Pain, heartburn, belching, and vomiting can become constant companions for a patient with such a disease as erosion of the stomach and duodenum.
These are conditions in which ulcerations form in the inner lining of these parts of the gastrointestinal tract - open wounds within the mucous membrane.
The course of the erosive process is relatively more favorable than that of the ulcerative process, since with timely treatment and healing, the defects do not lead to the formation of scar changes on the inner wall of the organ.
Causes and mechanisms of the disease
The main etiological factors leading to the occurrence of these pathological changes are:
- Infection with the pathogenic microbe H. pylori;
- Stress factors, psycho-emotional negative situations;
- Taking medications that irritate the internal gastric wall: NSAIDs, salicylates, hormonal agents, digitoxin, reserpine, some gastrotoxic antibiotics;
- Alcohol abuse, eating rough, spicy, hot or too cold food;
- Presence of duodenogastric reflux;
- Chronic diseases of the respiratory system and cardiovascular system, contributing to the development of oxygen starvation throughout the body, including in the gastric wall;
- Venous congestion in liver cirrhosis;
- Exposure to the gastrointestinal tract of salts of heavy metals, acids, alkalis and other occupational hazards;
- Diaphragm hernia;
- Malignant process in the gastroduodenal region.
Under the influence of the above factors, mechanisms for the development of defects and ulcerations of the inner wall of the stomach and duodenum are triggered:
- The production of protective factors decreases: mucus, alkaline pancreatic juice;
- Blood circulation in the gastroduodenal wall slows down;
- The rate of cellular regeneration decreases;
- Aggression factors are activated: HCl, pepsin production increases, and bile is refluxed into the stomach.
Causes
- Helicobacter pylori. The bacterium can penetrate from the lumen of the stomach into the area of the duodenum with chyme; it can damage the mucous membrane, provoking the development of erosive gastroduodenitis.
- Medicines. Long-term, uncontrolled use of steroidal and non-steroidal anti-inflammatory drugs leads to a weakening of the protective properties of the mucous membrane and cell destruction.
- Gastroesophageal reflux disease. Weakness of the gastrointestinal sphincter leads to the fact that chyme constantly moves from the stomach to the intestines, and since the acidity in different parts of the gastrointestinal tract is different, the risk of inflammation increases.
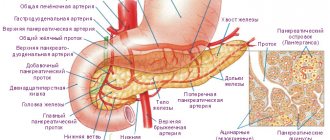
- Pancreatitis or Zollinger-Ellison syndrome (development of a tumor of the pancreas, resulting in increased enzyme production). Since the pancreas produces an increased amount of enzymes, they are capable of damaging the body’s own cells, and the process of self-digestion occurs.
- Smoking. Leads to disruption of the trophism of the gastrointestinal tract, a decrease in the local immune response, and destruction of the mucous protective film of the gastrointestinal tract.
- Nervous overstrain. Stress and depression lead to an increase in stomach acidity, the buffer system that protects the duodenum and creates an alkaline environment in it is depleted, and erosions form.
- Errors in diet. Overeating, consumption of preservatives, spicy, fatty and fried foods, unbalanced with nutrients, increases the load on the gastrointestinal tract.
- Autoimmune diseases. Crohn's disease or ulcerative colitis contributes to the destruction of the gastrointestinal mucosa under the influence of its own immune mechanisms.
- Oncopathology. The development of cancer contributes to the formation of erosions.
Classification of pathological changes
There are some types of pathological defects in the inner wall of the organ. There are erosions:
- Primary;
- Secondary – accompanying the underlying disease;
- Malignant - as one of the symptoms, a manifestation of a malignant process in the gastric lining (cancer, lymphoma);
- Benign.
1. Acute (most often complicated by bleeding, the duration of defects does not exceed seven days)
2. Chronic (existing for a long time and not epithelializing within a month)
Erosions - differences from ulcerative defects
Erosion of the stomach or duodenum is a superficial phenomenon that affects the mucous membranes and does not penetrate into the underlying layers of the organ. Unlike peptic ulcer disease, the layer consisting of muscles in this case is not involved in the pathological process, but this pathological condition is resolved more safely, without forming scars upon completion of the process.
This disease has been less studied compared to ulcers, since making such a diagnosis became possible only with the invention and the beginning of the practical implementation of fiber endoscopes, which make it possible to directly assess the condition of the mucous membranes.
With duodenal erosion, the symptoms may also differ somewhat from those of a peptic ulcer - the signs of the disease are less pronounced, the pain often does not bother patients at all, and the manifestations of chronic posthemorrhagic anemia come to the fore.
Symptoms and treatment of erosion of the stomach and duodenum
This disease manifests itself with unpleasant symptoms that cause significant discomfort to the patient and complicate his life, and can lead to temporary disability.
Patients complain of pain in the epigastric region, which occurs 1-2 hours after eating, of varying intensity: from moderate to severe, unbearable, paroxysmal.
Frequent symptoms are: heartburn, nausea, belching, vomiting, loss of appetite. Patients often deliberately refuse to eat for fear of pain and vomiting.
With long-term erosive defects, patients note pronounced weight loss. When examining the abdominal area and palpation, local pain in the epigastrium is revealed.
The clinical picture and general symptoms of this disease of the gastroduodenal region are very similar to ulcer-like symptoms. And diagnostic examination methods - FGDS - allow you to accurately differentiate these conditions.
About 20% of patients with erosive changes suffer from gastric bleeding (usually with acute mucosal defects). They are complications of the disease and manifest themselves in the form of black stool in the form of pulp (melena), and less often - vomiting mixed with blood (vomiting “coffee grounds”).
Severe bleeding is a life-threatening condition that requires immediate medical attention and hospitalization of the patient in a medical facility.
Hidden bleeding is more often observed in this pathology, which can make itself felt indirectly: general weakness, increased fatigue, pallor of the skin, slowly increasing anemia with low iron content in the body, detection of hidden blood in the stool by special test systems.
Erosive defects are always dangerous by progression and degeneration into an ulcer, the opening of bleeding and a tendency to malignancy. If this pathology has been identified, it is treatable in 100% of cases.
You can’t wait until it “goes away on its own” and delay therapy. A timely visit to a gastroenterologist, fulfillment of all his appointments, and regular medical supervision will allow you to maintain health and allow defects in the inner wall of the gastrointestinal tract to heal without a trace.
A gastroenterologist treats this pathology. The treatment regimen is selected individually, taking into account the severity of the process, the cause that caused the formation of ulcerations, chronic and concomitant diseases, and the characteristics of a particular organism.
Before starting treatment for the patient, the doctor will prescribe a set of diagnostic measures to clarify the diagnosis.
Prevention and prognosis
Erosion of the stomach and intestines, which made itself felt once, requires constant adherence to preventive measures. If you are indifferent to your health, the development of gastrointestinal ulcers will not take long to occur.
You should give up junk food in favor of a healthy and balanced diet. It is better to discuss all medications taken with your doctor, especially if they require long-term use.
If there is a history of erosive bulbitis, the patient needs to reconsider his bad habits, limit the consumption of alcohol and cigarettes.
With the right approach to therapy, the prognosis is favorable. Many manage to achieve stable remission by following all medical recommendations. Ignoring nutritional rules is fraught with the development of ulcers in the very near future.
Laboratory and instrumental diagnostics
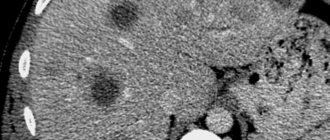
The main method of examination for this disease is FGDS or, as patients call it, a probe. When performing an FGDS, the doctor first macroscopically evaluates the surface defects of the mucous membrane, their size, quantity, and maturity.
Conducts differential diagnosis of defects from ulcers, oncopathology by taking a biopsy and subsequent microscopic examination of the biopsy and smears.
By taking a biopsy, rapid tests can be performed to detect Helicobacter as a causative pathological factor.
In addition to FGDS, the doctor recommends that the patient undergo the following laboratory and instrumental diagnostic methods:
- X-ray examination
Carrying out double contrast using a certain technique makes it possible to identify small round defects with a diameter of up to 3 mm with a small accumulation of radiopaque substance in the center.
- UAC
In the blood, a decrease in the content of red blood cells and hemoglobin, a low color index, hypochromia of red blood cells, and a decrease in iron levels may be observed.
- TANK
In a biochemical analysis, the content of total protein, bilirubin, aminotransferases, urea, creatinine, and iron must be examined.
- Fecal occult blood test
Using special rapid tests, the analysis allows you to identify bleeding without obvious clinical symptoms - hidden.
Nutrition
Nutritional therapy is extremely necessary for patients with diseases of the duodenum. The diet involves eliminating irritating foods, hot dishes, and alcohol.
The diet is based on the following principles:
- maintaining temperature conditions when preparing food;
- fractional meals;
- preference for liquid and soft foods, soups, cereals and purees;
- all dishes are allowed boiled and steamed;
- fried foods, canned foods, salted and smoked foods are excluded;
- a therapeutic diet allows you to drink a little milk or kefir, but only with normal bowel movements.
Foods that can provoke increased secretion of gastric juice are prohibited:
- meat and mushrooms, everything salted, fish broths, seasonings, pickled foods, spices;
- rye and fresh bread, baked goods with yeast;
- sorrel, onions, radishes, cabbage, corn;
- products that increase gas formation and provoke pain: carbonated drinks, strong coffee and tea.
https://youtu.be/XVvp61YQm9c
Principles of treatment for erosive processes in the stomach and duodenum
When the diagnosis is confirmed and the presence of defects in the inner wall of the stomach and duodenum is proven, the doctor will recommend a comprehensive treatment regimen, which will largely depend on the cause of the erosion.
Basic principles of treatment:
1. Etiological therapy
If the reason is contamination with pathogenic Helicobacter, eradication therapy with the use of antibiotics, bismuth salts and proton pump blockers is mandatory.
If the disease has developed as a result of the negative impact of drugs on the inner wall, complete abolition of drugs that irritate the mucous membrane and adherence to a diet will speed up the healing process.
If a patient is diagnosed with chronic diseases of the respiratory system and heart disease, which contribute to the development of hypoxia in the body and deterioration of blood circulation in the gastric wall, it is necessary to treat this pathology.
Normalization of blood gas composition while compensating for respiratory and cardiovascular failure will improve the condition of the gastrointestinal tract and reduce erosive defects.
If erosive processes serve as a symptom of gastrointestinal cancer pathology, consultation with an oncologist and treatment in a specialized hospital, the use of chemotherapy and cytostatics are necessary.
2. Symptomatic therapy
It is aimed at eliminating the symptoms of the disease, relieves pain, reduces the severity of heartburn, eliminates belching and nausea, reduces acidity, and eliminates the manifestations of iron deficiency anemia. Groups of drugs for symptomatic treatment include:
- Antacids (Almagel-Neo, Almagel-A, Maalox, Hefal) - have an enveloping effect
- Proton pump blockers (pantoprazole, omeprazole, omez, nolpaza) – lower pH, eliminate heartburn, belching, dyspeptic symptoms
- Histamine receptor blockers (famotidine, ranitidine) - also act to reduce acidity
- Antispasmodics (no-spa, drotaverine, spasmaton, bellasthesin) are indicated for severe pain syndrome
- Iron preparations (sorbifer, hemofer, ferumlek) are indicated for signs of anemia, symptoms of hidden bleeding
- Enzyme preparations (Creon, Mezim, Festal) - improve digestion processes, are indicated for signs of dyspepsia, concomitant pancreatitis, liver failure
- Reparants (solcoseryl, caleflon, gastrofarm) are drugs that improve regenerative processes in the gastroduodenal mucosa. Allowing the erosive defect to heal faster without any visible scars.
3. Medical nutrition
4. Physiotherapy
When is surgery necessary?
As a rule, the disease can be managed with the help of properly selected medications and diet. However, surgical treatment of duodenal erosion is sometimes necessary. Indications for the procedure are bleeding, which occurs if, as the area of erosion expands, a blood vessel is affected.
In this case, abdominal operations are performed extremely rarely. Typically, access to the intestine is achieved using endoscopic equipment. The doctor cauterizes the damaged vessel (and at the same time the area affected by erosion) with a laser or electrocoagulator.
In no case should you refuse the procedure, since in the absence of therapy, this pathology can easily lead to the appearance of ulcers.
Treatment of duodenal bulb erosion
The duodenum is the initial section of the small intestine, which has an expanded initial part - the bulb. It is this area that most often undergoes erosive changes, most likely due to its closer location to the stomach and its acidic contents.
Symptoms of bulbous defects are similar to gastric erosions; most often, pathology occurs in both parts of the gastrointestinal tract. Patients experience pain 1.5 hours after eating, heartburn, nausea, and vomiting of eaten food may occur.
Treatment of this disease does not differ from the treatment of erosive gastric processes.
Activities are being carried out on:
- Reducing high stomach acidity.
Once in the small intestine, excessively low gastric pH irritates the inner lining of the duodenal bulb, causing inflammation, swelling and hyperemia.
When acidity is normalized, the condition of the mucous membrane of the initial small intestinal section automatically improves.
For this purpose, antacids, omeprazole, pantoprazole, famotidine, and ranitidine are widely used. The drugs are usually prescribed in courses of 1 to 2 months; on the recommendation of a doctor, the period of use can be increased.
- Eradication of Helicobacter pylori infection
When a pathogenic microbe is identified, a three-component scheme is first carried out to destroy it. Including the simultaneous use of 3 drugs: omeprazole, amoxicillin or clarithromycin and metronidazole in appropriate dosages.
If there is no effect from therapy, a 4-component regimen may be recommended, which also recommends taking bismuth subsalicylate (de-nol) as an additional component.
- Normalization of motor skills
Often with erosive problems, reverse duodenogastric reflux and other disturbances of peristalsis and gastrointestinal motility are observed. In order to eliminate them and normalize the passage of the food bolus through the digestive sections, metoclopramide, domperidone, cisapride, and mosax are prescribed.
- Elimination of dyspeptic disorders
Enzyme preparations taken with meals help fight nausea, dyspepsia, and stool disorders: Creon, Mezim, Festal.
- Improving mucosal healing processes
Medicines taken orally or intramuscularly improve the reparative process and accelerate the healing of erosive defects: solcoseryl, caleflon, gastrofarm, retabolil.
Treatment must be comprehensive. Any medication intake must be accompanied by adherence to a diet and diet; only in this case can a positive effect from treatment occur.
Not even the most modern medications can guarantee the healing of erosive defects if the patient eats provoking foods that worsen the course of the disease.
Traditional medicine recipes
Folk remedies are used in consultation with a doctor.
Recommended:
- sea buckthorn oil in capsules three times a day before meals (not recommended for diseases of the liver or biliary tract);
- herbal mixture of yarrow, chamomile, mint, St. John's wort flowers and sage leaves in equal parts. Brew a teaspoon per glass of hot water and drink 150 grams before meals;
- a mixture of carrot juice and raw chicken yolks, half a glass 2 times a day before meals;
- chamomile infusion at the rate of 1 teaspoon (or sachet) of the product per cup of very hot water.
For treatment, a decoction of nettles (a tablespoon per glass of water) and a decoction of oat grains (in the same ratio) are also used. The decoctions are filtered, mixed and drunk ½ cup 30 minutes before each meal.
Diet and nutrition for erosion of the stomach and duodenum
Both in the acute period and during the healing stage of mucous defects, the patient should beware of provoking foods that cause increased production of hydrochloric acid and irritate the inner lining of the digestive tract.
Such products include:
- Spices
- Spices
- Smoked meats
- Fast food
- Canned food
- fried food
- Grilled products
- Animal fats
- Chocolate
- Garlic
- Strong coffee, tea
- Carbonated drinks
- Alcohol
In case of severe symptoms of exacerbation of the disease, a gentle diet is prescribed with the consumption of lean boiled meat, stewed vegetables, and mucous porridges.
The following products are allowed:
- White stale bread
- Milk soups
- Lean meats and fish
- Omelettes
- Puddings
- Skim cheese
- Mashed potatoes
- Kissel
- Milk if well tolerated
You need to eat in small portions, but often (5-6 times a day). Frequent meals in small quantities prevent duodenogastric reflux.
At the stage of healing of erosive processes, the patient can be transferred to his normal, habitual diet with the exception of acute foods that irritate the mucous membrane and provoking foods.
Juice products that are thermally processed by frying in a frying pan are contraindicated for this pathology, even in remission. It is better to give preference to culinary processing by baking in its own juice, boiling, stewing.
The diet for erosive changes should contain a sufficient amount of protein, since it is this that forms the basis for the regeneration of the inner wall of the digestive tract.
Treatment
Pathology therapy must be comprehensive. It includes diet, medication and, if necessary, surgical correction.
We recommend reading:
Ileocecal valve (Bauhinian valve): concept, location, structure and functions
Diet
The diet for erosive gastritis should be as gentle as possible for the stomach and intestines. Basic principles:
- Thermally processed food. All dishes must be cooked: boiled, steamed or baked.
- Dishes are served cold or warm. During the period of bleeding, preference is given to cold liquid foods, which promote reflex vasoconstriction and reduce bleeding. Hot food can cause bleeding by dilating blood vessels.
- Shredded food. Helps facilitate digestion. Preferably ground through a sieve, crushed in a blender, through a meat grinder.
| Recommended Products | Not Recommended Products |
|
|
Drugs
- Antacids (Almagel, Phosphalugel). Promote the formation of a protective film on the mucous membrane of the stomach and duodenum and reduce further damage.
- Proton pump or H2-histamine receptor inhibitors. Helps reduce the acidity of gastric juice and reduce its damaging effect on the intestinal mucosa.
- Antibacterial agents. In the presence of infectious inflammation (Helicobacter infection).
- Hemostatic agents. In case of severe bleeding, aminocaproic acid is used locally; drugs such as Etamsylate and Dicinone act systemically.
- Asymptomatic therapy. Correction of vitamin deficiencies, pain syndrome (with antispasmodics) and so on is carried out.
Surgery
Used in case of severe bleeding. Very rarely, they resort to removing part of the intestine or stomach - only with extensive defects.
The most commonly used local treatment is cauterization of the erosive area during fibrogastroduodenoscopy. The minimally invasive technique is effective and allows you to quickly stop bleeding and speed up regenerative processes.
Traditional methods
The main purpose of folk methods is to protect the mucous membrane from the effects of physical or chemical damaging factors and saturate the body with useful substances. These actions allow you to activate regeneration and speed up the healing process.
We recommend reading:
Sphincter of Oddi: characteristics and diseases of the anatomical structure
Use:
- natural oils: sea buckthorn, linseed, olive;
- fish fat;
- potato broth.
Complications
Sometimes this disease is complicated by massive bleeding. In this case, the stool becomes black. At the same time, coffee-colored vomit appears. The release of blood is dangerous due to the development of acute anemia.
Erosion can develop into an ulcer. The progression of the ulcer is fraught with its perforation. Perforation of the ulcer causes inflammation of the peritoneum - peritonitis . This disease can only be treated surgically, and the clock literally counts.
Finally, untreated erosion can develop into cancer.
The main symptoms that may indicate the appearance of intestinal erosion
Symptoms, like the underlying causes, can occur individually or together. The main manifestations of the disease include:
- frequent constipation;
- discomfort or pain of varying intensity in the middle and lower abdomen;
- bloating, excessive gas formation, flatulence;
- loss of appetite, sudden weight loss;
- in the later stages of the disease, intestinal bleeding of varying intensity may be observed.
Intestinal or stomach bleeding is the first sign, after which you should immediately consult a doctor. These symptoms are manifestations of quite serious diseases. To avoid more severe consequences, it is necessary to immediately identify the underlying cause and begin treatment.
Etiology of the disease
Erosion of the rectum is caused by an inflammatory reaction in the upper layer of the mucous membrane, which can be triggered by a number of reasons:
- Causes of an infectious nature: intestinal pathogens - chlamydia, campylobacter, herpes virus, streptococci, staphylococci, E. coli; syphilis; tuberculosis; gonorrheal proctitis; parasitic pathogens - worms, dysentery, balantidiasis.
- Mechanical damage: surgical treatment of other diseases, passage of swallowed solid objects, anal fissure, trauma during childbirth.
- Unhealthy diet: spicy foods, seasonings and spices, excessive alcohol consumption.
- Pathologies of the digestive system, leading to the entry of poorly processed food into the rectum, causing chronic constipation or diarrhea; inflammation of the gallbladder; gastritis and stomach ulcers; intestinal dysbiosis.
- Endocrine diseases: hepatitis, cirrhosis, pancreatitis.
- Hemopathies: impaired blood flow, diseases leading to blood stagnation, hemorrhoids, varicose veins, thrombophlebitis, heart failure, venous insufficiency with excessive periods of sitting.
- Malignant neoplasms in the rectum, metastases.
- Radiation damage, incl. during radiation therapy.
- Toxic poisoning: the most common is poisoning with lead or other heavy metals.
- Autoimmune causes: Crohn's disease, autoimmune inflammation of the colon.
- Indirect factors: nervous stress, hypothermia, diseases of the genital organs.
Types of diagnostics
Even the most qualified doctor will not be able to make such a diagnosis without conducting a series of examinations. In order to choose the right treatment, it is necessary, first of all, to make a correct diagnosis, which may be indicated by characteristic symptoms.
The main diagnostic methods for identifying intestinal erosion:
- stool examination;
- X-ray of the intestines (in which the intestines are filled with some kind of contrast agent);
- fibrogastroduodenoscopy (endoscopic examination, during which it is possible to examine up to 1 meter of the small intestine);
- sigmoidoscopy (a more detailed examination of the intestinal walls up to 30 centimeters long).