Causes
The duodenal bulb is topographically located near the pyloric section of the stomach. Therefore, if the functioning of the gastrointestinal tract organs is disrupted (in this case we are talking about the final section of the stomach and the initial section of the intestine), acidic contents may be thrown into the duodenum, where pH is alkaline. The aggressive effect of gastric juice irritates the intestinal wall, causing a violation of its integrity.
In addition to local factors, bad habits (smoking, alcohol abuse) and stressful situations also play a significant role in the pathogenesis of the disease. Detection of Helicobacter pylori in the body increases the risk of peptic ulcer disease.
Signs and symptoms
As such, there are no clear symptoms that would make it clear whether there is a scar or not. After a few years, the intestinal walls smooth out on their own and everything returns to normal. But if the peptic ulcer is repeated every time, then the scars, accordingly, become more numerous. This leads to a gradual narrowing of the intestinal walls and ultimately to complete intestinal obstruction. The signs of duodenal ulcer are the following:
- Pain that is localized in the upper abdomen. Such pain can be influenced by various factors. Their cause may be food intake, but then the pain appears after a couple of hours, or as a result of acidic contents entering the walls of the duodenum.
- Disorders due to disturbances in the normal functioning of the stomach. It is caused by increased acidity and is accompanied by nausea, vomiting, constipation or bloating. Due to these disorders, a person loses his appetite and, as a result, loses weight.
Pathogenesis
Erosion affects the surface layers, regeneration processes take place without scarring. An ulcer eats away at the wall of the organ down to the muscle tissue (with perforation, the muscle layer also becomes completely thin), so during the recovery stage it is not possible to avoid the development of a connective tissue scar.
The more often a person experiences exacerbations of peptic ulcer disease, the more severe the morphological and functional changes are experienced by the initial section of the intestine, represented by the duodenum.
In the development of scar deformity, experts distinguish the following stages: compensation, subcompensation, decompensation. Let's see what the difference is.
- The compensatory and subcompensatory stages are characterized by the presence of a lumen in the area of the duodenal bulb of at least 0.5 cm.
- The process is said to be decompensated when the degree of narrowing is significant (lumen diameter
Causes of pathology
Inflammatory cicatricial deformation of the intestine is formed at the site of a protracted duodenal ulcer.
Erosive lesions that turn into ulcerations develop due to the pathological effects of increased amounts of hydrochloric acid in gastric juice and pepsin, as in the formation of ulcers in the stomach.
If there is no treatment for the stomach and intestines, then peptic ulcer disease affects the lower layers of the epithelium and can lead to perforation of the intestinal wall with subsequent bleeding.
Reasons leading to the appearance of erosions and ulcers of the mucous membrane and, as a consequence, to cicatricial deformation of the duodenum:
- inflammatory processes on the mucous membrane (gastritis);
- long-term use of corticosteroids and NSAIDs (non-steroidal anti-inflammatory drugs);
- drinking alcoholic beverages in large quantities;
- repeated stress and nervous tension;
- increased secretion of gastrin, leading to an increase in the level of acid in gastric juice;
- the presence of Helicobacter Pylori bacteria on the mucous membrane;
- untimely treatment (ignoring the first symptoms of the disease).
These factors lead to the gradual development of inflammation of the gastric and duodenal mucosa.
Peptic ulcers and scars on the intestinal mucosa appear if treatment has not been prescribed. This process can take place in different parts of the duodenum, but is more often localized in the bulb.
Like all granulations, scar formation of the intestine tightens the tissues surrounding it, thereby changing the shape of the section.
1 - relief niche; 2 - relief-niche and cicatricial deformation of the duodenal bulb in the form of a trefoil; 3 - niche extending beyond the contour of the bulb; 4 - niche with an inflammatory shaft around
If scars are contained in large quantities in one place, then this accumulation leads to deformation of the duodenal bulb.
Clinic
Patients with deformation of the duodenal bulb are people with a long history of the disease. Clinically, each of the 3 stages described above is characterized by certain symptoms. Let's take a closer look at them.
Compensation phase. The movement of the food bolus through the gastrointestinal tract is slightly disturbed. Retention of gastric contents occurs for 6-8 hours.
Patients complain of:
- feeling of heaviness in the epigastric area after eating;
- nausea;
- periodic vomiting;
- belching (there is a feeling of acid in the mouth).
With a pronounced concomitant inflammatory process, periodic pain is also observed. There is deep, enhanced peristalsis.
The subcompensation phase is characterized by signs of motor-evacuation failure, the food bolus lingers in the stomach for up to 24 hours, peristalsis is weakened. The following symptoms are expressed:
- Constant feeling of heaviness localized in the epigastrium.
- The belching intensifies, acquiring a “rotten” character.
- Copious, frequent vomiting. Perhaps even in the morning, when the patient has not yet had breakfast. In this case, a large amount of eaten food leaves the stomach with signs of fermentation. People often induce vomiting because it provides temporary relief.
- Bad breath occurs due to stagnation and rotting of proteins.
In the decompensation phase, signs of intoxication increase. Due to the lack of lumen in the area of scar deformation, symptoms of complete intestinal obstruction develop.
- Weakness, obvious deterioration in general condition.
- Progressive loss of body weight.
- The presence of symptoms of dehydration: dry skin, sallow color, pointed facial features.
- Feeling of increased dryness in the mouth.
- Diuresis decreases.
- Tachycardia increases.
Increased disturbances in water-electrolyte metabolism lead to severe hypochloremia and hypocalcemia. And this in turn causes the appearance of signs of convulsive syndrome.
Duodenal ulcer
- pain syndrome, which is one of the main and main symptoms of duodenal ulcer. The pain is localized (located) in the epigastric region or above the navel. Duodenal ulcers are characterized by pain that appears on an empty stomach or 2-3 hours after eating (“hunger” pain), often at night (“night” pain). “Night” pain is associated with increased formation of hydrochloric acid in the stomach at night. The pain decreases after eating. Sometimes the pain radiates (gives) under the shoulder blades, to the back, to the heart area. Increased pain is caused by: dietary errors, overeating, alcohol consumption, stress, certain medications (for example, non-steroidal anti-inflammatory drugs (NSAIDs)), hormonal drugs (“steroid ulcers”);
- seasonality of exacerbations of the disease. Peptic ulcer disease is characterized by an exacerbation of symptoms in the spring and autumn, while in the summer and winter months the symptoms subside or are absent altogether;
- heartburn;
- belching;
- bloating;
- nausea;
- vomiting, which brings relief (sometimes patients induce vomiting on purpose);
- constipation (no bowel movements for several days or weeks), sometimes blood in the stool;
- irritability, bad mood and sleep;
- weight loss (despite good appetite).
Based on the frequency of exacerbations, the following forms of duodenal ulcer are distinguished:
- with frequent exacerbations (more than 2 times a year);
- with rare exacerbations (1-2 times a year).
According to the location of the ulcers:
- in the area of the duodenal bulb (the expanded part of the duodenum);
- in the post-bulb portion of the duodenum;
According to the depth of damage to the wall of the duodenum:
- superficial (minor wall defect);
- deep (deep damage to the wall of the duodenum).
According to the condition of the ulcer itself:
- stage of active exacerbation (typical clinical picture - pain, nausea, vomiting, etc.);
- scar formation (after healing of the ulcerative defect, a scar forms);
- remission (temporary absence of symptoms of the disease).
Depending on the cause of the disease, there are:
- “stress ulcers” (against the background of strong emotional tension, stress);
- “shock” ulcers (after serious injuries, severe burns, etc.);
- “steroid” ulcers (while taking hormonal drugs).
- Infection with the microorganism Helicobacter pylori (considered the leading cause of gastric inflammation and, over a long period of time, can lead to the development of duodenal ulcer).
- Genetic predisposition (heredity).
- Decreased immunity.
- Increased acidity of gastric juice, which, when entering the duodenum, has an irritating effect on its wall.
- Duodenitis (inflammation of the duodenum).
- Dry food, consumption of semi-finished products, carbonated drinks, spices and seasonings, smoked, fried, salted, spicy, too cold or hot food.
- Stress, nervous strain (“stress” ulcers).
- Severe burns, injuries, blood loss (“shock” ulcers). Taking certain medications: hormonal (“steroid” ulcers), non-steroidal anti-inflammatory drugs, antibiotics, etc.
- Excessive alcohol intake.
- Analysis of the medical history and complaints (when the complaints appeared, is the onset of pain related to eating, is the pain bothersome at night, is there a seasonality of exacerbations (autumn and spring), to which the patient associates the occurrence of symptoms).
- Analysis of life history (were there any diseases of the gastrointestinal tract: gastritis (inflammation of the stomach), duodenitis (inflammation of the duodenum)).
- Family history (does anyone in the family have similar complaints).
- General blood test (to determine the content of hemoglobin (a protein involved in the transport of oxygen), erythrocytes (red blood cells), platelets (blood cells that participate in blood clotting processes), leukocytes (white blood cells), etc.).
- General urine analysis.
- Fecal occult blood test for suspected bleeding from the gastrointestinal tract.
- Study of gastric juice acidity.
- Esophagogastroduodenoscopy (EGDS) is an examination of the mucous membrane of the esophagus, stomach and duodenum using a special device (endoscope). During the procedure, the mucous membrane of the stomach and duodenum is examined, the presence of ulcerative defects, their number and location are detected, and a piece of the mucous membrane is taken for examination (biopsy) of stomach cells to identify its diseases.
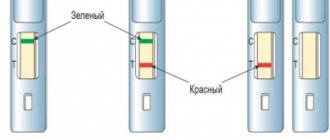
Diagnostics - detection of Helicobacter pylori:
- cytological examination (determination of the microorganism by examining a piece of the gastric mucosa obtained during a biopsy);
- urease breath test (determining the degree of Hpylori infection in exhaled air).
- Immunological research (determining the presence and titer (concentration) of antibodies (specific proteins)), etc.
- A consultation with a therapist is also possible.
- A rational and balanced diet (eating foods high in fiber (vegetables, fruits, herbs), avoiding fried, canned, too spicy and hot foods). It is recommended to eat boiled food, steamed food, semi-liquid food, eat frequently, 5-6 times a day, in small portions, and avoid excessive intake of alcohol.
Reception:
- antacids (drugs that reduce the acidity of gastric contents);
- antisecretory drugs (reducing the production of gastric juice);
- antibacterial drugs (to eliminate the microorganism Helicobacter pylori). Usually a combination of 3 or 4 antibacterial drugs is prescribed.
- Surgical treatment is carried out in case of complications, as well as in case of frequent relapses (exacerbation of the disease), in case of the formation of rough scars in the duodenum after healing of ulcers - with prolonged healing.
Bleeding from the duodenum. Observed:
- vomit “the color of coffee grounds”;
- dark, tarry stool;
- loss of consciousness with severe blood loss.
Ulcer perforation (rupture of the intestinal wall in the area of the ulcer). When perforation occurs:
- severe, unbearable pain (“dagger”);
- nausea, vomiting;
- tension in the abdominal muscles (“board” belly).
- The occurrence of peritonitis (inflammation of the peritoneum): with perforation (rupture of the intestinal wall in the area of the ulcer) the intestinal contents leak into the abdominal cavity.
- Penetration (spread of the inflammatory process from the duodenum to neighboring organs - liver, pancreas, etc.).
- Development of duodenitis (inflammation of the duodenum).
- Formation of scar narrowing of the duodenum.
- Tumor formation in the duodenum (malignancy).
- A rational and balanced diet (eating foods high in fiber (vegetables, fruits, herbs), avoiding fried, canned, too hot and spicy foods).
- Avoiding excessive alcohol consumption.
- Treatment of intestinal diseases, for example, duodenitis (inflammation of the duodenum).
Folk remedies
The disease is seasonal and in 90% of cases it is infectious in nature and requires etiological treatment in the autumn-spring period during the formation of acute ulcers or preventive therapy to prolong the period of remission.
It should be borne in mind that even during the subsidence of active inflammation and scarring of ulcerative defects, but in the presence of symptoms, the patient will need treatment.
If in the case of a gastric ulcer the picture of the disease is often erased, especially if it is located high in the bottom, body or cardiac part of the stomach, then with an ulcerative lesion of the duodenum, the classic symptoms of the disease develop, and the diagnosis is clear already at the preclinical stage. Further, in the pathology clinic, several stages of the process should be distinguished: acute, chronic ulcers, ulcerative-cicatricial and cicatricial deformities.
The most striking manifestations are observed during an acute bulb ulcer or during an exacerbation of a chronic ulcer. Typical signs are hunger pain 1.5-2 hours after eating or on an empty stomach, which is relieved by eating. Pain syndrome can be provoked by alcohol, spicy foods, smoking, and stress factors.
The pain is characterized by irradiation to the liver, back, and heart. Contrary to the majority opinion, heartburn is not a characteristic symptom of a gastric or duodenal ulcer, but indicates the presence of insufficiency of the cardiac sphincter (achalasia cardia), reflux of stomach contents into the esophagus and a possible increase in the level of acidity of gastric juice.
The same is indicated by belching and regurgitation of eaten food.
Pyloroduodenal stenosis is the result of scarring of a healed or active ulcer with severe inflammatory tissue infiltration. The following symptoms appear with stenosis:
- Vomiting with the smell of “rotten eggs” (periodically or with aggravation of the process, constantly occurring when the stomach is full).
- Heaviness after eating, heartburn, belching, regurgitation.
- Exhaustion due to poor digestion of food.
- Pain of varying severity (depending on the presence of an acute ulcer).
- At the end of the disease - dehydration, severe enterocolitis (intestinal pathology).
- Dermatitis.
- Nervous system disorders (signs of dementia).
- Possible seizures due to calcium loss.
Stenosis of the pylorus and duodenal bulb is functional, that is, associated with temporary severe swelling of the mucous membrane in the area of the ulcer.
On FEGDS, the endoscopist will record an ulcerative defect located in the area of the pylorus or duodenal bulb against the background of hyperemia (redness) and deformation of this part of the gastrointestinal tract.
In this case, vomiting, pain and heaviness in the abdomen, heartburn and nausea will disappear without a trace when the inflammation subsides and the ulcer heals (within 2-3 weeks of treatment).
Diagnostics
The diagnosis of “cicatricial deformity of the duodenal bulb” is made on the basis of the described symptom complex, gastroscopy data, X-ray results, and when studying the motor function of the gastrointestinal tract. A mandatory component of diagnostic measures is a comprehensive laboratory examination.
X-ray is indicated to detect an area of stenosis due to cicatricial deformation, clarify its nature, and the stage of compensation of the pathological process.
- The study is carried out after emptying the stomach using the polypositional technique.
- A double contrast method using a barium contrast mixture and air is also used.
- The narrowing of the lumen of the duodenum due to peptic ulcer is characterized by smooth contours and a smooth mucous membrane. In the case of a tumor process, there is a constant rigidity of the stenosis area, the contours are uneven, corroded, and a filling defect is observed.
- In the stage of decompensation, a significant expansion of the stomach containing a large amount of mucus, liquid, and food debris is determined by X-ray. Since the walls are hypotonic, the contrast mass immediately sinks to the bottom, forming a bowl with a horizontal level.
Laboratory research. Massive dehydration leads to loss of electrolytes, salts, protein, water, and chlorides.
- Hypoproteinemia.
- Hypokalemia.
- Azotemia.
- Alkalosis.
- Water and electrolyte imbalance: hypochloremia, hypocalcemia.
- Blood thickening.
- Polyhypovitaminosis.
- Decreased kidney function.
Treatment
Treatment of patients with cicatricial deformation of the duodenum is surgical. Significant importance is also given to preoperative preparation, which includes measures aimed at normalizing motor skills and restoring metabolic disorders.
First of all, regular gastric lavage is indicated. Taking into account the level of hypochloremia, hypokalemia, azotemia, metabolic alkalosis, hypoproteinemia, intravenous infusions of polyionic solutions and protein hydrolysates are performed:
- To correct the water-electrolyte composition, an isotonic solution is administered.
- To restore carbohydrate metabolism, 10-20% glucose is used.
- Normalization of protein balance is achieved by using plasma, proteins, and albumins.
- Cardiac glycosides are prescribed to stabilize the functioning of the cardiovascular system.
- Vitamins B, C, K are indicated for hypovitaminosis.
Peptic ulcer disease is dangerous due to the development of severe consequences. The morphological changes in the structure of organs that arise in this case are irreversible and lead to increased functional disorders. A healthy lifestyle, proper nutrition, absence of bad habits, minimizing stressful situations - all this significantly reduces the likelihood of signs of the disease and its complications.
Cicatricial deformation of the duodenal bulb is a residual form of the main pathological process associated with a severe form of erosion or ulcer of the corresponding localization of the underlying organ.
What are the additional reasons for the formation of such a structure? How is it detected and diagnosed? How effective is non-surgical treatment? You will read about this and much more in our article.
How to avoid and treat scar deformity?
Cicatricial deformity is a complication of intestinal ulcer. The most effective method to avoid the occurrence of this disease is to treat the ulcer in a timely manner and take the necessary measures to prevent its occurrence.
If, based on the results of laboratory tests, a bacterial cause of the development of the pathology has been established, then a course of antibacterial therapy aimed at destroying H. Pylori is necessary.
It consists of prescribing two antibiotics: Amoxicillin and Clarithromycin. Additionally, the drug Metronidazole may be prescribed. This scheme completely destroys the pathogenic microbe.
Medications aimed at reducing the secretory function of the stomach must be prescribed.
Because the high acidity of gastric juice greatly irritates the mucous membrane and leads to the formation of ulcers of the duodenal bulb.
Drug therapy gradually leads to a decrease in the amount of hydrochloric acid and pepsin produced.
Pathological processes are stopped under the influence of Omez and Nexium, and the life activity of the pathogenic bacteria ceases.
Patients with this disease should not engage in heavy physical labor or active sports, but they should walk more in the fresh air.
The patient needs peace of mind and should avoid stressful situations. You also need to get rid of bad habits: smoking and drinking alcohol.
Patients with diseases of the stomach and intestines need a gentle diet, regardless of the reasons that led to a violation of the integrity of the intestinal mucosa.
This prescription especially applies to patients with duodenal bulb ulcers.
Dietary nutrition should exclude all foods that can cause irritation to the surfaces of the gastrointestinal tract, and also have a beneficial effect on the proliferation of beneficial microorganisms in the intestines. Food is taken often, in small portions.
Food products must be completely cooked and preferably ground through a sieve. It is possible to consume porridges with water and dairy products.
During an exacerbation of pathology of the stomach and intestines, it is necessary:
- chew food thoroughly or grind it using a blender or sieve;
- eat every 2.5 hours;
- exclude rich soups and broths from the diet;
- do not use spices and herbs in the cooking process;
- Cold and hot food is prohibited.
Cicatricial deformation of the duodenal bulb is a residual form of the main pathological process associated with a severe form of erosion or ulcer of the corresponding localization of the underlying organ.
What are the additional reasons for the formation of such a structure? How is it detected and diagnosed? How effective is non-surgical treatment? You will read about this and much more in our article.
Reasons for the development of the pathological process
The duodenum, which is the initial section of the small intestine and located after the pylorus of the stomach, consists of several elements. The key is a bulb or ampoule that has longitudinal folding.
As part of various pathological processes and the formation of an inflammatory reaction on the mucous membranes of the organ, a partial change in the structure of the epithelium occurs, resulting in the creation of preconditions for the formation of scars.
Such deformations usually clearly indicate a partially or completely healed ulcer, but may also indicate other causes of pathology. The most famous:
- Incoming deformation against the background of severe edema due to the inflammatory process of the entire duodenum;
- Physical compression of the bulb due to the influence of external or internal factors - injuries, features of the anatomical structure of the patient’s neighboring organs, and so on;
- Systemic pathological processes affecting the gastrointestinal tract complex. In the latter case, scarring of the duodenal bulb is a secondary complication.
Symptoms of scar deformation of the duodenum
The symptoms of scar deformation of the duodenum are not specific and depend on the severity of scarring and its type, the presence of secondary provoking circumstances that form the prerequisites for exacerbation of the process.
In this context, during instrumental examination, asymmetry of the bulb is observed, caused by partial shortening of one of its contours, but the lumens of the organ are open, and the evacuation of the contents proceeds normally.
Primary, externally diagnosed signs are characteristic of moderate and severe deformities with the formation of diverticulum-like protrusions, “trefoils” within the framework of cicatricial convergence with a narrowing of the lumen up to 50% or more, a parallel slowdown in the function of evacuation of biological contents up to 1 day or more.
In this context, the following manifestations are possible:
- Pain in the upper abdomen radiating to the back and neighboring organs. The pain syndrome intensifies with prolonged fasting and at night;
- The appearance of belching , nausea, increased gas formation and intestinal discomfort, and other wide-spectrum dyspeptic disorders;
- Staining of vomit and feces with bloody inclusions, indicating the start of internal bleeding - such a symptom directly threatens the patient’s life and requires his immediate hospitalization in a hospital and intensive care unit.
In addition, a relapse of the ulcerative pathological process against the background of organ structures weakened by cicatricial deformations sometimes leads to partial or complete blocking of the passage to the pylorus, where hydrochloric acid for the stomach is located.
Ultimately, this causes the substance to enter the intestine with subsequent migration of pancreatic bile fluids through various parts of the gastrointestinal tract, contributing to the development of a complex pathological acute process.
Diagnosis of pathology
Determination of the primary and final diagnosis of cicatricial and ulcerative deformation of the duodenal bulb 12 is carried out comprehensively based on the results of laboratory instrumental studies. The main activities include the following procedures:
- X-ray examination with the introduction of barium-based contrast to assess the degree of evacuation function;
- Ultrasound of the duodenum. Allows you to assess the condition of the bulb in general terms;
- Penetrating fibrogastroduodenoscopy. The most informative, but invasive endoscopic technique;
- Other activities as necessary.
Treatment of scar deformity of the duodenal bulb
After determining the main diagnosis, the gastroenterologist prescribes individual treatment, including complex measures:
- Drug therapy;
- Diet;
- Preventive actions.
After the main inflammatory process has been removed, the rationality of performing surgical intervention to eliminate scar structures within the framework of classical surgery is considered.
As part of pharmaceutical treatment, painkillers and anti-inflammatory drugs , agents for improving peristalsis, corticosteroids, and colloidal solutions that restore mucous membranes are prescribed.
In addition, symptomatic treatment is carried out, eliminating the most unpleasant manifestations of the underlying ulcerative pathology and secondary cicatricial deformities of the duodenal bulb.
Various physiotherapeutic procedures are prescribed for the second time , including electrophoresis, UHF, balneological treatment, ozokerite applications and other actions as necessary.
Self-prescription for scar-inflammatory deformation of the duodenal bulb 12 of any medications, various procedures, including the use of folk recipes introduced into the main treatment regimen without the prior approval of a gastroenterologist, is strictly prohibited!
Causes of cicatricial deformity in duodenal bulb ulcer
The causes of peptic ulcer disease lie in the effect of increased concentrations of hydrochloric acid on the intestinal walls. It seems to corrode the mucous membrane, causing erosive formations and destroying the integrity of the tissues. There can be many catalysts for the development of the disease.
- microflora disturbance with a predominance of pathogenic microorganisms;
- a person’s choice in favor of an unhealthy diet, in which fried, spicy or hot foods, snacks on the run predominate;
- long-term use of a certain group of medications;
- bad habits: alcohol, smoking;
- exposure to regular stress;
- the presence of other gastrointestinal diseases;
- long-term helminthic infestation;
- genetic predisposition.
Also, an acute ulcer of the duodenal bulb can develop due to trauma to the epigastric region or internal damage to the mucosa due to an ingested foreign body, or the presence of chronic diseases. A thorough collection of the patient’s medical history and timely diagnosis will help determine the exact cause.
The cause of cicatricial deformation of the duodenal bulb 12 is the regular exacerbation of intestinal ulcer. The larger the area of tissue that is damaged, the more the tissue will subsequently become deformed.
This disease is not the last among diseases of this nature. YLDK in the first stages is very difficult to diagnose. The patient himself does not pay attention to the initial symptoms, such as nausea in the morning, feeling of hunger, mild stomach pain.
Quite common signals do not cause alertness, which is the main reason for the high incidence of this disease. The duodenum has a complex structure, its wall consists of:
- muscle layer;
- mucous layer;
- submucosal layer.
The ulcer located in the first layer is the affected part of the intestine, respectively, the submucosa and mucosa are destroyed. This disease received this name due to the fact that favorable conditions for the functioning of bacteria and infection are observed precisely in the first section (bulb).
There are cases when several ulcers form at once, most often they are paired and located in parallel. According to statistics, middle-aged and young people most often suffer from ILDC - about 70% of all cases.
Causes
ILDK is a serious disease that has a high percentage of diagnoses (more often than an ulcer outside the bulb). One of the main reasons is a failure of acidity (or rather, its increase, which allows bacteria to actively develop). Doctors name the following reasons:
- Helicobacter piloni (a very popular assumption about the cause of the disease. This bacterium attacks the cells that produce mucus, which quickly spreads throughout the stomach very quickly).
- Rough food (it is believed that food entering the intestine scratches it).
- Blood type (doctors do not exclude this fact; according to statistics, people with the first group get sick most often).
- Stress (an important reason. People often do not understand that frequent exercise, little sleep, constant irritability, worries can significantly affect health, or rather the formation of ulcers. All this happens due to the fact that, against the background of stress, it is intensively produced and enters the intestines gastric juice).
- The sun (prolonged sunbathing stimulates the production of gastrin (hormone), which affects the deterioration of the patient’s condition with ulcerative dysplasia and provokes complications).
- Medicines (incorrect diagnosis or self-medication can significantly worsen or provoke the disease).
- Eating disorders (consuming excessive amounts of spicy, fatty, carbonated drinks in the diet, using diets without prescription from nutritionists).
- Heredity.
- Alcohol, nicotine (their use changes the amount of gastrin production, worsens the situation as a whole, provokes illness, damaging the mucous membrane).
- Other diseases (an ulcer may form due to other diseases: HIV, hypercalcemia, liver cirrhosis, Crohn's disease).
Symptoms
There are several stages of the disease. At first, the symptoms that appear do not cause suspicion. But they are the ones you need to pay attention to for a quick and correct diagnosis.
The sooner the disease is noticed, the less consequences and harm it will cause to the body. Main symptoms:
- Heartburn. At first glance, it is a common symptom that patients attribute to the body’s reaction, for example, to spicy food. Not everyone knows that heartburn manifests itself in three out of five cases with an intestinal ulcer. This is due to the fact that a large amount of acidic stomach contents and inflammatory processes and changes in the intestine are discharged into the esophagus).
- Appetite disorders (the body’s rejection of food, a common occurrence, since food can provoke painful sensations. A sharp increase in appetite indicates that the condition improves with consumption of food).
- Pain (with an ulcer, unpleasant sensations appear two to three hours after eating. Frequent pain even in cases where the patient does not eat for about four hours. The characteristics and types of pain are very different. They can be in the morning or before bedtime, acute or aching, cutting, and also of varying duration. The pain is felt on the right side, it can radiate to the back area. Pain is caused by inflammation, disturbances in the functioning of the intestine, the accumulation of products that have not been processed).
- Vomiting/nausea (you can read more about vomiting here). This is also associated with rejection of food intake and inflammatory processes.
Complications
If you do not pay special attention to all the symptoms in the first stages, the ulcer may scar on its own. There is a high risk that this will cause a large number of complications, which significantly complicates the treatment and the patient’s survival rate. Complications are divided into two groups: Dysmorphic (change the structure of the intestine):
- cicatricial (due to scar formation, the intestinal walls narrow and can completely close its entire intestine);
- malignancy (a tumor develops at the site of the ulcer).
Destructive (corroding the intestines):
- penetration (infection of neighboring organs);
- bleeding;
- perforation.
Stages
- The first stage (healing is characteristic, the layers of epithelium are superimposed one on top);
- The second stage (healing, which is characterized by the appearance of papillomas on the surface of the intestine);
- Third stage (minor scars appear, with a detailed examination new ulcers are noticeable);
- Stage four (scars form).
Diagnostics
First of all, you need to understand that this disease is quite serious and its diagnosis and treatment are complex. In order for the disease to go as smoothly and painlessly as possible, it is necessary to consult a doctor in a timely manner for the correct prescription.
At the moment, the most common and effective method is fibrogastrodudenoscopy. With it, an optical umbrella is used, which is inserted into the intestine and you can easily determine the presence of ulcerative formations, find out the exact location, condition, and size. If the diagnosis is confirmed, then X-ray diagnostics, stool and blood tests are also used to clarify it.
Treatment
When diagnosing ulcerative ulcers, treatment directly depends on the stage of development of the ulcer, its size, and the number of scar formations. Therapy may be reduced to drug treatment.
At the moment, surgical intervention is almost never used for this disease (typical only in cases where there are contraindications to pills and medications or severe complications).
It is recommended to eat 4-5 times a day, but in small quantities. A mandatory criterion is that the food should not be cold or too hot (36-37 degrees). The use of nicotine and alcohol is not permissible. Recommendations:
- It is advisable to deny yourself spicy, fatty, fried, strong coffee and tea, and pastries.
- You will also have to give up vegetables: carrots, apples, pears, cabbage, tomatoes, radishes, cucumbers (all those that have fiber).
- Give up chewing gum.
- It is recommended to eat boiled, chopped food: porridge, soups, purees, fish (steam), cutlets. As for fruits: bananas, watermelons.
- Fermented milk products are also prohibited.
Folk remedies
One of the most effective and frequently used remedies is potato juice (freshly squeezed). It is recommended to use the American variety. The method is not very pleasant, but over time you easily get used to it. The product must be used three times a day.
The peculiarity and inconvenience is that the obligatory criterion is that the juice must be freshly squeezed. Potatoes must be grated on a fine grater and rubbed through a sieve (or squeezed through cheesecloth). In the first three to four days you need to drink a tablespoon three times a day, then you can reduce the dose to two spoons. Take 30 minutes before meals. The course lasts 3-4 weeks.
Our health is all we have. It is our duty to preserve it, which is why frequent preventive examinations are recommended for timely diagnosis of diseases. Pay special attention to all of the above symptoms. Do not self-medicate, but consult a doctor.
Diseases of the stomach and duodenum
Cicatricial deformation of the duodenal bulb is a condition of the initial part of the intestine that develops after an ulcer in this location, characterized by the formation of scars that change the shape and disrupt the function of the bulb.
In most cases, duodenal ulcers develop in the bulb (the border between the upper and lower gastrointestinal tract). Transbulbar sections (from the Latin bulbus - bulb) are affected by ulcerative defects much less often.
This is primarily due to the fact that it is in this place that the border between the acidic environment of the stomach and the alkaline environment of the intestine begins.
At the slightest malfunction and inflammation, a large amount of acid enters the bulb, causing destruction of the mucous membrane, the formation of erosions and ulcers - that is, it is the bulb that suffers first.
During the healing process of an ulcer of the duodenal bulb, a scar is formed. Just as scars form on the skin after a wound, so after an ulcer the completely normal structure of the tissue is never restored, being replaced by a dense connecting “tie” - a scar. If you treat a wound poorly, let it fester, and do not resort to modern medical care, instead of a wound you will soon have a disfiguring
Correction of the power plan
In most cases, in the absence of complications and multiple relapses of the pathological process, diet shows high effectiveness in moderate and advanced forms of cicatricial deformation of the duodenal bulb (DU). Correction of the diet begins with the exclusion of the heaviest foods that are prohibited for consumption in case of ulcers and deformities of the organ bulb. Completely prohibited:
- Any type of alcohol;
- Rye bread;
- Fatty fried foods;
- Pickles and smoked meats;
- Canned food and marinades;
- Rich broths.
Spices, sweets, coffee, and tea are consumed with great restriction.
Under additional control are any foods and dishes that can significantly affect the acidity of the stomach, cause intestinal hyperactivity, or, conversely, significantly slow down its work.
It is allowed to steam, boil, or, in extreme cases, bake. Food is served only warm. The consistency of the products is small pieces, paste-like and liquid (large pieces are not allowed).
Possible complications
Cicatricial deformation of the duodenal bulb often causes complications, especially in the presence of predisposing circumstances. The most common problems:
- Relapse of the ulcerative process. It is observed on average in a quarter of patients, even when they undergo full-scale treatment 3-6 months after therapy;
- Blockage of the duodenum. It is formed in the case of advanced forms of scar deformities, with the development of an extreme pathological process. Leads to systemic spillage of bile/hydrochloric acid throughout the gastrointestinal tract, requiring hospitalization;
- Bleeding. Caused by a violation of the integrity of the mucous membranes and epithelial structures in the localization of scars. Requires first aid and qualified treatment in a hospital with hospitalization of the patient.
- Secondary manifestations. Dyspeptic disorders that do not disappear for weeks and months, induction of the development of irritable bowel syndrome, and so on.
Prevention
In order not to encounter cicatricial deformation of the intestinal bulb, a person needs to follow preventive measures that are associated with ulcers and peptic ulcers. If it was not possible to avoid these diseases, then the patient needs:
- listen to the doctor's recommendations;
- undergo timely and correct treatment;
- do not break your diet;
- take medication.
In this case, all ulcers will be able to heal safely, and the peptic ulcer will not progress.
https://youtu.be/Nz4ulAx0VVY
Sannikov O. R., endoscopist, Ph.D. FBUZ MSCh No. 41 FMBA of Russia Glazov
The leading role of endoscopy in the diagnosis of ulcerative lesions of the stomach and duodenum (DU) is currently undeniable. However, the capabilities of this method in diagnosing chronic duodenal obstruction (CDO), often concomitant with peptic ulcer disease, are limited [4–6]. At the same time, macroscopic assessment of the condition of the mucous membrane and lumen of the organ, along with other visual signs (the presence of impurities, gaping sphincters) is important for the objective diagnosis of CDN [2, 3, 7].
Preventive actions
As part of basic preventive measures aimed at preventing the development of scar-ulcerative deformation of the duodenal bulb or the progression of the pathological process after healing of the ulcer, it is recommended to perform the following actions:
- Full completion of the rehabilitation period. It includes drug therapy, physiotherapy, and a special regimen;
- Dieting. The adaptive nutrition system must be adhered to on an ongoing basis, until the final disappearance of all signs of pathology, including those confirmed by diagnostic measures;
- Rejection of bad habits. First of all, we are talking about drinking alcohol and smoking;
- Moderate physical activity. If there is deformation of the duodenal bulb, active physical activity is contraindicated, however, light cardio training is acceptable and recommended;
- Regular preventive examinations. Includes a visit to a gastroenterologist, laboratory tests, ultrasound, fluoroscopy, and other procedures as necessary.
Victor Systemov - expert of the 1Travmpunkt site
Cicatricial deformation of the duodenal bulb is formed in the initial section of the intestine. The disease develops after an ulcer in the place where the wounds were. The disease is characterized by the formation of scars, which can change shape and disrupt the functioning of the bulb.
Symptoms of the disease
Cicatricial deformation of the bulb does not have specific symptoms. All body signals are standard, as for any other stomach disease. It is this problem that gets in the way of making a correct diagnosis; doctors often make mistakes here.
- regular nausea, less often vomiting, which does not bring adequate relief;
- subfebrile body temperature of a constant nature;
- dark bloody clots in the vomit, tarry stools;
- hunger pain in the epigastric region;
- heartburn with periodic reflux of stomach contents;
- the appearance of strange taste habits, decreased or increased appetite;
- heart rhythm disturbance.
Subsequently, several lesions form kissing ulcers that partially deform the intestinal wall. This leads to digestive problems, food stagnation and increased symptomatic manifestations.
https://www.youtube.com/watch?v=w8RxI47fXwU
The course of the disease is characterized by periods of exacerbation and remission. The formation of ulcers followed by scar tissue deformation is divided into three stages.
- Exacerbation. Inflammation of the bulb occurs with pronounced symptoms. Ulcerations appear that may bleed.
- Attenuation. There are no signs of the disease, but inflammation remains. Scars begin to form.
- Remission. The inflammatory process is sluggish, but the intestinal walls are still deformed, as a result of which the digestion process is disrupted.
Often, exacerbation makes itself felt in the off-season or during significant nervous shocks. The period of remission is not felt by the patient in any way, even if he does not adhere to the necessary diet and other medical recommendations.
Symptoms:
- The most common and sure symptom of a bulb ulcer is pain in the upper abdomen. Pain sensations can be sharp and burning, aching and piercing.
- The pain can radiate to the back or to the heart area. Such pain usually appears at the time of exacerbation of the ulcer and makes itself felt at night or in moments of hunger, but after eating the pain disappears.
- Sometimes the feeling of hunger haunts the patient even after eating, as a result of which the person suffers from belching, nausea, and vomiting.
- Flatulence and bloating may indicate the presence of a peptic ulcer and show that some organs are deformed.
- If a person suffers from abdominal pain at night, this is a signal of increased acidity in the body, since around two o’clock in the morning the stomach produces the largest amount of it. The disease may occur without any symptoms, which often occurs in older people.
- However, if a bulb ulcer is left unattended, blood may appear during vomiting or during bowel movements. This symptom indicates the onset of internal bleeding, which can be fatal.
The duodenal bulb is deformed as a result of the ulcerative process. This deformation appears directly at the beginning of the section where food enters from the stomach.
The contents of the duodenum in healthy people are alkaline. If a person develops an ulcer, the intestinal mucosa becomes inflamed and the environment becomes acidic. The produced acid riddles the organ with ulcers, after which scars remain on the mucous membrane. They are the ones who deform the bulb, tightening the mucous membrane.
Over time, the duodenal bulb will return to its normal shape, but if exacerbations occur frequently, they will lead to the appearance of more and more scars, which can tighten the passage into the intestines so much that food cannot continue its journey through the gastrointestinal tract, and correct The situation will only be possible through the intervention of a surgeon.
It is possible to stop changes in the structure of the duodenal bulb in similar ways as an ulcerative condition, but to do this you need to know what exact causes led to the disease. Many doctors believe that an incorrect rhythm of life, irregular food intake and junk food can affect the duodenal bulb to a greater extent than the stomach itself. Chronic duodenitis develops, in which the elevated level of gastric acidity remains stable.
The disease is not an ulcer in itself, but a poor diet, constant overexertion and frequent alcohol consumption can quickly lead to an ulcer. It’s enough just to protect yourself from such terrible diseases.
To do this, you need to normalize your daily routine, take care of your proper and timely nutrition, avoid bad habits and allow yourself walks in the fresh air more often. It should be remembered that chronic duodenitis makes itself felt in cold and wet weather, which usually occurs in spring and autumn, so a visit to the doctor and examination will not be superfluous. In addition to the medications recommended by your doctor, it is useful to drink mineral water and devote time to physical exercise.
As healthy foods, the doctor may recommend the patient white bread, vegetable soups without cabbage, boiled meat or fish, cereals, and puddings. It is recommended to take milk, cream, and cottage cheese if the duodenal bulb is deformed. Cheese, omelet and various sweet fruits without peel are allowed to be eaten with duodenitis: oranges, tangerines, tea with lemon. Of course, it is forbidden to consume alcoholic beverages, canned food, fatty ham, smoked and baked goods.
Obviously, nervous overstrain leads to the appearance of an ulcer of the duodenal bulb, so you should take care of the health of your nervous system and try to maintain your own comfortable state. Teas made from various herbs help a lot with this. For example, a mixture of plantain, marsh cudweed, valerian and motherwort, poured with one and a half glasses of boiled water and left for about twelve hours, will not only calm the nerves, but also have a beneficial effect on the condition of the mucous membrane of the duodenum.
Cicatricial ulcerative deformation of the duodenal bulb can be dangerous, especially if the patient does not care about his health and neglects the advice of a doctor. But if the patient completes the course of treatment on time and does not give up the diet and other doctor’s recommendations, the deformed tissue of the duodenal bulb will soon straighten out and the intestines will be able to function normally. Then the patient will not experience unpleasant symptoms. They only bother you when the connective tissue tightens the gap between two organs.
Compensation phase
The patient already has problems with the movement of the food bolus due to the fact that the duodenal bulb is deformed. However, these changes are insignificant; food is delayed for only 6-8 hours. But patients experience a number of unpleasant symptoms:
- there is a feeling of heaviness that bothers you after eating;
- patients complain of nausea and occasional vomiting;
- sour belching bothers you;
- if the patient has inflammation, pain may appear.
Subcompensation phase
If parts of the duodenum are significantly deformed, then the food bolus remains in the stomach much longer, up to 24 hours. This cannot but affect the well-being of patients:
- they are bothered by a constant feeling of heaviness, which appears not only after eating, but lasts all day;
- belching occurs, but with a rotten smell;
- patients have bad breath;
- they are bothered by frequent vomiting, sometimes it happens in the morning, even before the patients have eaten. All eaten food comes out with vomiting, but with signs of fermentation; low-grade fever may appear;
- patients have intoxication and dehydration of the 2nd degree.
Decompensation phase
What is the decompensation phase? In the area of cicatricial deformation, the lumen is completely blocked, and the patient is diagnosed with intestinal obstruction. He also has vomiting, which very early becomes fecal in nature. Patients may experience slight bloating and cramping pain. Intoxication and dehydration of the 3rd degree, dehydration increases rapidly.
Dehydration is the partial dehydration of a patient; his water-electrolyte balance is disturbed. If a patient has a mild degree of dehydration, then he loses only 5-6% of water, with a moderate degree - 5-10%, and with severe - more than 10%. If fluid loss exceeds 20%, the person dies. Therefore, a patient with intestinal obstruction must be urgently taken to a doctor.
If a person undergoes treatment on time, the deformed bulb tissue may straighten out over time. The duodenum will function normally. In this case, there will be no unpleasant symptoms.
Pathology appears only at an advanced stage. Symptoms become especially pronounced when the lumen narrows. The deformation process is characterized by the following features:
- paroxysmal pain in the navel and stomach, hunger pain;
- nausea after eating;
- colic;
- gas formation;
- heartburn with an unpleasant sour taste;
- bad breath (especially if the lumen is very narrowed - fermented food can give a foul odor from the oral cavity);
- coating on the tongue;
- vomiting with blood impurities - when bleeding opens.
Symptoms
The fact that scarring of the ulcer has begun is indicated by a small number of symptoms. The disease is an asymptomatic illness. It can develop over many years and not show any significant signs.
It is almost impossible to find out that the duodenal bulb has begun to deform. During research and identification of repeated attacks of peptic ulcer, in which new scars are formed, a narrowing of the lumen between the intestines and the stomach becomes noticeable.
However, the disease has some significant symptoms that are a bit similar to those of an ulcer:
- nausea before meals, in the morning and on an empty stomach;
- colic;
- flatulence;
- heartburn;
- constant feeling of hunger;
- there may be bleeding.
Why does deformation occur?
If the patient has only the superficial layers of the intestine damaged, that is, erosions form on them, then the healing process occurs without the formation of scars. In patients suffering from ulcers, the wounds are deeper, reaching into the muscle tissue. But if the patient followed all the doctor’s recommendations, the peptic ulcer was well treated, then where the ulcer was, a small linear defect forms, which does not affect the functioning of the intestine.
When the disease was not treated, the patient did not want to follow a diet, and there were many ulcers on the surface, the upper intestine will be covered with connective tissue that appears at the site of the defect, and such tissue is different from what was there before the scar appeared.
The intestines of such a patient change greatly and will never recover. Scars deform the duodenal bulb. The resulting connective tissue begins to tighten this section of the intestine, and it becomes deformed.
Diagnostics
To identify the disease, the doctor prescribes the same examination methods to the patient as for a stomach ulcer. Instrumental methods can help identify affected areas:
- fibrogastroduodenoscopy;
- X-ray of the stomach and duodenum;
- Ultrasound of the stomach.
Additionally, ultrasound of the digestive organs and gallbladder, endoscopic and X-ray examination of the intestines can be performed.
The doctor also resorts to laboratory diagnostic methods. To do this, the patient needs to undergo the following tests:
- blood;
- feces;
- study of hydrochloric acid levels.
Treatment
A peptic ulcer must be treated, especially if it has begun to heal. The disease can affect all organs, the symptoms will become stronger and malignant tumors may form. Doctors prohibit treating duodenal ulcers with any folk remedies. Therapy can only be prescribed by a doctor, which should consist of medications and diet.
Drug therapy is aimed at protecting the duodenal bulb from hydrochloric acid.
During treatment, the patient needs to adhere to the correct diet. The diet excludes the consumption of spicy, fried and fatty foods, ham, smoked meats, yeast products, and canned food. Doctors advise patients to eat:
- White bread;
- vegetables;
- soups without cabbage;
- cooked meat and fish;
- slimy porridge.
In order for the duodenal ulcer to heal, it is also recommended to consume dairy products - natural cream, cottage cheese, cheese. You can cook an omelet. In case of pathology, you can eat sweet fruits without rough peels.
Treatment of the disease
Deformation of the bulb is not an independent disease. After the tissue tightens, after a few years with proper treatment, the bulb will recover and return to its normal size. In the event that ulcers appear constantly in healed areas, the scars will tighten the lumen between the stomach and duodenum more and more.
This will make it very difficult for food from the stomach area to enter the duodenum. In this case, surgery is prescribed. There are no other treatments for this condition. The deformed area must be cut off.
There is no point in treating healed tissue with medications. If the lumen is not very narrowed, then doctors prescribe medications as therapy that will help relieve unpleasant symptoms - pain, heartburn, belching; eliminate the cause of the development of ulcers. Subject to all the rules of treatment and a healthy lifestyle, diet, signs of pathology will eventually cease to bother the person.
Diet is one of the main factors. You should exclude all foods that increase the production of hydrochloric acid. The diet should consist only of healthy foods that have undergone gentle heat treatment. Under no circumstances should you consume alcohol, carbonated drinks, baked goods, spicy foods, fried foods, pickles, marinades and smoked meats. Only in this case will it be possible to prevent negative consequences.
Forecast
If the treatment of a peptic ulcer is successful and correct, then the bulb will not be deformed, and a small scar may form on the organ. Large ulcers can cause tightening of the intestinal walls, which leads to obstruction.
With proper therapy, the healed section of the intestine can return to its original position for several months or a year. If the patient is faced with a severe form of duodenal ulcer, then quick and complete restoration of the organ is impossible.
What can be a health risk for deformation?
As a result of an incorrect lifestyle, various pathologies develop. Erosive and ulcerative changes in the gastrointestinal mucosa are one of them.
If the treatment of a peptic ulcer was carried out correctly, it forms a small scar consisting of connective tissue.
It will not have a negative impact on the activities of the body. Large, multiple, recurring ulcers can cause slight tightening of the intestinal wall or lead to complete obstruction.
As a rule, after months or years, the duodenal bulb returns to its original shape.
But with more severe forms of ulcerative lesions, this is impossible, especially if the patient does not adhere to proper nutrition and does not take medications.
1 - prolapse of a polyp on the leg; 2 - loss of folds of the mucous membrane
Cicatricial deformation of the duodenal bulb leads to disruption of digestive processes in the gastrointestinal tract.
This occurs because in addition to changes in the bulb, the proper functioning of the pylorus of the stomach is disrupted.
Because of this, large volumes of gastric juice are thrown into the intestines, and pancreatic enzymes and bile acids into the gastric cavity.
The consequences of this unnatural process are improper digestion, constipation, diarrhea, discomfort and pain in the abdominal cavity, and bitter belching.
The most serious complication is narrowing of the intestinal lumen by scar tissue, leading to obstruction. In medicine, compensated and decompensated intestinal obstruction are known.
With compensated obstruction, there is a clear narrowing of the intestinal passage, but functions are still possible.
In the case of decompensated intestinal obstruction, the passage of the food bolus is impossible in the required volume, the food stagnates and begins to ferment.
These pathological changes are accompanied by painful sensations in the upper abdomen, a feeling of fullness in the stomach, an unpleasant odor from the mouth, and excessive vomiting of undigested food.
Treatment of scar deformation of the duodenum is possible only with the help of surgery.
After surgery, it is necessary to follow a diet for a long period, strictly follow all the instructions of the attending doctor and not skip taking medications, otherwise massive formation of new scars is possible.