Types of complications
Under favorable circumstances, the ulcer can heal on its own with the formation of a scar at the site of its localization. If this does not happen, the pathology becomes chronic, continuing to destroy the walls of the organ, aggravating the course of the disease, causing serious consequences. Complications that arise during a long course of peptic ulcer disease can also occur chronically, remaining unnoticed for some time. The acute stage of any such pathology can lead to a life-threatening condition. The consequences of peptic ulcer disease can be:
- bleeding;
- penetration;
- perforation:
- pyloric stenosis;
- degeneration of an ulcer into an oncological form.
https://youtu.be/jFiec42I7uA
Perforation of the ulcer
This type of complications of peptic ulcer is characterized by damage (perforation) of the wall of the stomach or duodenum, due to which their contents enter the abdominal cavity. A defect occurs when hydrochloric acid, produced by the stomach during the digestion of food, affects the mucous membrane of the digestive organ, up to the formation of a through wound. If a person is not provided with urgent medical care, he may develop purulent inflammation of the abdominal cavity within a few hours.
Pathology is more often observed in men than in women, the average age of patients is 20-60 years. Perforation of the lower stomach is common, but the duodenum and esophagus can also be affected. The course of the disease can be divided into 3 periods:
- Painful shock is a condition when the contents of the epigastrium enter the abdominal cavity through the resulting hole in the damaged organ. At this stage, the patient feels severe cutting pain in the stomach area, gradually spreading to the entire abdomen, accompanied by fever, vomiting, and tachycardia.
A characteristic manifestation of a perforated ulcer is a board-like tension of the anterior abdominal wall, with significant pain on palpation.The patient has a need to take a position that will give him less discomfort, often lying on his side with his legs pulled up. Symptoms such as pale skin, low blood pressure, and slow heart rate are observed for up to 6 hours.
- Imaginary (false) well-being is a state when the pain shock stops, abdominal pain decreases or disappears completely, and tension in the abdominal muscles decreases. The production of gases in the intestines increases, and increased flatulence occurs. Blood pressure remains low, but the thready (weak) pulse is replaced by a rapid heartbeat, and a sensation of dry tongue and lips appears. The relatively calm period lasts 10-12 hours.
- The development of purulent inflammation of the peritoneum - peritonitis. This is the most severe stage of the disease, accompanied by high fever, a change in skin color to sallow, increasing thirst, and dry mouth. The skin becomes wet, sticky, the amount of urine discharge decreases, disappears completely, and the patient often loses consciousness. Food that enters the abdominal cavity rots, and bacteria multiply in it rapidly, catastrophically quickly. In the absence of urgent qualified medical care, death occurs within 3-4 days.
When diagnosing perforation of the walls of hollow organs, the criterion is the Shchetkin-Blumberg symptom, based on an analysis of the patient’s pain during palpation of the abdominal cavity. A sign of the presence of peritonitis is considered to be a pronounced increase in pain when the palpating hand is quickly removed from the abdominal cavity after slow pressure with three fingers - ring, middle and index. If the pain does not change when removing the arm, the diagnosis is not confirmed.
Articles on the topic
- Peptic ulcer disease in children: diagnosis, causes of development and complications
- Perforated gastric ulcer - treatment and complications
- Medicines for stomach ulcers - a list of medications to eliminate symptoms and prevent
Why does peptic ulcer develop?
The appearance of ulcers on the mucous membranes of the stomach provokes a violation of the internal secretion of the organ. Due to excess hydrochloric acid, the enzyme pepsin and bile, changes in lymph and blood circulation develop, which leads to the formation of ulcers. The main causes of pathology are the following unfavorable factors:
- infection with the bacterium Helicobacter pylori;
- bad habits, especially smoking on an empty stomach;
- stressful conditions;
- chronic diseases of the oral cavity - caries, stomatitis, periodontal disease;
- improper diet;
- uncontrolled use of anti-inflammatory medications;
- other diseases against which a stomach ulcer develops - tuberculosis, syphilis, hepatitis, pancreatitis;
- endocrine disorders.
Ulcer penetration
In the absence of proper treatment, the ulcer gradually develops, extends beyond the stomach, and penetrates into the tissues adjacent to it. In this case, they say that it penetrates, and various organs can be affected - the pancreas, liver, bile ducts, colon. The penetration process is characterized by the development of an inflammatory process, the occurrence of fistulas, and extensive fibrous adhesions. It is carried out in 3 stages:
- spread of the ulcer to all walls of the stomach and duodenum;
- the formation of adhesions between the outer membranes of the stomach or duodenum and adjacent organs;
- penetration of the ulcer into the tissue of a neighboring organ.
Epigastric pain during penetration becomes almost constant, in no way related to food intake; the use of antacids (drugs that neutralize hydrochloric acid in the gastrointestinal tract) does not bring relief to the patient. When penetrating into the pancreas, the pain radiates to the lumbar region; when the lesser omentum is affected, it radiates upward and to the right, towards the shoulder and collarbone.
Symptoms of the penetration process can be painful sensations in the area of the heart, navel, back, they can be of a girdling nature.
Diagnosis of ulcers affecting organs adjacent to the stomach and duodenum is carried out using a general blood test, fibrogastroduodenoscopy, and radiography. The patient's blood exhibits moderate leukocytosis and accelerated ESR. X-ray examination of the stomach during penetration reflects the deepening of the crater and the immobility of the localization zone of the formation. The results of fibrogastroduodenoscopy show round edges raised around the ulcer. Using ultrasound, changes in the liver and pancreas are recognized if penetration occurs in these organs.
Diagnosis of the disease
Laboratory and instrumental methods are used to make a diagnosis.
Laboratory diagnostics
Laboratory tests may indicate hidden bleeding or worsening of the ulcer. In a general blood test, a slight increase in the content of leukocytes and an increase in ESR are sometimes observed. When a chronic gastric ulcer often worsens and is accompanied by microbleeding, signs of anemia are possible: decreased hemoglobin concentration, decreased number of red blood cells, low hematocrit.
Gastric juice is also examined to determine the level of acidity, and stool is analyzed for the presence of occult blood. To determine Helicobacter pylori infection, a urease breath test and bacteriological examination of gastric contents, and enzyme immunoassay are used.
In peptic ulcer disease, the natural folds of the mucous membrane converge radially in the area of the defect, which can be determined using contrast radiography
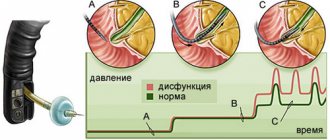
Instrumental methods
The most important and decisive method for diagnosing gastric ulcers is fibrogastroscopy (FEGS), in which a defect in the wall of the stomach is detected, its location, size and other parameters are determined. During FEGS, a biopsy is often taken (a small sample of tissue is pinched off with tweezers for histological examination) - this is necessary to clarify the nature of the ulcer and exclude cancer.
Important: you should consult a doctor at the first signs of a stomach ulcer in order to promptly diagnose the disease and receive the necessary treatment.
Additional studies include contrast radiography, electrogastroenterography and manometry. Characteristic radiological signs are the symptom of a “niche on the contour”, a filling defect and radial convergence of the folds of the stomach.
Manometry and electrography make it possible to determine violations of the motor function of the organ. You can learn more about the causes, types and how to identify a stomach ulcer by symptoms from this video:
Ulcerative bleeding
Complications of gastric and duodenal ulcers, accompanied by bleeding, occur no less frequently than perforation of the ulcer. Symptoms of this form of development of pathology can manifest themselves in the form of bloody vomiting, tarry (black) stools, the patient’s well-being in some circumstances changes slightly, with the ability to lead a normal lifestyle, in others it requires emergency medical intervention. There are 2 types of ulcer bleeding:
- Hidden - the patient may not be aware of the disease until it is reflected in the test results or there is a sharp deterioration in his health.
- Open – has recognizable symptoms, the patient’s condition is characterized by severe pallor of the skin, mucous membranes, dizziness, fainting, general weakness, shortness of breath, tachycardia. Sometimes collapse occurs - the face becomes pale, the pulse becomes thready, and the patient loses consciousness.
Diet to prevent stomach ulcers
Changing the diet is considered one of the key points on which the effectiveness of the prevention and treatment of gastric and duodenal ulcers depends. Failure to comply with the diet will lead to aggravation of the situation, bleeding and even death.
Basic rules for creating a diet.
- You need to select dishes only taking into account their ease of digestibility.
- Eliminate any factors and products that lead to inflammation of the mucous membrane.
- Avoid hot and cold dishes, heating food to 25-35 degrees.
- Prevent hunger. It is better to eat more often, but in small portions.
- Increase fluid intake.
Healthy foods:
- lean meat;
- lean fish, completely free of bones and cartilage;
- soft-boiled eggs and omelettes;
- potato;
- beet;
- carrot;
- cauliflower;
- pumpkin and zucchini;
- porridge: semolina, rice, buckwheat, oatmeal;
- pasta;
- crackers;
- biscuits;
- White bread;
- fruit puree;
- jam and marmalade;
- honey;
- milk.
The maximum allowable amount of salt per day is up to 6 g.
Contraindications:
- spicy;
- fat;
- salty;
- roast;
- herbs and spices;
- sausage;
- any conservation;
- radish;
- cucumbers;
- legumes;
- horseradish and mustard;
- onion and garlic;
- nuts;
- chocolate;
- citrus;
- sweet pastries;
- sparkling water;
- strong tea or coffee.
It is better to entrust the preparation of the complex to an experienced nutritionist, because this will help provide the body with all the necessary vitamins and minerals, preventing irritation of the walls. The selected products can eliminate the side effects of medications and enhance their effectiveness.
Without diet, treatment and prevention of gastric ulcer is impossible!
Pyloric and duodenal stenosis
Complications of stomach and duodenal ulcers can manifest themselves in the form of narrowing of the lumens of the pylorus (the septum that regulates the flow of stomach contents into the intestines) and the duodenum. This condition is called stenosis, the frequency of its occurrence in patients with ulcerative pathology is up to 15%. The course of the disease in this case is characterized by the following stages:
- Compensated pyloroduodenal - moderate narrowing of the lumen, in which increased motor activity of the stomach is required to push the food bolus. The patient experiences heartburn, sour belching, and a feeling of excessive stomach fullness after eating.
- Subcompensated - a violation of the evacuation abilities of the stomach, characterized by profuse vomiting some time after eating. Contents are found in the stomach even on an empty stomach, the patient feels a putrid odor from the mouth, pain even when taking a small portion of food.
- Decompensation - a progressive weakening of the motor function of the stomach, in which vomiting becomes frequent, does not bring relief. Thirst occurs, spontaneous muscle contractions, cramps, and the patient’s stomach expands greatly. Treatment of pyloric and duodenal stenosis at this stage of development should be surgical.
Causes and risk factors
Science considers Helicobacter pylori to be the main “culprit” of peptic ulcer; this bacterium is found in 97% of patients. However, bacteria constantly “live” in the digestive canal of many people, but do not cause either an ulcerative process or inflammation.
We recommend reading:
Intestinal inflammation: signs of pathology, use of diet and drugs for treatment
For the formation of an ulcerative defect, additional provoking moments are needed, which are as follows:
- taking medications that are collectively called “ulcerogenic” or that can damage the gastric mucosa: non-steroidal anti-inflammatory drugs, corticosteroid hormones, cytostatics, potassium preparations, centrally acting antihypertensive drugs;
- chronic systemic diseases: tuberculosis, chronic kidney failure, diabetes mellitus, sarcoidosis, viral hepatitis and cirrhosis of the liver, pancreatitis, syphilis;
- acute conditions in which the body is on the verge of survival: shock, massive burns, trauma, frostbite, sepsis;
- systematic eating dry food, eating stale foods, eating inedible things (occurs in mentally ill patients);
- emotional stress, especially chronic, and the predominance of negative emotions;
- abuse of alcohol and especially its substitutes;
- smoking;
- poverty and negative social processes that a person cannot overcome due to objective reasons.
Malignancy
In a chronic course, peptic ulcer of the stomach and duodenum can develop into a malignant form - malignancy. In the early stages, it is difficult to determine the presence of an oncological process by external manifestations; the main symptoms are the ineffectiveness of diet therapy and drug treatment. As the disease progresses, more pronounced signs of malignancy appear:
- decreased appetite, aversion to meat dishes;
- weight loss, exhaustion;
- pain in the stomach that cannot be eliminated by medications or food;
- abnormal stool, alternating constipation and diarrhea, the appearance of blood in the stool;
- nausea, vomiting, belching with a sour, putrid odor;
- heaviness, discomfort in the stomach;
- pallor of the skin and mucous membranes;
- asthenia – increased fatigue, impotence, weakness.
Treatment
Treatment is complex, one or another method is used to a greater or lesser extent depending on the specific situation.
The basis of recovery is following a diet, which changes slightly during periods of exacerbation and calm.
Diet
Proper nutrition for peptic ulcer disease is table No. 1 according to Pevzner, during an exacerbation 1A, and during remission or lull 1B.
We recommend reading:
H2-histamine blocking drugs and their use in gastroenterology
Table No. 1 consists of boiled, steamed or baked dishes without crust with a meal frequency of up to 6 times a day, a limit on table salt and a total calorie content of up to 3000 per day. The diet is complete and contains a full range of nutrients.
| Recommended Products | Not Recommended Products |
|
|
During an exacerbation, dishes are additionally pureed (table 1A) and served in a mushy form, and during remission they are prepared in the usual way. During an exacerbation, the amount of food should be reduced slightly, and be sure to stick to room temperature, since both cold and hot things greatly irritate the stomach.
Drugs
Drugs are used that act on the cause of the disease (etiotropic) and alleviate the symptoms (symptomatic). However, it is difficult to identify these drugs in each specific case, since peptic ulcer disease has many causes. The following groups of medications are used:
- antacids - neutralize hydrochloric acid and gastric pepsin;
- antisecretory drugs - suppress the production of gastric juice;
- proton pump inhibitors - suppress the synthesis of enzymes necessary for the production of hydrochloric acid;
- anticholinergics - also reduce acid production;
- antibacterial drugs - act on Helicobacter.
Depending on the situation, the underlying disease is treated if it led to the formation of an ulcer, the emotional state is normalized, or the effect of hormones is neutralized.
Surgery
It is used if conservative treatment does not bring the desired result, the ulcer has perforated or a narrowing (stenosis) has formed due to scarring.
Types of operations performed
- intersection of the branches of the vagus nerve, which stimulates the production of hydrochloric acid or vagotomy;
- removal of part of the stomach along with an ulcer - various modifications of the Billroth operation;
- restoration of patency of the pylorus of the stomach and duodenal bulb due to cicatricial narrowing or pyloroplasty;
- endoscopic operations performed without a wide incision - suturing an uncomplicated ulcer.
We recommend reading:
Intestinal ulcer: symptoms and manifestations of the disease, treatment methods
Recovery period
It proceeds faster and easier after endoscopic interventions, since there are practically no surgical wounds. After abdominal surgery, especially peritonitis caused by perforation, the rehabilitation period can drag on for several months.
During rehabilitation, bed rest, table No. 1A, and medications according to the situation are recommended.
Folk remedies
The use of traditional medicine methods is possible only during the next exacerbation of a peptic ulcer, if it is mild, as a supplement to the main treatment prescribed by a gastroenterologist.
Fresh potato juice has a good healing effect , which should be consumed daily half an hour before meals several times a day. The use of this method is limited by the fact that in urban conditions it is very difficult for a working person to adhere to such a frequency of administration.
Traditional medicine also recommends ghee with propolis, St. John's wort decoction, mumiyo, and plantain juice.