Treatment of erosive processes in the stomach and duodenum consists not only of medications, but also involves strict correction of the diet. The main goal of proper nutrition is not to irritate the mucous membranes of injured organs, but to support and restore them. Diet for gastric and duodenal ulcers is an integral part of successful treatment of the disease and prevention of further relapses.
The goal of a diet for ulcers is not to irritate the walls of diseased organs
List of foods that stimulate the production of hydrochloric acid in the stomach
- strong tea or coffee;
- fatty and rich broths;
- soups with meat, fish, mushrooms;
- fried foods (including vegetables);
- alcoholic drinks;
- sweet carbonated drinks;
- canned meat and fish;
- black bread;
- pies and pastries made from butter dough;
- seasonings and spices (especially pepper, cloves, mustard, horseradish).
Prohibited foods and dishes
There is a fairly impressive list of foods that need to be excluded from the diet of an ulcer. These include:
- smoked meats and marinades;
- strong broths, vegetable decoctions;
- hot spices;
- sour vegetables (sorrel, cabbage, mushrooms, spinach, fresh onions, garlic, soybeans), fruits;
- fried, dried, salted;
- fatty meat, fish;
- semi-finished products;
- hot, spicy cheese;
- rye, fresh, hot bread;
- dark chocolate, puff pastry cakes with rich cream, baked goods;
- carbonated drinks, kvass, strong tea, coffee, alcohol.
You should also limit your salt intake.
Therapeutic diet No. 1 for duodenal ulcer. Menu for the week
Therapeutic diet No. 1 or Table 1 is prescribed to patients suffering from duodenal and gastric ulcers, during exacerbations of chronic gastritis. Create a balanced menu, and remember that even dietary dishes can be very tasty if prepared correctly.
Print the menu “Diets for peptic ulcer disease” on the refrigerator
We present to your attention a sample menu of a therapeutic diet for duodenal ulcers for a week.
1
The first day:
- Breakfast: pureed oatmeal with milk and banana, weak black tea with honey;
- Second breakfast: fruit jelly;
- Lunch: vegetable cream soup, steamed beef souffle, crackers, juice diluted with water;
- Afternoon snack: 1 glass of rose hip decoction, marmalade;
- Dinner: mashed potatoes, steamed fish cutlet, green tea.
2
Second day:
- Breakfast: steam omelette of two eggs, tea without sugar;
- Second breakfast: low-fat cottage cheese;
- Lunch: meat cream soup, vegetable puree, fruit jelly;
- Afternoon snack: baby applesauce;
- Dinner: semolina porridge with milk, rosehip decoction.
3
Day three:
- Breakfast: noodles with milk and honey, weak tea;
- Second breakfast: cocoa, marshmallows;
- Lunch: slimy rice soup, steamed meatballs, dried fruit compote;
- Afternoon snack: baked apples;
- Dinner: mashed potatoes, fish soufflé, kefir.
4
Day four:
- Breakfast: soft-boiled egg, applesauce, herbal tea;
- Second breakfast: banana;
- Lunch: boiled turkey, mashed with mashed potatoes, peach juice diluted with water;
- Afternoon snack: crackers, glass of low-fat kefir;
- Dinner: vermicelli with grated mild low-fat cheese (can be processed), steamed cutlets, fruit jelly.
5
Day five:
- Breakfast: steam omelette, tea with milk;
- Second breakfast: rosehip decoction, marshmallows;
- Lunch: mashed potato soup, boiled (well boiled) lean fish, jelly;
- Afternoon snack: apple and carrot baby puree;
- Dinner: mashed potatoes, steamed zrazy, kefir.
6
Day six:
- Breakfast: low-fat cottage cheese with low-fat sour cream and honey, soft-boiled egg, compote;
- Second breakfast: “bird's milk”;
- Lunch: pureed soup with vegetables and noodles, steamed cutlets, rosehip broth;
- Afternoon snack: banana;
- Dinner: pureed rice milk porridge with a piece of butter, dried bread, marmalade, rosehip infusion.
7
Day seven:
- Breakfast: milk oatmeal, steamed meatballs, tea;
- Second breakfast: classic yogurt;
- Lunch: cream soup, noodle soup with meat, berry jelly;
- Afternoon snack: kefir, dry cookies;
- Dinner: semolina porridge with milk, a glass of herbal tea.
Every evening before going to bed, you can drink rosehip decoction, green tea, kefir with 1% fat content, yogurt .
Basics of therapeutic nutrition
Problems solved by diet therapy:
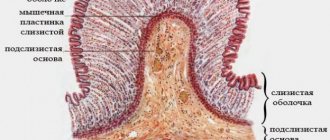
- regulation of the stomach;
- increased protection of the mucous membrane;
- neutralization of acidic stomach juices;
- reduction in ulcer healing time.
Proper nutrition can replace treatment for many diseases. Knowing and following its basic rules, you can create a tasty and healthy menu for stomach ulcers.
Medical nutrition consists of products that are easily excreted from the body and do not irritate the gastric mucosa.
The basis of the menu for stomach ulcers consists of boiled and pureed foods
Features of the diet for acute ulcers
First of all, you need to remove the irritating effects of hydrochloric acid in the stomach. To do this, you should remove foods that have this effect from your diet:
- Spices;
- Various spices;
- Any fried food;
- Strong meat broths;
- Rough food;
- Raw coarsely chopped vegetables;
- Berries with small seeds.
Avoid alcohol and carbonated sweet drinks.
Boiled food is best; using a slow cooker is acceptable.
Do not overeat, eat little by little, but often, preferably 6-7 times a day - this is the basic principle of proper nutrition.
Do not eat cold or highly heated food.
Permitted and prohibited products
Knowing which foods are allowed and which are prohibited for stomach ulcers, you can make the right choice of diet for every day.
| Products | Allowed | Forbidden |
| Soups | Uncooked meats, cereals, vegetables; dairy and fruit | Rich meat, fish, mushroom broths |
| Flour products | White bread (yesterday's baking), gray bread with bran, products made from soft dough, pasta in limited quantities. | Confectionery with cream, pastry products |
| Cereals | Porridges made from oatmeal, semolina, buckwheat and rice cereals | Porridges and legume dishes (peas, beans), millet porridge |
| Dairy | Low-fat milk, cottage cheese, kefir, yogurt, cheeses, sour cream, butter | High-fat dairy products, cream, sharp cheeses |
| Eggs | Soft-boiled and in the form of steam omelettes | Fried eggs |
| Meat and meat products | Low-fat veal, lamb, chicken, turkey, boiled or baked rabbit, steamed cutlets, soufflé, meatballs | Fried and fatty meats and poultry, offal (liver, tongue, etc.), smoked meats, canned food, lard |
| Fish | River and sea fish, baked (without crust) or boiled, soaked salted fish | Canned fish, fried and highly salted fish |
| Fresh vegetables (preferably boiled or baked) | Mashed potatoes, cucumbers, beets, carrots, tomatoes, sweet peppers, eggplants, cauliflower, vegetable juices | Green and onions, garlic, radishes, radishes, sorrel, spinach, mushrooms, pickled vegetables. In case of pain, limit the permitted list as much as possible |
| Fruits and berries | Apples, pears, bananas, peaches, apricots, melons, watermelon, sweet berries | All sour fruits and berries (except lemon) |
| Sweets | Honey, jam | Ice cream, chocolate |
| Beverages | Compotes, jelly, fruit and vegetable juices, weak tea with lemon, rosehip decoction | Cold and carbonated drinks, concentrated juices, coffee, strong tea, alcoholic drinks |
Therapeutic diet recipes No. 1
Slimy rice soup
Suitable for anyone who has problems with the stomach and duodenum. This soup coats the walls of the stomach well and saturates the patient. To prepare we will need:
- rice;
- milk;
- egg;
- boiled carrots;
- some greenery;
- a piece of butter.
Boil the rice in water until tender, then strain it through a fine sieve. Add a few tablespoons of rice to the rice water and bring to a boil over low heat. Mix the egg with milk, as for an omelette, and pour the milk-egg mixture into the rice water. After a few minutes, remove from heat. If desired, you can add finely chopped boiled carrots, some herbs and a piece of butter.
Lapshevnik with meat or cottage cheese
For this diet, you can prepare noodle soup with minced meat or fish , as well as low-fat cottage cheese . For the recipe you will need the following products:
- noodles or vermicelli;
- minced meat or cottage cheese;
- eggs;
- salt;
- a little sour cream.
Break the noodles into small pieces and cook until tender (there should be some liquid left in the pan with the pasta). Add minced meat or cottage cheese, a few eggs to the pasta, mix thoroughly. Grease a baking sheet with a small amount of vegetable oil. Spread the noodle soup in a thin layer, spread sour cream on top, and bake until done for 20-40 minutes, depending on the filling. Then cut the finished noodle maker into portioned pieces, and before serving, place a piece of butter on each portion.
Zrazy for a couple
To prepare the recipe you will need:
- ground beef or chicken;
- a little salt;
- egg;
- quail eggs according to the number of times.
Boil quail eggs until tender, cool and peel. Add a little salt and a raw chicken egg to the minced meat. You can also add some chopped herbs. Form zrazy, place a quail egg inside each cutlet. Steam zrazy in a double boiler, in a slow cooker, in a water bath or in the oven.
Beef or fish soufflé
Beef souffle is suitable both for patients with diseases of the gastrointestinal tract and for children's menus . Ingredients:
- beef;
- flour;
- milk;
- butter;
- chicken eggs;
- salt.
Rinse the beef well and boil until tender, then pass through a meat grinder several times. Immerse raw meat in boiling water to retain more vitamins and nutrients. In a dry frying pan, fry the flour until golden brown, then add butter to the flour and thoroughly stir the flour with the melted butter. Pour a little milk into the pan and simmer, stirring thoroughly, until thickened. Add the egg yolk, beaten egg white, milk sauce and salt to taste to the ground beef. Mix everything well and place on a greased baking sheet. Bake the souffle steamed or in the oven. Fish soufflé is prepared using the same principle, but instead of beef, use lean fish fillet.
Myths about duodenal ulcers:
Authorized products
A list of dishes and products allowed for diet number 1 is provided. The list of products is extensive, the patient’s food will not seem limited and boring.
- Bread baked from wheat flour, in case of exacerbation of peptic ulcer disease, is better to use yesterday's bread.
- It is permissible to consume baked goods in small quantities, without using yeast dough. Pies with fish, apples, and cottage cheese are allowed, which soothes the intestines and stomach ulceration.
- Biscuits, unsweetened cookies and crackers are served with tea in the diet for stomach ulcers. Food should not be too sweet.
- Soups with meat broth must take into account the main requirement - to cook in secondary broth. For meat, choose beef or chicken, removing the veins.
- Milk soups with pasta and cereals.
- The second dish for the treatment of stomach ulcers is prepared using lean boiled meat. It is allowed to use rabbit, chicken, turkey, and beef. Dishes include meatballs, meatballs, boiled meat in pieces, and zraza. The products are steamed so as not to irritate the ulcerative defect with aggressive substances and not to provoke malignancy.
- Low-fat fish varieties.
- Low-fat dairy products, fermented baked milk or yogurt, low-fat milk can be consumed in the subacute stage.
- Eggs in the diet for patients with stomach ulcers are present in the form of an omelet or soft-boiled.
- Choose berries and fruits that are sweet and pre-peeled. Baked apples or pears are allowed.
- The table for stomach ulcers allows for dessert marmalade, honey, marshmallows, jams, marshmallows, and non-sour jam.
- For drinks, drink rosehip infusion, teas, compotes or cocoa, not strongly brewed. First dilute the juices with water. It is allowed to drink juice made from fruits or berries, diluted with boiled water.
Recipes for dietary table No. 1 A
Rice porridge is prepared from crushed cereals. After cooking, add milk, cream, 20 grams of butter. In another cooking option, the cereal is first boiled, then ground or homogenized in a blender with the addition of milk and cream.
Milk decoction of rolled oatmeal. Bring the cereal to a thick state in boiling water. Filter the resulting mixture from large pieces, boil with milk for 10-15 minutes until a thick mucus-like consistency, add butter.
Grind oatmeal in a coffee grinder, cook over moderate heat until half cooked, add milk or cream for a liquid consistency, season with a spoonful of butter and stir until cooked.
Chicken eggs are allowed soft-boiled (boiling for 3 minutes). You cannot fry the omelet, only in a water bath.
Meat dishes of a soft, permitted consistency are prepared from the recommended types of meat, after boiling them until soft. The finished meat is ground in a food processor, meat grinder or blender. Dilute the resulting mixture to a liquid puree with cream, water, add 7 grams of butter, a pinch of salt.
Apple jelly helps alleviate inflammatory processes on the intestinal walls and accelerates the healing of damaged mucosa. To prepare for 1 liter of water, take two large sweet apples, a teaspoon of honey, 1 tablespoon of potato starch. The fruits are peeled and grated. Simmer the applesauce with honey for five minutes, add water and cook for 20 minutes. At the end of the process, remove the drink from the heat and add starch, stirring continuously until thickened.
Nutrition for gastric and duodenal ulcers during exacerbation and remission
Gastric and duodenal ulcers are a serious disease that requires a competent approach not only to treatment, but also to nutritional management. Persons suffering from peptic ulcer disease should adhere to a special gentle diet No. 1. The diet is especially important during an exacerbation period, when the load on the digestive organs should be minimal.
General principles of dietary nutrition
When organizing therapeutic nutrition, it is important to follow the principles of diet. Thanks to a balanced diet, you can significantly alleviate the course of the disease and speed up the process of entering stable remission.
The diet for patients with gastric and duodenal ulcers No. 1 is divided into table No. 1A (with severe exacerbation) and table No. 1B (as the patient’s condition improves). Diet 1B is prescribed after completion of a course of treatment using diet 1A.
General principles of the diet:
- balance and adequate calorie content - patients with ulcers should not be fed low-calorie, monotonous food; food must be nutritious (at least 2500-3000 kcal per day), contain a sufficient amount of vitamins, protein, carbohydrates, fats;
- fractional nutrition means eating food in small portions, the interval between them is at least 3 hours;
- correct temperature regime - cold or hot food is strictly prohibited, especially during exacerbation of gastric ulcer, when the mucous membrane is inflamed;
- restriction in salt consumption, up to complete refusal;
- a complete ban on fried, fatty, smoked foods, alcohol and carbonated drinks;
- avoidance of foods that can cause fermentation and increased gas formation;
- compliance with the drinking regime - it is recommended to drink up to 2 liters of clean water per day (if there are no problems with the kidneys and thyroid gland);
- mechanical and chemical sparing - products must be selected carefully to avoid irritating effects on the sore stomach;
- zigzag nutrition involves training the gastrointestinal tract and is used during remission; the essence of the principle is the short-term introduction of forbidden food into the patient’s diet (in small volumes), followed by a return to dietary nutrition;
- taking into account the time required to digest food is extremely important - adherence to the principle will allow food to be better absorbed without undue stress on the stomach.
Nutrition for patients with gastric and duodenal ulcers should be selected individually, taking into account weight and age, general condition, and taste preferences. Classic cooking options - boiling, stewing, steaming (multi-cooker, double boiler). Dietary nutrition is important to follow not only during an exacerbation, but also during remission.
Features of the diet during exacerbation of the disease
Diet for exacerbation of gastric and duodenal ulcers is an integral part of complex therapy. The ulcer worsens for various reasons - dietary errors, bad habits, stress and nervous shock - as a result, inflammation of the gastrointestinal mucosa occurs, pain develops, and the general condition worsens.
Compliance with diet No. 1A is aimed at maximally sparing the stomach and duodenum in terms of thermal, chemical, and mechanical effects. The diet helps smooth out the reflex excitability of the stomach and accelerate the scarring of ulcerative defects.
Diet No. 1A during the period of exacerbation of the disease is based on compliance with the rules:
- calorie restriction, but not less than 2200 kcal per day;
- limiting salt intake to 6 g per day;
- the consistency of the food is only liquid, puree, thoroughly pureed;
- food serving temperature - no more than 55°, no less than 15°.
The diet during an exacerbation of the disease is based on the consumption of mucous soups (ground), steam soufflés and omelettes, boiled eggs, jelly, steamed cottage cheese casseroles. Drinks allowed include sweet juices half diluted with water, weak tea, and infusion of rose hips.
Diet during remission
After achieving stable remission, the diet is significantly expanded. You can eat more high-calorie foods, including baked goods and sweets.
During the period of remission, which lasts more than a year, nutrition gradually approaches the standard diet of a healthy person.
But a number of restrictions must be observed:
- there should be at least 4 meals per day;
- overeating is unacceptable;
- limitation in the daily dose of salt to 10 g;
- alcohol, spicy and spicy foods, coffee are prohibited.
In remission with a duodenal ulcer, you can eat ripe bananas, strawberries, sour apples, and cherries. Drinks allowed include a variety of fruit and vegetable juices (with the exception of citrus fruits), compotes, jelly, and tea. The total volume of liquid (not counting first courses) should be at least 1.5 liters.
Authorized Products
Many people are interested in the question: what is allowed to eat if you have duodenal and stomach ulcers? The list of products allowed for consumption for such an illness is extensive; the patient will not go hungry.
- Bread is allowed, but only wheat and not freshly baked. In case of exacerbation, it is better to dry the bread in the oven and eat it in the form of crackers.
- Dairy dishes (porridge, soups) can be eaten during an exacerbation and in remission. Such food is nutritious, contains a lot of protein, envelops the stomach, reducing the secretion of gastric juice.
- Broths. Useful for exacerbations, the main thing is that the broth should be secondary, and it can be prepared from chicken, turkey, beef. It is allowed to cook soups (vegetable, cereal, with noodles) based on broths.
- Dairy and fermented milk products in the form of regular milk, fermented baked milk, low-fat sour cream and cream, cottage cheese and yoghurts (without dyes and E-additives), unleavened cheese (only during remission) are tasty, nutritious, and have a gentle effect on the gastrointestinal tract.
- Turkey, chicken, rabbit, beef are ideal for preparing main courses. There are many options - meatballs, cutlets, quenelles, zrazy, meatballs, soufflés and casseroles. The main thing is to steam them only.
- Lean and boneless fish, such as pike perch, is suitable. It is better to give preference to food made from minced fish, cooked in a double boiler or baked in foil.
- Eggs are allowed at any stage of the disease. The ideal cooking option is soft-boiled or steamed omelet.
- Cereals in the form of rice, buckwheat, oatmeal, and semolina are used to prepare porridges, soups, and side dishes. The main thing is to boil or wipe them well.
- Sweet fruits - bananas, soft pears and non-acidic apples - diversify the diet. In case of exacerbation, pears and apples should be peeled and baked.
- Sweets in the form of marshmallows, jam, marshmallows, fruit marmalade, jelly and mousses made from milk and fruits (berries) are allowed after the exacerbation has recovered (on 7-8 days).
- Oils are essential in nutrition. It is allowed to add olive, sunflower and butter to food.
- Drinks in the form of rosehip decoction or wheat bran, directly pressed juices (diluted with water by 50%), non-concentrated compotes, weak tea are tasty and healthy, quench thirst well without having a harsh effect on the stomach.
Source: https://zdorov-doma.ru/pitanie/dieta-pri-yazve-zheludka.html
Therapeutic diet therapy
In combination with medications, the patient is advised not to neglect the nutritional instructions of nutritionists and gastroenterologists, so that the inflammation subsides faster and the epithelium scars more intensively.
Diet order:
- Table No. 1 A. Low-calorie diet lasting from 7 to 14 days, depending on the severity of the disease. The effect on the digestive organs is limited as much as possible.
- Table No. 1 B. Medium calorie diet lasting from 10 to 30 days. Prescribed after the symptoms of the acute period have subsided.
- Table No. 1. A diet that meets the body’s nutritional needs. They last from 2 months to six months.
List of Accepted Products
There are many products that can be used for cooking. A variety of healthy dishes are prepared from them, however, you will have to limit the consumption of spices and salt and properly heat treat them (boil, bake, steam).
Here is a partial list of products that can be used:
- beef, veal, poultry, rabbit, lean fish;
- rice, rolled oats, semolina, boiled buckwheat;
- pasta, whole pasta should be chopped;
- eggs, 1–2 per day;
- milk, cream, yogurts, curdled milk, fresh kefir, cottage cheese, feta cheese;
- yesterday's white bread or crackers;
- non-sour berries, pureed or baked fruits, bananas;
- potatoes, carrots, beets, tomatoes in small quantities;
- good quality butter and ghee in small quantities;
- refined vegetable oils (olive, sunflower, corn) for cooking;
- honey, jam, jam, marmalade, marshmallows.
Prohibited foods may also become acceptable in rare cases and in very small quantities. For example, a holiday salad “herring under a fur coat” for a patient can be prepared by soaking it in water to reduce the content of salt and spices. Season the salad with low-fat sour cream sauce. But this can be done occasionally and only during a period of stable remission.
Nutrition is the key to a speedy recovery
When treating ulcers, the main goal is to relieve inflammation and restore the normal functioning of the damaged organ. Therefore, the diet for gastric and duodenal ulcers during the treatment period is aimed at lowering acid levels and normalizing the production of enzymes.
In addition, the regeneration of protective tissues and strengthening of weakened immunity depends on the amount of mineral elements and vitamins received by the body.
A special place in diets is occupied by products that help eliminate pain and physiological manifestations of pathology that are directly involved in the treatment of the disease:
- Buckwheat (buckwheat flour) – heals ulcers, is a source of iron, contains B vitamins, strengthens blood vessels and mucous membranes.
- Honey – neutralizes acids, relieves pain, relieves inflammation, increases hemoglobin levels, strengthens the immune system.
- Sea buckthorn (oil) – regulates and normalizes metabolism, is an excellent analgesic and healing agent, contains vitamins and omega acids involved in cell restoration.
- Walnuts (tincture) – walnut kernels contain lycine, which facilitates the absorption of proteins, as well as a large amount of vitamins and minerals that accelerate healing and recovery.
- Potatoes (decoction) – reduces acidity, acts as an anti-inflammatory agent, helps get rid of nausea, vomiting, heartburn.
- Cabbage (juice) - the substances included in its composition are involved in the restoration of mucous tissues and strengthen the immune system.
All ingredients used are baked, boiled, stewed. Many products are consumed in minimal quantities, and fruits and vegetables are pre-heat-treated.
Attention! One of the folk ways to combat the disease is a decoction of the peel of green walnuts. Traditional healers advise drinking one glass of this “medicine” on an empty stomach for two weeks.
Nutrition for a bleeding ulcer
For ulcer bleeding, a specialized diet is used. If indicated, the patient may receive parenteral nutrition until bleeding stops. After its cancellation, you are allowed to take 200 ml of liquid cold food per day. This can be milk, jelly, jelly, cream, after a while they add sour cream and raw eggs, slimy soups. As a result, the patient is transferred to Table No. 1A with expansion to the Table No. 1 option.
To combat anemia, a diet with a high protein content (140-150 g) is prescribed, while fats are somewhat limited (60-70 g). It is necessary to enrich the diet with iron, cobalt, copper, manganese, cyanocobalamin, so it is advisable to introduce dishes with liver and yeast. If you are feeling satisfactorily, after 1.5 months, unchopped food with the addition of fresh vegetables and fruits is allowed. Plums, apples and peaches can also be eaten ungrated.
What to consider when creating a menu
Following a diet for erosion of the stomach and duodenum involves following certain rules. Violating them will have unpleasant consequences.
- The menu should be varied and contain microelements and vitamins necessary for the normal functioning of the body.
- You need to consume at least 3000 calories per day. Preference is given to food that is easily digestible, but at the same time satisfying and nutritious.
- The list of permitted products includes cereals. A gastroenterologist will advise you on what cereals you can eat. Usually this is rice, oatmeal and semolina.
- Fruits are not recommended to be consumed fresh; it is better to bake or boil them. Before eating, the product is peeled and grated.
- Patients with peptic ulcer disease can include canned food for children in their diet.
- Dairy products include cottage cheese, fresh milk, and a small amount of cream.
- Soups for ulcers should have the consistency of puree.
- Chicken eggs are allowed and served in a semi-liquid state - soft-boiled.
- When choosing between sugar and honey, it is better to give preference to the latter option. The bee product heals ulcers.
- Those with a sweet tooth are allowed to include healthy desserts with pectin in their diet - marmalade, marshmallows and marshmallows.
- The juice can be natural, unpackaged. It is better to dilute it with water.
- The rapid healing of ulcers or erosion is facilitated by the use of a decoction of wheat bran or rose hips.
Basic principles
Experts make the following dietary requirements:
- high nutritional value of the diet;
- a balanced diet, which should include proteins, fats, carbohydrates, vitamins, minerals;
- products should not irritate the gastrointestinal mucosa;
- eating food at room temperature;
- avoidance of foods that increase the secretion of gastric juice;
- fractional meals in small portions;
- eating mashed pureed food;
- limiting table salt.
The most useful products
There are several products that can have a beneficial effect on the mucous membrane of the stomach and duodenum in the presence of ulcers. This is low-fat pasteurized milk, honey and cabbage juice. The products gently envelop the stomach, reducing the aggressive influence of digestive juices, promote the healing of ulcers, and have a detrimental effect on Helicobacter pylori.
- Milk must be included in the diet of people suffering from peptic ulcer. Regular consumption of milk helps ulcerative defects in the mucous membrane to heal faster and relieves attacks of pain.
- Honey is no less useful. It should be eaten in small quantities, but daily. Honey is able to protect the walls of the stomach from increased secretion of hydrochloric acid, relieve acute inflammation, and relieve dyspeptic symptoms such as belching, heartburn, a feeling of heaviness and nausea.
- Cabbage juice has a healing effect, helping to heal ulcers. This ability is due to the presence of a high content of vitamin U in freshly squeezed juice.
Diet for stomach ulcers at home: what to eat?
A stomach ulcer is a disease of part of the digestive system. Therefore, nutrition plays a huge role in this disease. The nutritional system for stomach ulcers is the key to successful treatment. You will learn about which products are allowed and prohibited for this disease in the article.
Features of the diet in the acute phase
Recommended foods for stomach ulcers
During the period of severe pain and the acute phase of the disease, including in the presence of complications, frequent split meals are necessary with the complete exclusion of any food that will, at least slightly, irritate the digestive tract. There should not be a long period of fasting during an ulcer - the feeling of hunger in combination with the natural production of hydrochloric acid negatively affects the walls of the stomach.
The following diet for one to two weeks during exacerbation of the pathology will be considered optimal:
- eating 6-7 times a day;
- portions are small;
- complete exclusion of any fried, smoked, pickled, sweet, fatty foods;
- food is served in crushed (puree) or liquid form, at moderate temperature.
Therapeutic nutrition for peptic ulcer disease
If the patient does not eat enough of the portion, its volume should not be increased. It is considered acceptable to increase the number of meals up to 7-8 times.
Recommended menu for acute illness
| Eating | Dishes |
| Breakfast | A couple of soft-boiled eggs / omelet / any milk porridge (semolina, pearl barley, rice, vermicelli). Lightly brewed green leaf tea. Cottage cheese. 1 teaspoon honey |
| Lunch | Fruit puree with a little milk (banana, peach, apricot) |
| Dinner | Vegetable or potato puree soup with croutons. Boiled chicken or fish fillet / steam cutlets. Garnish with rice or mashed potatoes. Salad of boiled vegetables (carrots and beets). Compote |
| Afternoon snack | Cottage cheese casserole with raisins, strawberries / Baked apple or pear with honey. Chamomile or rosehip decoction |
| Dinner | Boneless chicken fillet or dietary fish / soup / cottage cheese casserole |
| Snack before bed | A glass of warm milk with honey or kefir |
Useful and harmful foods for stomach ulcers
Following this kind of diet after 7-8 days leads to a significant improvement in a person’s well-being - pain in the epigastric region is eliminated, heartburn and nausea are less bothersome, and appetite improves. At this time, it is necessary to adjust the dosage and combination of medications and update the menu.
Products that have a healing effect
There are three products available that have a healing effect.
- Fresh potato juice. A simple superfood that can be used for healing. It has regenerating, wound-healing, analgesic, and anti-inflammatory effects. Potato juice also destroys pathogenic flora that is present in the stomach. Prepare juice from fresh, high-quality potatoes and drink immediately. Take outside the period of exacerbation, half an hour before meals, for 3 weeks in a row. Volume: start with a few spoons, increase to 150 ml per day. It is better to take it diluted with water, 1:1.
- Low fat milk. Envelops the walls of the stomach, protects the organ from the aggressive effects of foods and gastric juice, accelerates the regeneration process, dulls or even relieves pain.
- Honey. You can eat honey in small quantities every day: the product is rich in microelements, vitamins, and has a beneficial effect on the entire gastrointestinal tract. As for the ulcerative process, honey helps relieve inflammation, reduces secretion, neutralizes the effect of hydrochloric acid, and relieves pain. Honey reduces nausea and heartburn inherent in the disease, and increases the level of hemoglobin in the blood.
- Fresh cabbage juice. Contains a stable form of ascorbic acid and anti-ulcer vitamin U. The juice has been proven to be effective in accelerating wound scarring and against Helicobacter pylory.
They can be included in the list of dishes, the only caveat is about cabbage juice: you can drink it freshly prepared, diluted with water (1:1), no more than 100 ml at a time, 2-3 times a day. The most important thing is only during the period of remission!
Diet rules
To scar an ulcer, you need a large amount of nutrients and vitamins, this is especially important when bleeding, so fasting is contraindicated. Only in case of a bleeding ulcer and after surgery, you should abstain and not eat for the first two days until the attending physician allows it. Then you need to eat regularly, often, and the caloric content of the daily menu should be 2800–3000 calories.
When creating a menu for a stomach ulcer for one day or a week, consider not only the quantity and calorie content of foods, but also the ratio of proteins, fats, and carbohydrates. Food should be mostly protein with a minimum content of fat and fiber. In the acute period, it is recommended to reduce the proportion of carbohydrates, as they stimulate gastric motility and can cause pain.
To replenish the body's need for vitamins and microelements, fresh juices of vegetables and fruits will be useful. For example, cabbage, even boiled, is contraindicated for patients with ulcers, but fresh cabbage juice is useful because it contains vitamins C and U. A patient with an ulcer needs to drink milk every day or include it in the menu in the form of porridges and milk soups. Don’t forget about bee products (honey, propolis) that help improve immunity and heal the mucous membrane.
Option 2 – when symptoms subside
What to eat if you have a stomach ulcer during remission? The following daily menu is suitable for this:
- Breakfast: steamed omelette, rice porridge, fruit puree, rosehip drink.
- Second breakfast: fruit jelly.
- Lunch: milk oatmeal soup, meatballs, berry jelly.
- Afternoon snack: crackers, apple drink.
- Dinner: fish balls, buckwheat porridge, jelly.
- Before bed: 1 glass of milk.
This diet is suitable for those patients who have pain, nausea, vomiting, and heartburn. The menu can be prescribed to people on bed rest.
Main principles
The causative agent of gastrointestinal ulcers and perforation of ulcers is a spiral-shaped bacterium called Helicobacter pylori. It affects the mucous membranes of the stomach. The pathological process is accompanied by:
- pain in the lower abdomen;
- frequent belching;
- nausea;
- heartburn.
Lack of or delayed treatment will lead to complications that are dangerous to humans. During therapy, it is recommended to adhere to a special diet. The patient's diet should contain only those foods that stimulate the secretion of juice in the stomach. Dishes from the menu help protect the mucous membranes of the gastrointestinal tract from mechanical or thermal damage. Patients are advised to eat food at room temperature, always in processed form.
The diets used for exacerbations of gastric and duodenal ulcers are dominated by:
- milk products;
- porridge;
- vegetable soups;
- chicken or turkey that has undergone culinary processing - boiled or steamed.
It will take at least 10-12 days to stick to this diet. The menu is based on the following principles:
- Nutrition for ulcerative pathologies is fractional, in small portions. A day from 4 to 5 times.
- When preparing a diet, preference is given to low-calorie dishes.
- Products are boiled or steamed. Afterwards, the food is crushed or passed through a blender or meat grinder.
- The consistency of the dishes should resemble liquid porridge or soup.
- Preference is given to food at room temperature.
- Consumption of salt and spices is limited as much as possible.
Rules for eating
If you want to get rid of the unpleasant symptoms that have arisen due to a stomach or duodenal ulcer as quickly as possible, you need to strictly monitor your diet. To maximize the period of remission, a diet for gastrointestinal diseases should last at least six months.
Let us highlight the main criteria that must be observed for ulcers of the duodenal bulb, stomach or rectum:
- It is highly undesirable to eat at night. The last meal should be taken at least 3.5 hours before bedtime. If we are talking about liquids (kefir, jelly, compote) - 2 hours.
- The diet for ulcers of the esophagus, duodenum or stomach is as gentle as possible. In order not to irritate the inflamed surface, you need to completely avoid spicy foods, excessively salty dishes, marinades, etc.
- In case of intestinal dysfunction, food should have an exclusively liquid consistency.
- Some foods provoke the production of gastric juice. For example, fruits. For this reason, ulcer sufferers, especially during exacerbation of the disease, are advised to consume fruit only after heat treatment.
- You need to eat at regular intervals. Experts call 3.5 hours the ideal option.
The same principles must be followed after medical intervention, for example, after surgery for a duodenal or gastric ulcer.
The diet rules are based on standard ones. However, each person is unique, therefore, depending on the characteristics of the body, as well as the course of the disease, the principles of the menu may be different. A gastroenterologist will tell you in detail about individual proper nutrition.
Things to take care of
Additional conditions for a gentle diet for the successful treatment of stomach ulcers or gastritis:
- It is advisable to prepare meals at home; you need to give up ready-made food that is sold in stores.
- People who suffer from gastric ulcers (GUP) or duodenal ulcers need to use a double boiler or multicooker for cooking. This is how most beneficial microelements are preserved in products.
- The temperature of the dish should be equal to body temperature. This will help avoid injury to the surface of the stomach.
- Products in the diet for ulcers should not cause bloating and gas formation.
- It is necessary to continue to adhere to the diet after an ulcer.
Compliance with the treatment table is 70% of success in the treatment of gastrointestinal diseases.
Basic rules when choosing a diet
Before finding out what you can eat if you have a peptic ulcer and what you can’t, you should familiarize yourself with the principles of building a healthy diet. In fact, there are not so many rules, and knowing them by heart, everyone can easily create a menu for the week without resorting to the help of medical reference books. So, what everyone who suffers from this disease needs to know about diet:
- Food consumed should not have a mechanical or chemical effect on the mucous membrane;
- When creating a diet for ulcer patients, it is necessary to give preference to foods with high energy value. The menu for peptic ulcers should include foods containing large amounts of minerals and vitamins. The ratio of carbohydrates to proteins and fats should be in the proportion of 4/1/1;
- It is necessary to completely exclude foods that strongly stimulate the secretion of gastric juice;
- For gastric ulcers, meals should be taken as often as possible, with a minimum frequency of once every three hours;
- Special dietary dishes, regardless of their composition and method of preparation, must be thoroughly boiled and processed so as not to have a mechanical effect on the mucous membrane;
- Try to drink more liquid - the minimum volume per day should be 1.5 liters;
- A special feature of the diet for stomach ulcers is minimal salt consumption or complete abstinence;
- An effective diet for ulcers should provide the body with a full range of nutrients, in other words, eat healthy and nutritious foods, and not ready-made semi-finished products;
- Make sure that the food is not excessively hot or cold; ready-made meals for ulcer patients should be heated to approximately 30 0C;
- For patients with stomach ulcers, it is prohibited to consume alcoholic beverages, as well as drinks containing carbon dioxide;
- You should also not eat foods that contribute to the formation of intestinal gases.
If you are guided by these rules when compiling a list of products, you can achieve an improvement in the general symptoms of the disease, while the menu for patients with ulcers will allow them to feel full and maintain good health. And it is also important that the process of eating during an ulcer brings pleasure and maintains a good appetite.