How many sphincters of the colon are known?
Many people don’t know anything other than the sphincter of the rectum. By the way: the mouth is also a sphincter. Generally speaking, how many sphincters are in the digestive system: thirty-five. Such a clever gateway system. The gastrointestinal tract is like a complex conveyor belt. These “gates” operate between different workshops. Obviously, between, for example, the esophagus and the stomach there is a sphincter. Between the small and large intestines, too. In the area where the bile ducts flow into the lumen of the duodenum there is also a valve - the sphincter of Oddi. Now about less obvious things: there are sphincters in the colon too. Eleven.
Methods for diagnosing the condition of an anatomical structure
The diagnostic value of different methods differs.
- Laboratory determination of the level of liver and pancreatic enzymes is important if the material (venous blood) was taken during a painful attack, at other times it indicates an obstruction in the bile ducts.
- Ultrasound - the diameter of the ducts is determined before and after eating fatty foods; normally, the diameter does not change or even decreases slightly. Dilatation of the ducts by more than 2 mm indicates blockage of the duct; the method has no specificity.
- Hepatobiliary scintigraphy - determines the transit time of the isotope from the liver to the duodenum. The delay in passage confirms the presence of DSO.
- Endoscopic retrograde cholangiopancreatography or ERCP is a therapeutic and diagnostic procedure in which contrast is injected directly into the ducts, then an x-ray is taken. At the same time, the narrowed ducts open, small stones are washed out, and a biopsy is possible during the manipulation.
- Manometry of the sphincter of Oddi is considered the “gold standard” for diagnosing DSO. It is performed using a triple-lumen catheter, which is inserted into the common bile and pancreatic ducts. The study is performed during duodenoscopy. The results are recorded on an attached recording device. The features of motor activity of the sphincter are studied. The base pressure is determined, then the pressure is measured in different areas. The normal difference between the pressure of the sphincter and the duodenum is 10 mmHg. When the sphincter spasms, the pressure in it can increase to 135 mm Hg. A complication of manometry is pancreatitis, so the method is used only for strict indications, not for everyone.
We recommend reading:
Duodenal erosion: symptoms, treatment and prognosis for life
If the anatomical structures are not damaged, then adequate treatment along with a regular balanced diet will help get rid of DSO.
In continuation of the topic, be sure to read:
- Details about the intestines: structure, sections and functions of the organ
- Small intestine: location, structure and functions
- Duodenum: location, structure and functions
- Large duodenal (Vater) papilla: location, functions and diseases of the structure
- Duodenitis (inflammation of the duodenum): symptoms and treatment methods
- Intestinal erosion: causes, symptoms and treatment methods
- Duodenal erosion: symptoms, treatment and prognosis for life
- Preparation for gastroscopy and procedure
- Cancer of the papilla of Vater: symptoms, stages, treatment and prognosis for life
- Antisecretory agents: list and types of drugs, application features
Gateway system
In general, normally there are narrowings in the large intestine, which have been described for a long time. Nevertheless, little attention is paid to this in modern literature. What does this lead to? And to the fact that during diagnostic studies, anatomical narrowings are sometimes mistaken for organic pathology. This is very important, especially if after irrigoscopy you are deciding on surgery. During my work I have to communicate a lot with endoscopists, who constantly observe these sphincters during colonoscopy.
So, in order.
https://youtu.be/QV4ruIfLVC0
Treatment
Diagnosis of rectal diseases
Treatment for the development of this syndrome should be based on what specific disease is causing the spasm. To find out the cause, you need to consult a doctor who can prescribe both a regular relaxing massage and surgical intervention as therapy.
We invite you to watch the professor’s video lecture on the anatomy of the rectum:
https://youtube.com/watch?v=QV4ruIfLVC0%3Ffeature%3Doembed
Medicines
To treat spasms, the following are usually prescribed:
- Antispasmodics;
- Painkillers;
- Antibacterial drugs;
- Laxatives.
Basically, all medications are prescribed in the form of suppositories or ointments, but you can resort to using tablets.
You can also use helper procedures:
- Thermal;
- Physiotherapeutic;
- Electronic sleep;
- Microclysters;
- Massotherapy;
- Applications, etc.
Benefits of massage
For spasms, massage may be prescribed. In this case, the doctor may recommend both a rectal massage, which should be performed by a medical specialist, and a regular relaxing massage if the spasm is neurogenic in nature.
Doctors often prescribe acupuncture massage to prevent disease, as well as to relieve stress on the patient.
Acupuncture and simply relaxing massage has proven itself well in the early stages of diseases manifested in the form of spasm of the anal sphincters.
Traditional methods
Traditional methods offer several ways to help get rid of anal muscle spasm. These include:
- Baths with solutions of potassium permanganate, medicinal herbs, especially chamomile;
- Enemas and microenemas with healing decoctions;
- Tampons and rectal suppositories made from medicinal herbs.
Types of sphincters of the large intestine
Ileocecal valve. Varolius valve. Or Bauhin's valve (valva ileocaecalis)
Described by the Italian anatomist Constanzio Varolio and the Swiss physician Caspar Bauhin. Located in the area of transition of the final section of the small intestine, the ileum, into the cecum. Its function is very important. With inflammation (bauginitis) as well as with functional deficiency, it leads to a number of problems. Therefore it will go into a separate topic.
Cecocolic sphincter (Busi sphincter)
Endoscopists are well aware of this sphincter: when performing a colonoscope, a funnel-shaped narrowing is determined before the entrance to the cecum. It was first described by the German pathologist Otto Busi at the end of the 19th century.
Hirsch valve
Identified by a German doctor of the early 20th century, JSHirsch. Not as pronounced as the previous one. It is found in the ascending colon slightly below the hepatic flexure of the colon.
Cannon-Boehm sphincter. Or right transverse colon sphincter
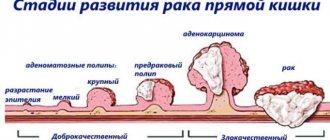
It is also called the right sphincter of Cannon. Well, because there is also a left sphincter - also on the left transverse colon, but on the left, closer to the splenic flexure (identified in 5% of cases, not recognized by some authors, so it was not included in the list). The right sphincter of Cannon is located between the right and middle third of the transverse colon. For quite a long time, scientists have been arguing about the origin and function of intestinal sphincters. According to one hypothesis, sphincters are areas in which the innervation of neighboring nerve plexuses is duplicated. Dr. Cannon described one such sphincter located where embryologically the hindgut becomes the hindgut. Unlike ringed colon cancer, the narrowing formed by Cannon's sphincter changes its shape during a series of irrigoscopy images.
Payr-Strauss sphincter
In 1905, the German surgeon Erwin Payr described a characteristic clinical picture that occurs when the colon narrows in the area of the splenic flexure. This symptom complex is called Payr's syndrome.
Sphincter Balli sphincter
Located in the area of transition of the descending colon to the sigmoid colon. The author himself, when he identified this narrowing, considered it only functional. Subsequently, anatomical thickening of smooth muscles was also revealed. During endoscopy it is detected in 20% of cases, usually oval in shape.
Rossi sphincter
Nazan in honor of the Italian doctor K. Rossi at the beginning of the 20th century. Located at the junction of the abdominal part of the sigmoid colon into the pelvic colon.
Sphincter of Bern-Pirogov-Moutier (sigmorectal sphincter)
Located at the junction of the sigmoid colon and the pelvic colon. The French gastroenterologist Francois Moutier took a great part in the description of this valve.
Proximal rectal sphincter or Nelaton sphincter
This narrowing is detected 8 cm from the anus. Participates in the complex mechanism of defecation. Described by Augustus Nelaton, a French surgeon.
10 and 11. Internal and external sphincter
They deserve a separate topic.
Surgeon Palamarchuk
If you find a typo in the text, please let me know. Select a piece of text and press Ctrl+Enter.
Tags: anatomy, diagnostics, sphincter, colon
- Related Posts
- Migrating motor complex: or how the intestines self-cleanse
- I eat and go to the toilet. Why is that?
- Pacemaker for the intestines
« Previous entry
Symptoms and manifestations
It is not difficult to identify disturbances in the functioning of the internal sphincter, since this condition has the following characteristic features:
- The patient often begins to experience pain in the anus. In this case, the nature of the pain will be sharp, burning, cutting and paroxysmal. Sometimes the pain can also radiate to the perineum, lower back and lower abdomen.
- During the act of defecation, a person may feel colic and severe pain in the anus. Moreover, cramps are also sometimes observed at rest. Usually, after a warm bath, the discomfort subsides for a while.
Judging by surveys of patients, we can also say that stress or severe nervous strain can trigger the resumption of pain.
Moreover, this disease is most often observed in women aged forty to fifty years, as well as in men suffering from excess weight.
Short description
What is this, sphincter? This is a formation of muscle tissue that records the transition of contents throughout the body. The sphincter ring takes on the main task: contraction or narrowing . Such a formation can change in configuration, relax or tense. Muscles take part in many processes, for example, during communication or digestion of food.
Disturbances in the functioning of the sphincters often leave an imprint on health. A person may suffer from frequent vomiting and bile entering the esophagus caused by reflux.
If problems arise with the functioning of the muscles in the lower abdomen, stagnant processes of feces are observed, which causes severe pain to the person.