783
According to statistics, liver cirrhosis is diagnosed in women three times less often than in men. Typically, the diagnosis is made to patients aged 35-40 to 60 years. The disease does not immediately manifest itself as pain in the hypochondrium, a jaundiced tint of the skin and mucous membranes.
At the initial stage, symptoms of liver cirrhosis in women may be hidden and resemble other pathologies. This makes early diagnosis difficult and entails irreversible changes in the structure of the organ.
Cirrhosis - what is it?
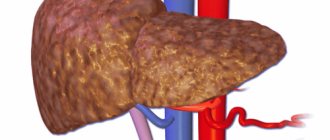
Gradual replacement of hepatocytes with fibrous tissue
Eight thousand years ago, a supernova exploded in the constellation Cygnus, and a nebula appeared in its place. It is poetically called “veil”, “fishing net”, or simply cirrus, cirrus. Cirrhosis and cirrus are the same root words. Cirrhosis is the growth of a mesh structure in the liver.
Normally, the liver consists of cells - hepatocytes, which are penetrated by blood capillaries, and at the exit from them bile is formed, which also collects in the bile ducts. These cells are arranged in tiers, in orderly rows, which are clearly visible under a microscope. These rows are called hepatic lobules, which are strictly organized. Larger segments, lobes of the liver, and the organ itself are made up of lobules.
Hepatocytes make up the liver parenchyma. Parenchyma is a specific tissue of an organ, which constitutes its “meaning”, distinguishing it from others. For example, the parenchyma of the liver and pancreas differ from each other because the functions of these organs are different.
In addition to the intensively working liver cells, there is a supporting (framework) tissue, or stroma - it looks like a network, or a veil. Consists of connective or fibrous tissue. And this framework in any organ is the same in cellular composition. The main role of the stroma is to be a “skeleton” for glandular tissue. With cirrhosis of the liver, all working tissue (parenchyma) gradually dies, and instead there is a proliferation of fibrous tissue. She does not “know how” to do anything, and cannot replace dead hepatocytes. Essentially, with cirrhosis, the entire liver is a rigid mesh, a “washcloth,” of overgrown stroma, interspersed with remnants of working tissue.
Since the liver is a vital organ, cirrhosis of the liver leads to irreversible chronic liver failure and death of the patient. The only chance to survive is a liver transplant.
Causes of cirrhosis
Of course, as with any disease in general, the causes of liver cirrhosis can be hidden even after a thorough and comprehensive examination. In this case, a diagnosis of cryptogenic cirrhosis is made. But this happens very rarely. Much more often, the causes of cirrhosis are more prosaic, both in men and women. Here are the most likely “candidates”:
- The presence of viral hepatitis, including B, C, D. Very rarely, acute hepatitis can transform into cirrhosis, but still the main role belongs to the chronic course, with medium or high activity. In women with hepatitis B and C, with such activity in 25% of cases, the outcome of hepatitis in cirrhosis is possible;
- Regular consumption of alcoholic beverages, alcoholism. If women's daily alcohol intake in terms of ethyl alcohol is 60 - 110 g, then 10% of patients will develop cirrhosis after many years of alcohol consumption. This corresponds to approximately 1.5 liters of strong beer per day (100 g of 96% alcohol). It is important that among female alcoholics, the number of patients with liver cirrhosis at a young age has recently increased;
- Hereditary metabolic diseases (antitrypsin deficiency, hemochromatosis, Wilson-Konovalov disease and others);
- As a side effect on medications (methotrexate, anti-tuberculosis drugs);
- Hepatotoxic poisons (carbon tetrachloride);
- Processes that lead to obstruction of the bile ducts (in this case, women develop secondary biliary cirrhosis). This is cholelithiasis, duct strictures, cholangitis, as well as incomplete obstruction, with partial patency. Usually, under such conditions, cirrhosis of the liver forms within a year;
- In the presence of venous stagnation in the liver tissue (with Budd-Chiari syndrome). The cause may lie far beyond the organ - for example, with valvular defects of the tricuspid valve, with adhesive and constrictive pericarditis.
Cirrhosis can also be caused by parasitic infections (schistosomiasis), autoimmune hepatitis, and other causes.
The effect of alcohol on the body
With regular and long-term alcohol abuse, damage to almost all organs and systems develops. In this case, the liver especially suffers, since it takes the main “blow”, because it is there that the oxidation and processing of alcohol into components that are safe for the body occurs. When the processing function of the liver is impaired, alcoholic liver disease develops, which goes through three stages. The terminal (last) stage is alcoholic cirrhosis of the liver (ALC) or “alcoholic cirrhosis.”
When does “alcoholic cirrhosis” develop?
A measure of alcohol consumption is the amount of consumed ethanol or ethyl alcohol contained in an alcoholic drink. Its content in an alcoholic drink can be calculated using the formula: vol. % x 0.8 = amount of ethyl alcohol in grams per 100 ml of drink. Where vol. % or % vol. - volume percentages (degrees) of alcohol (English - % vol.), usually indicated on a bottle of alcohol-containing drink.
According to statistics, alcoholic cirrhosis of the liver develops in 10–20% of people (according to some data - in a third) who regularly abuse alcohol.
Drinking ethanol doses of 80 ml or more per day by an adult male for 10–15 years leads to irreversible changes in the liver and the development of cirrhosis. And for women this amount is even lower - from 40 ml per day. The given figures are approximate, since the mechanism of ADC development is influenced by many factors.
What are the first signs of liver cirrhosis?
Alcoholic cirrhosis is not immediately noticeable!
Unfortunately, this disease does not always occur with a clear clinical picture. The first signs of liver cirrhosis in women largely depend on the degree of activity of the process. Hepatologists distinguish the following variants of the course of cirrhosis:
- For the overwhelming majority of women (60%), the clinic is bright, and it is simply impossible not to notice it;
- In 20% of cases, the disease is latent, and there are not enough complaints to detect it in a targeted way. Often signs are revealed in tests, as random findings, or during examinations;
- Finally, another 20% of patients “never received” an intravital diagnosis. In this case, this diagnosis is determined only at autopsy.
However, there are a number of symptoms that are characteristic of the initial stages of cirrhotic liver degeneration. The only pity is that they are easy to “miss”, since they can indicate a very wide range of diseases. Judge for yourself, early symptoms of liver cirrhosis include:
- flatulence, or bloating;
- pain and feeling of heaviness in the epigastrium;
- decreased performance;
- weight loss.
If the patient is examined by a doctor, it is possible to detect both an increase in the size of the liver and a thickening of its edge, the appearance of tuberosity, and loss of elasticity. Its free edge will be pointed and dense.
Then, over time, the clinical manifestations of cirrhosis will be varied and specific. This will often make it possible to make a clinical diagnosis even at first glance at the patient.
Etiology
Clinicians note that biliary cirrhosis is most often diagnosed in women. As for etiological factors, the development of the disease is most often provoked by the following:
- infections and viruses;
- taking drugs that promote self-destruction of the body;
- excess hormones - estrogens;
- genetic predisposition;
- the influence of xenobiotics, which are found in cosmetics, food additives and flavor enhancers.
In addition, cirrhosis of the liver can develop due to alcoholism and drug use.
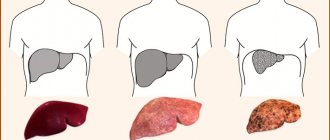
Symptoms and stages of development of cirrhosis
Additional manifestations of the disease
In the advanced stage of clinical manifestations, the symptoms of cirrhosis are composed, like a mosaic, of the following main disorders:
- Manifestations of liver failure (protein synthesis decreases, including for blood clotting);
- Portal hypertension syndrome (increased pressure in the portal vein, which absorbs all the blood flowing from the intestines with absorbed food). This blood goes to the liver for “checking” and neutralization, but with cirrhosis there is a problem with its normal flow through the liver.
These conditions progress and lead to a characteristic clinical picture. Symptoms of liver cirrhosis in women at an advanced stage are as follows:
- Hepatosplenomegaly (enlarged liver and spleen). In the later stages of cirrhosis, on the contrary, a decrease in liver size occurs;
- The appearance of telangiectasia, or “spider veins” on the skin;
- Palmar erythema, or severe redness of the palms;
- The appearance of jaundice - first transient, and then permanent;
- Pain and heaviness in the right hypochondrium;
- With increased activity and progression of cirrhosis, periods of increased temperature are possible, which are accompanied by jaundice and deterioration of health;
- A terrible symptom of portal hypertension is varicose veins of internal organs (stomach, intestines, esophagus) - wherever the “watersheds” of the portal system and the vena cava meet. Increased pressure in the portal vein system forces it to shunt, or dump blood into other pools, and this leads to bleeding.
For example, bleeding from esophageal varices in patients with cirrhosis often leads to death, since it occurs against the background of anemia and a pronounced decrease in blood clotting ability.
- Ascites, or accumulation of free fluid in the abdominal cavity. This is a common symptom of decompensated, advanced cirrhosis.
The belly is large, tense like a ball, its skin is stretched, like a drum, and shiny: the umbilical depression is not visible, it has disappeared. When tapping on the side of the abdomen, if you place your palm on the other side, you can feel a wave of liquid reaching it. Often ascites is accompanied by varicose veins of the anterior abdominal wall, which resemble snakes on the head of Medusa the Gorgon.
This happens because increased pressure in the portal vein system leads to sweating of the liquid part of the blood plasma, which “drains” into the abdominal cavity. Newly diagnosed ascites is always an indication for hospitalization.
Laboratory symptoms of cirrhosis are characterized by a decrease in all red bone marrow sprouts (anemia, thrombocytopenia, leukopenia). After all, a shrinking healthy liver synthesizes little protein, and there is simply nothing to build blood cells from. As a result of leukopenia, purulent processes occur, and due to a decrease in the synthesis of antibodies, the woman begins to develop infectious diseases. Since there is “no means” for the synthesis of platelets, a characteristic sign of low protein-synthesizing function of the liver in cirrhosis is the appearance of bleeding (uterine, nasal from the gums), prolonged blooming of bruises and their appearance as a result of any, even the most minor injuries.
In a biochemical blood test, the level of ALT and AST increases. Normally, these enzymes are located inside liver cells, but when they rapidly decompose, they enter the blood, forming the syndromes of cytolysis and necrosis.
Diagnostics
A doctor can make an accurate diagnosis only after laboratory and instrumental studies. These examination methods include:
- study of blood, urine and feces;
- biochemical blood test;
- Ultrasound and tomography of the abdominal part;
- detection of hepatitis antibodies;
- puncture biopsy.
When examining the disease on ultrasound, the following will indicate cirrhosis:
- uneven organ lining;
- high echogenicity of the parenchyma;
- compactions in the structure of the organ;
- pathologies in the parenchyma area.
“Cheerful pot-bellied leopard,” or why is the disease dangerous?
ascites
If the activity of cirrhosis increases, the pain intensifies, the temperature rises, skin itching and jaundice appear, and spider veins appear. For a long time, the process can proceed with compensation, but if ascites, bleeding, swelling, fever appear, jaundice increases, and encephalopathy develops, then this indicates a catastrophic decrease in liver function.
The appearance of the patient, close to a sad outcome, is characteristic: he is a “cheerful, pot-bellied leopard,” as one of the resuscitators dubbed him. This means that the patient is in a state of euphoria and lack of criticism, and in the intensive care unit he is tied to a bed. A tense, fluid-filled abdomen rises above the body like a mountain, which can hold over 20 liters of ascitic fluid. The skin color of such severe patients is lemon yellow, since jaundice is “layered” on severe anemia and pallor of the skin, and spots of bruises and hemorrhages are scattered throughout the body, which from a distance really resembles the skin of a leopard.
From this condition there is “one step” to profuse bleeding from varicose veins of the esophagus and intestines. Ascitic fluid in conditions of reduced immunity can easily become infected with the development of peritonitis, and hepatic encephalopathy and failure can progress to coma.
The appearance of heptocellular carcinoma, or liver cancer, the occurrence of thrombosis in the portal vein system, and septic complications should not be underestimated.
Principles of treatment of liver cirrhosis
The main task of treatment at the initial stage of liver cirrhosis is to prevent increased activity, decompensation and the occurrence of complications. We list the basic principles of patient management:
- Compliance with a gentle regimen, with limited load, in case of decompensation - bed rest;
- The diet for cirrhosis of any etiology completely excludes alcohol, and proceeds according to the type of table No. 5;
- If the stage is compensated and activity is low, then medications are not needed: they also harm the liver;
- If decompensation occurs, then vitamins, Essentiale, Heptral and Ursofalk are indicated. The use of “berlition” is indicated;
- For decompensation, daily infusion of glucose, vitamins, and calcium gluconate is indicated;
- In case of ascites and a pronounced decrease in protein, albumin 20% and concentrated plasma are transfused.
Each type of cirrhosis has its own specific treatment: viral forms require the use of interferons and antiviral therapy, autoimmune decompensation is controlled by hormones.
If there is a high risk of bleeding, then portocaval anastomoses are artificially created, thus surgical prevention of fatal bleeding is carried out.
How long do people live with cirrhosis, and what should we strive for?
Despite the fact that the course of cirrhosis in women and men is irreversible, modern hepatology can slow down and even “freeze” this process. The main thing is not to lead the matter to decompensation, since with it the three-year survival rate does not exceed 40%. With late diagnosis of cirrhosis, at the stage of advanced symptoms, survival does not exceed 5 years. If the patient has severe ascites, then the usual life expectancy after this sign of decompensation also does not exceed 5–6 years.
But if, for example, a patient is diagnosed with alcoholic cirrhosis in the initial stages, when an adequate person pays attention to his complaints and symptoms, then if he completely abstains from alcohol, he can live with compensated cirrhosis for ten or more years. And then prepare for a liver transplant, which will prolong the patient’s life for many years.
In exactly the same way, if you carefully monitor chronic viral hepatitis, following all medical prescriptions, and keeping its activity low, you can feel good for many years, maintaining a high level of quality of life.
Modern medicine also has resources that have not yet been studied, such as autotransplantation of stem cells. It is known that in in vitro experiments, the cells took root and turned into healthy liver tissue, which in experiments on mice helped reduce the symptoms of experimental cirrhosis. Therefore, in the future, perhaps even during the life of the younger generation, it will be possible to create a new healthy, or artificial, liver.
Tags:
my stomach hurts like my liver hurts
Instrumental methods
The use of various devices in the diagnosis of liver cirrhosis is also a common practice. Moreover, in the modern world this is practically the norm in all existing clinics (including those that cannot boast of the most expensive equipment).
The first procedure used is, of course, ultrasound, better known by the short abbreviation ultrasound. In this particular case, it is used to accurately determine the size and structure of the liver and spleen.
Further, it is impossible to do without a puncture biopsy of the liver, or, in short, a puncture. This painful and complicated procedure is required to remove a piece of the liver for later laboratory testing (as the two methods often interact).
More modern clinics often use a procedure called computed tomography, or CT, to treat symptoms of alcoholic cirrhosis. There is some similarity with ultrasound, but in this case the matter is not limited to one image. On the contrary, a whole series is made, which is then compared and analyzed in order to obtain an accurate “picture” of the condition of the liver and spleen.
This procedure is often complemented by MRI - magnetic resonance imaging - for the same purposes.