A well-designed diet for gastric reflux gastritis is even more important for eliminating the symptoms of the pathology than prescribing medications. A diet aimed at neutralizing digestive juices with high acidity, restoring the balance of intestinal microflora and accelerating the healing of damaged mucosa will help to quickly restore performance in case of esophagitis and gastritis and return to your normal lifestyle.
List of prohibited products
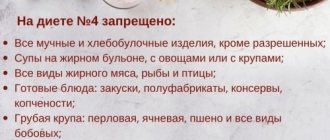
A diet for GERD with high acidity - low levels accompany this pathology in exceptional cases - prohibits many foods. But first of all, you need to give up the following:
- Drinks – alcohol-containing, strongly brewed black teas, cocoa, coffee, any soda, drinks with mint flavor and prepared on its basis.
- Chocolate.
- Vegetables and fruits that can cause heartburn. The list is individual in each case.
- Dairy products with high fat content - milk (more than 2%), yoghurts, cheeses, cottage cheese, cream.
- Roasted meat products.
- Fried foods, in particular potatoes.
- Fast food.
The dishes are spicy in taste.
List of approved products
The diet for gastroesophageal reflux disease is quite varied, which is due to a fairly wide list of permitted foods.
What to eat:
- Eggs. They are served exclusively soft-boiled (no more than 2 pieces per day) or in the form of an omelet cooked in a double boiler.
- Low-fat fish - navaga, perch, cod, carp, pike perch.
- Dietary varieties of meat are veal, poultry (the skin must be removed), beef, rabbit. Can be served in the form of meatballs, cutlets, soufflés and casseroles. Steam or bake in the oven under foil.
- Fermented milk and low-fat dairy products. After meals, low-fat yogurt, yogurt and kefir are allowed. Cottage cheese seasoned with sour cream or in a casserole. Non-acidic sour cream can be used for dressing. Milk - depending on individual intolerance.
- Vegetable oils (corn, olive, sunflower) - no more than 20 ml per day.
- Butter – no more than 20 grams per day.
- Fresh vegetables - peeled tomatoes, cucumbers, cabbage with soft leaves, carrots, greens.
- Potatoes, peas, pumpkin, zucchini - for making purees and casseroles.
- Yesterday's bread made from wheat flour.
- Porridge (semi-liquid or pureed). Semolina, oatmeal, rice and buckwheat are allowed.
- Sweets - marmalade, plain cookies, jelly, jelly, marshmallows.
- Fruits and berries with a sweet taste, in particular watermelon. They help strengthen the immune defense and also provide the body with all the necessary vitamins. But if you have GERD, eating them fresh is prohibited: they can provoke heartburn by increasing the production of gastric juice. Bananas and exotic fruits should be eaten before meals.
- Soups. To prepare the dish, skimmed (low-fat) broths are used. It is prohibited to use all types of legumes (peas, beans, lentils) for thickening. It is advisable to prepare puree soups, since they have virtually no effect on the mucous membrane of the esophagus and stomach. The menu can be varied with pasta, fruit, and milk soups. They can also be prepared from fish or chicken.
- Side dishes. Pasta can be served no more than 2 times a week. Mashed potatoes.
Healthy recipes
During the acute stage of the disease and during its transition to the resting stage, all dishes are pureed and served at a comfortable temperature
The diet for gastritis with reflux in the acute stage is extremely simple; no special recipes are required. The diet consists of mineral water, herbal decoctions, pureed rice porridge with water, and mashed baked sweet apples. After a few days, improvement occurs and the diet expands. You will have to follow a strict diet for at least 3 months, so it is worth stocking up on interesting recipes that will not harm the patient and will delight him on weekdays and holidays.
Beetroot dietetic
Beetroot soup without tomato paste is suitable for a patient with reflux gastritis; sour cream and herbs are added after the disease becomes chronic
This light soup is best prepared in the summer from young root vegetables and served completely cooled at room temperature. An excellent alternative for patients who find it difficult to give up borscht.
Ingredients for cooking:
- beets – 1 large;
- carrot – medium;
- potatoes - 1 medium;
- onion - half;
- salt, vegetable oil.
Cooking algorithm:
- Wash the vegetables, peel and cut into strips.
- Bring 2 liters of water to a boil in a saucepan, place the vegetables in a saucepan, pour in a spoonful of vegetable oil, and also put on the fire.
- Cook vegetables, stirring, 5 minutes. – they shouldn’t fry. Pour in two ladles of water from the pan and simmer covered for 10 minutes.
- Place the vegetables in a pan of boiling water, add salt, cover with a lid, and cook until fully cooked.
- Turn off the finished beetroot soup and cool. Grind in a blender or rub through a sieve.
If desired, chicken quenelles and liver soufflé are served with beetroot soup - recipe below.
Liver soufflé
To prepare liver soufflé, use an oven or slow cooker.
This dish is an alternative to fatty liver pate; it is served as a stand-alone dish for breakfast, dinner, or as a side dish for viscous porridges. You can serve the soufflé with biscuits and toasted bread.
Ingredients for cooking:
- chicken or beef liver, fresh, not frozen – 500 g;
- egg - 2 pieces;
- carrot – 1 medium;
- milk - a third of a glass;
- flour – 3-4 tablespoons;
- salt;
- butter.
The classic recipe calls for onions. The vegetable is added for long-term, persistent remission.
Cooking algorithm:
- Wash the carrots and boil in boiling water for 15 minutes.
- Rinse the liver, remove all veins and films, trim off the fat, cut into pieces if necessary.
- Using a blender or meat grinder, puree the liver with carrots.
- Separate the whites from the yolks. Grind the yolks with salt and add to the liver mass.
- Pour in milk, stir, add flour, stir again.
- Beat the whites and carefully fold into the mixture.
- Grease the mold with butter and carefully pour the mixture. Place on a baking sheet, pour half a glass of cold water onto the bottom of the baking sheet, bake in the oven at 180 degrees for 30-40 minutes.
Cool the soufflé, cut into slices, serve with toasted bread, mashed potatoes, or porridge. A soufflé from poultry or fish fillet is prepared in the same way.
Diet according to Pevzner
When diagnosing GERD, the patient is assigned to table No. 1. It is necessary to observe it during the period of exacerbation or during the initial detection of the disease. Duration – 1 week. The menu includes gentle dishes that can have minimal impact on the inflamed esophageal mucosa. This promotes accelerated healing and scarring of the resulting ulcers.
Allowed foods can be boiled or steamed. Dishes are served pureed or liquid. Serving hot or cold is prohibited: food must be warm. The patient is served steamed omelettes, jelly, soups, and various cereals. Meals for GERD are divided - every 3 hours in small portions. The diet for GERD with esophagitis and high acidity of gastric juice has some differences.
If the disease is complicated by the development of esophagitis, then the patient’s food is served exclusively pureed. This solves the typical problem of dysphagia for this form of the disease (pain when swallowing, food getting stuck in the throat). For breakfast, it is recommended to serve porridge and warm teas; kefir is ideal for an afternoon snack. For lunch - puree soup. Boiled vegetables can be garnished with mashed potatoes, first crushed using a blender.
With a combined course of GERD and gastritis, in which acidity is increased, a gentle diet is necessary. Sweets, spices, fatty/spicy foods, and carbonated drinks are strictly prohibited. The menu must be agreed with the attending physician.
During the period of exacerbation of GERD, in addition to taking medications, it is necessary to follow a strict diet. The patient is allowed porridge cooked in water and other boiled dishes. You need to follow it for one to two weeks, until your overall well-being improves.
Sample daily menu:
- breakfast - porridge and rosehip decoction;
- second breakfast - cottage cheese;
- lunch - soup, boiled breast with a side dish of boiled vegetables;
- afternoon snack - vegetable salad of boiled beets with carrots, seasoned with vegetable oil;
- dinner - vegetable stew or cottage cheese casserole.
During the period of remission of the disease, the list of permitted products can be slightly expanded. For example, a patient can eat sweets, but in limited quantities. Fatty dishes and foods are still prohibited.
Sample menu for the day:
- breakfast – cottage cheese with sour cream, tea, dry biscuits;
- second breakfast - sweet berry jelly;
- lunch - soup with low-fat broth, boiled meat with side dish;
- afternoon snack – sweet juice with biscuits;
- dinner - steamed cutlets, garnished with vegetable stew.
Prevention of exacerbation of GERD consists of following the basic principles of dietary nutrition. For breakfast, you should serve porridge, adding raisins to it for variety and improved taste. Second breakfast - biscuits and permitted drinks. Cereal soups, lean meats, and vegetable salads are good for lunch. Afternoon snack – a decoction of rose hips and jelly. You can take fish to prepare dishes for dinner.
Herbal decoction
Traditional medicine offers many recipes for herbal decoctions that help alleviate the human condition and improve the digestion process.
Medicinal decoctions:
- chamomile relieves inflammation and soothes;
- Rose hips are rich in vitamin C and have a beneficial effect on the stomach;
- calendula relieves discomfort and inflammation in the stomach;
- plantain has healing abilities.
All decoctions can be drunk throughout the day in between meals. Taking decoctions before bed is most effective.
Treatment of gastritis reflux consists of adjusting nutrition and following a certain diet. Specially selected ingredients improve digestion, reduce stress on the stomach and eliminate the unpleasant symptoms of gastritis.
Basic lifestyle recommendations for gerb
A detailed list of prohibited and permitted foods allows you to follow the instructions exactly and easily create a varied daily diet and menu for the week. Additional intake of medicinal herbal decoctions will help you quickly cope with the discomfort of gastritis and improve your well-being.
The information on our website is provided by qualified doctors and is for informational purposes only. Don't self-medicate! Be sure to consult a specialist!
Gastroenterologist, professor, doctor of medical sciences. Prescribes diagnostics and carries out treatment. Expert of the group for the study of inflammatory diseases. Author of more than 300 scientific papers.
Diseases of the gastric tract are among the most common pathologies. This is easily explained: the accelerated pace of life, unbalanced and irregular nutrition, constant stress and bad habits can undermine even good health.
Reflux gastritis is an insidious disease. For a long time the patient does not notice any negative manifestations, and when they appear, it turns out that the disease is in an acute form. In this case, medications alone are not enough; you also need to adjust your diet. The diet and menu for each day are approved together with the attending physician, so that the food is not only healthy, but also tasty.
So, what is gastritis reflux, how does it differ from ordinary inflammation of the stomach, and what foods can patients eat?
Diet for reflux
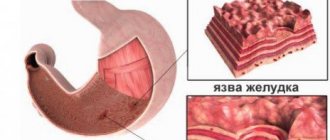
Reflux gastritis develops due to the fact that the sphincter muscles begin to work in the wrong mode. As a result of the pathology, the contents of the duodenum are released into the patient’s stomach. Reflux is considered a form of chronic gastritis, and therefore requires clear treatment. Diet for reflux is a mandatory part of therapy.
The disease, or rather the discharge, is filled with harmful acids, which significantly damage the mucous-type lining in the patient's stomach, which is the main cause of gastritis.
Almost everyone has heard about gastritis, but not about its reflux form. Therefore, it is important to understand in detail what it is, as well as what diet is necessary for reflux gastritis .
Important! Diseases associated with the gastrointestinal tract require in-depth analysis. That is why it is important not to come up with a treatment for yourself, but to contact a specialist who will think through all aspects of therapy, including dietary nutrition.
Video
Gastroduodenal reflux (GDR) is the reflux of contents from the duodenum into the stomach. This process occurs in approximately 15% of healthy people, mostly at night. Reflux is considered a disease if daily intragastric pH-metry reveals an increase in the acidity of gastric juice above five.
In 30% of patients, duodenogastric reflux is considered an independent pathology. In the remaining 70%, GHD accompanies diseases of the initial parts of the gastrointestinal tract. Men and women suffer from this disease equally.
Symptoms of the disease
The problem in detecting and further working on this problem is that the pathology itself, as a rule, occurs without pronounced symptoms. However, in some cases, the following signs of the disease are present:
- Dizziness, a state of general weakness.
- Reluctance to eat, weight loss.
- Painful sensations in the stomach, especially after eating.
- A feeling that the stomach is full both during and immediately after eating. Often accompanied by bloating, belching, and a bitter taste.
- Constipation/diarrhea, which may alternate.
- Sometimes severe dry mouth occurs, causing small ulcers to appear on the skin around the lips.
- Nausea and vomiting, which is mixed with bile.
Symptoms, treatment and diet for reflux gastritis should be taken into account by everyone who suffers from problems with the gastrointestinal tract. The thing is that quite often patients do not even suspect that there is a problem. Due to the absence or weak manifestation of signs, this is understandable.
Important! Regularly conduct complete examinations with a gastroenterologist, immediately contact a specialist if there are deviations that may seem unimportant to you. Any little things can signal a serious pathology.
What should be in the diet
Important! The diet for autoimmune hypothyroidism or other disorders of this type has its own specific characteristics, which is why only a specialist must prescribe nutrition and create a menu.
It is important to understand that another subtype of the disease, duodenogastric reflux, is not always a pathology and can manifest itself in a completely healthy person. Thus, the problem has been recorded in a significant number of people at night, during sleep. However, if acidity increases by more than 5 percent per day, then such a deviation is already considered pathological and requires special treatment. You also need a diet for duodeno-gastric reflux .
Diet food
Almost all deviations from the norm that are associated with the gastrointestinal tract are accompanied by therapeutic nutrition. This integral part of therapy allows you to restore the correct flow of all processes in the body. This disease is characterized by specific symptoms, so all treatment is aimed at restoring motility function in the intestine. In addition, the treatment ensures the normalization of microflora, binds bile acids, and also neutralizes them. All this helps reduce the negative effect on the gastric walls.
A diet for gastric reflux gastritis works exclusively in conjunction with drug treatment. Only in pairs can therapy restore the body and bring all systems into proper condition. The diet for neutralizing acids should be as gentle as possible, therefore it cannot include the following foods and dishes:
- High fat content.
- Too spicy and spicy.
- Salty.
- Fried.
- Canned, pickled.
- Smoked.
All of the previously listed products can cause severe irritation of the gastric mucosa and also cause damage to it. However, in addition to this, the diet for gastric reflux excludes components that can provoke dumping syndrome. These products include honey, milk porridge, sugar and jam. Alcoholic drinks and cigarettes are completely prohibited.
Dietary nutrition for this pathology is characterized by a number of specific requirements:
- Clear meal schedule by the hour. It should be the same every day. It is worth eating often and in small portions.
- The food consumed should be at room temperature, and be sure to avoid very hot and cold foods. This also applies to drinks.
- Drinking is prohibited during meals. This can be done before/after 15 minutes.
- Based on acid levels, drinking mineral water is often recommended.
Important! The diet menu for gastric reflux gastritis should be as thoughtful and balanced as possible. Therefore, it is better to have it compiled by a professional. Remember that treatment of pathology without proper nutrition is usually ineffective and very long-lasting. In addition, harmful products can cause serious deviations and worsening of the condition.
Next, it is worth considering the list of those dishes that are acceptable and recommended for eating with this pathology. These include:
- Slimy types of soups that are prepared from certain types of cereals.
- Not a strong brewed tea, which is best diluted with milk.
- Dairy types of soups, but with ground cereal.
- Kissel/puree/jelly (necessarily from fresh fruits and berries that are well ripened).
- Vegetable-type soups must be pureed, and the broth must be weak.
- Boiled meat, always finely chopped or ground.
- Porridge with milk – preferably slightly viscous and pureed. It is imperative that the cereal is well boiled.
- Boiled or steamed fish.
- Eggs - you can cook them soft-boiled, steamed omelet or use only whites.
- Whole milk, cream.
- Vegetable puree. Potatoes, cauliflower, zucchini, carrots, etc. are suitable for gastroesophageal reflux diet.
- Fresh, non-sour cottage cheese, which is well ground.
- Stale bread made from white flour.
Diet menu for reflux gastritis
The very first thing doctors recommend, in addition to medications, is a diet for such reflux gastritis. Without it, the situation may simply get out of control.
Special nutrition is the most necessary thing for such a disease. Separately, medications will not give any effect, they will only dull the symptoms and hide the pain, and then not for long. If nothing is done about such gastritis, an ulcer, intestinal or stomach tumor develops very quickly. But this diet should only be prescribed by a doctor, taking into account the patient’s condition. Perhaps it is at this moment of examination that an exacerbation occurs, which requires completely different measures than the initial stage.
In addition, reflux gastritis often occurs against the background of other diseases, for example, it often occurs with esophagitis - a disease of the esophagus and inflammation of its lining. In this case, the diet should be slightly different, so as not to irritate the esophagus, food should be crushed as much as possible.
But first, before radically changing your lifestyle, you need to make sure that the disease exists at all.
Symptoms of reflux gastritis
The danger of the disease is that in the first stages it is not felt at all and is asymptomatic. But in some cases the following unpleasant moments can be traced:
- Pain in the stomach that appears immediately after eating.
- Feeling like your stomach is full, even when you are hungry or have just started eating, a feeling of heaviness.
- Constant bloating, belching with an attack of bitterness.
- Nausea, vomiting (bile in vomit).
- Problems with the toilet - constipation or, on the contrary, diarrhea.
- Ulcers appear in the corners of the lips, a feeling of thirst and dry mouth.
- Dizziness, feeling of weakness.
- Weight loss due to decreased appetite.
All these symptoms do not appear immediately. There may be one or two present at the initial stage, which any person attributes to fatigue, ailments and does not attach importance to them. However, if they are definitely related to the stomach, then it is better to contact a gastroenterologist and simply carry out preventive examinations. After the onset of the disease, it progresses rapidly, all symptoms become more obvious and pronounced.
Advice from a gastroenterologist
The disease causes discomfort and disrupts a person’s usual way of life. Therefore, the patient’s natural desire is to get rid of reflux and its associated symptoms.
To achieve an effective treatment result, gastroenterologists advise:
- Adhere to the diet and nature of your diet, exclude from the menu foods that provoke bile reflux.
- Reduce the impact of stress factors and other negative causes.
- Treat concomitant diseases in a timely manner.
- Include regular moderate physical activity.
- Stabilize your weight.
- Follow the recommendations of a specialist on taking medications.
- Give up bad habits - alcohol and smoking.
Pathology of the digestive system, which is accompanied by the entry of bile into the upper sections, can be successfully treated thanks to modern methods of diagnosis and treatment. However, the main condition on the path to recovery is the joint work of the doctor and the patient.
Why does the disease occur?
Knowing the risk group, you can quickly determine that reflux gastritis has begun, so as not to waste time. Here are the following factors:
- operations on the stomach or intestines;
- long-term use of antibiotics and other strong drugs, such as hormones;
- abuse of nicotine and alcohol;
- constant stress and nerves;
- predominantly poor nutrition, addiction to fatty and spicy foods, which are characterized by high acidity;
- irregular meals.
If all these points apply to you, then preventive examinations with a doctor should become a mandatory norm.
Why is there a lot of bile in the stomach?
Reflux is more common in people of middle and older age groups. Less commonly seen in children. Let's look at the reasons for the reflux of bile into the stomach and esophagus and give advice from gastroenterologists that reduce the risk of developing the disease. There are pathophysiological factors that cause secretions to accumulate in the intestines and move up. These include conditions:
- decreased tone in the lower parts of the digestive tract;
- dysfunction of the sphincter of Oddi;
- changes in the nervous coordination of the gastrointestinal system;
- thickening and stagnation of bile in the gallbladder;
- increased pressure in the abdominal cavity.
If there is a lot of bile in the stomach, external reasons may be:
- Inflammatory processes of the liver, gall bladder and bile ducts.
- Formation of stones in the lumen of the bile ducts and bladder.
- Taking medications for a long time, which leads to a decrease in sphincter tone (NSAIDs - non-steroidal anti-inflammatory drugs).
- Tumors of benign and malignant nature.
- Surgical interventions: removal of the gallbladder, radical surgical techniques for stomach cancer, reconstruction of the pylorus and bile ducts.
- Constant physical activity, which leads to increased intra-abdominal pressure.
- Overeating, especially fatty foods.
- Alcohol abuse and smoking.
- Overweight.
- Long-term exposure to stress factors.
- The release of bile into the stomach is also observed during pregnancy.
The combination of several unfavorable factors increases the likelihood of developing pathological reflux of bile into the stomach and esophagus.
Treatment of reflux gastritis
As mentioned above, all treatment is based on two pillars: taking medications and a special diet. In addition, if superficial gastritis began due to complications after surgery, then doctors are in no hurry to prescribe medications. On the contrary, they can cause exacerbation, and sometimes even the development of ulcers. In this case, all that remains is to strictly follow the diet - and then the symptoms will disappear on their own.
If reflux gastritis becomes acute, then medications are urgently prescribed to stabilize the proper functioning of the duodenum, and vitamin complexes are prescribed. And only in the most advanced cases is surgery performed.
Diet for reflux gastritis
To restore healthy intestinal motility, reduce acidity and general symptoms, a therapeutic diet is simply necessary. It should also normalize the natural microflora in the stomach. Diet foods are less irritating to the walls of the stomach and intestines.
A special gentle menu should exclude the following types of products:
- fat;
- fried;
- spicy;
- too spicy;
- canned;
- salty.
It is also necessary to exclude products that cause dumping syndrome. This is honey, jam, too-fatty porridge with milk, and fatty dairy products in general. Naturally, alcohol and cigarettes are prohibited.
Meals should be small, but frequent. Eating occurs at the same time. And the dishes cannot be hot or cold - only warm. During the meal itself, it is forbidden to drink, even if it is just clean water. You can drink only after 20 minutes have passed. Depending on the acidity of the stomach, in most cases mineral waters have a very beneficial effect.
Physiology of bile secretion
Bile formation is a continuous process carried out by liver cells. Its accumulation and concentration occurs in the gallbladder.
When food enters the upper parts of the digestive tract under the influence of nerve impulses, the secretion of the common bile duct enters the duodenum through the sphincter of Oddi, where it participates in the digestion of the bolus of food. In a healthy person, motor and secretory function is a harmonious system. However, if its functioning is disrupted, bile reflux into the stomach and food may enter the upper digestive tract.
Menu and dishes to eat
You can immediately indicate the dishes that are allowed on the diet. The daily menu is formed from them, just alternate them for variety. These include:
- viscous soups from cereals;
- milk soups, only cereals should be ground;
- vegetable broth soups;
- viscous porridge;
- steamed or boiled lean meat;
- boiled or steamed fish;
- mashed potatoes and other vegetables with water;
- steamed omelettes and hard-boiled eggs;
- fresh and not too fatty cottage cheese;
- yesterday's bread or oven-dried crackers;
- a little butter and refined oil;
- jellies and mousses from fruits and berries (non-acidic);
- weak tea, maybe with milk.
You cannot eat flour, cakes, chocolate, various pastries and pies. Any seasonings, semi-finished products, canned food are prohibited. Steep meat broths should also be excluded. Mushrooms are dangerous during this period, it is better to remove them. Pure vegetables and fruits are undesirable. Fermented milk products are prohibited. If you follow the menu, reflux gastritis will go away very quickly.
How to create a patient’s diet for a week and a day
At first, creating a balanced menu is difficult, but after two to three weeks the patient gets involved and gets used to the new food culture
The menu for every day for reflux gastritis necessarily includes a liquid dish (mucoid soup with cereals, pureed vegetable soup with water), a meat or fish dish in the form of pate, meatballs, quenelles as a source of protein and a fruit dessert in the form of soufflé, mousse, jelly as a source of vitamins and minerals.