An ulcer is fraught with serious complications. The doctor treating the patient makes a variety of prescriptions, but one of them is a mandatory diet after stomach bleeding. It comes to the most prominent place in this pathology. It is this that allows you to restore the functions of the organ, stabilize the condition of its mucous membrane and alleviate the symptoms of the disease.
If the patient is in the stage of severe exacerbation of peptic ulcer disease, then he is given intravenous nutrition, but most often a regular diet is used. Specialists have developed tables 1, 1a and 1b . If the pathology is complicated by intestinal bleeding, then No. 4 .
Diet after stomach bleeding
When such a complication of a peptic ulcer develops, the patient is recommended to eat a low-calorie diet, divided into small portions, which are served to him five to six times a day.
This diet reduces the overall acidity of the stomach, normalizes muscle contractions of the organ and restores the cells of its inner lining.
The diet helps the patient during the rehabilitation period and alleviates his condition.
General rules and principles
The main requirements for the treatment table after ulcer bleeding are:
- careful processing of products;
- complete refusal of food that stimulates the internal glands that produce hydrochloric acid;
- steaming or pureeing food;
- inadmissibility of any overeating;
- preventing the consumption of overheated or supercooled food; maximum reduction in its calorie content;
- anesthesia.
Authorized Products
To completely improve the digestive system, it is necessary to give preference to a variety of soups, preferably vegetable ones, seasoned with buckwheat, semolina, oatmeal or rice.
Plant foods seasoned with eggs and milk, as well as lean minced meat, fish or poultry can be very useful.
The patient is allowed to eat some lean ham, jellied, well-processed seafood, liver pate or lean herring.
Rolling oats, buckwheat, semolina or rice porridge can be useful for ulcers in the period after gastric bleeding.
It is allowed to eat chopped vermicelli or noodles that have been thoroughly boiled beforehand.
Very often they make puree from broccoli, natural green peas, potatoes, carrots, and beets. You can season your dishes with fresh parsley. They snack on biscuits, stale bread or rolls.
Fresh kefir, milk, fermented baked milk, not too rich cream, low-acid sour cream, cottage cheese, grated cheese, as well as eggs in a bag or in the form of a steamed omelet, will be useful for a person suffering from a stomach ulcer, especially with bleeding.
For dessert, it is better for the patient to serve jelly, marshmallows, jelly, compote, honey, meringues, marshmallows, puree or sweet jam.
It is recommended to drink infusions and decoctions of medicinal plants, juice from sweet fruits or berries and weak tea diluted with milk.
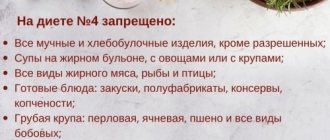
Prohibited Products
The following should be completely excluded from your daily diet:
- spicy dishes;
- fried food;
- fatty meats, poultry and fish;
- canned food;
- alcohol;
- pancakes;
- rich broths from meat or fish;
- fresh baked goods;
- freshly baked bread;
- rutabaga;
- peas;
- dairy products with pronounced acidity;
- radish;
- turnip;
- sorrel;
- sour berries;
- cabbage;
- squash and eggplant caviar;
- mushrooms;
- dried fruits;
- decoctions of fiber-rich vegetables;
- wheat;
- hominy;
- ice cream;
- chocolate;
- any fatty sauces;
- salt;
- sugar;
- spices;
- coffee;
- barley;
- barley porridge, etc.
Causes
The reasons for the development of bleeding from the esophagus are as follows:
- Varicose veins of the esophagus. It is this pathology that causes most severe bleeding. It is formed as a manifestation of the late stage of various diseases, leading to an increase in pressure in the portal vein system. This leads to stagnation of blood in the veins of the esophagus, their enlargement, stretching, tortuosity, and the formation of varicose nodes. The wall above the varicose veins stretches, thins, and becomes easily wounded. It can be damaged even with careful examination with an endoscope, consumption of even relatively hard food, vomiting, straining, and surges in blood pressure. In addition, her inflammation can quickly set in, which makes her even more vulnerable.
In 80% of cases, esophageal varicose veins form as a complication of liver cirrhosis and liver failure. The insidiousness of this pathology is that dilated veins do not make themselves felt for a long time and the first manifestation is sudden massive bleeding.
Varicose veins in the esophagus can be the result of a congenital abnormality of their structure. But this is rare and, as a rule, does not lead to such a significant increase in them as with acquired varicose veins.
With cirrhosis of the liver, the veins in the lower part of the esophagus, where the portocaval anastomoses are located, are affected. In heart failure, varicose veins also form. As a rule, veins change along the entire length of the esophagus. With malignant goiter, changes in veins form in the upper parts of the esophagus.
- Mallory-Weiss syndrome. Its essence is longitudinal ruptures of the esophagus during vomiting. About 10% of all gastrointestinal bleedings are due to this pathology.
- Injury to the esophagus due to chest injuries.
- Esophageal angioma.
- Rendu-Osler disease.
- Injury to the esophagus from rough food or a foreign body.
- A tumor of the esophagus with its growth into the wall of the vessel with its damage.
- Iatrogenic damage, possible when examined with a rigid endoscope.
- Erosion and ulcers of the esophagus involving the vascular wall.
Recommendations for preparing food for patients
If the ulcer is complicated, then at first the sick person is allowed to take food only in liquid or puree form. It is blanched, steamed, baked or stewed.
As soon as the patient begins to feel significantly better, new ingredients are added to his diet and the amount of food is increased.
- steam cooking semolina porridge with plenty of water or milk and a small piece of cow butter, as well as egg dishes;
- a small piece of lean meat or fish;
- baked apple.
It is very important to correctly combine different products with each other. You cannot include in the patient’s diet anything that will make it difficult for him to digest.
Therefore, the menu should be compiled according to a principle that takes into account easy digestibility. You should know that liquid is retained in the gastrointestinal tract for ninety minutes, vegetables and bread for one hundred and eighty, and meat for three hundred.
Diagnosis of the disease
To make an accurate diagnosis, you must undergo the following examination:
- a general blood test establishes the fact of bleeding, which will show a decrease in hemoglobin and red blood cells;
- stool analysis will help determine hidden hemorrhage;
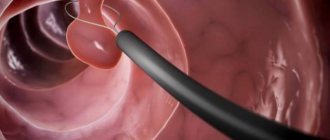
- FGDS is an accurate method that will not only help determine the location of bleeding, but also administer a hemostatic injection and stitch up the burst vessel;
- Ultrasound will not help accurately determine the location of the pathology, but will determine the condition of the internal organs;
- MRI, CT will determine the cause of hemorrhage;
- X-ray with the introduction of a dye will reveal the localization of the pathology.
To treat gastrointestinal diseases, people successfully use Galina Savinova’s method. Read more >>>
Approximate daily diet
Dietary meals during the day involve a certain menu option.
- In the morning, it is recommended to eat steamed fresh cottage cheese puree with the addition of one chopped banana. Wash it down with milk jelly.
- Late breakfast includes pear soufflé and rosehip infusion.
- For lunch they serve zucchini soup seasoned with rolled oats. For satiety, the patient is offered stale bread. The second course involves a steamed chicken cutlet with a side dish of potatoes boiled in milk. It is better to crush it first.
- Towards evening, carrot jelly or an apple baked in the oven are served.
- For dinner, it is better to eat an omelette cooked in a double boiler, a biscuit with a piece of mild cheese, and also drink weak tea with cream.
- At night, nutritionists advise taking a glass of milk with crackers.
Emergency help
If bleeding occurs, you must call an ambulance as soon as possible. It is important to reassure the patient and invite him to take a horizontal position, which will help control blood loss and limit its entry into the digestive tract.
You need to create comfort for the patient; remove excess clothing and cover him with a blanket. It is necessary to monitor the pulse and blood pressure, which should be checked every 10 minutes. Do not offer the patient anything to drink or eat. A decrease in blood pressure and an increase in heart rate indicate greater blood loss. A condition is considered dangerous when a decrease in blood pressure is recorded below 80 mm Hg, and the pulse rate is 130 beats per minute.
To prevent loss of consciousness, the patient can be sprayed with water or allowed to inhale ammonia. Ice helps, which the patient should take in small pieces. The patient must be transported on a stretcher, in a horizontal position, which allows him to limit his physical activity.
Diet for stomach ulcers
Peptic ulcer disease is a chronic disease in which, due to various disorders, an ulcer forms in the stomach or duodenum. The disease is cyclical, that is, there are periods of exacerbation and remission.
Diets for stomach ulcers
The diet is intended for patients with gastric and duodenal ulcers in the acute phase, acute gastritis, chronic gastritis with normal and increased secretion and chronic gastroduodeitis in the acute phase.
The diet for stomach ulcers contains a normal amount of fat (100 g), a reduced amount of carbohydrates (200 g), the lower limit of the physiological norm of protein (80 g), and a limited amount of table salt (8 g). Free liquid (tea, milk, rosehip decoction)—1.5-2 l. The daily ration weight is 2.5 kg, energy value is 2000-2200 kcal.
The diet is mechanically, chemically and thermally gentle. Food is given in liquid and semi-liquid form, mainly milk. Plant retina and extractive substances of meat, fish, vegetables, and mushrooms are excluded. The temperature of cold dishes is not lower than 15°C, hot food - not higher than 62°C. Patients should eat small meals, 6-7 times a day.
Recommended for consumption: porridge with water or milk, steam souffles and purees from lean meats and fish, milk, mucous and milk soups from cereals, except buckwheat and wheat, cream, freshly prepared unleavened cottage cheese with milk and sugar, steam omelette, steam curd pudding, soft-boiled egg, fruit and berry jelly, jellies, mousses, juices, homogenized vegetables, rosehip decoction, sugar, honey. Butter is added to the finished dish.
Contraindicated: raw and cooked vegetables, bread and baked goods, legumes, pasta, mushrooms, meat broth, fish and vegetable broth, alcoholic drinks, carbonated water, marinades, pickles, cocoa, chocolate.
Diet No. 1 b
Used after 8-10 days of using diet No. 1 a.
The diet contains a normal amount of proteins (100 g) and fats (100 g), a limited amount of carbohydrates (300 g) and table salt (8-10 g). Free liquid 1.5-2 l. The weight of the daily diet is 2.5-3 kg, the energy value of the diet is 2600-3000 kcal per day. The diet is mechanically and chemically less gentle than diet No. 1 a. Food is predominantly dairy, in puree and semi-liquid form, boiled in water or steamed. Vegetable fiber and extractive substances of meat, fish, vegetables, and mushrooms are excluded. The temperature of cold dishes is not lower than 15°C, hot food - not higher than 62°C. Patients should eat 6 times a day, in small portions.
Recommended for consumption: white bread crackers, thinly sliced and not browned. Soups based on a mucous decoction with the addition of pureed cereals and an egg-milk mixture. Cutlets, meatballs, dumplings, rolls, soufflé from lean meats (beef, veal), poultry (chicken, turkey) and fish (pike perch, cod, silver hake) steamed or boiled in water. Milk pureed porridges made from buckwheat, oatmeal, semolina and rice. Soft-boiled egg, steam omelette. From sweet fruits and berries - jelly, jellies, juices. Sugar, honey Milk, cream, freshly prepared cottage cheese with milk and sugar, steamed cottage cheese soufflé. Tea with milk or cream. Rosehip decoction with sugar. Butter is added to the finished dish.
Contraindicated: legumes, mushrooms, pasta and alcoholic drinks, strong tea, black coffee.
Diet No. 1
This diet is used in the attenuation phase of exacerbation of peptic ulcer disease and for acute gastritis during the recovery period.
The diet is physiologically complete with a normal content of proteins (100-120 g), fats (100-120 g) and carbohydrates (400-450 g). Table salt is within the lower limit of the physiological norm (8-10 g). Free liquid 1.5 l. The weight of the daily ration is 3 kg. The energy value of the diet is 3000-3500 kcal per day.
The diet is mechanically less gentle compared to diet No. 1 b. Chemical and thermal irritants and stimulants of gastric secretion are excluded. Food is given mainly pureed, boiled or steamed. Baked dishes without a rough crust are allowed in limited quantities. The temperature of cold dishes is not lower than 15°C, hot food is not higher than 62°C. Small meals 5-6 times a day.
Recommended for consumption: day-old or dried wheat bread, crackers, biscuits and dry cookies. Soups based on a slimy broth with the addition of pureed boiled vegetables, cereals, cream, and egg-milk mixture. Lean meats (beef, veal, rabbit) chopped, lean poultry (chicken, turkey) chopped or in pieces, lean fish (pike perch, cod, silver hake) in pieces, steamed or boiled in water. Boiled pureed vegetables (potatoes, zucchini, pumpkin, carrots, cauliflower, beets) in the form of purees and steam soufflés. In the absence of contraindications, 100 g of ripe raw tomatoes per day is allowed. Porridges from various cereals, except millet, in pureed form with the addition of milk or cream, mashed steamed puddings from cereals. Boiled vermicelli. In the absence of contraindications, a small amount of green pea puree. Soft-boiled eggs, steam omelettes. From sweet fruits and berries - jelly, jellies, mousses, pureed compotes, juices, jams, apples and pears baked with sugar. Whole milk, cream, fresh cottage cheese in the form of soufflés, casseroles, cheesecakes, sour cream 15 g per dish, fermented milk products 1-2 glasses per day if well tolerated. Dill and parsley, cinnamon, cloves. Milk sauce without frying flour with the addition of sour cream or butter, fruit juice, weak tea with milk or cream, rose hip decoction with sugar. In the absence of contraindications, olive and sunflower oil in dishes is useful.
Diagnostic procedures
The first thing that happens is collecting anamnesis, that is, interviewing and examining the patient. At a doctor’s appointment, the patient talks about complaints about his condition and previous illnesses. During an external examination, the result of tapping the patient is studied, the appearance of swelling, the condition of the mucous membranes, and skin color are analyzed.
Depending on the symptoms, the doctor determines the order of instrumental examinations
Diagnostic methods include the following studies:
- radiography;
- esophagoscopy;
- Ultrasound
Using a hardware method, changes in the shape of the esophageal mucosa, the causes of bleeding, and prediction of the next ruptures of blood vessels are determined.
The next stage is laboratory testing. The patient undergoes general and biochemical blood tests, and the liver is examined in detail as a possible source of esophageal bleeding.
Important! A correctly made diagnosis indicates the disease that is the cause of the disorders, with a mandatory listing of the identified complications.
After making an accurate diagnosis, the doctor determines a treatment method aimed at stopping bleeding, carrying out therapy and preventive actions regarding varicose veins of the esophagus, aimed at preventing such health problems in the future.
Bleeding due to a stomach ulcer: what to do?
Most people suffer from a disease such as stomach ulcers. It is impossible to cure it completely, but it is possible to alleviate the symptoms, which significantly complicate the life of any sick person.
A common occurrence is bleeding from a stomach ulcer, which causes fear in many. It is promoted by lesions in the walls of the stomach, injuries, as well as psychological stress.
Bleeding from a stomach ulcer. How to prevent it
Bleeding from a stomach ulcer does not always make itself felt. Many people do not even suspect that they have developed this disease. The main symptoms when it is felt are acute pain in the abdomen, nausea, vomiting, headache and tingling in the heart. Also, bleeding from a stomach ulcer is divided into two stages:
- Sudden – accompanied by acute pain and malaise, and in some cases even loss of consciousness;
- Permanent. With it, the ulcer can bleed every day without causing severe pain. This is due to overuse of medications.
Constant bleeding from a stomach ulcer causes chronic fatigue and drowsiness. Blood is gradually eliminated from the body along with feces, without changing its color.
In any case, at the first symptoms you should consult a doctor, because bleeding from a stomach ulcer with acute pain requires immediate hospitalization. It is impossible to stop him on your own!
Treatment and prevention of stomach ulcers
In order to stop the bleeding, doctors use a complex of hemostatic agents and if this fails, then it is stopped with the help of surgery. After this, the patient is prescribed bed rest for 10-14 days, during which certain procedures are prescribed. One of the standard ones is an enema. It is placed once a day. This is necessary in order to remove remaining blood from the stomach.
Bleeding from a stomach ulcer is a rather complex and dangerous complication. Therefore, the sooner you start treatment, the easier the consequences will be.
An important condition is to follow a diet that excludes the consumption of fatty and heavy foods, as well as foods that increase stomach acidity. Alcohol and carbonated drinks are not allowed.
A stomach ulcer at the initial stage does not pose a high danger if treatment is started on time!
Treatment
Therapy depends on the degree of bleeding and its cause. The directions of treatment are as follows:
- Stop bleeding.
- Replenishment of lost fluid and blood components.
- Preventing relapses.
- Treatment of the root cause of changes in the esophagus.
- Symptomatic treatment.
The difficulty of stopping bleeding is explained by the deep location of the esophagus in the chest and the inability to quickly access it.
Do not apply pressure to the bleeding site or apply a tourniquet. In order to detect a bleeding area, it takes time, which can be catastrophically short in case of acute blood loss, and the availability of special equipment.
A patient with esophageal bleeding requires urgent hospitalization
The following methods are available to stop bleeding:
- Use of hemostatic drugs. This is effective for very minor bleeding.
- Blackmore probe. Its peculiarity is the presence of a cuff, which is inflated when the probe is inserted into the stomach. The cuff is located at the level of the esophagus. Swelling, it presses tightly against its walls, stopping the bleeding.
- Endoscopic electrocoagulation. Rarely used for minor bleeding.
- Ligation, clipping of vessels. Performed endoscopically. Unfortunately, the thin tissue of the esophagus above the bleeding varicose veins is thinned and often inflamed. When applying sutures and clips, it can be damaged by them. There remains a high risk of recurrent bleeding.
- Sclerosis of veins using special substances.
- Transjugular intrahepatic portosystemic shunt (TIP S). In this case, a stent is inserted to connect the large hepatic veins with the branches of the portal vein.
- Devascularizing surgical operations.
- For Malory-Weiss syndrome, if conservative therapy and endoscopic intervention are ineffective, the Bayeux operation is performed.
Replacement therapy with blood components is carried out. For the treatment of coagulopathies, fresh frozen plasma and platelet concentrate are used. With the development of hemorrhagic shock, drug support is provided for the vital functions of cardiac activity and respiration.