Bronchial asthma in children is a chronic disease of the respiratory tract associated with bronchial hyperreactivity, that is, their increased sensitivity to irritants. The disease is widespread: according to statistics, it affects approximately 7% of children. The disease can manifest at any age and in children of any gender, but most often occurs in boys from 2 to 10 years old.
Bronchial asthma is a common chronic disease among children
The main clinical sign of bronchial asthma in a child is periodic attacks of difficulty breathing or suffocation caused by widespread reversible bronchial obstruction associated with bronchospasm, hypersecretion of mucus and swelling of the mucous membrane.
In recent years, the incidence of bronchial asthma in children has been increasing everywhere, but especially in economically developed countries. Experts explain this by the fact that every year more and more artificial materials, household chemicals, and industrial food products containing a large number of allergens are used. It should be borne in mind that the disease often remains undiagnosed, as it can masquerade as other pathologies of the respiratory system and, above all, as an exacerbation of chronic obstructive pulmonary diseases (COPD).
Causes and risk factors
Risk factors for the development of bronchial asthma in children are:
- hereditary predisposition;
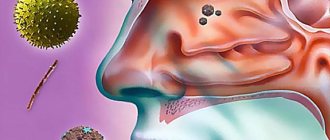
- constant contact with allergens (waste products of house dust mites, mold spores, plant pollen, proteins of dried urine and saliva, dander and pet hair, bird fluff, food allergens, cockroach allergens);
- passive smoking (inhalation of tobacco smoke).
Factors-provocateurs (triggers) affecting the inflamed mucous membrane of the bronchi and leading to the development of an attack of bronchial asthma in children are:
- acute respiratory viral infections;
- air pollutants such as sulfur or nitrogen oxides;
- β-blockers;
- nonsteroidal anti-inflammatory drugs (Aspirin, Analgin, Paracetamol, Nurofen, etc.);
- pungent odors;
- significant physical activity;
- sinusitis;
- inhalation of cold air;
- gastroesophageal reflux.
Risk factors for the development of bronchial asthma in children
The formation of bronchial asthma in children begins with the development of a special form of chronic inflammation in the bronchi, which causes their hyperreactivity, that is, increased sensitivity to the effects of nonspecific irritants. In the pathogenesis of this inflammation, the leading role belongs to lymphocytes, mast cells and eosinophils - cells of the immune system.
After puberty, bronchial asthma attacks stop in 20–40% of children. For others, the disease persists throughout their lives.
Hyperreactive inflamed bronchi respond to trigger factors by hypersecretion of mucus, spasm of bronchial smooth muscles, edema and infiltration of the mucous membrane. All this leads to the development of obstructive respiratory syndrome, which is clinically manifested by an attack of suffocation or shortness of breath.
Causes of pathology
The main cause of attacks is considered to be hyperactivity of the bronchi , which instantly react to various stimuli.
The most common reasons:
- Most often, asthma develops in boys, as they have structural features of the bronchi .
- Overweight children also often suffer from asthma. The diaphragm occupies a high position and therefore insufficient ventilation of the lungs occurs.
- Genetic predisposition plays an important role in the development of this disease.
- Some foods should be excluded: chocolate, nuts, fish .
Sometimes asthma is the final stage of allergic manifestations .
First, urticaria appears, then eczema with itching, and only then the body reacts to the irritant with an asthmatic attack.
Often attacks occur after bronchitis or after a respiratory illness.
Forms of the disease
According to the etiology, bronchial asthma in children can be:
- allergic;
- non-allergic;
- mixed;
- unspecified.
Doctors identify aspirin-induced bronchial asthma as a special form. For her, the trigger factor is the child taking non-steroidal anti-inflammatory drugs. Often complicated by the development of status asthmaticus.
Depending on the severity, there are several types of clinical course of bronchial asthma in children:
- Mild episodic. Attacks occur less than once a week. During the interictal period, the child has no signs of bronchial asthma, and lung function is not impaired.
- Mild persistent. Attacks occur more than once a week, but not daily. During an exacerbation, the child’s sleep is disturbed and normal daytime activity deteriorates. Spirometry values are normal.
- Medium-heavy. Attacks of suffocation occur almost daily. As a result, children's activity and sleep are significantly affected. To improve their condition, they require daily use of inhaled β-antagonists. Spirometry indicators are reduced by 20–40% of the age norm.
- Heavy. Attacks of suffocation occur several times a day, often at night. Frequent exacerbations cause disturbances in the child’s psychomotor development. Indicators of external respiration function are reduced by more than 40% of the age norm.
Condition of the respiratory tract in bronchial asthma
Feeling of tightness in the chest
When the airways located in the lungs are strained, they narrow. The air is exhaled with difficulty. When air is forced out through the narrow airways, it causes wheezing and a feeling of tightness in the chest. This causes serious discomfort, including painful sensations reminiscent of cardiac dysfunction. In addition, when compressed, shortness of breath appears, as a result of which a lack of air is felt. There is a feeling of compression of the chest and the inability to exhale. At the same time, fear and panic arise, fear of unnecessary movements. The child must also be kept from excessive throwing, so as not to aggravate his condition. In severe cases, you should immediately call a doctor.
Symptoms of bronchial asthma in children
Attacks of suffocation or difficulty breathing in children suffering from bronchial asthma can occur at any time of the day, but most often they occur at night. The main symptoms of bronchial asthma in children:
- attack of expiratory shortness of breath (difficulty in exhaling) or suffocation;
- nonproductive cough with viscous, difficult-to-clear sputum;
- cardiopalmus;
- whistling dry (buzzing) wheezing, intensifying at the moment of inhalation; they are heard not only during auscultation, but also at a distance and therefore they are also called distant wheezing;
- boxed percussion sound, the appearance of which is explained by hyperairiness of the lung tissue.
Unproductive cough and difficulty exhaling are symptoms of bronchial asthma in a child
Symptoms of bronchial asthma in children during a severe attack become different:
- the number of breathing sounds decreases;
- cyanosis of the skin and mucous membranes appears and increases;
- paradoxical pulse (an increase in the number of pulse waves at the moment of exhalation and a significant decrease until complete disappearance at the moment of inspiration);
- participation in the act of breathing of auxiliary muscles;
- taking a forced position (sitting, leaning your hands on the bed, the back of a chair or your knees).
In children, the development of an attack of bronchial asthma is often preceded by a period of precursors (dry cough, nasal congestion, headache, anxiety, sleep disturbance). The attack lasts from several minutes to several days.
If an attack of bronchial asthma continues in a child for more than six hours in a row, this condition is regarded as status asthmaticus.
After the resolution of an attack of bronchial asthma in children, thick and viscous sputum is released, which leads to easier breathing. Tachycardia gives way to bradycardia. Blood pressure decreases. The child becomes lethargic, lethargic, indifferent to his surroundings, and often falls soundly asleep.
In the interictal periods, children suffering from bronchial asthma can feel quite satisfactory.
Typical symptoms
It is quite difficult to detect asthma in a child. This is explained by the fact that the symptoms of bronchial asthma are similar to those of a common cold or viral disease. Therefore, parents often do not even realize that a serious pathology is developing.
It should be noted that with bronchial asthma there is no increase in temperature . A few days before the main symptoms of asthma, warning signs appear. At this time, children are irritated, sleep poorly and are excited.
Manifestations of harbingers:
- In the morning, your baby has mucus running from his nose and sneezes frequently.
- After a couple of hours, a dry cough appears.
- In the middle of the day the cough intensifies and becomes wet.
- After a maximum of two days, the cough becomes paroxysmal.
Then the warning signs stop and the main symptoms of the disease appear.
Manifestations of the main signs:
- A severe coughing attack occurs before going to bed or after waking up.
- The upright position reduces coughing.
- Before an attack, the child begins to cry and be capricious, as his nose is blocked.
- Shortness of breath occurs.
- Breathing is intermittent and accompanied by whistling.
- There are atypical manifestations - itching and rashes on the skin.
If asthma has become severe, attacks begin to occur at any time.
Diagnostics
To correctly diagnose bronchial asthma in children, it is necessary to take into account data from an allergic history, laboratory, physical and instrumental studies.
Laboratory testing methods for suspected bronchial asthma in children include:
- complete blood count (eosinophilia is often detected);
- sputum microscopy (Charcot-Leiden crystals, Kurshman spirals, a significant amount of epithelium and eosinophils);
- study of the gas composition of arterial blood.
Diagnosis of bronchial asthma in children includes a number of special studies:
- pulmonary function test (spirometry);
- performing skin tests to identify causally significant allergens;
- detection of bronchial hyperactivity (provocative tests with a suspected allergen, physical activity, cold air, hypertonic sodium chloride solution, acetylcholine, histamine);
- chest x-ray;
- bronchoscopy (performed extremely rarely).
Spirometry allows you to study lung function if bronchial asthma is suspected in children
Differential diagnosis is necessary with the following conditions:
- bronchial foreign bodies;
- bronchogenic cysts;
- tracheo- and bronchomalacia;
- obstructive bronchitis;
- bronchiolitis obliterans;
- cystic fibrosis;
- laryngospasm;
- acute respiratory viral infection.
Bronchial asthma is widespread: according to statistics, it affects approximately 7% of children. The disease can manifest at any age and in children of any gender, but most often occurs in boys from 2 to 10 years old.
Providing first aid during an attack
Parents are required to sense the onset of an asthma attack in a timely manner and be able to quickly eliminate it.
Attention should be paid to the child's breathing and appearance :
- The breathing rate should be no more than 20 breaths per minute.
- When breathing, the child's shoulders should not rise. The rest of the muscles should not be used either.
- Before an attack, the child’s nostrils begin to dilate.
- A bad sign is hoarse breathing.
- A dry cough may also indicate the development of asthma.
- You should monitor your child's skin. If you have asthma, the body spends a lot of effort to restore breathing, and this leads to the fact that the skin becomes sticky and pale.
- During a severe attack, the skin in the nose area becomes bluish. This indicates a lack of oxygen. The condition is very dangerous, so you should always have inhalers at home.
The attack occurs suddenly and without any reason. In this case, emergency assistance is needed .
In such a situation, when inflammation has occurred in the respiratory tract (edema, bronchospasm), the choking child needs to ease breathing with a strong bronchodilator.
The most effective way is an inhaler , which allows the drug particles to instantly reach the affected area of the bronchi.
A good and proven drug for providing immediate assistance is Salbutamol . It is prescribed by a doctor, and the parents of a sick child are required to know how to use the device.
Children under 5 years old do not yet know how to inhale correctly. Therefore, for such babies there are special inhalers - nebulizers . It is often necessary to use spacers. The inhaler itself is inserted into such a device.
During an acute attack, the child is given certain doses of the drug. The inhalation process is carried out every 10 minutes and continues until breathing normalizes. If there is no improvement, then hospitalization is required .
You should not be afraid of the inhaler, as there is no danger of overdose.
Treatment of bronchial asthma in children
The main directions of treatment of bronchial asthma in children are:
- identifying factors that cause exacerbation of bronchial asthma and eliminating or limiting contact with triggers;
- basic hypoallergenic diet;
- drug therapy;
- non-drug restorative treatment.
Drug therapy for bronchial asthma in children is carried out using the following groups of drugs:
- bronchodilators (adrenergic receptor stimulants, methylxanthines, anticholinergics);
- glucocorticoids;
- mast cell membrane stabilizers;
- leukotriene inhibitors.
Symptomatic medications can quickly relieve bronchospasm
In order to prevent exacerbations of bronchial asthma, children are prescribed basic drug therapy. Its scheme is largely determined by the severity of the disease:
- mild intermittent asthma - short-acting bronchodilators (β-adrenergic agonists) if necessary, but not more than 3 times a week;
- mild persistent asthma - daily cromalin sodium or glucocorticoids by inhalation plus long-acting bronchodilators, if necessary short-acting bronchodilators, but not more than 3-4 times a day;
- moderate asthma - daily inhaled administration of glucocorticoids in a dose of up to 2,000 mcg, long-acting bronchodilators; if necessary, short-acting bronchodilators can be used (no more than 3-4 times a day);
- severe asthma - daily inhaled administration of glucocorticoids (if necessary, they can be prescribed in a short course in the form of tablets or injections), long-acting bronchodilators; to stop an attack - short-acting bronchodilators.
Treatment for an attack of bronchial asthma in children includes:
- oxygen therapy;
- β-adrenergic agonists (Salbutamol) by inhalation;
- adrenaline hydrochloride subcutaneously;
- Eufillin intravenously;
- glucocorticoids orally.
Indications for hospitalization are:
- the patient belongs to a high mortality group;
- ineffectiveness of the treatment;
- development of status asthmaticus;
- severe exacerbation (forced expiratory volume in 1 second is less than 60% of the age norm).
In the treatment of bronchial asthma in children, it is important to identify and eliminate the allergen that is the trigger factor. To do this, there is often a need to change the child’s diet and life (hypoallergenic diet, hypoallergenic lifestyle, change of place of residence, parting with a pet). In addition, children may be prescribed long-term antihistamines.
For effective treatment of bronchial asthma in a child, it is important to identify the allergen and eliminate it
If the allergen is known, but it is impossible to get rid of contact with it for one reason or another, then specific immunotherapy is prescribed. This method is based on introducing to the patient (parenterally, orally or sublingually) gradually increasing doses of the allergen, which reduces the body's sensitivity to it, that is, hyposensitization occurs.
Doctors identify aspirin-induced bronchial asthma as a special form. For her, the trigger factor is the child taking non-steroidal anti-inflammatory drugs.
During the period of remission, children with bronchial asthma are prescribed physical therapy:
- speleotherapy;
- breathing exercises;
- acupressure;
- chest massage;
- hydrotherapy;
- ultraphonophoresis;
- electrophoresis;
- magnetic therapy;
- DMV therapy;
- inductothermy;
- aeroionotherapy.
Features of the disease
How does asthma begin? Bronchial asthma is a negative reaction of the bronchi to a specific allergen.
The pathology is often hereditary and manifests itself at an early age.
Exacerbations are replaced by remission, and the duration of these periods depends on the characteristics of the child, living conditions, and medications used. The disease cannot be contracted .
When a child develops a cough after interacting with children who have the same symptoms, this indicates bronchial obstruction. It occurs due to the effect of the virus on the bronchi.
The diagnosis does not mean that the child will be disabled, but many restrictions will be required.
Eliminating the disease is very difficult, but with the help of medications you can maintain remission for a long time .
Possible consequences and complications
The main complications of bronchial asthma are:
- status asthmaticus;
- pneumothorax;
- pulmonary heart.
In children suffering from a severe form of the disease, glucocorticoid therapy may be accompanied by the development of a number of side effects:
- disturbances in water and electrolyte balance with the possible appearance of edema;
- increased blood pressure;
- increased release of calcium from the body, which is accompanied by increased fragility of bone tissue;
- an increase in blood glucose concentration, up to the formation of steroid diabetes mellitus;
- increased risk of occurrence and exacerbation of gastric and duodenal ulcers;
- decreased tissue regenerative capacity;
- increased blood clotting, which increases the risk of thrombosis;
- decreased resistance to infections;
- obesity;
- moon-shaped face;
- neurological disorders.
What is absolutely forbidden to do?
Asthma attacks do not always end well . There are also deaths associated with this disease. Unfortunately, it is often not the disease itself that is to blame for the death of children, but the unreasonable actions of the parents.
This happens if inadequate medications have been used. A child who is having a suffocation attack should not be given :
- sedatives . Such drugs prevent deep breathing, and this is unacceptable during a severe asthma attack;
- expectorants . Mucolytics activate the formation of mucus, and in asthma there is already an excess of it;
- antibiotics _ These drugs are the most useless for asthma. They can only be used for complications (pneumonia).
Forecast
The prognosis for life in children with bronchial asthma is generally favorable. After puberty, bronchial asthma attacks stop in 20–40% of children. For others, the disease persists throughout their lives. The risk of death during a choking attack increases in the following cases:
- history of more than three hospitalizations per year;
- history of hospitalization in the intensive care unit;
- there were cases of mechanical ventilation (artificial pulmonary ventilation);
- an attack of bronchial asthma was at least once accompanied by loss of consciousness.
Forms
The bronchial form comes in the following forms:
- Asthma is non-allergic . This form occurs due to endocrine diseases, overload of the nervous system or ingestion of microorganisms.
- Mixed asthma. This pathology is characterized by all possible symptoms of this disease.
- Allergic . This type of asthma manifests itself as:
- a combination of symptoms of pathology and a runny nose, accompanied by copious discharge;
- cough with phlegm;
- reactions to contact with a stimulus.
Children of any age are at risk of developing asthma, but it most often develops in children under 5 years of age.
Prevention of bronchial asthma in children
The importance of preventing bronchial asthma in children cannot be overestimated. It includes:
- breastfeeding during the first year of life;
- gradual introduction of complementary foods in strict accordance with the child’s age;
- timely active treatment of respiratory diseases;
- keeping the home clean (wet cleaning, avoiding carpets and soft toys);
- refusal to keep pets (if any, careful adherence to hygiene rules);
- preventing children from inhaling tobacco smoke (passive smoking);
- regular exercise;
- annual holiday on the sea coast or in the mountains.
Video from YouTube on the topic of the article:
Wheezing
Often exhalation is accompanied by a high-pitched dull or noisy sound, which is characterized as wheezing. This indicates difficulty breathing due to mucus accumulated in the bronchi or trachea or spasms of the respiratory system. Sometimes it may be a foreign object that has entered the respiratory tract.
One of the most likely causes of wheezing is bronchial asthma. This disease affects 5 percent of children from the age of six months. In mild asthma, whistling sounds are rarely produced. A whistling sound when exhaling may indicate the presence of other diseases. The final diagnosis is made by the pediatrician after a thorough diagnosis.
Drug-free therapy
There are also ways to treat bronchial asthma. They mean:
- therapeutic exercises;
- physiotherapy;
- massage;
- hardening;
- breathing techniques;
- visiting salt caves.
Herbal medicine complements traditional treatment and helps to increase the period of remission. Decoctions of medicinal herbs are used. They are prepared daily and taken for a long time. Doses should be agreed with your doctor.
Bronchial asthma sometimes disappears on its own during adolescence, but this does not happen often.
Drug treatment
Drug treatment can be divided into two types:
- symptomatic treatment, that is, elimination of the attack;
- basic therapy.
Only the doctor chooses the treatment tactics. Self-medication is absolutely excluded , since illiterate use of medications will aggravate the disease and can lead to respiratory failure.
Symptomatic treatment consists of the use of bronchodilators: Salbutamol, Ventolin . In severe cases, corticosteroid drugs are used. The main route of administration is inhalation.
Unfortunately, all drugs of this type of treatment have a temporary effect. And uncontrolled use of such drugs will lead to the fact that the bronchi will stop responding to the medicine. Therefore, the dose of the drug should be strictly controlled .
Basic therapy is selected individually, taking into account the severity of asthma and the characteristics of the child.
The following drugs are used:
- Antihistamines - Suprastin, Tavegil, Claritin.
- Antiallergic - Intal, Ketotifen.
- Antibiotics – sanitize foci of infection.
Sometimes hormonal drugs are prescribed to prevent exacerbations of the disease. Leukotriene inhibitors are often used, which reduce sensitivity to allergens.
Treatment is canceled if remission is observed for two years. In case of relapse, treatment should be started again.
Prevention
To reduce asthma attacks to a minimum, preventive measures are necessary . They must be taken if the child is predisposed to this disease.
How to prevent this pathology:
- Books must be stored in locked cabinets.
- There is no need to store clothes in the child's room.
- You should not buy soft toys.
- It is advisable to wash bed linen with hypoallergenic powders.
- The presence of animals in the apartment is undesirable.
- During the cleaning period, the child should be removed from the room.
- The linoleum should be replaced with another covering.
Following these simple recommendations will help avoid exacerbation of the disease .
Previously, asthmatics adjusted their lives to the disease. Much was strictly prohibited. Children especially suffered from this - they couldn’t get a puppy, they couldn’t jump.
But today everything has changed. Advances in medicine have allowed children to live full lives along with other people .
Dr. Komarovsky about asthma in this video:
Causes of asthma in a child
Asthma attacks in children occur due to bronchial hyperreactivity. The allergen to which the child reacts causes hyperreactivity.
The main reason for this reaction is hereditary predisposition.
The state of the child’s immune system greatly influences the possibility of developing asthma.
In addition, the first signs of asthma in children may occur due to poor environmental conditions, when large quantities of dust, exhaust gases, and other impurities are present in the air.
The child may react with asthma attacks to foods. Also, allergies in the form of asthma can be caused by certain medications and household chemicals, pet hair, pollen, and cold or dry air.
Children who are overweight are more susceptible to the disease.
What parents should pay attention to
Parents can independently identify the first signs of bronchial asthma in children.
Sometimes this is difficult, since the symptoms are similar to a cold or viral diseases. But if asthma occurs, the child does not have a fever, and the cough is dry and frequent.
You can assume the possibility of this disease if:
- First, mucous discharge from the nose (watery) is observed, the child sneezes after sleep.
- In the morning the child coughs (the cough is weak and dry).
- After lunch it may become more intense and turn moist.
- On the second day it turns into dry paroxysmal.
- The child suffers from shortness of breath, breathes with difficulty, with whistling, breaths are frequent and incomplete.
- Seizures occur at any time.
If the area of the labial triangle turns blue, immediate hospitalization is necessary.
Blueness in the labial area indicates a lack of oxygen. In any case, you should immediately show the child to a specialist to prevent severe complications of potential bronchial asthma.
Which children may be at risk?
Pediatric doctors primarily pay attention to children about whom the following information is known:
- the child has a hereditary predisposition to bronchial asthma and other allergic manifestations;
- the baby was diagnosed with atopic dermatitis or allergic rhinitis;
- the medical history records repeated episodes of childhood croup;
- the child often suffers from ARVI and has signs of broncho-obstructive syndrome due to any colds or viral diseases.
Preventive measures
Pediatricians recommend preventive measures for asthma in infants:
- Extending breastfeeding up to a year.
- Smooth transition from mother's milk to complementary foods.
- Removing pets and anything that collects dust (carpets of books) from the child’s room.
- Constantly carrying out wet cleaning without using household chemicals.
- Increasing immunity (taking vitamins, including fruits and vegetables in the diet, constant walks in the fresh air).
If it is not possible to accommodate a pet, try to ensure that the baby has as little contact with it as possible. A combination of drug treatment and prevention, together with parental care, will help the child recover faster. Asthma in infants is completely curable if the problem is corrected in time.
Treatment
Includes methods of drug and non-drug therapy. The process is long, in some cases lifelong, so parents should be patient and not believe in miracle pills and other treatments that can get rid of the disease at once.
Older asthmatic children need to be explained that this is a necessity, and if all recommendations are strictly followed, they will be able to live a full life.
Complications
Most often, against the background of a previous illness, infants may develop pulmonary atelectasis - this is a decline and adhesion of the pulmonary vesicles. The lungs reach this state due to the lack of air in the tissues. The lack of air is due to the fact that swelling of the bronchi is added to the still narrow lumen of the newborn.
Atelectasis, in turn, leads to bronchiectasis - severe dilatation of the bronchi, due to damage to the bronchial wall and pneumosclerosis - replacement of lung tissue with connective tissue. The proliferation of connective tissue deforms the bronchi, sharply compacts and wrinkles the lung tissue. There is no air entering the lungs and they shrink.
Causes of the disease
Increased bronchial reactivity may be due to:
Hereditary predisposition
Approximately 60% of sick children have relatives suffering from bronchial asthma.
The disease may not manifest itself, however, the chances that asthma will manifest itself in childhood increases if:
- The child was born premature;
- Appeared as a result of difficult childbirth or after a difficult pregnancy;
- When a child lives in conditions with poor ecology.
Environmental factors:
- Various allergenic substances found in food products;
- Dust: home and industrial;
- Household chemicals;
- Tobacco smoke;
- Pollutants contained in the air;
- Perfumes;
- Microbial particles: bacteria, viruses, fungi, which cannot always provoke diseases (for example, sinusitis or ARVI), but can easily provoke an attack of bronchial asthma;
- Certain medications;
- Frequent changes in environmental conditions: high humidity, cold, thunderstorms;
- Feathers and down of birds;
- Animal saliva.
As a rule, bronchial asthma occurs when a number of allergens are combined.
Internal factors:
- Endocrine, infectious, neuropsychiatric diseases, high weight of the child.
- Other factors, namely physical activity.
The course of asthma is significantly aggravated by diseases of the internal organs.
The cause is the gastrointestinal tract, in which various pathologies often develop: gastritis, gastroduodenitis, constipation, dysbacteriosis, biliary dyskinesia.
First aid
First of all, the child needs to be calmed down. Psychosomatics plays an important role in the development of an attack.
- Remove tight clothing, open a window to allow fresh air into the room (avoid cold air).
- Give the child an inhaler or nebulizer, you can supplement it with an aminophylline tablet.
- It is advisable to make a warm bath for your hands and feet.
If these measures do not stop the attack within half an hour, call an ambulance. Waiting any longer may cause you to stop breathing!
Treatment of bronchial asthma in children depends on the form, cause and degree of the disease. Hospitalization is required for severe exacerbations and if serious complications have developed - status asthmaticus, emphysema. In other cases, the child is treated at home, under the supervision of his parents.
Prevention is based on removing the allergen from the child’s environment. To do this, daily wet cleaning is carried out, and an impermeable cover can be put on the mattress. This alleviates the child’s condition if he has an allergic form.
Inhalation forms of drugs are used. Most of them contain glucocorticoids in combination with a beta-agonist. This combination gives a pronounced anti-inflammatory effect and makes breathing easier. Children can use the inhaler from the age of five years. Before this, the drugs are administered through a nebulizer or spacer.
Inhalers are prescribed by a doctor. They can be used only when an attack occurs or on an ongoing basis. To stop the symptoms of an attack, salbutamol is most often used.
Antiallergic drugs zafirlukast, montelukast, sodium cromoglycate are prescribed in tablet form. Used as prevention and treatment of exacerbations. Sometimes they are prescribed for regular use if the effect of inhalation is insufficient.
There are benefits for medications if you are registered as disabled.
Folk remedies
Can be used as an auxiliary method or prevention. Treatment is carried out using infusions of herbs, ginger, and propolis preparations. Of the herbs, the most effective are “Breast collection”, licorice root, and chamomile decoction.
Treatment with traditional methods is contraindicated if you are allergic to the components of the product. This can cause a very severe asthma attack, severe exacerbation and subsequent disability.