Abnormal bowel movements and black stool due to stomach ulcers
Black feces with a stomach ulcer may be accompanied by vomiting with blood, but it may also be without it.
Usually melena #8212; a sign of a duodenal ulcer, but it also occurs when bleeding from a stomach ulcer occurs relatively slowly. Melena is often observed 12 hours after the onset of blood loss. With massive blood loss due to an ulcer, black feces have a tarry appearance, since a large number of blood breakdown products quickly move through the intestines. If the blood loss is small, black stool with an ulcer has a more formal appearance. Sometimes with constipation, melena appears only on the third day. Often constipation due to stomach ulcers occurs with a strict diet low in fiber-rich foods. Such constipation is considered nutritional. Poor motor skills are worsened if patients have an exacerbation and are forced to stay in bed for a long time. In addition, constipation is caused by a reflex effect on the colon, as well as an increase in the tone of the vagus nerve. The condition is aggravated by constitutional weakness of the press, as well as taking medications (Almagel, Calcium Carbonate). During an exacerbation, sometimes constipation is tolerated worse than pain and comes first.
Diarrhea in most cases can be of a medicinal nature associated with the use of magnesia. In other patients, diarrhea is not a typical symptom of mucosal ulceration. During an exacerbation, half of the patients experience constipation and other dyspeptic symptoms. With blood loss, a change in stool color may be accompanied by fainting and weakness. If blood loss is more than a liter, patients may go into shock. In this case, the severity of the condition is assessed not only by the amount of blood lost, but also by the rate of bleeding. Hidden blood loss leads to multiple organ disorders, the development of azotemia, and subsequently intoxication.
Interesting materials on this topic!
Sauces have long been used in cooking to improve and diversify the taste.
The causes of the development of the most common stomach disease, chronic gastritis, are primarily.
If 25 years ago the main method of treating ulcers was surgery, then p.
Comments from readers of the article Chair
Leave a review or comment
Add a comment Cancel reply
PANCREATITIS
TYPES OF PANCREATITIS
WHO HAPPENS?
NUTRITION BASICS
ATTENTION! THE INFORMATION PUBLISHED ON THE SITE IS FOR INFORMATIONAL NATURE ONLY AND IS NOT A RECOMMENDATION FOR USE. NECESSARILY
CONSULT YOUR DOCTOR!
End-stage symptoms
This stage is characterized by a worsening of all external and internal signs of liver cirrhosis:
- The level of bilirubin increases with the progression of liver cirrhosis, which is manifested by severe jaundice of the skin.
- Edema worsens due to a progressive decrease in albumin in the blood.
- The number of platelets decreases, which leads to bleeding, and white blood cells, which can manifest as persistent infections.
- At this stage, the liver may shrink as its tissue is replaced by fibrous tissue.
- Intestinal dysfunction often leads to the proliferation of pathological flora.
- Development of complications:
- Ascites is an accumulation of fluid in the abdominal cavity. Prescribing diuretics does not bring relief, and puncture of the abdominal cavity in order to remove ascitic fluid has to be done constantly.
- Hepatic encephalopathy is a disorder of the brain, manifested in deterioration of memory, consciousness, and intellectual activity. This complication is due to the fact that bilirubin has a pronounced toxic effect on the brain and is able to penetrate the blood-brain barrier - a kind of protection of the brain from the action of many toxic substances.
- Portal hypertension is an increase in pressure in the portal vein of the liver, which leads to activation of bypass venous vessels - collaterals. The load on these vessels is so great that they begin to dilate. This happens with the veins of the esophagus and the veins of the rectum, from which poorly controlled bleeding can develop. A characteristic picture is formed by collaterals visible on the anterior abdominal wall; the symptom is called “Medusa’s head”.
Feces and urine in liver cirrhosis
The changes also affect physiological waste, that is, feces and urine, which can change their color, which is associated with a violation of the conversion and exchange of bilirubin.
Urine becomes darker, sometimes compared to the color of dark beer, and the color of feces with cirrhosis, on the contrary, becomes light.
Why is urine yellow and stool brown?
- In the small intestine, bilirubin, which enters there from the gallbladder, is converted into urobilin, which is excreted from the body in urine and gives it a yellow color.
- Stercobilin is formed in the large intestine, which turns stool brown.
With liver pathology, the formation of stercobilin is disrupted, which leads to discoloration of feces, and an increase in the amount of urobilin, as evidenced by dark urine.
Abnormal bowel movements and black stool due to stomach ulcers
Black feces with a stomach ulcer may be accompanied by vomiting with blood, but it may also be without it. Usually melena #8212; a sign of a duodenal ulcer, but it also occurs when bleeding from a stomach ulcer occurs relatively slowly. Melena is often observed 12 hours after the onset of blood loss. With massive blood loss due to an ulcer, black feces have a tarry appearance, since a large number of blood breakdown products quickly move through the intestines. If the blood loss is small, black stool with an ulcer has a more formal appearance. Sometimes with constipation, melena appears only on the third day.
Often constipation due to stomach ulcers occurs with a strict diet low in fiber-rich foods. Such constipation is considered nutritional. Poor motor skills are worsened if patients have an exacerbation and are forced to stay in bed for a long time. In addition, constipation is caused by a reflex effect on the colon, as well as an increase in the tone of the vagus nerve. The condition is aggravated by constitutional weakness of the press, as well as taking medications (Almagel, Calcium Carbonate). During an exacerbation, sometimes constipation is tolerated worse than pain and comes first.
Change in appearance of stool
Changes in the appearance of stool may indicate that there is cancer or another pathological process in the intestines. With constipation it becomes denser, with diarrhea it becomes mushy and liquid. If the cancer partially blocks the lumen of the intestine, the stool becomes pencil thin (“ribbon stool”). In addition to cancer and benign tumors of the intestine, this symptom can be caused by diseases such as hemorrhoids, irritable bowel syndrome, colitis, and parasites.
Change in stool color
With bowel cancer, the stool may become black, resemble tar in appearance, and have an unpleasant odor. This type of stool is called melena, and it looks like this because the blood is exposed to digestive juices in the stomach and intestines. Thus, melena can be a manifestation of cancer of the esophagus, stomach, and small intestine.
In order for the stool to darken and acquire a tarry appearance, at least 500 ml of blood must enter the intestines. If such a symptom occurs, you should immediately consult a doctor!
If bleeding in the digestive tract is suspected, which does not manifest itself in a change in the appearance of stool (so-called occult bleeding), a stool test for occult blood is prescribed. The most common type of test is the benzidine test (Gregersen reaction) . This laboratory diagnostic method plays an important role in detecting cancer and some other diseases; it is indicated in the following cases:
- Prolonged constipation, diarrhea, mushy stool.
- Stomach ache.
- False urge to defecate.
- Unexplained loss of appetite, weight.
- If cancer is detected during a colonoscopy (endoscopic examination of the colon).
- If during FEGDS (endoscopic examination of the esophagus, stomach, duodenum) tumors or ulcers are detected.
The fecal occult blood test is a very sensitive test. It can show positive results for nosebleeds and bleeding gums. This must be taken into account and the results of the analysis must be evaluated in combination with other diagnostic methods.
Bleeding from the rectum, blood in the stool
If the source of bleeding is in the lower intestines, the patient may experience the following symptoms:
- traces of blood on toilet paper;
- traces of blood on underwear, sheets;
- streaks of blood in the stool;
- bleeding from the rectum.
If you notice traces of blood on toilet paper more than twice, blood in your stool, or bright scarlet blood coming out of your rectum, you should consult a doctor immediately.
Prevention and early diagnosis of colon cancer
If the patient experiences stool changes, he is referred to a coloproctologist. During the appointment, the doctor finds out what symptoms bother the patient, for how long, what he was sick with during his life, and whether there are any intestinal pathologies in close relatives. Then a digital examination of the rectum is performed.
In order to detect cancer and other intestinal pathologies, the following studies are used:
- Proctoscopy and colonoscopy are endoscopic examinations of the rectum and colon. These diagnostic methods allow you to visualize cancer, polyps and other pathological changes.
- A biopsy is a test that can be done during an endoscopy. Using a special instrument, the doctor obtains a fragment of the pathologically altered area of the intestinal mucosa and sends it to the laboratory, where examination is carried out under a microscope. If malignant cells are found, it is cancer.
- Fecal occult blood test.
- Complete blood count - helps identify anemia due to bleeding.
- If colon cancer has already been diagnosed, a biochemical blood test is prescribed to assess liver function, since there may be cancer metastases in it.
- Blood test for tumor markers: carcinoembryonic antigen (CEA) and CA 19-9 . This study is not very informative in diagnosing cancer, as it can produce false-positive and false-negative results. Tests for tumor markers are used as part of a comprehensive examination to monitor the effectiveness of treatment and detect relapse.
- Once colorectal cancer is diagnosed, CT scans, ultrasounds, MRIs, angiography, chest x-rays, and PET scans are performed to assess its spread and determine its stage.
Screening tests help diagnose cancer before changes in stool occur. Colonoscopy is used as the main type of screening. It is recommended for all people over 50 years of age. At the European Clinic, this study is performed by experienced doctors using modern equipment. To ensure that the patient does not experience any unpleasant sensations during the procedure, our doctors immerse him in a state of light anesthesia - “medicated sleep.”
Stomach pain
Ulcers occur on the lining of the stomach, and for this reason the most common symptom of their development is pain in the abdominal area. It is usually felt between the lower chest and the navel. It can be both dull and sharp. When gastric juice enters damaged areas of the stomach, the pain is felt more strongly. Depending on the severity of the disease, pain can last from several minutes to several hours. As a rule, it worsens at night or on an empty stomach. However, an ulcer does not always cause pain, especially in the early stages of its development.
Stage and grade of stomach cancer
The most common classification of cancer is based on the stages and degrees of tumor spread throughout the body.
Stage 1A is diagnosed if the cancerous tumor is located within the gastric mucosa and the lymph nodes are not affected.
Stage 1B:
- The cancer is still within the lining of the stomach, but one or two lymph nodes have already been involved.
- This stage also includes cancer that grows into the muscle layer of the stomach wall, if the lymph nodes are not affected.
Stage 2A:
- The cancer is confined to the gastric mucosa, but has also affected 3-6 lymph nodes.
- The cancer has spread to the muscle layer of the stomach wall and to 1-2 lymph nodes.
- The lymph nodes are not affected, but the cancer has spread to the outer lining of the stomach.
Stage 2B:
- Cancer of the stomach lining, but has also affected seven or more lymph nodes.
- The cancer has spread to the muscle layer of the stomach wall and to 3–6 lymph nodes.
- The cancer has spread to the outer lining of the stomach and to 1 or 2 lymph nodes.
- The lymph nodes are not affected, but the cancer has spread beyond the stomach.
Stage 3A:
- The cancer has spread to the muscle layer of the stomach wall and to 7 or more lymph nodes.
- The cancer has spread to the outer lining of the stomach and to 3–6 lymph nodes.
- The cancer has spread beyond the stomach and to 1 or 2 lymph nodes.
Stage 3B:
- The cancer has spread to the outer lining of the stomach and to 7 or more lymph nodes.
- The cancer has spread beyond the stomach and to 3–6 lymph nodes.
- The cancer has spread beyond the stomach to surrounding tissue and possibly to one or two lymph nodes.
Stage 3C. Cancer has spread beyond the outer lining of the stomach to surrounding tissues and organs and to 3 or more lymph nodes.
Stage 4: The cancer has spread to another organ, such as the liver or lungs.
In most cases, stomach cancer is diagnosed at the third or fourth stage, when complete cure is usually no longer possible.
There are 3 degrees of malignancy of stomach cancer:
- low - the tumor grows slowly;
- medium - cancer with a high rate of spread;
- high - aggressive cancer that grows very quickly.
Vomiting blood
The formation of ulcers on the gastric mucosa is often accompanied by vomiting. If during it a person feels acute pain in the abdomen and notices particles of blood in the vomit, then this may be a sure sign of the active development of a stomach ulcer. This symptom should not be missed. Sometimes with an ulcer, the vomit looks like a viscous, brown-brown thick substance. This is a sign that the integrity of the blood vessels in the stomach is compromised and urgent treatment is necessary. Vomiting blood indicates wounds on the mucous membrane.
Bloody and purulent impurities in the stool
When blood and pus appear in the stool, tar-black stools are observed. Sometimes it has a green tint. In addition, a person experiences the following symptoms:
- constant nausea;
- frequent fainting;
- bloody vomiting - the discharge looks like coffee grounds.
If there is a perforation of the ulcer, in addition to bloody stool, the person experiences severe pain in the right side. In addition, there is a risk of increased heart rate, fainting, and cold sweating.
Omborrhoids may occur against the background of the disease
Dark color of stool
Blood from stomach ulcers also affects the color of the stool. The onset of a peptic ulcer may be indicated by a darkish tint of stool and its unusual viscous consistency. In such cases, it is important to promptly seek medical help. If there is bleeding in the stomach, the stool will gradually turn from light yellow, brown to black. Changes in the color and consistency of stool occur due to a chemical reaction between gastric juice and hemoglobin in the intestines. Sometimes there may be blood clots in the stool.
Black stool: main causes
The reason for the formation of a dark, almost black color of the stool can be certain foods (beets, pomegranate, prunes, black currants, blueberries, blood sausage) or medications (iron and bismuth preparations, activated carbon). But usually stools with a change in color occur over the next 1-2 days, then returning to their usual color.
If the diet has not changed, and no medications, multivitamins, or nutritional supplements have been taken, the appearance of black stool is an alarming sign, especially if it is tarry, thin, or accompanied by weakness and malaise. Similar to bright scarlet color, black stool indicates diseases and pathologies leading to gastrointestinal bleeding.
Heartburn
Heartburn is nothing more than a symptom of acid reflux, and it may well be associated with a stomach ulcer. If the burning sensation in the esophagus goes away immediately after drinking water, then this should not cause much concern. But constant discomfort in the stomach may well indicate a peptic ulcer. In this case, heartburn appears immediately after eating and is often accompanied by hiccups. If it causes great discomfort, it is important to seek medical help.
What can be called constipation?
Each person has his own rhythm of defecation - bowel movements. Some people do this every day and at the “classic” time - in the morning, while others have bowel movements every few days. The rate of formation and volume of feces expelled primarily depends on the mass of dietary fiber consumed.
For meat-eating Europeans, the standard is indicated as 200 grams daily, for Africans - 450 grams twice a day, but this is similar to the “average temperature in the hospital.” Having a bowel movement every third day cannot be considered abnormal unless it causes suffering.
There are 7 criteria for true constipation and at least two must be present simultaneously:
- Rarity of defecation
- The need for prolonged straining to expel stool
- Hard stool like “nuts” or with dense fragments
- Unpleasant feeling of incomplete emptying
- Feeling of obstruction in the rectum
- The need to “pick out”, which is scientifically called “manipulation”
- Defecation less than three times a week.
To make a diagnosis, the specific Rome criteria require that symptoms occur in every fourth bowel movement and last longer than 3 months.
Fast weight loss with ulcers
Many people with stomach ulcers experience unexplained weight loss. This occurs due to a sharp loss of appetite, abdominal pain, and gag reflexes - frequent companions of this disease. Even when eating the usual amount of food, patients will still lose weight. Unexplained and sudden weight loss may indicate many other health problems. In any case, this phenomenon cannot be ignored.
Causes of stool lightening
When an adult’s stool suddenly turns light, questions arise. There are fairly harmless reasons for stool becoming discolored:
- Eating cottage cheese, sour cream, milk and other fermented milk products (fecal matter will be yellow, light yellow or white).
- If the stool is yellow, this may be a consequence of eating melons, bananas, pears and apples, pumpkins and other yellow-orange foods.
- The stool may be light yellow due to the use of antibacterial and anti-inflammatory drugs.
- If a woman’s stool turns lighter, this is due to taking oral contraceptives.
- Drinking large amounts of alcohol can cause stool to become light, pale, or completely white.
- The rapid speed at which feces move through the intestinal tract means that the feces do not have time to color properly, and then light-colored poop comes out of the adult’s body.
Any of the above reasons for lightening the stool of an adult is not a big cause for concern, especially if such a sign as light or colorless stool is a one-time occurrence. You will only need to worry if pale yellow, sandy, or light green stool bothers an adult for more than a week in a row, and there are additional symptoms of improper functioning of the digestive tract.
E. Malysheva’s recipe for constipation
My dears, it is not expensive pills that will help you normalize digestion and stool, and relieve constipation, but a simple folk, long-forgotten recipe. Write down quickly, brew 1 tbsp. spoon.
Intolerance to fatty foods
Most often, this symptom is associated with gallstones. But difficulties with digesting fatty foods can also be a sign of peptic ulcer disease. This is caused by visceral sensitization - an increased degree of sensitivity of the damaged mucosa. In such cases, there is often an ulcer of the pyloric canal. Intolerance to foods rich in fat is often accompanied by nausea and bloating.
People suffering from peptic ulcers should avoid consuming foods with high fat content. After all, they increase the production of gastric juices and negatively affect the stomach tissue. In addition, it is advisable to avoid drinks containing caffeine, alcohol and gases. It is best to completely switch to a healthy diet and proper drinking regimen, which will have a positive effect on the healing of the stomach.
Constipation in colon cancer
Transverse colon carcinoma, by its very presence, affects intestinal function, changing its peristalsis. As a rule, patients complain of discomfort, bloating and alternating constipation with loose stools.
A dangerous complication of the disease is intestinal obstruction due to partial and then complete blocking of the lumen of the intestinal tube by the tumor.
Patients suffering from carcinoma do not pay attention to the abnormality of the bowel movement, considering it a natural symptom of the disease. Nevertheless, episodes of stool retention in combination with difficult passage of gases with a “drum” abdomen and increasing abdominal pain are evidence of increasing obstruction, which is still compensated.
A three-day absence of stool with no passage of intestinal gases with a progressive deterioration of the condition is a reason for an urgent visit to an oncologist with suspicion of subcompensation of intestinal function. These manifestations for more than three days with an increasingly worsening condition, an increase in symptoms of intoxication, severe pain and vomiting, most likely indicate a complete blockage of the intestinal lumen. The consequences are fatal if you skip urgent medical attention.
One of the most important signs of rectal carcinoma is uneven stool, either constipation or diarrhea, with dissatisfaction with the act due to seemingly incomplete emptying.
The rectum is a well-extensible ampoule, the capacity of the tube is very impressive and reaches 20 cm in the largest diameter. Therefore, obstruction is an infrequent manifestation of the disease, but constipation will be caused by dyssynergism of the muscles involved in the cancerous conglomerate and metastases to the lymph nodes along the neurovascular bundles.
Insufficiency of secretion production by glandular cells with inflammation accompanying the tumor and post-radiation changes add to the chances of stool compaction.
Loss of appetite
At the initial stage of peptic ulcer disease, a sharp cooling of interest in food is often observed. This is often associated with sudden and severe pain in the stomach. As a rule, pain after eating causes fear and aversion to eating. Therefore, people prefer not to eat anything to avoid subsequent discomfort. A loss of appetite can lead to weakness and fatigue, which can negatively affect your overall health. If you lose your appetite for no apparent reason, you should immediately consult a doctor for advice.
If at least one of the symptoms described above appears, you need to make an appointment with your doctor. It is very important to respond to the problem in a timely manner, otherwise the disease will be difficult to treat and will cause a lot of unpleasant consequences.
Appearance with cirrhosis of the liver
Yellow skin color
At the initial stage of the disease, not everyone can notice any changes, but the further the disease develops, the more obvious the change in skin color will become. The first to change their natural shade are the eye sclera, palms and soles of the feet. Only in the last stages will the whole body change color completely.
Thin, sickly face and body
With liver diseases, a person often notices a significant decrease in body weight and a noticeable deterioration in health, but understands the seriousness of the situation only when it becomes critical and the disease becomes incurable.
Bright lips, palms and mucous membranes
If your lips and tongue turn red and look like they are varnished, you should think twice and rush to the doctor. Despite the fact that this sign may clearly indicate that the patient has cirrhosis of the liver, it is also characteristic of a number of other diseases (lichen planus, candidiasis of the oral mucosa).
Another sign that indirectly indicates the development of the disease in the body is hepatic palm syndrome (palmar erythema).
If you discover this alarming symptom, you should urgently contact a specialist who, after a detailed interview, will definitely prescribe the necessary tests:
- thorough examination of the inner surface of the hands;
- general and detailed blood and urine tests;
- Ultrasound and X-ray;
- MRI and CT;
- biopsy.
Unhealthy dry skin
Dry skin in people with liver cirrhosis is associated with a fairly large number of factors, one of which is hormonal imbalance syndrome. This can only be combated symptomatically - by moisturizing and nourishing the skin with special ointments and creams. The effect of such treatment will not last long, so satisfactory skin condition must be constantly maintained.
Redness of cheekbones
During the course of the disease, the skin of the entire body acquires a jaundiced tint, but malar erythema is clearly visible on the face.
Significant enlargement of the abdomen with ascites
One of the clear signs indicating progressive cirrhosis is ascites.
Fluid accumulates in the abdominal cavity, which leads to various kinds of unpleasant consequences. Ascites does not appear immediately; the initial volumes of fluid are quite small. The disease then progresses according to the following scenario:
- the volume of the abdomen increases sharply (the skin becomes stretched, the vessels are clearly visible through it, and when a blow to the abdomen occurs, a vibration effect occurs);
- the stomach continues to grow, the patient feels strong pressure in the epigastric region;
- the lungs are compressed, which impairs respiratory functions;
- serious problems arise with the digestive system, since the organs of the gastrointestinal tract are subjected to severe compression;
- possible inflammatory processes in the genitourinary system;
- lower limbs swell;
- the navel protrudes and a large umbilical hernia forms.
Treatment before and after surgery
This malignant cancer originates from the epithelium of the rectum.
This tumor has the characteristic features of any malignant formation - rapid growth, invasion of neighboring tissues, metastasis. Men and women are equally susceptible to the disease. An increase in the number of cases is observed from the age of 45, and the peak incidence occurs among 75-year-olds.
The type of tumor is determined by its location:
- Anorectal location is typical for 5-8% of cases.
- Ampullary occurs more often than others, up to 80%. This is a pathology in the widest part of the intestine.
- Supraampullary localization in up to 12% of patients.
The nature of tumor growth can be:
- exophytic – grows into the intestinal lumen;
- endophytic - grows through the thickness of the wall, infiltrates it, and can cover it circularly;
- mixed growth.
According to the histological picture, the neoplasm can be:
- glandular cancer (adenocarcinoma);
- solid;
- signet ring cell;
- skirr;
- squamous.
Discussing rectal problems is something shameful for many people. Therefore, the first signs of pathology often remain without due attention. The initial symptoms of rectal cancer are changes in stool character. Frequent changes in constipation and diarrhea appear, and the shape of stool changes. It becomes much thinner than before. The feeling of incomplete defecation, discomfort, and increased formation of gases are disturbing.
The development of the tumor process causes long-term signs of rectal cancer:
- mucus and blood in stool;
- purulent discharge;
- feeling of fullness in the intestines;
- bloating;
- pain in the rectal area;
- chronic fatigue, fatigue;
- anemia;
- weight loss.
In the initial stages, there may be no manifestations of the disease. If anemia of unknown origin is detected, it is worth looking for the cause of hidden bleeding. Perhaps it's cancer.
Late stages are characterized by damage to other organs:
- germination into neighboring organs, formation of interorgan fistulas;
- purulent-inflammatory processes – paraproctitis, pelvic phlegmon;
- perforation of a tumor of supramullary localization with the development of peritonitis;
- bleeding.
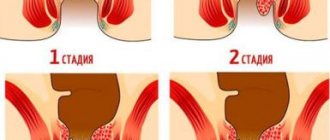
In the photo of rectal cancer, you can see that it significantly narrows the intestinal lumen. This causes constipation, a full stomach, and flatulence.
In this photo, the carcinoma is growing infiltratively, covering the wall.
The course of the cancer process progresses in the absence of proper treatment. The stage is determined by the degree of damage to the intestine itself, its growth through the wall, the presence of metastases in the lymph nodes, and distant lesions of other organs.
In this regard, tumors are divided into 4 stages. This distribution is universal for any malignant tumors.
The small size of the tumor and its growth only through the mucous and submucosal layer of the rectum, without affecting the muscular and serous layer, allows surgical removal of the tumor itself. Sometimes it is possible to perform surgery through the colon using a colonoscope.
If it has grown into the muscle layer, then rectal resection or extirpation (complete removal of the organ) is indicated. The perirectal tissue and lymph nodes are also removed, in which metastases are already detected in 20% of cases. To perform the operation, two approaches are used - laparotomy (dissection of the abdominal wall) and laparoscopy (operation using video equipment through several punctures in the abdomen).
The type of surgery is selected based on the location of the tumor. The high position makes it possible to remove the tumor and temporarily bring the end of the intestine to the abdominal wall - to form a colostomy for defecation. Such manipulation is necessary if it is not yet possible to sew the ends of the intestine together. The second stage, after some time, restores the integrity of the intestine.
If the tumor process is located low, if there is no healthy tissue left below it, the affected area and anus are removed, and a colostomy is applied to the abdominal wall.
Chemotherapy and radiation therapy are indicated for patients with stage 2 or higher tumors.
If before the operation metastases were detected in several lymph nodes, and the tumor has grown into the muscle layer, then at the stage of preparation for the operation a short course of radiation therapy is carried out for 5 days. This allows you to destroy early metastases and reduce the size of the formation itself.
Treatment of rectal cancer after surgery is carried out after obtaining pathomorphological data on the removed tissues. The issue of radiation or its combination with chemotherapy is being decided. Radiation therapy after surgery destroys the remaining cells in the area of the primary tumor and prevents its recurrence. In inoperable patients, it alleviates the condition.
Sensitivity to chemotherapy is detected in 30% of patients. It is prescribed for therapeutic purposes to destroy metastases.
Chemotherapy is also carried out adjuvantly - to prevent the spread of carcinoma if damage to several lymph nodes is detected.
The method of therapy improves the quality and life expectancy of patients with metastases. Platinum preparations, 5-fluorouracil, leucovarin, and calcium folinate are used. Medicines are administered intravenously in courses of several days. Chemotherapy is also used in combination with radiation before surgery for locally advanced cancer. This combined treatment is carried out for 1-1.5 months, and after the end of irradiation, surgery is performed 6 months later.
| Stage | Characteristic signs |
| 0 (precancerous condition) | The presence of benign formations in the lumen of the colon (polyps, adenomas), foci of chronic inflammation with erosive and ulcerative defects of the mucosa and anal fissures (Crohn's disease, ulcerative colitis, hemorrhoids). These pathological conditions of the lower digestive tract are harbingers of malignant neoplasms. Regional lymph nodes (close to the affected organ) are not enlarged. |
| I (first) | A tumor of small size (up to 2 cm) is diagnosed, involving the mucous membrane of the intestinal wall. One lymph node in any of the regional collectors may be enlarged (fusion of large lymphatic vessels). A cancerous tumor develops in place; atypical cells do not spread throughout the body. |
| II (second) | A malignant neoplasm measuring from 2 to 5 cm is detected. The tumor grows into the mucous and submucosal layer of the intestinal wall. Enlarged lymph nodes in regional collectors (2-3 in different places). The cancer does not spread beyond the organ, there are no metastases. |
| III (third) | A cancerous tumor of significant size (from 5 to 10 cm) is diagnosed. The neoplasm involves the muscular layer of the intestinal wall, but does not extend beyond the serosa (outer membrane). The malignant process can be bilateral. The tumor partially or completely blocks the intestinal lumen. A large number of regional lymph nodes in all collectors increases. Secondary foci of the malignant process begin to form. The tumor is detected in regional lymph nodes. There are no distant metastases. |
| IV (fourth) | The final and most severe stage of cancer. The malignant neoplasm reaches large sizes (more than 10 cm), affecting all layers (mucosal, submucosal, muscular) of the intestinal wall. The outer (serous) membrane grows and extends beyond the organ. Regional lymph nodes become significantly enlarged, merge into conglomerates, become inflamed and ulcerate. The tumor disintegrates, cancer cells spread throughout the body (to tissues, organs and distant lymph nodes) with the formation of metastases. Most often, atypical cells end up in the liver, lungs, kidneys and bones. In the presence of distant metastases, stage IV is assigned regardless of the size of the tumor and damage to the lymph nodes. |
A small malignant tumor does not block the intestinal lumen. There are no metastases. Consequently, symptoms in the initial stages of tumor development are nonspecific. Clinical manifestations can be associated with any inflammatory bowel disease or digestive disorder. Therefore, it is important not to waste time and conduct early diagnosis. Colon cancer at stages I-II is highly treatable.
Dyspeptic syndrome. Associated with digestive disorders, characterized by the following symptoms:
- constant feeling of nausea;
- heartburn;
- belching sour;
- bitter taste in the mouth;
- decreased appetite.
Enterocolitic syndrome. It is characterized by intestinal dysbiosis of the type of fermentative dyspepsia. Accompanied by a disruption in the process of formation of feces and their removal from the body. The following symptoms are present:
- alternation of constipation (“sheep” feces) with diarrhea (foamy stool with an unpleasant smell of fermentation);
- bloating and rumbling in the abdomen as a result of increased gas formation;
- a feeling of heaviness and fullness in the abdominal cavity even after defecation;
- the appearance of mucus, streaks of blood or pus in the stool.
Asthenic syndrome. Accompanied by weakness, drowsiness, and increased fatigue.
Pain syndrome. In the initial stages of intestinal cancer, it is mild. Periodic aching pain in the abdomen or painful urge (tenesmus) before defecation are possible.
Anemic syndrome. Characterized by pallor of the skin and mucous membranes of the mouth; periodic dizziness.
The cancerous tumor reaches an impressive size and blocks the intestinal lumen, causing partial or complete obstruction. Metastases appear. Due to the disintegration of the malignant neoplasm, severe intoxication develops, sharply worsening the patient’s condition. An aversion to food appears, followed by exhaustion of the body (cachexia).
Obstruction syndrome. It occurs due to narrowing (stenosis) of the intestinal lumen due to a growing cancerous tumor. The blockage may be partial or complete. The process of excretion of feces is disrupted. Stenosis of the final section of the large intestine (sigmoid or rectum) is accompanied by an attack of cramping pain and severe bleeding (scarlet blood) from the anus.
As a result of complete obstruction, signs of acute intestinal obstruction develop:
- vomiting with feces;
- severe cramping pain in the abdomen;
- absence of stool and gas production for more than 3 days;
- “raspberry jelly” symptom (discharge of mucus with blood from the rectum);
- asymmetrical “oblique” belly;
- accumulation of fluid in the abdominal cavity (ascites).
- Diarrhea or constipation that lasts several days.
- Change in the appearance of stool. It becomes pencil thin because the tumor narrows the lumen of the intestine.
- After visiting the toilet, there remains a feeling of discomfort, a feeling that the intestines have not completely emptied.
- Bleeding from the rectum.
- Blood in the stool.
- Dark, tarry stool - in medical parlance, this appearance of stool is called melena.
- Pain, cramps in the abdomen.
- Unexplained weight loss.
- Constant weakness, increased fatigue.
- Maintain a normal weight. Obesity is one of the risk factors for cancer.
- Exercise regularly.
- Eat healthy. Your diet should contain a lot of vegetables, fruits, grains, and fiber-rich foods. Eating large amounts of red and processed meat contributes to the development of cancer.
- Minimize alcohol consumption and stop smoking. These bad habits contribute to the development of cancer not only in the intestines, but also in other organs.
Clinical picture of intestinal oncology
Like any cancer, intestinal cancer needs to be diagnosed at the earliest stages, but often patients begin to be treated for the wrong disease because of the first symptoms. Because of this, they waste a lot of time, and later the intestinal oncology moves to a new stage, and it is much more difficult to treat.
That is why the most important thing is to understand the pathology and identify cancer as early as possible. The cancer itself can be located anywhere in the intestine, and, of course, the first and subsequent symptoms will greatly depend on the location.
First signs
The worst thing is that in the first stages the patient feels practically nothing, which is why he loses a lot of time. There is a theory that the tumor itself, as well as malignant cells, releases small amounts of painkillers into neighboring tissues. Therefore, the patient does not feel anything at the very beginning. But there are several syndromes that may indicate bowel cancer:
- Enterocolitic syndrome - usually occurs with cancer on the left side of the colon or cecum. In this case, fermentation of the food coma appears, the process of feces itself is disrupted, constant bloating, long-term constipation, which can then abruptly give way to diarrhea.
- Stenosis - here usually the cancer itself goes to the stage when the neoplasm clogs the intestine itself and interferes with the passage of feces. Then it becomes difficult for the patient to go to the toilet, and constipation occurs quite often. Bloating and severe abdominal pain and colic. The pain associated with bowel cancer goes away immediately after defecation.
- Dyspeptic syndrome - usually accompanied by vomiting, constant nausea, painful and severe heartburn, as well as a constant bitter taste in the mouth. The syndrome is associated with the fact that cancer causes disruption of the digestive process.
- Pseudospastic - the layers of the peritoneum become inflamed, causing a strong drop in temperature, severe abdominal pain, and intoxication occurs, which is why the person constantly feels bad and gets tired quickly.
- Cystitis - the cancer itself already deeply covers the intestinal tissue and affects nearby organs: the bladder, uterus and ovaries in women. There is pain when urinating, the appearance of blood in the urine, as well as bloody and mucous discharge from the vagina.
- Other symptoms are fatigue and constant weakness throughout the body. Pale and very dry skin, drier and other mucous layers and membranes, constantly rising body temperature, chills, headache and dizziness, indigestion. A feeling of constant fullness in the intestines, even after defecation. Blood in the stool or even bleeding from the anus may cause intestinal carcinoma.