A person becomes a carrier of the hepatitis C virus when it enters his body. The pathogen does not harm its host and can be transmitted to other people. The category of virus carriers includes patients with a chronic disease that is in a period of weakening: hepatitis C is present in the body, but its signs are not observed.
It is possible to detect hepatitis C carriage only through laboratory tests.
The risk of infection depends on the degree of activity of the virus itself. When the disease enters an acute stage, the carrier is especially dangerous to others if precautions are not taken, since the viral concentration in the blood increases significantly. In chronic hepatitis, the number of pathogens is significantly reduced. In this regard, the patient is less dangerous.
What is the difference between a hepatitis C carrier and a patient?
The disease is caused by a virus that enters the body through the blood. From this moment, carriage of the virus begins, or, as they say, a person becomes a carrier. Not the entire medical community today has come to a consensus on whether there is a difference between two seemingly similar concepts - the patient and the carrier. Some doctors believe that inactive carriage is already hepatitis, but in a dormant form.
Carriage of hepatitis according to ICD-10 has the code Z22.5, which means “carrier of the causative agent of a viral disease.” However, this code was recently removed from the ICD due to its lack of specification. Usually it was called carriage of hepatitis B (Australian antigen).
The next stage after carriage is the onset of the disease. It does not always occur and has a different ICD code.
If the body has a strong enough immune system, then you can not only not get sick, but also stop being a carrier of HCV on your own. This occurs because enough antibodies are produced to neutralize the virus. However, other cases are also possible. If antibodies have not yet been produced in the body, but the processes of liver inflammation are not observed, this means that the immune system is working well and inhibits the development of HCV, while maintaining carriage. In the non-scientific environment, this state is called “dormant”; it can occur for a long time and unnoticed.
However, not every person’s immune system is able to cope with the virus on its own, so if you are a carrier, an inflammatory process can begin at any time. Such a person is already called a patient with hepatitis C, although carriage will continue. The further course of the disease depends on the characteristics of the body and the treatment performed.
Carriage of pathogens
What does it mean to be a carrier of hepatitis C? This question worries many and remains relevant, because as mentioned earlier, the virus can remain in a person’s blood for five, ten or more years without making itself felt.
This raises another question: can the carrier be considered sick and is there any threat to his body, since his health remains normal?
Of course, the presence of a class “C” virus in the body should already be considered a disease, because the virus does not show any signs only because it is contained by the patient’s immune system. However, its spread continues constantly, the disease is slowly but surely gaining strength and, as studies show, in such cases changes in the liver tissue still occur.
How is hepatitis C virus carriage manifested and diagnosed?
Symptoms of HCV carriage are subtle. It is not difficult to carry out tests that indicate the presence of antibodies, but there must be a reason for this. Hepatitis C is characterized by a long subclinical period when no symptoms appear. Also, sometimes the virus can have the usual symptoms of milder illnesses, such as a cold or food poisoning. Therefore, most often the carrier becomes acquainted with the diagnosis unexpectedly.
Typically, the latent (hidden) period of the disease lasts from 3 to 25 weeks. After this, acute hepatitis begins, when signs already appear. First of all this:
- aching joints;
- temperature up to 38°C;
- pain in the liver area;
- nausea.
Similar symptoms describe a large number of other diseases, but such information cannot be neglected. If hepatitis is not treated at the acute stage, it will become chronic, which significantly damages the liver.
To identify carriers of the virus, it is necessary to undergo laboratory tests:
- PCR is a qualitative and quantitative study to detect RNA-containing viruses in the blood and their quantity.
- ELISA – detection of immunoglobulins (antibodies) to the pathogen. Antibodies are detected approximately a month after infection. In 5% of people they are not detected at all - neither during carriage, nor in the acute phase of the disease.
Ultrasound examination of the liver is used to identify complications.
The state of the carrier's body
The disease develops over years and is hidden. If the hepatitis B virus is detected at the very beginning, treatment can be started in a timely manner to achieve complete remission, and precautions can be taken to avoid transmitting the virus to others.
Cirrhosis of the liver
Chronic hepatitis B can be controlled by correcting its development. To do this, you will have to take maintenance medications for the rest of your life. But even so, there remains a high risk of developing the disease up to the onset of oncology or cirrhosis. The probability of this is at least 10% for each carrier. An infectious person is dangerous to others; throughout his life he will carry a “time bomb” inside himself.
Liver cirrhosis is a very serious complication of hepatitis B. The body’s condition is deteriorating all the time, as the organ itself changes - scars appear on it, functionality is impaired, which gradually leads to its failure. A liver transplant may be required. In extreme cases, cirrhosis of the liver can be fatal.
- stagnation of blood in the portal vein;
- accumulation of fluid in the peritoneum - ascites;
- enlarged spleen;
- changes in blood composition;
- sudden weight loss;
- deterioration of general condition, constant fatigue and much more.
There is a risk of internal bleeding in the digestive system and the development of peritonitis. With timely diagnosis and treatment, the prognosis is favorable. Therefore, when external signs appear, it is necessary to undergo a comprehensive examination. The liver in any form of hepatitis B can be supported with the right medications. But in any case, the condition of the infected organism may worsen over the years.
Treatment
According to statistics, approximately 30% of HCV carriers experience complete disappearance of the virus without therapy. That is, the immune system itself reacts to the virus and secretes antibodies that stop the carriage of HCV. This is possible before the onset of the disease or at the stage of acute hepatitis C. The World Health Organization (WHO) recommends treating HCV at any stage. However, the course of treatment remains very expensive. A person must independently assess the risk based on the recommendations of doctors. Sometimes the doctor advises to wait and observe the progression of the carrier state.
After the acute form, the disease enters the chronic stage. In this case, treatment is necessary, because chronicity means the inability of the immune system to cope on its own. Untreated hepatitis C leads to diseases that can be fatal. Most often, the liver suffers from cirrhosis, fibrosis or cancer.
According to WHO recommendations, the main treatment is a course of 2-4 months with the prescription of direct antiviral drugs. These are Sofosbuvir, Ledipasvir, Daclatasvir, Pibrentasvir and their analogues. By acting directly on the pathogen, these drugs reduce the viral load, which reduces damage to the liver.
However, in addition to the cost of drugs, there is another limitation - therapy is not prescribed to children under 12 years of age who are HCV carriers.
To alleviate the condition, vitamins and sorbents are prescribed to improve the functioning of the immune system and relieve symptoms of intoxication.
A separate case is the treatment of HCV during pregnancy. The risk of transmission of the virus from a mother with HCV carriage to the fetus is very low, about 3-5%, so the health of the unborn child is not at risk. The real danger is taking medications for the virus that have a negative effect on the fetus. During pregnancy, doctors should suspend treatment for hepatitis C unless there are serious reasons (exacerbation or worsening of the woman's condition).
Symptoms
Once in the human body, the hepatitis C virus always manifests itself in a certain way. Before entering the latent stage, the body experiences an acute stage. The symptoms of this condition are:
- Increased body temperature;
- Abnormal stool;
- Nausea, bitter taste in the mouth;
- Discolored stool;
- Dark urine.
The last two symptoms always indicate liver problems. If other manifestations can be associated with anything, then white feces and dark urine are always confirmation of organ diseases. These symptoms cannot be ignored. Only those people who are responsible for their health, take care of it, pay attention to such minor deviations, get a chance for a full recovery.
The earlier the fact of hepatitis C infection is detected, the easier it is to get rid of it. The patient faces long, complex and expensive treatment, but he gets the opportunity to fully recover.
5-7 years ago, hepatitis C was considered an incurable disease with a 100% fatal outcome. Now the situation has changed diametrically opposite, thanks to the introduction of innovative treatment regimens based on taking drugs that directly affect the virus.
If you feel unpleasant symptoms, consult a doctor and get examined. If you are found to be a carrier of the hepatitis C virus, find out what actions to take now.
Possible complications
After the transition of viral hepatitis C from the carrier stage to the acute form, gradual changes in the body begin. The first to be affected is the liver, which is gradually destroyed. In the future - cirrhosis and hepatocellular carcinoma (carcinoma).
However, carriage of the virus does not only cause liver disease. General condition worsens:
- general weakness;
- constant dizziness;
- loss of appetite for food;
- deterioration of blood clotting, which leads to serious blood loss even with weak and shallow wounds.
Carriage of hepatitis C causes a general weakening of the immune system, which allows other pathogens to easily enter the body.
The lifespan of HCV virus carriers depends on many factors - genotype, duration of infection, and the ability of the immune system to resist infection. People don’t die from hepatitis C; its consequences are deadly. These are liver cancer and cirrhosis, which develop within 15-30 years after infection, and in HIV-infected people - after 5 years. Therefore, it is recommended to begin treatment immediately after detection of hepatitis carriage.
Virus carriage during pregnancy
Viral hepatitis C is especially dangerous during pregnancy. Therefore, it is important to protect the fetus from infection as much as possible, since the pathogen has the ability to penetrate the placenta. But the most common route of exposure is childbirth, when there is close contact with the mother's biological fluid.
Advice! If the mother is a carrier of the virus, even if she has not shown any symptoms, she must register with a hepatologist.
He will prescribe the necessary tests, conduct an examination, and determine a schedule of planned visits. It is this specialist, based on data on the course of pregnancy, who makes a decision on the possibility of a natural method of delivery. This is allowed provided there is no active infection.
Experts do not have a consensus on the advisability of a cesarean section for hepatitis C. As practice shows, the risk of infection of the fetus is lower, but is still invariably present. The decision is made in each individual case, based on the results of the analyzes. A test that requires obtaining blood from the umbilical cord can confirm whether a child has hepatitis C or not.
Is the carrier infectious to others?
Like other viral diseases, HCV carriage is transmitted through blood, that is, you can become a carrier through contact with infected blood. If you follow certain rules of prevention, the carrier remains safe for others and society as a whole:
- Use only your own personal razor and toothbrush - blood can come out of the wearer’s gums and be transmitted to wounds in the oral cavity of a healthy person.
- Do not share syringes with other people.
- Make sure that the tattoo machine or piercing service uses disposable needles that have not previously been used on other people.
- Don't use drugs. Often, HCV carriage is detected in people suffering from drug addiction, because they almost always use one common syringe for injections.
- In case of intermittent sexual intercourse, use condoms to reduce the likelihood of contact with damage to the partners' genitals.
If you follow generally accepted rules of personal hygiene, contact with the blood of a virus carrier is unlikely, which means that the likelihood of contracting hepatitis is negligible.
Safety regulations
Carriage of hepatitis C imposes on a person the obligation to report his status not only to attending physicians, but also to other specialists who provide dental treatment, perform medical procedures or manipulate blood. Do not underestimate the danger posed by the virus. Therefore, you need to follow a number of simple rules:
- When taking tests or visiting a specialized clinic, report the presence of the virus in the body.
- Do not donate blood; even its individual component is not suitable for these purposes.
- Warn doctors during instrumental diagnostic methods, when undergoing an examination or professional medical examination.
- Do not use other people's shaving equipment, tweezers or nail clippers.
- Medical personnel providing assistance to a virus carrier must use medical gloves to prevent accidental exposure to the pathogen.
- The sexual partner must be warned about the presence of hepatovirus and use contraception during the process.
- If there are small children in the house, to prevent accidental infection, the carrier’s personal belongings are hidden or placed in a locker with a lock.
Relatives of a person who suffers from hepatitis should also know about these rules. They will help protect yourself from infection.
Possibility of getting infected through hugs
The likelihood of transmitting the virus through hugs is minimal. The same goes for handshakes and kisses. Exceptions are cases when the integrity of the oral mucosa is compromised, as well as general and local immunity is reduced. The growth, reproduction and spread of viral infection occurs in the blood plasma. While maintaining the integrity of the skin, touch does not lead to transmission of infection. Tactile contact is possible and important so that a person with hepatitis C feels important and needed. When providing first aid, it is important to have disposable protective gloves in your first aid kit.
Important! As part of general services for the provision of preventive care and therapy, absolutely all people, loved ones and relatives of a person with hepatitis C are advised to be regularly diagnosed for hepatitis C and HIV (human immunodeficiency virus).
Some people have a strong immune response to a viral infection and the body is able to independently cope with the causative agent of the pathological process. Killer cells stop the growth and spread of the virus and specific therapy is no longer required. Antibodies in the blood plasma indicate that a person has had the virus.
Features of sexual transmission of the virus
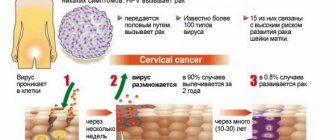
Hepatitis C is transmitted sexually infrequently: in 5-7% of cases. There is a high probability of becoming infected during sex in the following cases:
- sexual intercourse against the background of bloody discharge caused by gynecological diseases, as well as after gynecological intervention;
- intimacy during menstrual bleeding;
- defloration during contact.
Low-risk contacts include interaction with the urine of a carrier of the infection, as well as “deep” wet kisses.
If the virus is detected in a partner and other methods of infection are unlikely or excluded, this indicates a sexual method of transmission of the viral infection.
Chances of getting infected through sex
Married couples should not abstain from sexual activity if one of the partners is a carrier of a viral infection. Semen contains a small concentration of the virus; infection is possible in no more than 4-6% of cases. The risk increases against the background of decreased immunity due to:
- helminthic infestation;
- bacterial infection;
- unhealthy diet;
- bad habits;
- poor quality sleep;
- source of chronic infection in the body: carious teeth. tonsils;
- therapy with immunosuppressive drugs;
- surgical intervention.
Important! Sexual intimacy is not recommended against the background of aggravated type 1 herpes, chronic disease of the ENT organs, during menstruation, or if the integrity of the mucous membranes of the genital organs is damaged.
The disease occurs in a latent form, so regular diagnosis of both sexual partners allows you to avoid serious complications in the future. The virus is transmitted parenterally: through direct contact of healthy blood with infected blood. To reduce the likelihood of infection during sexual intercourse, it is recommended to adhere to the following recommendations:
- refrain from contact during menstrual bleeding;
- refuse kissing if there is a violation of the integrity or ulcerative lesions in the area of the oral mucosa;
- use barrier methods of contraception.
After sexual intercourse, it is recommended to use individual personal hygiene products. This allows you to reduce the risk of infection by more than 2.5 times.
Prevention of disease development
Men, according to statistics, are more likely to encounter the hepatitis B virus than women. But prevention is necessary for every person, regardless of whether he is a carrier or not.
Preventive rules to avoid infection with the virus:
- Do not drink “raw” water - it should be boiled or filtered.
- Wash vegetables and fruits.
- Consume products only after heat treatment.
- Avoid contact with body fluids of other people.
- Use protection during sexual intercourse.
- Maintain hygiene, do not take other people's things.
Hepatitis B is transmitted primarily through blood, which can remain on any object for a long time. The hepatitis virus also persists with it, since it is very resistant. Blood can remain on razors, toothbrushes, even simple scissors - so you should not use other people's personal hygiene items.
If the diagnosis has already been established, it is recommended to undergo examinations at least once every six months. Medical control over the condition of the infected person is established for life. The prognosis for hepatitis B virus carriers is quite favorable. With proper monitoring, the virus in the body does not reactivate, and in some cases it is completely cured.
The chronic type of the disease can last for several decades. To prevent an acute course, the patient must take medications regularly. The disease can progress to a progressive stage, which leads to the formation of cancer cells or the development of cirrhosis of the filter organ. Replacement of parenchymal liver tissue with fibrous connective tissue occurs in 10% of cases.
Cirrhosis is a consequence of the chronic course of the disease. It is characterized by structural changes in the filter organ, followed by the formation of scar tissue and a decrease in its functions. Symptoms of liver cell death take years to develop.
If you are a carrier of the hepatitis B virus, then at the first stage, small convoluted vessels appearing through the skin, reminiscent of a cobweb (spider veins). The skin on the hands turns abnormally red, nodules, rashes and ulcers form. As the disease progresses, the following signs appear:
- difficulty in the outflow of blood through the portal vein;
- accumulation of exudate or transudate in the free abdominal cavity (edema of the abdomen);
- development of splenomegaly (pathological increase in the size of the spleen);
- a critical decrease in the number of leukocytes and platelets in the peripheral blood;
- increased fatigue and overwork;
- deterioration of health;
- sudden weight loss.
For most patients, the question is whether cirrhosis can cause complications? The pathology caused by the final stage of chronic liver disease can cause pathological dilatation of the veins of the esophagus with the formation of irregularities (varixes) with subsequent bleeding, as well as bacterial and aseptic inflammation in the abdominal cavity.
High, medium and low risk contacts
If one of the family members has become infected with hepatitis C, close people also need to be tested for the viral infection. Once the diagnosis is confirmed, it is necessary to begin treatment with modern direct-acting antiviral drugs as soon as possible. Medicines can be used with prior agreement and as prescribed by a gastroenterologist or hepatologist.
Infection occurs through direct contact with a high concentration of the virus, which actively multiplies in the blood plasma. Therefore, high-risk contacts include:
- sharing drugs using shared syringes;
- direct interaction with contaminated donor blood during its transfusion;
- birth from a mother with hepatitis C, with a history of HIV or its complication - AIDS;
- medical manipulations performed with poorly processed instruments: surgery, dental procedures.
Transmission of a viral infection is possible when visiting unverified beauty salons and tattoo parlors where piercings, tattoos, trimmed manicures and pedicures and other traumatic procedures with instruments that have not been properly processed are performed.
Important! Neglecting basic safety measures can lead to large-scale infection of people.
Infected husbands and wives are often unaware of their infection. The manifestation of the virus is manifested by an increase in body temperature, deterioration in general health, pain and aches in the joints, decreased performance and other symptoms of intoxication. The manifestations are non-specific, there is no icteric period, so hepatitis can easily be confused with a cold, acute respiratory viral infection or flu.
Low-risk contacts include interaction with biological fluids that contain minimal concentrations of viral hepatitis: sweat, tears, urine of a carrier of the infection.