal diseases can cause internal bleeding with anemia and blood infection.
- Ulcers and inflammation increase the risk of gastrointestinal tumors.
A coprogram is...
Chyme, or food gruel, moves through the gastrointestinal tract and fecal masses are formed in the large intestine. At all stages, breakdown occurs, and then absorption of useful substances occurs. The composition of the stool helps determine whether there are any abnormalities in the internal organs. A scatological examination helps to identify a variety of diseases.
A coprogram is a chemical, macroscopic, microscopic examination, after which a detailed description of the feces is given. Coprograms can identify certain diseases. These may be disorders of the stomach, pancreas, intestines; inflammatory processes in the digestive tract, dysbiosis, malabsorption, colitis.
What other stool parameters are important?
Stool analysis is called a coprogram. This is a study of physical and chemical properties, as well as the result of microscopy.
We recommend reading:
Culture for intestinal dysbiosis: details of the analysis
The coprogram examines the following parameters:
- properties of hydrochloric acid and stomach enzymes;
- enzymatic activity of the pancreas;
- liver function;
- the speed of food movement through the stomach and intestines;
- quality of absorption in the duodenum and small intestine;
- the presence of inflammation in different parts of the digestive canal;
- normal or pathological composition of microflora;
- the presence of colitis - ulcerative, allergic or spastic.
A normal coprogram looks like this:
- form – decorated;
- consistency – soft;
- Brown color;
- the smell is specific and not sharp;
- reaction – neutral;
- connective tissue – no;
- muscle fibers - no;
- striation of muscle fibers – no striation;
- neutral fat - no, a small amount is found in children in the first month of life;
- fatty acids – no;
- indigestible fiber – moderate amount;
- soap - no;
- Digestible fiber – no;
- starch grains outside – and intracellular – no;
- iodophilic bacteria - no;
- mucus - no;
- leukocytes – single ones are allowed;
- red blood cells - no;
- epithelium - no;
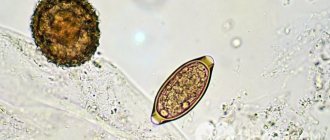
- protozoa - no;
- yeast fungi - no;
- crystals - no.
Modern understanding of the concepts of “enteritis” and “colitis”. Classification of intestinal diseases.
1. Inflammatory bowel diseases.
2.Functional bowel diseases.
3. Organic intestinal diseases (intestinal tumors).
4. Abnormalities of intestinal development.
5. Intestinal diseases caused by enzymopathies.
Non-infectious enteritis and colitis.
This is a group of inflammatory-degenerative diseases of different etiology and pathogenesis, most often of the mucous membrane of the small and (or) large intestines with disruption of all intestinal functions.
Chronic enteritis is a chronic polyetiological inflammatory disease of the small intestine with disruption of its function, structural changes in the mucous membrane, and, over a long period of time, its atrophy.
From a modern point of view, chronic enteritis is considered more like an “enteropathy”, with predominantly dystrophic degenerative, and subsequently atrophic changes in the small intestine. The term “chronic enteritis” itself is largely arbitrary and does not reflect the essence of pathological changes in the small intestine, where inflammatory disorders as such are least represented.
In this case, histologically, along with a very moderate inflammatory infiltration, swelling of the villi, shortening of some of them, flattening of the surface of the epithelium with smoothness of the boundaries between the remaining cells are detected. As a rule, over time, atrophy of the mucous membrane develops, it becomes thinner, the villi become flattened, and for a greater or lesser extent they are completely absent.
Chronic colitis is a chronic inflammatory disease of the large intestine with disruption of its function and the development of dystrophic and atrophic changes in the mucous membrane.
Etiopathogenesis of chronic enterocolitis:
- systematic nutritional disorders;
- industrial intoxication (salts of heavy metals, etc.).
- household intoxication (long-term use of drugs, alcohol, nicotine);
- food allergies;
- radiation injuries;
- concomitant enteritis with pancreatitis, gastritis, cholecystitis;
- genetic predisposition.
Under the influence of etiological factors, inflammatory and dystrophic processes develop in the intestinal mucosa, digestive and motor function is impaired.
According to ICD-10, non-infectious enteritis and colitis include:
1. Crohn's disease.
2. Ulcerative colitis.
3. Other non-infectious gastroenteritis and colitis.
4. Radiation colitis and gastroenteritis.
5. Toxic colitis (lead, arsenic, zinc, mercury, phosphorus, etc.).
6. Drug-induced enteritis and colitis (NSAIDs, cytostatics, antibiotics, corticosteroids, etc.).
7. Allergic gastroenteritis and colitis.
Nutritional factor, helminthiases, giardiasis is a factor predisposing to the development of enterocolitis.
With chronic gastritis, pancreatitis, hepatitis, liver cirrhosis, fermentopathy, intestinal ischemia, dysbacteriosis, secondary enterocolitis may occur.
Who came up with this method for diagnosing constipation?
The method, as its name suggests, was developed by scientists from the University of Bristol, which is located in the UK. It was first published and proposed for the diagnosis of constipation and other disorders in 1997.
Since then, the Bristol scale has been used all over the world - doctors have recognized it as a very effective and important diagnostic method.
- The Bristol scale helps to evaluate only the shape of stool. It does not take into account other indicators, such as color, blood, mucus, undigested particles, etc.
- This method will not help detect many serious health problems, especially in people who have chronic diseases.
- And even more so, you cannot, based only on this scale, independently, without a doctor, diagnose yourself.
However, by the consistency of the stool you can assess the general condition of the intestines and, if necessary, take a laxative to quickly cope with the problem. For example, with functional constipation not associated with serious diseases, the drug Microlax® helps.
Some medications can cause problems with bowel movements. If you start taking any medication and notice a change in the consistency of your stool, you should immediately tell your doctor. Your doctor may stop the medication, prescribe a substitute that doesn't have this side effect, change the dosage, or recommend taking laxatives while you are undergoing treatment.
If you know what types of stool there are and know how to use the Bristol scale, you speak the same language with your doctor. Of course, this will help the doctor more correctly assess your condition and prescribe the most effective treatment.
Type 1 stool spent the longest time in the colon, and type 7 stool spent the shortest time.
Lumpy type feces (1 and 2) are difficult to pass and require straining.
Loose or watery stool passes too quickly and can cause problems.
What type of chair is ideal?
The feeling that you need to have a bowel movement is clear, but not urgent. When you are already sitting on the toilet, there is no delay. No special effort or strain is required. The feces come out smoothly and smoothly. Afterwards, only a pleasant feeling of relief remains.
This corresponds to stool type 4 on the Bristol Stool Scale
Read a more detailed article about constipation in children HERE
About feces in children
Goat pellets in the stool - lack of fluid in the stool and intestinal spasticity (feces are thrown out in portions) Green color - bacteria Sour smell - candida, Yeast-like stool, with candida spores, airy, porous, sour Slurry - bacteria, poor breakdown of complex carbohydrates
Stool color is also important
darker indicates pronounced rotting; lighter indicates fermentation (or takes on the color of the food eaten)