Anaphylactic shock is a generalized reaction of the body to an allergen. The pathology is accompanied by impaired circulation, which leads to the development of oxygen starvation and multiple organ failure. If medical care is not provided in a timely manner, there is a high risk of death.
Pathophysiology
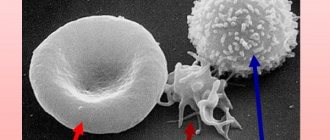
Anaphylactic shock is a type I allergic reaction. Upon repeated contact of a sensitized organism with an allergen, the latter binds to tissue mast cells (MCs) fixed on the surface and circulating basophils IgE - At.
MCs are located predominantly in the submucosal layer and skin near blood vessels. Interaction between IgE and allergen on the surface of inflammatory mediators, including histamine.
Histamine released from mast cells leads to the inclusion of a complex of reactions, the final stage of which is the release of diverse mast cells, acts on H1 and H2 receptors of target organs: smooth muscle, secretory cells, nerve endings, which leads to dilation and increased vascular permeability, bronchospasm, hyperproduction of mucus .
Prostaglandins, leukotrienes and other biologically active substances synthesized upon activation of mast cells cause similar changes.
An increase in the concentration of histamine and other allergy mediators in the blood serum leads to the dilation of small-caliber vessels, an increase in the permeability of the vascular wall, and the release of the liquid part of the blood into the tissues.
Histamine causes spasm of the pre- and post-capillary sphincters, and the pre-capillary sphincters quickly relax, and an additional volume of blood enters the capillary zone, leading to the release of fluid into the tissue. The capacity of the vascular bed sharply increases and the volume of circulating blood decreases.
A decrease in vascular tone leads to a sharp drop in vascular resistance, which results in a decrease in blood pressure - “peripheral vascular collapse”.
A decrease in blood pressure leads to a decrease in venous return of blood to the heart, and, consequently, the stroke volume of the heart decreases. The minute volume of the heart is initially compensated by tachycardia, then also decreases.
A drop in blood pressure leads to disruption of blood flow in vital organs (heart, kidneys, brain, etc.), and the release of pressor hormones decreases. Thus, the mechanism of blood pressure drop in AS differs from other types of shock.
The peculiarities of AS are that in other types of shock, when the volume of blood volume decreases, adrenaline is released, causing vasospasm, an increase in PVR and maintenance of blood pressure; in AS, a similar compensatory mechanism does not work due to the development of acute peripheral vascular collapse.
Clinical syndromes:
- acute cardiovascular failure:
- hypotension.
Acute respiratory failure:
- diffuse spasm of bronchial smooth muscles;
- acute swelling of the mucous membrane;
- pulmonary edema.
Gastrointestinal tract:
- pain syndrome;
- involuntary defecation;
- intestinal bleeding.
Genitourinary system:
- spasm of the smooth muscles of the uterus (miscarriage in pregnant women);
- involuntary urination.
Central nervous system:
- convulsions;
- disturbance of consciousness;
- cerebral edema.
Who is at risk?
No one is immune from the development of anaphylaxis. It can start in anyone, but there are still those people for whom the risk of getting anaphylactic shock is much higher than others. These include people with a history of asthma (including bronchial asthma), eczema, urticaria, dermatitis, and allergic rhinitis.
Patients with mastocytosis are prone to similar allergic reactions. This is a disease in which there is a pathological proliferation of mast cells (immune cells of connective tissue) and their accumulation in tissues and bone marrow.
It is almost impossible to predict the possibility of developing anaphylactic shock. He is dangerous because of surprise. If a person has previously had anaphylactic shock, he must always have with him a card indicating the clinical picture of the shock he suffered, indicating allergens, and the results of the latest allergy tests.
You should pay attention to your well-being when taking previously untried medications, consuming unfamiliar and exotic food, visiting arboretums with unfamiliar flowering plants, and exercise caution when walking in nature, avoiding contact with insects, spiders and reptiles.
Tags: Anaphylactic shock
Anaphylactoid shock
The release of biologically active substances (BAS) from mast cells and basophils can occur without the participation of IgE-Abs. Some drugs and food products have a direct pharmacological effect on MCs, releasing mediators (histamine liberators), or activate the complement system with the formation of anaphylatoxins C 3a and C 5a.
Such reactions are called anaphylactoid, they develop under the influence of iodine-containing X-ray contrast agents, amphotericin-B, sodium thiopental, chloramphenicol, sulfabromophthalein, sodium dihydrochlorate, opiates, dextran: vancomycin, some muscle relaxants, consumption of certain foods (nuts, oysters, crabs, strawberries, etc. .).
The clinical manifestations of anaphylactic and anaphylactoid shock are identical.
Symptoms
Clinical signs depend on the severity of the disease. When allergens enter the body, the symptoms of anaphylactic shock appear in several periods. At the initial stage, it is characterized by skin manifestations (itching, urticaria), a drop in blood pressure, nausea, headache, increased heart rate, and a slight tingling sensation in the muscles. During the height of the pathogenesis of an anaphylactic reaction, the symptoms worsen. Numbness of the limbs leads to convulsions, nausea progresses to vomiting. Due to Quincke's edema, the patient is at risk of breathing problems.
Poor circulation is especially dangerous. In severe cases, this can lead to cerebral edema, which can result in a stroke. The period of ridding the body of an anaphylactic reaction lasts several days, depending on the severity of the case. At this time, you need to try to protect yourself from possible reintroduction of the allergen.
- Hemodez - instructions for use, composition, release form, indications, side effects, analogues and price
- ADSM vaccination for adults - reactions and complications. When and where do adults get the ADSM vaccine?
- Anti-Rhesus immunoglobulin - instructions for use and indications, release form and price
Causes of anaphylactic shock
The development of AS can be caused by various substances, usually of a protein or protein-polysaccharide nature, as well as haptens - low-molecular compounds that acquire their allergenicity after binding the hapten itself or one of its metabolites to host proteins.
The time for the appearance of clinical signs of AS depends on the method of introducing the allergen into the body: with intravenous administration, the reaction can develop within 10-15 seconds, intramuscular - after 1-2 minutes, orally - after 20-30 minutes.
The most common cause of anaphylactic shock is drugs . Among the causes of LAS, according to our observations, NSAIDs came to the fore, and in 62% of cases the cause was metamizole sodium. Second and third places are occupied by local anesthetics and antibiotics.
LAS was most often caused by amide anesthetics (64%). In every third patient, novocaine was the cause of LAS. It should be noted that there are cross-reactions between novocaine and other local anesthetics - para-aminobenzoic acid esters.
There were no cross-reactions observed between the above-mentioned group of local anesthetics and amide derivatives, as well as between drugs within the group of amide local anesthetics. It is noteworthy that LAS developed, in particular, after the use of applications with lidocaine by a dentist, and topical application of gel with lidocaine by a cosmetologist.
Among antibacterial drugs, β-lactam antibiotics continue to play a leading role as a cause of LAS. According to statistics, on average, for every 7.5 million penicillin injections, there is 1 case of anaphylactic shock with a fatal outcome. Most often, LAS was caused by natural and semisynthetic penicillins (93% of LAS due to β-lactam antibiotics) and less frequently by cephalosporins.
It should be borne in mind that more than 30% of patients allergic to penicillin have cross-reactions with cephalosporins. LAS developed not only after intramuscular and oral use of antibiotics, but also when using eye drops with antibiotics, and performing an intradermal test with lincomycin.
Next in importance are nitrofuran derivatives, vaccines and serums (PSS, COCAB and hepatitis B vaccine), plasma expanders and enzymes.
Others (20%): isolated cases of the development of LAS on no-shpu, biseptol, sodium thiosulfate, vitamin B6, nicotinic acid, cordarone, afobazole, etc. In every sixth patient, the role of the drug in the development of LAS was obvious, but it was not possible to establish the cause possible due to the fact that the patient was taking two, three or more medications at once.
Previously, manifestations of drug allergies were observed in almost every second patient with LAS (46%). It is important to note that when prescribing medications, medical workers do not always collect allergic and pharmacological anamnesis, re-prescribe drugs, including combination drugs, which previously caused an allergic reaction in the form of urticaria, Quincke's edema and even anaphylactic shock, in every third patient with LAS (32%).
Taking into account the above, it is necessary to emphasize the need for rational use of drugs, avoid polypharmacy, remember the interaction of various pharmacological groups, and carefully collect allergological and pharmacological anamnesis by doctors of all specialties.
Hymenoptera insect stings are the second cause of anaphylactic shock after drugs.
AS due to hymenoptera stings are characterized by a more severe course, since, as a rule, they develop at a sufficient distance from medical institutions, and therefore first medical aid is provided in most cases untimely. The cause of allergic reactions is the poison that enters the body when stung. AS most often developed from wasp stings.
Food products and nutritional supplements. Most often, AS is associated with the consumption of fish, crustaceans, nuts, dairy products, and egg whites. The antigenicity of food products may be reduced during cooking.
The cause of AS may be seeds, halva, milk thistle and other products of plant origin that give cross-reactions in patients with hay fever. The development of AS can be triggered by the consumption of certain foods (celery, shrimp, apples, buckwheat, nuts, chicken) after physical activity.
Severe anaphylactic reactions can be caused by papain contained in some canned meats, as well as sulfites (sulfite, bisulfite, potassium and sodium metabisulfite).
Emergency medical care
The above-described first aid measures primarily include monitoring the victim’s condition and basic life support measures.
It should be understood that anaphylactic shock in any case must be treated with medication. It is advisable to do this under the supervision of a medical specialist, however, in case of critical situations, it is possible to carry out independent therapy using appropriate medications and the necessary procedures.
Algorithm for providing emergency care for anaphylactic shock:
- Use of adrenaline. It is administered by injection or intramuscularly, in critical situations through clothing into the middle part of the thigh on the outside or deltoid muscle. Adult dosage – 0.1 percent solution of 0.4-0.5 ml. Children's dosage – identical concentration of 0.1-0.3 ml. If there is no effect, the injection is repeated every 10-15 minutes depending on the condition of the victim.
In case of severe conditions associated with anaphylactic shock, intravenous drip administration of 1 ml of solution at a dosage of 30 drops/minute, diluted in 400 ml of isotonic saline, is recommended.If intravenous injection is not possible, the corresponding procedure is performed directly into the trachea;
- Hormonal agents. Intramuscular administration of dexamethasone. For severe atrophic shock - 20 mg once, then 3 mg/kg body weight in portions throughout the day;
- Antihistamines. As an emergency measure, a combination of tavegil, suprastin and diphenhydramine. As an adjuvant - oral administration of loratadine, ranitidine, cetirizine or suprastin;
- Airway dilators. Used in situations where an acute and severe allergic reaction causes bronchospasm and breathing problems. The most effective are aminophylline intravenously up to 10 ml one-time, salbutamol in the form of an aerosol using inhalation administration.
Clinical picture of anaphylactic shock
There are five clinical types of AS:
- Typical form.
- Hemodynamic option.
- Asphyxial option.
- Cerebral option.
- Abdominal option.
Typical shape
The leading symptom of this form of AS is hypotension due to the development of acute peripheral vascular collapse, which is usually accompanied by acute respiratory failure caused by laryngeal edema or bronchospasm.
An acute state of discomfort arises, patients complain of severe weakness, a feeling of tingling and itching of the skin of the face, hands, head, a feeling of a rush of blood to the head, face, tongue, a feeling of a nettle burn. A state of internal anxiety arises, a feeling of impending danger, fear of death.
Patients are concerned about heaviness behind the sternum or a feeling of compression of the chest, difficulty breathing, nausea, vomiting, sharp cough, pain in the heart, dizziness or headaches of varying intensity. Sometimes I have abdominal pain. The typical form is often accompanied by loss of consciousness.
Objective picture : skin hyperemia or pallor, cyanosis, possible urticaria and Quincke's edema, severe sweating. Characteristic is the development of clonic convulsions of the limbs, and sometimes full-blown convulsive seizures, motor restlessness, involuntary acts of urination and defecation.
The pupils are dilated and do not respond to light. Thread-like pulse, tachycardia (less often bradycardia), arrhythmia. Heart sounds are muffled, hypotension. Breathing disorders (shortness of breath, difficulty breathing frequently with wheezing, foam at the mouth). Auscultation: large bubbling wet and dry rales. Due to pronounced swelling of the mucous membrane of the tracheobronchial tree, total bronchospasm, respiratory sounds may be absent until the picture of a “silent lung”.
The typical form of AS is characterized by the following main features:
- arterial hypotension;
- respiratory failure;
- disturbance of consciousness;
- skin vegetative-vascular reactions;
- convulsive syndrome.
The typical form of AS occurred in 53% of cases.
Hemodynamic variant
In the clinical picture, the symptoms of impaired cardiovascular activity come first: severe pain in the heart area, a significant decrease in blood pressure, dullness of tones, weak pulse and its disappearance, cardiac arrhythmia up to asystole.
Spasm of peripheral vessels (pallor) or their expansion (generalized “flaming” hyperemia), dysfunction of microcirculation (marbling of the skin, cyanosis) are observed. Signs of decompensation of external respiration and the central nervous system are much less pronounced.
Acute heart failure is the leading pathological syndrome in the hemodynamic variant of AS. The hemodynamic variant of AS occurred in 30% of cases and, with correct timely diagnosis and intensive therapy, ends favorably.
Asphyxial variant
The clinical picture is dominated by acute respiratory failure caused by swelling of the mucous membrane of the larynx, with partial or complete closure of its lumen or bronchospasm, up to complete obstruction of the bronchioles, interstitial or alveolar edema of the lung with a significant disruption of gas exchange.
In the initial period or with a mild favorable course of this variant of AS, signs of decompensation of hemodynamics and central nervous system function usually do not appear, but they can appear secondarily during a protracted course of AS. The severity and prognosis are mainly determined by the degree of respiratory failure.
Chronic pulmonary pathology (chronic bronchitis, bronchial asthma, pneumonia, pneumosclerosis, bronchiectasis, etc.) predisposes to the development of the asphyxial variant of AS. This form of AS occurred in 17% of cases.
Cerebral variant
The clinical picture is characterized mainly by changes in the central nervous system with symptoms of psychomotor agitation, fear, impaired consciousness, convulsions, and respiratory arrhythmia. In severe cases, symptoms of cerebral edema and epistatus occur, followed by respiratory and cardiac arrest.
Some patients experience symptoms characteristic of acute cerebrovascular accident: sudden loss of consciousness, convulsions, stiffness of the neck muscles, making diagnosis difficult.
Convulsive manifestations (twitching of individual muscles, hyperkinesis, local convulsions) can be observed both at the beginning of the clinical picture and in subsequent stages of AS, after the activity of the respiratory and cardiovascular systems has improved. Disturbances of consciousness are not always deep, more often confusion and stupor.
Abdominal option
The appearance of symptoms of an acute abdomen (sharp pain in the epigastric region, signs of peritoneal irritation) is typical, which often leads to erroneous diagnoses: perforated ulcer, intestinal obstruction, pancreatitis. Sharp pain in the heart area can lead to an erroneous diagnosis of “acute myocardial infarction.”
Other symptoms typical of AS are less pronounced and not life-threatening. Mild disturbances of consciousness and a slight decrease in blood pressure are observed. Abdominal pain syndrome usually occurs within 20-30 minutes. after the first symptoms of AS appear.
Symptoms of an acute allergic reaction
Both local and systemic reactions, including acute ones, can be observed. Typical signs:
- Itching and rashes on the skin, as well as mucous membranes;
- Swelling in the face, neck, limbs and genitals;
- Disruption of the respiratory system with the rapid development of swelling of the throat, cough, difficulty breathing, hoarseness, mucous discharge from the nasal cavity;
- Cardiovascular pathologies. In particular – a drop in blood pressure, chest pain, increased heart rate;
- Disruption of the central nervous system. From headache, weakness and subjective feeling of fear and loss of consciousness and convulsions;
- Dyspeptic disorders. These include abdominal pain, intestinal cramps, nausea, vomiting, diarrhea and impaired swallowing reflex.
Types of anaphylactic shock
- Acute malignant.
- Acute benign.
- Lingering.
- Recurrent.
- Abortive.
- Lightning fast.
Acute malignant course of AS is more often observed in the typical variant. Characterized by an acute onset, a rapid drop in blood pressure (diastolic blood pressure often drops to 0), impaired consciousness, and an increase in symptoms of respiratory failure with bronchospasm. The symptoms of AS progresses, despite intensive anti-shock therapy, up to the development of severe pulmonary edema, a persistent decrease in blood pressure and a deep coma. High probability of death.
The acute benign course of AS is characterized by a favorable outcome with correct, timely diagnosis of AS and emergency, complete treatment. Despite the severity of all the main clinical manifestations of AS, the emerging symptoms are not characterized by progression and respond well to reverse development under the influence of anti-shock measures.
Protracted and recurrent course of AS. Initial signs develop rapidly with typical clinical syndromes, and a protracted course appears only after active anti-shock therapy, which gives a temporary and partial effect.
In a recurrent course, after normalization of blood pressure and recovery of the patient from shock, a drop in blood pressure is again observed. Subsequently, the clinical symptoms are not so acute, but are characterized by a certain resistance to therapy. It is more often observed when taking long-acting drugs (bicillin, for example).
Abortive course - anaphylactic shock quickly stops, often without medications. This variant of AS occurs in patients receiving antishock drugs. Thus, in one of the patients we observed, a second AS due to a wasp sting developed while taking prednisolone for maintenance treatment of bronchial asthma. The clinical picture of AS was not pronounced, in contrast to the first episode of AS, when the patient did not receive prednisolone.
Lightning shock is the rapid development of AS during the first seconds, most often with intravenous infusions.
Emergency care standard and nurse action algorithm
As part of the provision of emergency qualified medical care, the nurse is obliged to use the appropriate drugs from the standard anti-shock kit in the first aid kit, having also carried out the necessary preparatory actions. The classic scheme of the standard of emergency medical care for anaphylactic shock:
- Stopping the entry of the allergen into the body and applying cold to the problem location;
- Monitoring the current state, in particular breathing, blood circulation, consciousness, airway patency with a parallel call to a resuscitation team or ambulance;
- Administration of epinephrine according to the attached instructions, taking into account the patient’s age. To carry out the procedure, a 0.1 percent solution of adrenaline is used.
- The use of glucocorticosteroids and antihistamines as an adjunct to drug therapy;
- Ensuring complete rest for the victim, moving him horizontally with slightly raised legs;
- Carrying out tracheal intubation or conicotomy in the presence of severe swelling of the larynx or pharynx, which does not make it possible to ensure full breathing;
- Performing chest compressions and artificial respiration in the absence of such vital signs until the arrival of the resuscitation team.
Factors that increase the severity of AS
- The patient has bronchial asthma.
- Concomitant diseases of the cardiovascular system.
- Concomitant therapy: beta-blockers; MAO inhibitors; ACE inhibitors.
With the development of AS in patients with bronchial asthma or patients receiving treatment with beta-blockers, on the one hand, the reaction of the respiratory tract to biologically active substances released during AS increases, on the other hand, the influence of pharmacological drugs (adrenaline) used during resuscitation measures for AS decreases.
Particular caution should be exercised when prescribing beta-blockers to patients receiving SIT with allergens and patients with a history of idiopathic anaphylaxis. Difficulties in elimination from CABG may occur in patients receiving beta-blocker therapy for concomitant diseases of the cardiovascular system and glaucoma.
Before prescribing an “anaphylactogenic” drug to a patient receiving beta-blockers, consideration should be given to adjusting the concomitant treatment (replacing beta-blockers with calcium antagonists or other antihypertensive drugs).
ACE inhibitors - can cause swelling of the tongue and pharynx with the development of life-threatening asphyxia, “Capoten cough”.
MAO inhibitors - can enhance the side effects of adrenaline by inhibiting the enzyme that breaks it down.
Systemic reactions are more often observed when administering SIT to patients with uncontrolled asthma, therefore it is necessary to determine FEV1 before prescribing SIT and during treatment with allergens and cancel injections if FEV1 is less than 70% of the expected value.
Providing emergency care in a dental office
As part of the implementation of dental measures, after using a number of medications that cause severe reactions such as acute cardiovascular or adrenal insufficiency, a specialized specialist is obliged not only to identify the problem, correctly assessing the clinical manifestation, but also to provide the patient with possible pre-medical care.
As part of emergency care for anaphylactic shock, the algorithm of actions is as follows:
- Immediately stop using the drug that caused the reaction;
- Lay the victim horizontally with his back down and raise his lower limbs;
- With a rapid increase in blood pressure, adrenaline should be injected subcutaneously from 0.5 to 1 ml, diluted in 5 ml of saline. You can puncture both the site of introduction of the allergen, and directly inject the corresponding agent into the trachea, observing safety precautions;
- As a supplement, if there is no increase in blood pressure, glucose and saline are administered. It is also rational to use prednisolone at a dose of 5 mg/kg body weight;
- In the presence of airway obstruction, oxygen therapy with aminophylline is performed at a rate of 10 milliliters intravenously. If no improvement in breathing is observed, then endotracheal intubation is necessary;
- Waiting for the medical team to arrive and, if necessary, performing manual resuscitation aimed at restoring heartbeat and breathing.
Treatment of anaphylactic shock
- Relief of acute circulatory and respiratory disorders.
- Compensation for the resulting adrenocortical insufficiency.
- Neutralization and inhibition of the AG-AT reaction in the blood of biologically active substances.
- Blocking the entry of the allergen into the bloodstream.
- Maintaining vital functions of the body or resuscitation in a serious condition (clinical death).
The drug of choice in the treatment of AS is adrenaline (INN - epinephrine). Timely and early administration of epinephrine can prevent the development of more severe symptoms. All activities must be carried out clearly, quickly and persistently; the success of therapy depends on this. Mandatory anti-shock therapeutic measures:
- carried out at the site of AS occurrence;
- drugs are administered intramuscularly so as not to waste time searching for veins;
- if AS occurs during intravenous drip administration of medication, then the needle is left in the vein and medications are administered through it.
- stop administering the drug that caused AS.
- lay the patient down, placing his legs in an elevated position, turn his head to the side to prevent tongue retraction and asphyxia. Remove removable dentures.
Adrenaline is administered in a dose of 0.3-0.5 ml of 0.1% solution intramuscularly; if necessary, injections are repeated after 15-20 minutes until blood pressure normalizes.
Prick the injection site of the drug (or the sting site) with a 0.1% solution of adrenaline, diluted 1:10, at 5-6 points. If a bee stings, remove the sting. A venous tourniquet is applied to the limb above the lesion site, loosened for 1-2 minutes. every 10 minutes.
Administer prednisolone at a rate of 1-2 mg/kg body weight or hydrocortisone (100-300 mg) or dexamethasone (4-20 mg).
Suprastin 2% - 2-4 ml or diphenhydramine 1% - 1-2 ml or tavegil 0.1% - 2 ml is administered intramuscularly. It is undesirable to administer phenothiazine antihistamines.
For bronchospasm - 2.4% aminophylline solution - 5.0-10.0 ml or β2-adrenergic agonists by inhalation (salbutamol, ventolin, berotec). If there is cyanosis, dyspnea, or wheezing, provide oxygen supply.
For heart failure, cardiac glycosides are administered, diuretics are administered for signs of pulmonary edema.
In case of severe convulsive syndrome, a 0.5% solution of seduxen is administered - 2-4 ml.
When taking the drug orally, the stomach is washed out. If the medicine is dripped into the nose or eyes, it is necessary to rinse them with running water and drip a 0.1% solution of adrenaline and a 1% solution of hydrocortisone.
Intensive therapy for AS
If there is no effect from mandatory anti-shock measures, intensive anti-shock therapy is carried out in the intensive care unit or in a specialized department.
Intravenous access is provided and medications are administered IV. Drop or stream 1-2 ml of 1% mezatone in a 5% glucose solution.
Pressor amines: dopamine 400 mg (2 ampoules) in 5% glucose, continue infusion until systolic blood pressure reaches 90 mmHg, then titrate.
In case of asphyxia, bronchodilators are administered: 2.4% solution of aminophylline 10.0.
Prednisolone is administered intravenously at the rate of 1-5 mg/kg body weight, or dexamethasone 12-20 mg, or hydrocortisone 125-500 mg in saline solution.
The dose of diuretics and cardiac glycosides is determined based on the patient’s condition. For convulsions, 2-4 ml of 0.5% seduxen is administered.
For patients in whom AS has developed while taking β-blockers, glucagon is administered 1-5 ml intravenously as a bolus, then titrated at a rate of 5-15 mcg per minute. Glucagon - has a direct positive inotropic effect (increases MOS and SV). 1 bottle contains 1 mg (1 ml).
For bradycardia, atropine is administered 0.3-0.5 mg subcutaneously every 10 minutes, maximum 2 mg.
In case of severe hemodynamic disorders, infusion therapy is carried out, the volume of which is determined by the state of hemodynamics (isotonic sodium chloride solution up to 1-1.5 l, plasma expanders).
All patients who have undergone AS (including the abortive form) must be hospitalized. After stopping the acute reaction, it is necessary to monitor patients for 2 weeks, since late complications may develop: allergic myocarditis, glomerulonephritis, intestinal bleeding.
Therefore, the following indicators are examined over time: general blood and urine analysis, ECG, feces for the Gregersen reaction, urea, blood creatinine. Patients continue to take oral glucocorticosteroids 15-20 mg with a decrease over the course of a week until complete withdrawal, as well as oral antihistamines.
Severity
There is the following classification:
- Stage 1 is characterized by pressure below normal by 30-40 mmHg (normal pressure ranges from 120-110/90-70 mmHg). The person is excited and may develop a panic attack. The reaction appears within 30 minutes or longer. Therefore, there is a high chance that first aid for anaphylactic shock will be effective when a person is just anticipating the onset of an attack;
- Grade 2 – symptoms develop from 10-15 minutes to 30 minutes. The pressure drops to 90-60/40 mm Hg, loss of consciousness is possible. Also, since there is a reserve of time, there is a good chance of emergency assistance;
- 3rd degree. Anaphylaxis develops within a few minutes, the patient may faint, systolic pressure is in the range of 60-30 mmHg, diastolic pressure is usually not determined. The chances of successful treatment are low.
- 4th degree. It is also called fulminant (fulminant) shock. Develops in a few seconds. The person immediately faints; the pressure cannot be determined. The chances of resuscitation are almost zero. Fortunately, grade 4 is extremely rare.
Measures to reduce the risk of developing AS
Careful collection of allergy history, information about drug intolerance, pharmacological history and recording in medical documentation. For patients with a history of allergic reactions, medications should be administered after testing. Prescribing medications taking into account their tolerability and cross-reactions.
Assessment of pharmacotherapy currently received by the patient for concomitant diseases. Whenever possible, preference is given to oral forms of drugs over parenteral administration.
Mandatory observation of the patient for 30 minutes after the administration of any, primarily, potentially allergenic injection drug, including allergens during SIT. Exclusion of immunotherapy for uncontrolled asthma.
The presence of information with patients that will allow, even if they are in an unconscious state, to obtain information about their allergic disease (in the form of a bracelet, necklace, card).
A patient with a high risk of accidental exposure to a known allergen, as well as a patient with idiopathic anaphylaxis, must have an emergency kit, including:
- adrenaline solution for emergency administration;
- first generation oral antihistamines;
- tourniquet
Measures to reduce the risk of insect stings
- During the summer months, go outside in clothes that cover your body as much as possible. Choose light-colored clothing and avoid bright fabrics, as they attract insects.
- When an insect appears nearby, do not make sudden movements or wave your arms.
- Don't walk barefoot on the grass.
- When outdoors, wear a hat, as insects can get tangled in your hair.
- When going outdoors, do not use strong-smelling cosmetics: perfumes, deodorants, hairsprays, etc.
- It is recommended to have insecticides in the kitchen in the summer.
- Avoid visiting places where garbage accumulates, especially garbage containers in yards, as insects are attracted to food products and smells.
- Use caution when preparing and eating food outdoors.
- Avoid the use of propolis and drugs containing it (apilak, propoceum, proposol, propomizol and others).
R. S. Fassakhov, I. D. Reshetnikova, G. S. Voitsekhovich, L. V. Makarova, N. A. Gorshunova
2009
Causes
The hell of allergy manifestations from an anaphylactic reaction of the body can occur from contact with specific allergens that are found in medications and food products. Insect bites and contact with certain animals and plants are dangerous. With the advent of new antibiotics and drugs on the market, doctors have noted negative reactions of the body to some medications. The highest risk groups are injections of penicillin, administration of contrast solutions and painkillers. Food allergies are often caused by the following foods:
- nuts;
- citrus;
- seafood;
- food additives and flavorings.
Consequences and complications
After recovery from allergic shock, some symptoms may persist. Common consequences:
- headache, it occurs due to cerebral hypoxia;
- nausea and vomiting;
- muscle pain, shortness of breath;
- lethargy, decreased reactions;
- discomfort in the heart region due to ischemia of the heart muscle.
Sometimes concomitant diseases occur against the background of a previous allergy. Repeated exposure to irritants should not be allowed, since complications of the drug and other forms develop bronchial asthma, hepatitis, myocarditis, and diffuse damage to the nervous system. 10-15 days after the allergy, cases of recurrent swelling or hives occur.
Diagnostics
The picture of an anaphylactic illness requires rapid emergency treatment to avoid severe manifestations of immune reactions. It is important to quickly identify the disease. Often, the algorithm of actions provides for the need for an urgent diagnosis, administration of medications and assistance. To confirm, the following diagnostic methods are used:
- complete blood count (red blood cells, leukocytes, eosinophils);
- biochemical research;
- X-ray of the lungs;
- allergy tests to identify specific antibodies.
Etiology
Anaphylactic shock is often caused by drugs, insect bites, and foods. Rarely, it occurs upon contact with latex and during physical activity. In some cases, the cause of anaphylactic shock cannot be determined. Possible causes of this condition are listed in the table:
| Cause | Number of patients | % |
| Medicines | 40 | 34 |
| Insect bites | 28 | 24 |
| Products | 22 | 18 |
| Exercise stress | 10 | 8 |
| Latex | 9 | 8 |
| SIT (specific immunotherapy) | 1 | 1 |
| Cause unknown | 8 | 7 |
| Total | 118 | 100 |
Anaphylactic shock can be caused by any medication. It is most often caused by antibiotics, anti-inflammatories, hormones, serums, vaccines and chemotherapy. Among food products, common causes are nuts, fish and dairy products, and eggs.
Emergency first aid
Parents need to know how to provide emergency care for anaphylactic shock in children. The algorithm of actions is as follows:
- Place the injured child on any hard surface with his legs elevated. For example, you can put it on the floor and put a bag or folded clothes under your feet.
- Call an ambulance.
- If the baby is vomiting, then the head should be turned to the side so that the vomit does not get into the throat.
- Open windows and doors if the victim is indoors. Remove excess clothing.
- Remove the allergen. In case of an insect bite (wasp, bee), i.e., quickly remove the sting and apply ice. If you have a food allergy, rinse your stomach.
- Check the wrist or carotid artery for a pulse.
- Check your breathing by holding a mirror to your mouth.
- Perform an indirect massage if there is no heartbeat or breathing. If there is a pulse, it is contraindicated.
First aid for anaphylaxis
Therapy should be started immediately when the first signs of anaphylactic shock are detected!
But first of all, call an ambulance and be sure to tell the dispatcher that the child is showing signs of anaphylaxis.
Before the doctor arrives:
- lay the baby horizontally and raise the legs;
- provide fresh air access to the room;
- give the victim either his usual anti-allergy drug or whatever is on hand;
- if you have it in your medicine cabinet, give an injection of adrenaline or dexamethasone/prednisolone;
- if there is no pulsation in the carotid arteries, begin artificial heart massage;
- If the baby is not breathing, start performing artificial respiration.
Try to find out the cause of the allergic reaction, find out from the victim what preceded it. This is necessary in order to stop exposure to the allergen as much as possible.
If a reaction occurs to a sting, for example, of a wasp, it is necessary to disinfect the area with an antiseptic, cool it and apply a tourniquet above the bite site.
And don't panic under any circumstances! Now the life and health of the child depend on the clarity and speed of your actions.
Prevention
It is possible to prevent an anaphylactic reaction by reducing the risk of contact with irritants. To do this, limit the consumption of foods that cause allergies. If primary symptoms are detected and it is impossible to independently identify the irritant, they undergo special tests that help determine it. To prevent drug allergies, the attending physician should examine the previous medical history before prescribing therapy. Tests must be carried out before administering medications to risk groups.
Treatment in hospital
A patient with anaphylactic shock is assisted by resuscitators in the intensive care unit. If the airway is obstructed, an endotracheal tube is inserted into the trachea to provide oxygen access. In critical cases with tracheal spasm, a tracheotomy (dissection of the tracheal rings) is performed.
For further treatment of anaphylactic shock, the following types of drugs are used:
- Adrenaline solution. Administered intravenously using droppers, constantly monitoring the pressure. The product has a complex effect, normalizes blood pressure, and eliminates pulmonary spasm. Adrenaline suppresses the release of antibodies into the blood.
- Glucocorticosteroids (dexamethasone, prednisolone). They inhibit the development of immune reactions and reduce the intensity of the inflammatory process.
- Antihistamines (claritin, tavegil, suprastin). First they are administered by injection, then switched to tablets. These drugs suppress the action of free histamine, which blocks the effects it produces. Antihistamines should be administered after blood pressure has normalized, as they can lower it.
- If the patient has developed respiratory failure, he is administered methylxanthines (caffeine, theobromine, theophylline). These drugs have a pronounced antispasmodic effect, relax smooth muscles, reduce bronchospasm,
- To eliminate vascular insufficiency, crystalloid and colloid solutions (ringer, gelofusin, riopolyglucin) are administered. They improve blood microcirculation and reduce its viscosity.
- Diuretic (diuretic) drugs (furosemide, minnitol) are used to prevent pulmonary and cerebral edema.
- Tranquilizers (Relanium, Seduxen) are used for severe convulsive syndrome. They eliminate feelings of anxiety and fear, relax muscles, and normalize the functioning of the autonomic nervous system.
- Local hormonal drugs (prednisolone ointment, hydrocortisone). They are used for skin manifestations of allergies.
- Absorbable ointments (heparin, troxevasin). Used to dissolve cones at bite sites.
- Inhalation of humidified oxygen to normalize lung function and eliminate symptoms of hypoxia.
Treatment in the hospital lasts 8-10 days, then the patient is monitored to prevent complications.
What is anaphylaxis
Anaphylaxis (anaphylactic shock) is an immediate allergic reaction, which is expressed in a sharp increase in the body’s sensitivity to both a reintroduced allergen and a substance that first entered the body. The reaction develops at a speed from a few seconds to a couple of hours.
The concept was first defined at the beginning of the 20th century by the Russian scientist A.M. Bezredka. and the French immunologist Charles Richet, the latter receiving a Nobel Prize for his discovery.
The severity of anaphylaxis is not affected by either the route of entry of the allergen or its dose. Shock can develop from a minimal amount of a medicine or product.
Most often, anaphylaxis manifests itself as a reaction to drugs, in which case the fatal outcome is 15-20%. Due to the increase in the number of people suffering from food allergies, there has been an increase in the number of cases of anaphylaxis in recent years.
How does pathology develop?
The body's reaction to anaphylaxis goes through three successive stages:
- immunological reaction;
- pathochemical reaction;
- pathophysiological reaction.
Immune cells come into contact with allergens, releasing antibodies (GE Ig). Due to the effects of antibodies, the body releases histamine, heparin and other inflammatory factors. These inflammatory mediators spread throughout all organs and tissues. As a result, blood thickening occurs and its circulation is disrupted.
First, the peripheral, then the central circulation is disrupted. As a result of poor blood flow to the brain, hypoxia occurs. The blood clots, heart failure develops, and the heart stops.
What should be in a first aid kit in case of anaphylactic shock?
All medical institutions must stock first aid kits to provide emergency medical care. In accordance with the standards developed by the Ministry of Health, the first aid kit for anaphylactic shock should include the following drugs and consumables:
- 0.1% adrenaline solution 10 ampoules of 1 ml;
- 0.9% sodium chloride solution – 2 containers of 400 ml each;
- Reopoliglucin - 2 bottles of 400 ml;
- Prednisolone – 10 ampoules of 30 mg;
- Diphenhydramine 1% - 10 ampoules of 1 ml;
- Eufillin 2.4% - 10 ampoules of 5 ml;
- Medical alcohol 70% - 30 ml bottle;
- Disposable sterile syringes with a capacity of 2 ml and 10 ml - 10 pieces each;
- Systems for intravenous infusions (droppers) – 2 pieces;
- Peripheral catheter for intravenous infusions – 1 piece;
- Sterile medical cotton wool - 1 pack;
- Tourniquet – 1 piece
The first aid kit must be supplied with instructions.
Kinds
Allergic shock develops at different rates. Symptoms can occur gradually or in a matter of seconds. Variants of anaphylactic manifestations:
- Protracted – proceeds more slowly than the acute type develops. For example, when injecting long-acting drugs. The presence of this form of development of the disease requires long-term observation of the patient by a doctor.
- The fulminant type is marked by acute respiratory and vascular failure. The first clinical manifestations require emergency care. Acute allergic reactions are dangerous with a sharp course, which leads to loss of consciousness and Quincke's edema. Even an adult may not have time to understand what is happening to him.
- Abortive development, in contrast to the relief of acute allergic diseases, is easy to treat and poses fewer health risks.
- The recurrent type is characterized by the resumption of manifestations of allergic shock. This occurs due to the substance being reintroduced into the body without the patient's knowledge.
Diagnostic methods
It is very important to identify this disease as early as possible - the prognosis for a person’s life directly depends on this.
Symptoms of anaphylactic shock resemble those of many other diseases.
Therefore, the main factor for determining an accurate diagnosis is the correct collection of anamnesis.
In addition, the following studies are being conducted:
- General blood analysis. In anaphylactic shock, a decrease in the number of red blood cells, an increase in leukocytes and an increase in eosinophils are detected.
- Blood chemistry. In this case, liver enzymes and kidney tests increase.
- Plain radiography of the chest. This study shows interstitial pulmonary edema.
- Linked immunosorbent assay. This procedure allows you to detect specific antibodies - immunoglobulins E and G.
To determine the provoking factor, the patient may need to consult an allergist, who will prescribe special tests.
However, they must be carried out as carefully as possible to prevent the body from overreacting.
The safest method is the radioallergen sorbent test. Using this radioimmunological technique, it is possible to identify the allergen without interfering with the patient’s body.
During this procedure, the interaction of human blood with allergenic substances is analyzed.
When a large number of antibodies are released after the next injection, we can talk about the detection of a provoking factor.