- Types of rhinosinusitis
- Factors predisposing to the development of rhinosinusitis
- Reasons for the development of rhinosinusitis
- Development mechanism
- Symptoms of rhinosinusitis
- Diagnosis and recommended clinical studies
- Laboratory research methods
- Instrumental research methods
- Differential diagnosis
- General principles of treatment
- Forecast
Rhinosinusitis is an inflammation of the mucous membrane of the paranasal sinuses.
What is rhinosinusitis
If the inflammatory process in the respiratory system simultaneously affects the nasal cavity and sinuses (the amount does not matter), the doctor diagnoses “rhinosinusitis” or “sinusitis”. Both words refer to the same disease. Inflammation of the mucous membrane can either occur due to mechanical damage, or be a complication of ARVI, acute runny nose, or other infectious viral or bacterial diseases. Treatment for rhinosinusitis depends on the cause. Already at the first symptoms, a visit to an otolaryngologist is necessary, since the patient may receive as a complication:
- bronchial asthma;
- abscesses in the soft tissues of the face;
- intracranial changes (in rare cases, sinusitis leads to brain abscess, meningitis);
- visual impairment due to damage to the optic nerves;
- purulent inflammation of the middle ear;
- damage to the nervous system.
Infectious agents
Rhinosinusitis can be triggered by trauma, which will lead to a deviated nasal septum or narrowing of the sinuses, or result from physiological pathologies in the structure of the face and respiratory system, but most cases of this disease are associated with the activity of pathogenic microorganisms. This could be due to:
- viruses;
- bacteria;
- mushrooms.
Allergic rhinosinusitis
Chronic allergic rhinosinusitis develops when there is an allergy to various irritants. Local symptoms of the pathology are: burning, itching, watery nasal discharge, sneezing, lacrimation.
The seasonal form is manifested, in addition to local symptoms, by general ones - malaise, drowsiness, headache, irritability. The disease is associated with exposure to allergens on the body - pollen, wool, drugs.
Treatment of allergic rhinosinusitis involves identifying and eliminating the irritant. The patient is prescribed antihistamines.
Causes
Such a complex problem as rhinosinusitis does not arise out of nowhere, even if a person has become infected with the influenza virus. In addition to a general decrease in the defense of the immune system and colds, predisposing factors play a role, and the more of them, the higher the likelihood of getting rhinosinusitis. These include:
- polyps in the nasal cavity;
- pathologies of the endocrine system;
- deviated nasal septum;
- allergic rhinitis;
- problems with the development of the anatomical structures of the nasal cavity (impaired patency of the natural anastomoses of the sinuses, interfering with the timely removal of bacteria through active mucociliary transport);
- immunodeficiency states;
- pathologies of nearby organs.
Symptoms and severity
Symptoms are similar to the common cold and sinusitis.
The main symptoms indicating combined inflammation of the nasal and sinus mucosa:
- nasal congestion;
- copious discharge, often with pus. In case of allergic inflammation, the discharge is liquid, abundant, itching in the nose, sneezing, lacrimation are disturbing;
- pain and a feeling of fullness in the projection of the diseased sinus;
- fever.
There are mild, moderate and severe forms of the disease. Treatment tactics depend on the severity.
Lung
Symptoms: stuffy nose, discharge in the form of mucus, sometimes with pus, it can flow from the nose or flow down the throat. The temperature is either absent or rises to 37.5°C. Worried about headache and general weakness.
Medium-heavy
Symptoms: stuffy nose, purulent discharge, flowing out of the nose or into the throat, temperature above 37.5°C, general weakness, headache. The pain in the nasal sinuses bothers me, the pain radiates to the ears and teeth. The general condition is more serious.
Heavy
Symptoms: nasal congestion, profuse purulent discharge, headache, temperature rises above 38°C, palpation of the diseased sinus causes severe pain. There are always changes in the general blood test, characteristic of inflammatory processes. In severe cases of the disease, ocular or intracranial complications are present.
Symptoms of rhinosinusitis
Kinds
This disease can have several forms, which are determined by the pathogen, symptoms, and rate of development. Based on these differences, doctors have derived 4 main classifications, and to understand how to treat rhinosinusitis at home, you need to correctly and completely determine its type. Division can be carried out:
- By etiology: Viral - rhinoviruses, influenza and parainfluenza viruses, adenoviruses are involved here, and sinusitis of viral etiology always occurs in an acute form
- Bacterial - the causative agents are pneumoniae and pyogenic streptococci, Haemophilus influenzae, Pseudomonas aeruginosa and Escherichia coli, Moraxella, Staphylococcus aureus, Enterobacteriaceae.
- Fungal - the disease is provoked by Aspergillus, Alternaria, Culvularia, mainly it is a superinfection (coinfection of an infected cell with another strain or microorganism).
- Mixed - the inflammation is of a bacterial nature, and then gets a viral or fungal complication, or it all starts with the flu, and then a bacterial disease is added.
- maxillary – classic sinusitis;
- Light form.
- Spicy.
Why can a person get rhinosinusitis?
Most often, due to their constant employment, people suffer from ARVI and runny nose on their legs, despite the fact that all experts recommend bed rest. This is the first step to rhinosinusitis.
In addition, the inflammatory process in the nose quickly activates with physical deformation of the nasal walls. Thus, a deviated septum, the presence of adenoids or polyps in the nose interfere with its independent cleansing, which leads to stagnation of mucus.
If a viral infection enters the body, the mucous membrane swells and the glands begin to actively secrete their secretions. When mucus stagnates, bacteria can easily settle there. If patients use antibacterial drugs uncontrollably, fungal rhinosinusitis develops.
Chronic allergies, bronchial asthma, and a weakened immune system may also be the cause. The influence of poor ecology is considered to be an external factor of the disease.
General symptoms of the disease
The main manifestation of rhinosinusitis at any localization of inflammation is a violation of nasal breathing, which may be accompanied by mucous discharge (at the last stage - with pus), which is absent if the nose is blocked. Doctors include the following general symptoms of rhinosinusitis in people of all ages:
- increase in body temperature to 38-39 degrees (absent if the disease is chronic);
- runny nose;
- weakness;
- loss of appetite;
- headaches (at the end of the day);
- difficulty breathing;
- nasal voice;
- impaired sense of smell.
Frontit
When the inflammatory process affects the frontal lobe, rhinosinusitis immediately moves to a severe stage - the natural outflow of mucus from this area is reduced, and if abnormalities in the structure of the bones are added to this, frontal sinusitis can become chronic. The main symptoms include pain in the forehead in the morning (due to stagnation of secretions in the sinuses), which can be aggravated by the same sensations in the eyes, photophobia and loss of smell. As complications arise, the following are added:
- change in skin color;
- swelling of the forehead;
- collateral edema of the upper eyelid.
Ethmoiditis
The ethmoid labyrinth of the sinuses is located at the very base of the nose, so with an inflammatory process in this area, the main symptom is pain affecting the bones of the orbit. Additionally, ethmoiditis will be characterized by a decrease in the sense of smell or its complete loss, nasal congestion, and the appearance of purulent or mucopurulent discharge. Children have a fever. If the disease has reached a severe stage, bone destruction will begin, so the following will appear:
- hyperemia and swelling of the inner corner of the eye;
- swelling of the medial area of the eyelid;
- exophthalmos;
- impaired visual acuity.
- Instructions for use of Sinupret nasal drops for children and adults - composition, analogues and price
- Sinupret tablets for adults and children
- Fungus Alternaria alternata - routes of infection, signs, symptoms and treatment methods
Sinusitis
The most common form of rhinosinusitis is sinusitis - an inflammatory process in the maxillary sinuses, considered a complication of influenza, measles, acute runny nose and a consequence of a deviated nasal septum. It is characterized by a nagging pain that intensifies when the head is tilted forward and is localized in the area of the nose and bridge of the nose. Additional symptoms:
- difficulty in nasal breathing along with the appearance of nasality in the voice;
- headache (late evening);
- nasal discharge is green (purulent) or yellow if there is no congestion;
- permanent runny nose;
- sleep disturbance.
Sphenoiditis
If acute rhinosinusitis, which affected the ethmoid sinuses, was not cured, the process can reach the posterior sections and develop in the sphenoid sinuses, which will be the beginning of sphenoiditis. It is always acute in nature and is considered the most dangerous, since it can easily provoke complications in the eyes and brain. In the initial stages, the course of the disease may be asymptomatic, and later acute sphenoiditis will manifest itself:
- pain in the temporal zone, forehead and eyes;
- insomnia;
- decreased performance;
- constant aching pain in the back of the head;
- dizziness;
- copious thick discharge from the nasal passages.
Symptoms of rhinosinusitis
Acute rhinosinusitis is manifested by the following clinical signs:
- Intoxication - fever, fatigue, feeling of weakness, bloating and pressure in the ears;
- Impaired nasal breathing - nasal congestion, difficulty breathing, cough, decreased or absent sense of smell, excessive discharge, bad breath;
- Pain syndrome is pain and discomfort in the area of the affected sinus, which intensifies when the patient bends forward.
Symptoms that require urgent attention to an otolaryngologist:
- Swelling of the face,
- Visual abnormalities
- Mental disorders.
Acute rhinosinusitis develops quickly and is accompanied by vivid clinical symptoms and severe intoxication. Within a week from the onset of the disease, patients’ performance decreases, the upper part of the face swells, and the pain in the head becomes paroxysmal. Pathogenic microorganisms, actively multiplying, affect neighboring sinuses and cause the development of complications.
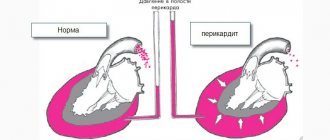
With chronic inflammation, the anastomosis between the nose and sinus swells and narrows. There is a lack of oxygen, which, in turn, increases inflammation. The main cause of chronic pathology is untreated acute rhinosinusitis.
Provoking factors:
- Congenital or acquired defects of the nasopharynx;
- Facial injuries;
- Allergic reactions;
- Regular inhalation of polluted or dusty air;
- Severe intoxication;
- Bad habits.
Symptoms: purulent discharge, weakened sense of smell and hearing, nasal voice, feeling of fullness in the sinus area. Exacerbation of the chronic process is manifested by symptoms identical to acute rhinosinusitis.
Chronic rhinosinusitis, according to the type of inflammation, is divided into catarrhal, purulent, polypous, cystic, mixed.
Chronic rhinosinusitis is a longer-lasting disease, but with less intense symptoms. Its duration is twenty to thirty weeks. The sluggish form of the pathology is often painless or with mild pain, causing irritability and weakness in patients. Due to the absence of characteristic symptoms, complications with chronic rhinosinusitis occur much more often than with acute rhinosinusitis.
Features
The symptoms of sinusitis need to be analyzed not only by the localization of the inflammatory process - it is important to take into account the severity of the disease, its etiology and the nature of its manifestation. So acute necessarily manifests itself in pronounced pain, but always has a short duration, subacute will be sluggish, lasting up to 3 months. In chronic cases, symptoms persist for longer than 12 weeks, and in recurrent cases, up to 4 exacerbations can occur in a year, with periods between them longer than 2 months.
Catarrhal
An acute inflammatory process of the sinus mucosa lasts 2-3 weeks and can affect the right or left side, or both. The main manifestation is an increase in body temperature and mucous discharge from the nose, which gradually thickens. If swelling of the affected area appears (often catarrhal rhinosinusitis affects several sinuses), the discharge stops, and the nose becomes completely blocked. Gradually, mucus accumulates in the nasopharynx, and an inflammatory process begins on the conjunctiva.
Acute purulent
With proper treatment, the duration of the acute form, even complicated by purulent discharge, does not exceed 4 weeks, while all the symptoms are pronounced - especially pain. In such a situation, there are several affected sinuses with purulent contents, so the pain can affect half the face or the entire surface. Thick green nasal discharge, increased body temperature, symptoms of severe intoxication and swelling are the main manifestations of the acute phase.
Chronic
If rhinosinusitis is observed for 12 weeks or longer, the severity of symptoms is smoothed out, not counting periods of exacerbation, we are talking about a chronic form. The structure of the mucous membrane changes; with any hypothermia or decreased immunity, especially complicated by an infectious disease, the acute stage returns again. Often, chronic rhinosinusitis in children and adults affects individual sinuses. Nasal congestion, weakness and decreased sense of smell are constant companions of this disease.
Polypous sinusitis
Against the background of a chronic form, to which therapeutic measures have not been applied, polyps may begin to appear - formations from hypertrophied tissue filled with infiltrate. The more they become, the more nasal breathing becomes difficult, so the patient is forced to breathe through his nose. There may be complaints of a foreign body in the nasal passages, pain, stuffy ears and difficulty swallowing food.
- The child’s nose cannot breathe - causes of congestion, diagnosis, treatment with medications and folk remedies
- ENT diseases in adults and children
- Sprays for sinusitis
Allergic
Against the background of prolonged rhinitis, provoked by seasonal allergies, a person may develop allergic sinusitis. It goes away even without the use of antihistamines and is characterized by sneezing, constant itching in the nasopharynx, and redness of the eyes. There may be watery discharge from the nose, swelling that causes difficulty breathing, and skin rashes.
Purulent rhinosinusitis
Purulent rhinosinusitis is a bacterial inflammation of the nasal mucosa and paranasal sinuses. The disease has pronounced clinical symptoms: fever, toothache, purulent nasal discharge, soreness and swelling of the face in the affected sinuses, other signs of intoxication - poor sleep and appetite, muscle pain, aching joints, weakness.
Purulent rhinosinusitis is a dangerous disease that is often complicated by meningitis, abscesses or empyema of the brain and orbit.
Treatment of the pathology is complex, including antibiotics, mucolytics, antihistamines, decongestants, immunomodulators.
Diagnosis of rhinosinusitis
When the first symptoms appear, you need to contact an ENT doctor who will analyze the patient’s complaints and conduct a general examination. If the clinical manifestations of the disease are identical to those characteristic of rhinosinusitis, the doctor will prescribe additional examinations:
- Anterior rhinoscopy (posterior - less often).
- Endoscopy.
- X-ray of the paranasal sinuses - to examine the sphenoid and frontal sinuses.
- Ultrasound – for the diagnosis of cysts, inflammation of the frontal sinuses.
- Computed tomography – to assess the anatomical features of the nose.
- Laboratory identification of the pathogen - the most reliable is a diagnostic puncture of the maxillary sinus, but bacterial culture of the exudate contents, a blood test, and a smear for eosinophils may be required.
Diagnostics
The diagnosis of the disease is made by an ENT doctor based on the patient’s complaints, assessment of the general condition, otolaryngological examination, results of laboratory and instrumental studies.
- After listening to the patient’s complaints and collecting anamnesis, the doctor proceeds to a physical examination, during which he palpates the forehead and cheekbones. This allows you to determine local soreness and detect abnormalities in the nasal cavity.
- An otolaryngological examination includes rhinoscopy, otoscopy and pharyngoscopy.
- Microbiological examination of nasopharyngeal discharge and sinus contents allows us to identify the causative agent of the disease, identify it and determine its sensitivity to antibiotics.
- Additional instrumental research methods: computed tomography, radiography, magnetic resonance imaging.
How to treat
Therapeutic measures should be aimed at eliminating the pathogenic microorganisms that provoked sinusitis (if it is not caused by injury) and affecting the symptoms. For this purpose, drainage of the sinuses is carried out - conservative or surgical, depending on the severity of the disease, and antiviral or antibacterial drugs are necessarily used. Additionally, immunomodulators are needed. You can add to symptomatic therapy:
- regular ventilation of the room;
- maintaining optimal humidity;
- drinking plenty of fluids (there is intoxication of the body).
Drug therapy
If rhinosinusitis is not complicated by a bacterial infection or pus, there is no need for antibiotics: they are mainly recommended for severe stages, especially if the inflammation has gone to the frontal sinuses, to prevent brain damage. Often, penicillin and cephalosporin series are prescribed, or macrolides, which destroy protein synthesis in the cell of the pathogenic bacterium. In other cases, complex drug treatment of rhinosinusitis consists of:
- Mucolytics - to liquefy the contents of the sinuses.
- Hormonal drugs (topical steroids) - for 3 weeks.
- Antiviral drugs - Anaferon, Amantadine, etc.
- Vasoconstrictor drops - for a short period of time to restore the outflow of sinus contents and eliminate swelling.
Surgical methods
The most common method of surgical treatment of rhinosinusitis is puncture (puncture) of the maxillary sinuses. It is performed under local anesthesia and is prescribed mainly for sinusitis with severe pain and large accumulation of fluid. The procedure involves washing the maxillary sinuses with an antiseptic and then administering the medicine. The patient's condition quickly improves, the inflammation is eliminated, but several procedures are needed for a complete cure, and the atypical structure of the sinuses can provoke complications. The following may also be prescribed:
- YAMIK catheter is an alternative to puncture for frontal sinusitis and ethmoiditis, a non-invasive intervention. An antiseptic substance is fed into the sinus through a probe, after which the medicine is injected there. This way you can clear all the sinuses, but you also need several procedures to achieve a complete cure for sinusitis.
- Removal of polyps: Endoscopy - insertion of a surgical instrument into the sinus through the nasal passage, healthy tissue is not damaged, the risk of relapse is reduced by 50%.
- Sinusotomy - through opening the facial bone and removing part of it. The downside is the long rehabilitation period and the presence of a large number of contraindications. Recurrence of sinusitis cannot be ruled out.
Non-drug methods
Nasal rinsing is the main procedure that helps fight rhinosinusitis, which is carried out using saline or sea water on a schedule at intervals of 1-2 hours. It helps remove leakage and affect inflammation. If sinusitis was preceded by odontogenic sinusitis, mouth rinses will be required. In addition to saline solution, herbal decoctions are used for this purpose. Additionally, the doctor may prescribe physiotherapy:
- UHF;
- electrophoresis;
- laser treatment;
- exposure to diadynamic currents.
Stages of the disease
Depending on how long the clinical symptoms last, the following forms of rhinosinusitis are distinguished:
- acute – the disease lasts for at least one month, and the symptoms are pronounced;
- subacute - a person is sick for about three months, but after recovery the symptoms completely stop;
- recurrent - the duration of symptoms is more than 10 days, and such episodes can occur up to 4 times a year;
- chronic rhinosinusitis – bothering a person for more than 3 months.
Treatment of sinusitis in children
Pediatric sinusitis therapy involves an emphasis on topical medications, even if these are antibiotics. It is advisable to use vasoconstrictors (Otrivin, Nazivin) only before bedtime, 1-2 drops into the nasal passage. Doctors try not to use steroids and NSAIDs in children. Mostly children from 2.5 years old are prescribed:
- Bioparox – 1 press for each nasal passage 4 times a day.
- Polydexa - 1 injection into the nostril 3 times a day, the course of treatment is 5 days.
- Protargol is a local antiseptic, 3 drops are administered into each nasal passage up to 3 times a day.
Treatment of the disease
The main principle of treatment is a local effect on the source of inflammation, as well as work to improve the protective functions of the body. The doctor’s task is to help destroy the causative agent of the disease, prevent complications and cases of relapse, and reduce the duration of symptoms.
Before starting to treat rhinosinusitis, doctors must conduct an instrumental examination, collect the patient’s medical history, and conduct laboratory tests.
Characteristic clinical manifestations suggest the use of antibacterial therapy. If there is purulent inflammation, antibiotics must be prescribed.
To cure chronic rhinosinusitis, physiomagnetic therapy and laser treatment are used to relieve swelling, in addition to special means. The contents of all sinuses must be removed, and allergens must also be dealt with.
If you have to deal with maxillary rhinosinusitis, puncture and cleaning are very often resorted to, since they are quite easy to perform. This makes it possible to rinse the sinuses from accumulated secretions, as well as treat them with antiseptic agents.
Depending on the current situation, the clinic may recommend rinsing the nose with solutions, performing so-called nasal showers, and being treated with ultrasound, microwaves or ultra-high-frequency current.
How to treat rhinosinusitis in adults
Rinsing the nasal passages can be done with a simple saline solution or take Aqualor or Aquamaris spray (they are also recommended for children). Vasoconstrictor drugs are selected based on phenylephrine, naphazoline, tetrizoline - these are Sanorin, Vibracil, Otrivin. However, the basis of drug therapy is:
- Antibiotics for bacterial infections - Erythromycin, Augmentin, Ceftriaxone.
- Antipyretics for fever - Paracetamol, Nurofen.
- Topical corticosteroids to relieve inflammation and swelling - Beconase, Alcedim.
- Mucolytics – Fluditec, Fluimucil.
Manifestation of rhinosinusitis during pregnancy
During such a delicate period, a woman’s body experiences hormonal changes, so the nasal mucosa may swell. Discharge and bleeding appear from the nose. In addition, the cause may be a respiratory viral infection.
The manifestation of the disease is discomfort in nasal breathing for 10 days or more. So, the attending physician understands that a complication of simple rhinitis has developed into rhinosinusitis. The respiratory function becomes very complicated, so a specialist may prescribe the use of vasoconstrictor drugs.
Traditional methods
In addition to drug treatment, you can use procedures from traditional medicine: the main one is steam inhalation. They are performed for chronic sinusitis without fever. You need to breathe hot steam for 10-15 minutes, using a decoction of sage, chamomile or calendula. A couple more recipes for traditional treatment:
- After rinsing, instill thuja oil (1 drop into each passage) 2 times a day, especially if you need to cure rhinosinusitis in a child.
- Mix 1 tsp. honey, baking soda and vegetable oil, warm and soak in the turunda mixture, which should be inserted into the nose for 20-25 minutes. 3 times a day.
- Place Kalanchoe juice daily, 2 drops into each nasal passage.
General principles of treatment
The main goals of treatment for rhinosinusitis are:
- Reducing the duration of the disease.
- Prevention of the development of orbital and intracranial complications.
- Eradication of the pathogen.
From this perspective, the basic method of treating acute bacterial rhinosinusitis (moderate and severe forms) and exacerbation of chronic rhinosinusitis is empirical antibacterial therapy.
The main indications for prescribing antimicrobial drugs include:
- Anamnesis characteristic of rhinosinusitis.
- Severity of clinical manifestations.
- The presence of purulent discharge in the nasal passages.
Antibacterial therapy, taking into account the type and sensitivity of a specific pathogen identified during a bacteriological study, does not at all guarantee success due to the high probability of “traveling” microflora entering the test material during sampling. In addition, the results of in vitro sensitivity studies of the identified microorganism do not always correlate with the clinical effectiveness of individual antibacterial drugs. The reasons for this may be a significant increase in antibacterial activity as a result of the unidirectional effect of the antibiotic and its metabolite and the ability to specifically achieve bactericidal concentrations precisely at the site of infection.
Antibacterial therapy for acute bacterial rhinosinusitis
On an outpatient basis, oral antimicrobial drugs are predominantly prescribed.
Taking into account the spectrum of typical pathogens and Russian data on their antibiotic resistance, the drug of first choice for acute bacterial rhinosinusitis is amoxicillin.
In the absence of a noticeable clinical effect, after three days the drug should be replaced with an antibiotic active against penicillin-resistant S. pneumonia and β-lactamase-producing H. influenzae. In this case, III-IV generation cephalosparins or new fluoroquinolones are prescribed.
If you are intolerant to penicillin drugs (and due to possible cross-allergic reactions, cephalosporins should also not be prescribed), the drugs of choice are macrolides.
If the patient is hospitalized, the parenteral route of administration of antimicrobial drugs is preferable.
Antibacterial therapy for exacerbations of chronic rhinosinusitis
When treating exacerbations of chronic rhinosinusitis, oral amoxicillin/clavulanate is considered the drug of choice.
Alternative drugs (prescribed in case of ineffectiveness of the antimicrobial drugs of choice) currently include fluoroquinolones of the III-IV generations. In patients under 16 years of age, alternative drugs include macrolides. Considering the significant role of obstruction of the natural openings of the paranasal sinuses in the pathogenesis of rhinosinusitis, vasoconstrictor drugs, which are prescribed either locally or orally, are of great importance in its treatment.
In the treatment of acute and chronic rhinosinusitis, herbal medicines that have anti-inflammatory and mucolytic effects are also used.
Puncture and probing of the paranasal sinuses
These methods allow you to rinse the affected sinus with an antiseptic solution, remove pathological secretions from it, and administer medications (antiseptics, proteolytic enzymes, glucocorticosteroids). In some cases, puncture and lavage of the paranasal sinuses can eliminate the blockade of its natural anastomosis. It is believed that regular removal of exudate during purulent rhinosinusitis protects local immune factors from proteolysis and increases the content of Ig and complement in the affected sinus by 2-3 times, stimulating the mechanisms of local antibacterial defense. The most common and easier to perform is puncture of the maxillary sinus. It is most often used in the treatment of rhinosinusitis.
Forced drainage method
The method has certain advantages over treatment with repeated punctures. The presence of a catheter creates an additional path for evacuating secretions from the affected sinus, increases air exchange, and eliminates negative pressure when the natural anastomosis is blocked or acts as a valve.
Other methods
Nasal showers, rinsing the nasal cavity with a warm isotonic solution and physiotherapy (ultrahigh-frequency currents, microwave therapy, ultrasound).
Surgery
Indications for surgical treatment for bacterial rhinosinusitis arise when antibiotic therapy is ineffective and orbital or intracranial complications develop.
In surgical treatment, the prevailing trend is towards minimal invasiveness. Less traumatic functional endoscopic interventions give better results, are accompanied by fewer complications, and are less likely to contribute to the progression of the disease and the development of bronchial asthma than classical operations with radical removal of the mucous membrane and nasal turbinates.
Therapy for fungal forms of rhinosinusitis
For a fungal ball, antifungal medications are not prescribed. Treatment is surgical (endoscopic). Complete removal of fungal masses from the paranasal sinuses guarantees recovery. Treatment of allergic fungal rhinosinusitis is surgical (in the presence of large polyps). Treatment of superficial sinonasal mycosis involves removing the substrate for the growth of fungal mycelium.
Disease prevention
Due to the infectious etiology of sinusitis, the most reliable way of protection remains strengthening the immune system: regular intake of immunostimulants, normalization of work and rest schedules, prevention of vitamin deficiency, moderate physical activity. A few more points:
- stop smoking;
- treat colds in a timely manner, especially for children;
- control the humidity in the room.
Treatment of rhinosinusitis
Treatment of the disease should be carried out after examination and necessary tests as prescribed by the doctor. The best results are achieved by an integrated approach to treatment, which combines not only the use of medications, but also the use of physiotherapeutic methods and traditional medicine. If there is no result and in the presence of certain forms of the disease, surgical intervention will be required.
Drug therapy
Prescription of medications is carried out after analyzing the contents of the nasal sinuses. If bacteria provoke rhinosinusitis, antibacterial treatment is required.
The most commonly prescribed medications are Azithromycin or Clarithromycin. If the temperature persists, antibiotic injections are prescribed. A course is prescribed for 10–14 days.
Alternative Methods
Very often it happens that traditional treatment becomes precisely the inaction on the part of the patient, which leads to a chronic form of the disease. It is important to understand that the implementation of such alternative recipes can only be an auxiliary purpose against the background of official medicine. In addition, some folk remedies are potential allergens for a person with a certain problem.
Before choosing herbal preparations, decoctions, ointments and tinctures, it is better to contact an otolaryngologist and enlist his official support. Folk remedies are best used if there is a genetic predisposition to a characteristic ailment for the purpose of prevention. Such a prescription will be effective and safe, especially if it is combined with walks in the fresh air, giving up bad habits, and moderate cardio exercise.
In conclusion, we can add that chronic rhinosinusitis cannot be treated, but if a problem does arise in the body, it should not be left to chance. You need to contact an otolaryngologist for help and be registered with this highly specialized specialist until complete healing (if it is, of course, possible for a specific clinical picture).
Features of the disease in children and pregnant women
Sinusitis often affects young children, since all of their paranasal sinuses are underdeveloped (their final development occurs around the age of 12), and their immunity is not strong. These factors also make the disease more dangerous because babies are at greater risk of complications and cannot tell what is bothering them. Also, acute purulent rhinosinusitis in children is more likely to turn into chronic.
During pregnancy, the body becomes vulnerable for the same reason – decreased immunity. In addition, the development of rhinosinusitis in pregnant women can be affected by hormonal changes. The danger of the disease in expectant mothers is that it is undesirable for them to take strong medications, and many drugs are generally contraindicated due to their negative effect on the fetus. Therefore, treatment requires a special approach.
Drug therapy
Acute purulent rhinosinusitis responds well to drug therapy. The use of recipes from traditional healers is unacceptable. In this way, the patient will only waste time, and the disease will continue to progress. Therapy is prescribed after a comprehensive diagnostic examination. Usually, for the treatment of purulent rhinosinusitis, doctors prescribe several medications with different effects simultaneously:
- Antibacterial medications have proven their effectiveness in severe infectious processes. They are selected strictly by the doctor, taking into account the type of pathogen and the patient’s health condition. At the initial stage of purulent rhinosinusitis, Amoxicillin is most often prescribed. If he fails to cope with the infectious process in three days, antibiotics of the tetracycline group are selected.
- Antihistamines for rhinosinusitis are used to eliminate increased swelling. They also reduce the amount of mucus produced so that air can circulate freely. Among antihistamines, the following drugs have proven themselves to be excellent: Tavegil, Claritin and Loratadine. To moisturize the mucous membrane with rhinosinusitis, you can use nasal sprays (Polydexa, Vibracil).
- To activate the body's defenses, multivitamin complexes and so-called immunomodulators are prescribed. They have a beneficial effect on all systems and accelerate the process of combating pathogenic flora.
- To reduce inflammation during purulent rhinosinusitis, the following medications are recommended: Nurofen, Paracetamol, Ibuprofen. These drugs not only relieve the disorder, but also fight fever and inflammatory reactions. It is worth noting that long-term use of antipyretics is not recommended.
The presented treatment regimen is considered common for all patients diagnosed with purulent rhinosinusitis. What does it mean? The attending physician, depending on the patient’s condition and the presence of certain symptoms, may slightly modify it. This is why self-therapy is extremely undesirable.
Classification
Modern medicine identifies many types of rhinosinusitis. They are classified according to the time and nature of the flow, location and many other criteria.
- According to the causative agent of infection: bacterial, viral, fungal and mixed.
- According to the location of the inflammatory process: right-sided, left-sided, bilateral.
- According to the type of disease: chronic, acute and recurrent.
- According to the type of inflamed sinus: sphenoiditis, sinusitis, ethmoiditis, frontal sinusitis.
- According to the severity of the course: severe, mild and moderate forms.
Depending on the type of disease and the severity of its course, the doctor selects the necessary course of therapy. If you correctly follow all medical recommendations, coping with rhinosinusitis will not be difficult. How to suspect the development of this disease? What symptoms accompany this?
Symptomatic manifestations
Symptoms of chronic sinusitis are as follows: nasal congestion is noted, which is why a person sleeps poorly; it turns out to be impossible to breathe through the nose, the patient begins to breathe through the mouth; lacrimation; moderate clear or more often purulent snot; decreased or even complete loss of odor perception; There is a constant migration of mucus and pus along the back wall of the pharynx, which gives a taste in the mouth and bad breath.
The voice changes in timbre - it becomes nasal. Pain appears in the area of the affected sinuses. There is a feeling of heaviness of the face and cephalalgia; Analgesics help temporarily and not completely. When the process worsens, the main sign is an increase in all symptoms, as in an acute process.
Nasal congestion increases, snot becomes thick, viscous, and changes color - often greenish or yellowish. Facial algia and cephalgia also become stronger.
There is no fever, but there is a low-grade fever. Increased swelling is present not only in the sinuses and nose, it spreads to the skin of the face: eyelids, cheeks.
Treatment of purulent rhinosinusitis at home
For those who prefer traditional methods of treatment, we have compiled a list of the most popular remedies against rhinosinusitis:
- Plant drops. You can use beet, carrot, onion, garlic, aloe or Kalanchoe juice as antiseptic drops. Instill it from a pipette, 3-6 drops into each nostril 3 times a day. Onion and garlic juice can burn the lining of the nose, so they need to be diluted with water.
- Saline solution. It’s very simple to make: mix 1 liter of boiled or distilled water and 1 tbsp. salt (can be sea salt). Some people also add a couple of drops of iodine. This solution should be rinsed in each nostril using a small bulb, syringe or a special teapot (sold in pharmacies).
- Steam inhalations. Also an accessible and well-known method. For inhalation, it is more convenient to use a steam inhaler (also sold in pharmacies), but you can do it the old fashioned way - breathe over the steam from a pan for about 10 minutes. Many websites recommend adding herbal decoctions or essential oils to water, but doctors claim that this has little effect, because the essence of inhalation is steaming viscous sputum and improving microcirculation in tissues, and for this just steam will do.
- Nasal applications. They help relieve inflammation, relieve some pain and eliminate infection. For example, you can soap a cotton swab with laundry soap and put it in your nostril for 10 minutes, or grate an onion, mix with honey, wrap the mixture in a bandage and also put it in your nose.
- Boosting immunity. To strengthen the body's defenses during illness, it is recommended to take vitamin C or echinacea.
Classification of chronic rhinosinusitis
There are 3 forms of chronic rhinosinusitis:
- no nasal polyps (common inflammation);
- polypous (with nasal polyps);
- allergic rhinosinusitis.
In origin, it can be infectious (viral, bacterial and fungal) and non-infectious (caused by allergies, deviated nasal septum, immunodeficiency diseases, etc.).
This classification has great therapeutic significance, since each type of rhinosinusitis has its own manifestations and is treated differently.
Etiology (pathogens)
The causes of acute rhinosinusitis can be divided into two large groups:
- infectious in nature (caused by numerous bacteria, viruses, fungi);
- allergic nature (appear under the influence of various allergens).
The most common sources that provoke acute catarrhal rhinosinusitis are respiratory viral infections or, simply put, common colds.
By penetrating the paranasal sinuses, viruses can cause inflammation. As a rule, when an infection enters the nasal cavity, the body responds with an instant immune reaction, an increase in the amount of mucus, and the formation of edema. All this leads to difficulty in releasing contents from the paranasal sinuses. Additional favorable conditions are created for the further proliferation of pathogenic microorganisms and the formation of pus.
Some types of bacteria can be constantly present in the human body in minimal quantities. However, they do not cause an inflammatory reaction. But in the event of a decrease in protective functions and the formation of congestion in the paranasal sinuses, these bacteria begin to multiply intensively, often provoking acute purulent polysinusitis.
Chronic inflammation of the paranasal sinuses, inhalation of cold air, vasomotor rhinitis (constant nasal congestion) and even some deodorants are quite capable of triggering acute polysinusitis.
In addition, there are a number of pathological conditions that are predisposing factors for the development of acute rhinosinusitis:
- anatomical features of the nasal cavity (deformed nasal septum, polyps, enlarged turbinates, etc.);
- immunodeficiency state;
- the presence of other diseases (allergic rhinitis, cystic fibrosis, adenoiditis, etc.);
- a certain lifestyle (smoking, diving).
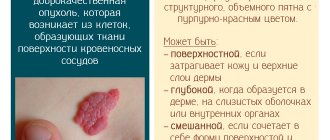
Polypous rhinosinusitis
The mucous membrane of the nasal passages consists of soft tissues. With frequent inflammatory processes, it becomes thinner, and the body, having received a signal about this, begins to grow a new layer. Quite often, these overgrown pieces differ in appearance from the mucous membrane: they are shaped like a drop, and inside they are filled with infiltrate (accumulation of lymph and blood). This formation is called a polyp; it makes nasal breathing difficult and can lead to the development of many diseases.
Polypous growths can be quite large. In this case, constant discomfort is felt, the sense of smell deteriorates, and it seems as if there is a foreign body in the nose. Polyps can also block the sinuses, allowing pus to accumulate in them. This is how polypous rhinosinusitis develops.
Vasomotor rhinosinusitis
The development of vasomotor rhinosinusitis can also begin against the background of an acute viral infection. Its occurrence is associated with disruption of the functioning of nerve endings. When any irritant appears (cold, heat, strong odors), the nasal mucosa reacts quite violently: severe swelling appears, and the discharge becomes very abundant.
Vasomotor rhinosinusitis often develops in pregnant women. This occurs as a result of a sharp change in hormonal levels during pregnancy. Usually after childbirth everything returns to normal even without drug treatment.
Types of rhinosinusitis
In medicine, it is customary to classify diseases. This helps in diagnosis, correct treatment, and selection of medications. Rhinosinusitis is systematized according to several parameters. Types of disease by etiology:
| Pathogens | Note | |
| Bacterial | enterobacteria staphylococcus Pseudomonas aeruginosa, Escherichia coli streptococcus | |
| Viral | rhinoviruses adenoviruses parainfluenza flu | occurs in acute form |
| Fungal | mushrooms of the genus Candida, Aspergillus | several microorganisms infect a cell at once |
| Mixed | begins with a bacterial infection, complicated by other types |
Inflammatory disease is classified according to several parameters. According to the nature of the course, acute, chronic, and recurrent forms are distinguished. Localization of the process can be one-sided or two-sided. The course of the disease varies in severity - mild, moderate, severe. The types of the disease are classified according to the location of the lesion:
- maxillary – sinusitis;
- ethmoidal - parts of the ethmoid sinuses are affected - ethmoiditis;
- frontal – frontal areas are affected – frontal sinusitis;
- sphenoidal – inflamed sphenoid sinuses – sphenoiditis.
Spicy
Diseases in this form begin rapidly and require urgent medical attention. The progression of the patient’s disease occurs over a week. Acute rhinosinusitis has a characteristic clinical picture:
- intoxication – fever, pressure in the ears, feeling of weakness, weakness, fever;
- decreased sense of smell;
- swelling of the face;
- paroxysmal headaches;
- nasality;
- labored breathing;
- bad breath;
- nasal congestion;
- mucous discharge;
- discomfort, squeezing in the sinus area.
If symptoms have not changed within a week, a bacterial infection cannot be ruled out. This condition requires hospitalization and antibiotic therapy. This will help avoid the development of the disease in a chronic form and the occurrence of serious complications. Provoking factors for the occurrence of an acute inflammatory process in the nasal sinuses are:
- incorrect or incomplete treatment of sinusitis;
- disturbances in the discharge of mucous exudate;
- deviated nasal septum.
Chronic
If acute rhinosinusitis is not completely cured, it leads to the development of chronic pathology. The disease can last up to six months. The provoking factors for the occurrence of this form of pathology are:
- allergic reactions;
- severe form of intoxication;
- facial injuries;
- smoking;
- constant inhalation of dusty, polluted air;
- acquired, congenital defects of the nasopharynx.
Chronic rhinosinusitis is characterized by the presence of mild symptoms. This type of disease is dangerous due to the development of complications. The narrowing of the anastomosis between the sinus and nose as a result of edema reduces the supply of oxygen, which intensifies the inflammatory process. The following clinical picture of the disease is observed:
- weakened sense of smell;
- hearing impairment;
- constant nasal congestion;
- lack of temperature;
- nasal voice;
- labored breathing;
- discharge from the nose of mucous secretion with pus;
- distension in the sinuses;
- irritation;
- weakness.
Polyposis
Advanced inflammation of the paranasal sinuses leads to the proliferation of mucous membranes. Chronic polypous rhinosinusitis develops against the background of a decrease in the concentration of immunoglobulin G. The provoking factor is exposure to aggressive chemicals, allergens, viruses, and a hereditary predisposition to allergies. The development of the disease occurs according to the following scheme:
- swelling of the mucous membranes occurs;
- the walls thicken and grow;
- outgrowths are formed - polyps;
- stagnation of purulent contents occurs in the sinuses.
The disease is dangerous due to its complications - meningitis, damage to the eyeballs. Surgical treatment is required - removal of polyps. The clinical picture is characterized by symptoms:
- nasal congestion;
- sensation of a foreign body inside;
- loss or decrease in taste and smell;
- swallowing problems – in advanced cases;
- sleep disturbance;
- tachycardia;
- stuffy ears;
- chronic fatigue;
- pain in the head, sinus area.
Purulent
Rhinosinusitis of this type is bacterial in nature. Often, the activation of pathogenic microorganisms on the mucous membranes of the nose and sinuses occurs due to injury. The disease is dangerous due to life-threatening complications - abscesses, empyema of the orbits, brain, meningitis, and requires hospital treatment. The clinical symptoms of this pathology are clearly expressed:
- purulent nasal discharge;
- fever;
- toothache, headache;
- swelling of the face at the site of sinus lesions;
- sleep disturbance;
- lack of appetite;
- weakness;
- aching joints;
- muscle pain;
- heat.
Allergic
The provoking factors for the development of this type of disease are exposure to allergens. This can be food, medicines, plants, dust, fungal spores, animal hair. Allergic rhinosinusitis requires the exclusion of irritants that lead to the disease and the use of antihistamines. The disease is distinguished by clinical symptoms:
- redness of the eyeball;
- copious clear exudate from the nose;
- lacrimation;
- itching in the nasopharynx;
- irritability;
- malaise;
- headache;
- drowsiness;
- sneezing.
Catarrhal
A disease that occurs without purulent discharge is also called viral runny nose. Catarrhal rhinosinusitis is distinguished by abundant and transparent mucous exudate. The disease is provoked by:
- fungal, viral infections of the upper respiratory tract;
- neoplasms, polyps in the nasal cavity;
- weakened immunity;
- deviated nasal septum;
- hypothermia;
- dental infections;
- allergies.
The inflammatory process is dangerous with complications and requires timely treatment to eliminate them. The disease has a clinical picture:
- elevated temperature;
- swelling of several sinuses;
- nasal congestion;
- inflammation of the conjunctiva of the eyes;
- loss of smell;
- dryness, burning sensation in the nasal cavity;
- hypothermia;
- headache;
- swelling;
- profuse lacrimation;
- lack of sleep.
Vasomotor
If the tone of the blood vessels in the paranasal sinuses and nasal cavity is disturbed, swelling of the mucous membranes occurs. Vasomotor rhinosinusitis begins against the background of colds and acute respiratory viral infections. Provoke the development of the disease:
- frequent use of nasal drops;
- stressful situations;
- changes in hormonal levels;
- smoking;
- changes in air temperature;
- hypothermia;
- alcohol consumption;
- chronic stomach diseases;
- anatomical pathologies of the nose;
- injuries.
Sudden dilation of blood vessels leads to the appearance of edema, while the clinical picture of the disease is characterized by constant nasal congestion, watery mucous discharge, which turns into green exudate as the disease progresses. Symptoms observed:
- nasal voice;
- sneezing;
- lacrimation;
- labored breathing;
- decreased sense of smell;
- headache;
- lack of appetite;
- sleep disorder;
- temperature increase.
Flushing efficiency
When dealing with chronic rhinosinusitis, rinsing the nose with special solutions is very effective.
In the clinic, in the ENT doctor’s office, they perform nasal lavage according to Proetz. People most often call this procedure “cuckoo”. A tube is inserted into one nostril to administer the rinsing solution, and a tube is inserted into the other, through which the liquid will be sucked out by a compressor unit. During rinsing, the patient must repeat “peek-a-boo” so that the solution does not enter the oropharynx. A more modern method is flushing using a YAMIK catheter. Unfortunately, this catheter is not available in all medical institutions, but the procedure can be a real alternative to a painful puncture of the maxillary sinus. First, local anesthesia of the nose is performed. Then a rubber catheter is inserted into the nasal passage and both balloons are inflated. One of them is located in the nostril, and the second in the nasopharynx. As a result, the nasal cavity is hermetically sealed. A syringe is inserted into a special outlet of the catheter and the contents of the sinuses are sucked out. The medicine is injected with another syringe. The YAMIK catheter, without violating the integrity of the mucous membrane, provides access to all paranasal sinuses. Of course, it will not be possible to empty all the sinuses at once, but in 5-6 procedures they will be cleared.
If the maxillary sinus is filled with pus, the patient suffers from headache and facial pain. When rinsing does not help, a puncture is necessary. Under local anesthesia, the thinnest wall of the maxillary sinus is pierced with a special thin needle. First, an antiseptic solution is injected there, and at the end the sinus is filled with medicine.
The procedure allows you to quickly cleanse the purulent contents of the maxillary sinus, alleviate the patient’s condition and administer an antibiotic directly to the point of inflammation.
Most likely, to completely cleanse the sinuses you will have to repeat the procedure several times. A puncture is possible only in case of sinusitis; treatment of other sinuses with this method of treatment is not feasible.
Treatment of chronic rhinosinusitis often includes lavage and punctures. Unpleasant and painful procedures will have to be repeated several times. To avoid suffering yourself, do not let a runny nose take its course. If it does not go away on its own within a week, visit an otolaryngologist and get treatment.
The essence of pathology and its causes
When a runny nose occurs, purulent secretion does not begin to be produced immediately. At first, the discharge is almost completely transparent. If the disease is characterized only by bacterial etiology, then with proper therapy it will not turn into a purulent form. Usually people don’t pay attention to a runny nose and believe that the disorder will go away on its own. In a patient with good immunity, the elements of the body immediately attack the pathogenic flora and eliminate it. In this case, the purulent secretion from the nasal cavity first becomes milky and thickens, and after about 3 days it finally disappears. Thus, the pathological process does not occur in everyone. A runny nose in almost all cases is accompanied by severe swelling of the mucous membrane and rapidly developing inflammation against the background of the activity of the following factors:
- inhalation of carcinogenic substances during smoking;
- the presence of respiratory ailments;
- the presence of fungi in the nasal cavity;
- allergic reactions;
- uncontrolled use of medications;
- proliferation of adenoids;
- the presence of cystic formations or polyps;
- disruption of the functioning of the endocrine system.
Due to severe swelling, excessively narrow passages are blocked. Therefore, the purulent secretion is not released freely, and full air circulation stops. Due to the lack of sufficient oxygen volumes, pathogenic flora begins to multiply in the cavities. The main product of its vital activity is purulent secretion. It begins to accumulate in the sinuses, significantly increasing inflammation. At the same time, the liquid puts constant pressure on their nerve endings. As a result, when lifting or turning the head normally, the patient experiences painful discomfort. If treatment for purulent rhinosinusitis is not started in a timely manner, the likelihood of complications increases. The secretion, under its own weight, can be “pushed” further into the cavity, spreading to neighboring sinuses and ears.
Negative consequences progress very quickly, and sometimes even lead to death.
Diagnosis of the disease
Symptoms and treatment of acute rhinosinusitis in adults are interrelated. Therefore, before prescribing various medications, the doctor must study all the patient’s complaints, as well as conduct a series of diagnostic tests. After all, different forms of the disease are treated differently. In addition, other diseases of the nasopharynx (measles, whooping cough, scarlet fever and others) manifest similar symptoms.
After contacting a specialist, the patient must describe his feelings as accurately as possible. He must say how long ago the nasal congestion began, whether there is heavy discharge, and whether it is purulent in nature. The patient must note whether he has headaches and how intense they are. During a conversation with the patient, the doctor may ask additional questions regarding the course of the disease.
Then the doctor conducts a general examination. To do this, he feels his forehead and cheeks and beats them. If severe pain appears during this, the doctor can make a preliminary diagnosis - frontal sinusitis or sinusitis. If there is severe swelling in the cheeks and eyes, there is a high probability of severe sinusitis. In this case, immediate hospitalization of the patient is required. However, to make a final diagnosis, the doctor must conduct additional diagnostic tests, which include:
- Rhinoscopy, or general examination of the nose. With rhinosinusitis, the nasal mucosa is red and swollen, and purulent or mucous discharge is observed in the passages.
- Endoscopic examination. This is a method that is an alternative to radiography. If purulent discharge is found in the middle nasal passages, the doctor diagnoses sinusitis or frontal sinusitis. When pus is present in the upper tract, the likelihood of ethmoiditis or sphenoiditis is high.
- Radiography. Using this method, you can determine whether there is a pathological process in the paranasal sinuses. If they are filled with mucus or pus, the sinuses will appear dark on an x-ray. Depending on the form of darkening, the doctor distinguishes catarrhal sinusitis from purulent sinusitis.
- Puncture of the maxillary sinus. The procedure is quite unpleasant and painful, so it is carried out using an anesthetic . The maxillary sinus is pierced with a thin long needle and its contents are drawn out with a syringe. Then the sinus is washed and the medicine is injected into it.
- Ultrasound. It is rarely used to diagnose rhinosinusitis, since it is not always possible to make an accurate diagnosis using ultrasound.
- CT scan. It is also rarely used because this method is expensive.
The material taken during puncture is used to determine the bacteria that became the causative agent of the disease. The analysis also allows you to determine whether the microorganism is resistant to antibiotic drugs. The doctor begins to treat rhinosinusitis only after an accurate diagnosis and determination of the form of the disease.
Prognosis and complications
Purulent rhinosinusitis is a dangerous disease, so treatment should not be neglected. If measures to eliminate the disease are applied immediately after its discovery, and you strictly follow the doctor’s instructions, then the disease will leave the body within 7-10 days.
An unfavorable prognosis is given to patients who consulted a doctor late (when there are already complications or they are inevitable), ignored prescribed treatment regimens, gave preference to traditional medicine and severely advanced the disease.
Among the complications of purulent rhinosinusitis are the following diseases and conditions:
- Meningitis;
- Otitis;
- Sepsis;
- Bacteremia;
- Pyemia;
- Periostitis, osteomyelitis;
- Purulent periodontitis, pulpitis;
- Inflammation in the middle and lower respiratory tract;
- Cellulitis of the cellular spaces of the head;
- Abscesses in the maxillofacial area;
- Neuritis of the trigeminal and facial nerve;
- Secondary damage to the kidneys, liver, cardiovascular system.
Although many of these ailments appear rarely as complications of rhinosinusitis, they are very dangerous and should not be discounted.
Treatment of purulent sinusitis
It is important to consult an otolaryngologist at the first manifestations of the disease, since only a doctor can make an accurate diagnosis and, in accordance with it, determine how to treat sinusitis in a particular case. In general, treatment of pathology should be comprehensive and may include:
- use of medicines;
- rinsing the nasal cavity (saline or antiseptic solution, etc.);
- physiotherapeutic procedures – electrophoresis, UHF therapy;
- minimally invasive treatment techniques – use of the YAMIK sinus catheter, balloon sinuplasty;
- puncture (puncture) of the sinus;
- opening of the affected sinus.
The list of medications prescribed to patients with purulent inflammation of the paranasal sinuses includes:
- antibiotics in the form of injection solutions and tablets. The selection of an effective drug is carried out after receiving the results of microflora culture. The study allows us to determine which group of antibacterial agents the bacteria that cause inflammation are most sensitive to. In some cases, antibiotic sprays are sufficient. They act directly at the site of inflammation and in extremely rare cases lead to the development of adverse reactions;
- vasoconstrictors. The use of this group of drugs should not exceed 7 days; a longer course can lead to atrophic changes in the nasal mucosa and the development of addiction to the active components. In adults, such drugs are used in the form of sprays, in children - drops;
- anti-inflammatory drugs;
- antifungal drugs. They are prescribed in cases where the cause of the development of pathology is a fungal infection.
Washing the nasal cavity using the Cuckoo method is carried out by a doctor in a physiotherapy room. The medicine is poured into one nostril of the patient, and a suction is installed into the other. To prevent the solution from getting into the pharynx, during the procedure the patient says “ku-ku,” which helps the soft palate adhere to the back wall of the pharynx. Thanks to this, the drug enters directly into the sinuses, and the mucus and purulent exudate that have accumulated in them are washed out.
In the absence of timely treatment of this form of inflammation, complications may develop in the form of meningitis, osteomyelitis, abscess, tracheitis, bronchitis or pneumonia.
At home, for rinsing, antiseptic agents or a saline solution can be injected into the nasal cavity using a syringe without a needle, a syringe, or a nasal douche.
Physiotherapeutic procedures are used to eliminate the inflammatory process, reduce intoxication, improve microcirculation, and also to activate metabolic processes in affected tissues. Their implementation during purulent inflammation is contraindicated in cases where the outflow of secretions is impossible.
The use of the YAMIK sinus catheter in some cases allows you to avoid puncture
Minimally invasive treatment techniques are used to stimulate the outflow of secretions from the sinuses. They are highly effective, and the risk of complications during their implementation is minimal. These techniques include:
- YAMIK procedure is a procedure performed under superficial anesthesia of the nasal mucosa, which is carried out using a catheter with two balloons. The first is located at its end and is necessary for insertion into the nostril and removal into the nasopharynx, and the second, in the middle of the catheter, remains directly next to the nostril. The device is also equipped with two lumens. A syringe is attached to the first, which is used to inject air to seal the nasal cavity. A syringe is connected to the second, through which an antiseptic solution is injected. The procedure allows you to remove the contents from the sinuses without surgical intervention;
- Balloon sinuplasty is a minimally invasive method of treating sinusitis, in which a conductor with a special balloon is inserted into the anastomosis of the nasal sinus. The procedure is performed under local anesthesia and endoscopic control. The balloon is filled with liquid, which helps open the lumen for the evacuation of pus.
The question of whether a puncture is necessary is decided by the doctor after assessing the effectiveness of the therapy and the risk of complications.
Puncture is one of the most effective and fastest methods for extracting pus from the affected sinus. Its implementation is justified in the following cases:
- the purulent process occurs in one or more sinuses with the outlet closed;
- the drug treatment was ineffective;
- the patient complains of severe headache that cannot be treated with medication;
- body temperature does not decrease after taking antibiotics for three days.
The puncture also has an important diagnostic value, since it allows one to assess the patency of the sinus anastomosis and determine the nature of the pathological process. The procedure algorithm differs depending on the cavity in which the inflammation occurs.
The severity of signs of acute or chronic forms of pathology differ. The process may be complicated by the appearance of symptoms of intoxication due to the proliferation of pathogenic microflora.
Opening the affected sinus is performed only in cases where other treatment methods have proven ineffective, the patient's condition is deteriorating and there is a risk of complications.
Also, folk remedies can be used as an auxiliary therapy, but only as prescribed by a doctor, since some of them can aggravate the course of the pathology. For example, heating the nasal cavity, widely used in alternative medicine, is contraindicated in case of purulent inflammation, since heat increases the formation of exudate in the affected sinus.
Treatment at home
Most people prefer to be treated at home. This is quite acceptable if the disease is not advanced and the doctor does not see the need for hospitalization. In this case, prescribed medications are used and physiotherapeutic procedures are performed.
During the treatment period, it is best not to go to work or study, as this can negatively affect the course of the disease and lead to complications. Drink more warm water, ventilate the room, provide yourself with bed rest.
Antibiotics
Since the infection is caused by bacterial microorganisms, it is necessary to use antibiotic drugs. For any purulent infection, doctors must examine the exudate in the laboratory (Gram staining, culture, determination of the strain of the pathogenic microorganism and the antibiotic to which it is sensitive). Ideally, antibiotics are prescribed to which specific microflora are sensitive. But the most widely used drugs are broad-spectrum drugs from the following groups:
- penicillins (Augmentin, Amoxicillin),
- macrolides (Erythromycin, Azithromycin),
- cephalosporins (Ceftriaxone).
- fluoroquinolones (Cefazolin),
Such drugs are considered systemic and potent, so their use should always be discussed with your doctor.
Local antibiotics
We are talking about nasal drops and sprays with an antibiotic effect. Although there are a variety of drugs on the market, the most common are sprays:
- Isofra.
- Polydexa.
Polydexa contains two antibiotic components, anti-inflammatory and vasoconstrictor. This drug is used for more advanced clinical cases. Isofra contains only one antibiotic component, therefore it is used mainly for mild to moderate severity of the disease.
Saline solutions
Preparations such as Physiomer, Humer, Marimer are prescribed to moisturize the nasal mucosa, reduce the density of exudate and its rapid removal. They do not have a therapeutic effect, but they help the pus to quickly exit the sinuses and remove from the walls of the nose.
Vasoconstrictor drops
If you have not used vasoconstrictor drops before treatment, your doctor may prescribe them for a couple of days to facilitate nasal breathing until the illness partially subsides. Such drugs include:
- Naphthyzin,
- Nasonex,
- Galazolin,
- Nazol,
- Nazivin.
Antihistamines and anti-inflammatory drugs
A notable feature of antihistamine-type drugs is the ability to quickly remove swelling in tissues and mucous membranes. Therefore, they are prescribed if the swelling is very severe and it is not possible to eliminate it with the help of vasoconstrictor drops. Antihistamine drugs include Loratadine, Aleron, Cetrin. All of them are sold in tablets.
Non-steroidal anti-inflammatory drugs. Ibuprofen, Paracetamol, Diclofenac, Mefenamic acid and other medications of this type help relieve symptoms of inflammation in the sinuses and eliminate symptoms of intoxication.
Homeopathic remedies
Herbal preparations help the exudate become more liquid and leave the sinuses faster. This effect speeds up recovery and also prevents the occurrence of complications of the disease. Well-proven remedies include Sinupret, which is sold in the form of drops for internal use and tablets.
The doctor may prescribe other drugs for self-administration at his own discretion, based on medical history and indications.
Treatment at home with traditional medicine recipes is also possible. But you should not get carried away with them - if no positive dynamics are observed for several days, consult a doctor immediately. Acute purulent infections entail terrible complications that are best not to be dealt with.
Possible complications
Violation of the correct treatment can lead to the following complications: inflammation expands to involve the soft tissues of the face and respiratory tract;
- otitis;
- eye complications (purulent inflammation of the eye sockets, leading to loss of vision as a whole).
- complications from the brain and skull: brain abscesses; inflammation of its membranes; osteomyelitis;
- Cavernous sinus thrombosis (accumulation of blood in the dura mater); symptoms include cephalgia, bulging eyes, convulsive syndrome, and other central nervous system disorders.
- sepsis;
- cholesteatoma - the appearance of a cavity with dead epithelial cells surrounded by a connective tissue capsule;
- osteomyelitis;
- mucocele - the formation of a cyst inside the sinus due to obstruction of the excretory duct;
- inflammation of the periosteum (periostitis); pain in the corner of the eye and root of the nose;
- exophthalmos (bulging eyes);
- chemosis - the eyelid line and conjunctiva become swollen.
With sufficient treatment, complications of this kind are rare. Complications can also arise in the form of diseases of the nasopharynx and larynx. These are chronic pharyngitis, laryngitis, tonsillitis, dacryocystitis (inflammation of the nasolacrimal duct); a constant lack of oxygen causes a decrease in memory and attention; constant daytime sleepiness. Due to nasal congestion, air cannot pass into the nasal cavity and apnea may occur - stopping breathing during sleep - obstructive sleep apnea syndrome (OSA).
Causes
Rhinosinusitis is a pathology in the development of which many factors are involved:
- Reduced immunity (due to weakening of the body’s defenses, pathogenic and opportunistic microorganisms can cause inflammation).
- Pathogenic strains of pathogens.
- Congenital and acquired defects of the nasal cavity and its septum, preventing the passage of air and the discharge of mucus (the accumulation of microorganisms triggers the infectious process).
- Anomalies of the outlet openings of the paranasal sinuses.
- Polyps, tumors of the nasal cavity or skull bones that form the sinuses.
- Dental manipulations leading to the spread of infection (manifested by sinusitis).
- Secondary rhinosinusitis (due to late detection or treatment of infectious diseases).
Thus, the trigger mechanisms of the infectious process are:
- Viral infections (rhinovirus, picornavirus, coronavirus, respiratory syncytial)
- Bacterial infection (caused by streptococci, staphylococci, moraxella)
- Allergic reactions (occurs against the background of sensitization of the body to allergens, through which pro-inflammatory cytokines are activated and aseptic inflammation develops)
An integrated approach to treatment
For a quick recovery in the treatment of sinusitis, multicomponent therapy is used, it includes:
- Etiotropic treatment - affects the etiological factor, that is, viruses, fungi or bacteria;
- Pathogenetic treatment - affects the process of disease development;
- Symptomatic treatment - reduces or completely eliminates the symptoms of the disease.
Viral rhinosinusitis
Acute rhinosinusitis usually goes through two stages in its development: viral and bacterial. At the viral stage, pathogenic viral agents attach to the mucous membrane, causing its swelling and increased exudation, that is, the formation of discharge.
Not only the nasal mucosa and paranasal sinuses are involved in inflammation; simultaneously with rhinosinusitis, the patient may be bothered by:
- Conjunctivitis (watery eyes);
- Pharyngitis, tracheitis (cough, hoarseness);
- Enterocolitis, colitis (abdominal pain, stool upset).
Cough, nasal congestion, lacrimation - symptoms of viral rhinosinusitis
Digestive upset due to viral rhinosinusitis is more typical for children, but sometimes occurs in adults.
To treat viral rhinosinusitis in adults, you do not need to take antibacterial drugs, because antibiotics are not effective against viruses. At this stage of the disease, pathogenetic and symptomatic treatment is sufficient (they will be discussed below).
Antiviral drugs are most effective when taken from the first days of the disease:
| Interferon inducers | Anaferon, Kagocel | |
Interferon preparations:
| Genferon, Viferon, Lactoferon; Genferon Light. |
According to the latest instructions for the treatment of viral rhinosinusitis, the administration of nasal steroids, mainly containing mometasone - Nasonex, Maurice, is effective. These drugs have an anti-inflammatory and anti-edematous effect, thus facilitating the drainage of the sinuses and inhibiting inflammation of the mucous membrane. More details about nasal steroids later in the article.
Acute bacterial rhinosinusitis
Swelling of the mucous membrane, copious discharge, a block of natural anastomosis between the sinus and the nasal cavity contributes to the proliferation of microorganisms and the development of the bacterial process.
According to the latest recommendations, there are several symptoms that indicate a transition to the bacterial stage:
- Purulent discharge from the nose, taste of pus in the mouth;
- Unilateral or bilateral nasal congestion;
- Severe pain in the projection of the paranasal sinuses onto the bones of the face.
The appearance of these signs indicates the need to prescribe an antibacterial agent. Antibiotics for rhinosinusitis can be in the form of local or systemic use.
A spray for rhinosinusitis with an antibacterial or antiseptic effect can be used independently or as part of systemic treatment with antimicrobial drugs.
The most commonly used:
| Polydexa with phenylephrine | A combined drug containing antibiotics (Polymyxin and Neomycin), an anti-inflammatory component (Dexamethasone) and a vasoconstrictor component (Phenylephrine). The advantage of this nasal spray over other drugs is the presence of phenylephrine and dexamethasone. These two components relieve swelling, suppress inflammation, improve sinus drainage, and promote healing. | |
| Isofra/Framinazine | The nasal spray contains the topical antibacterial drug framycetin. In order for the antibiotic to achieve its goal, it is recommended to rinse and blow your nose thoroughly before use. Isofra is produced by the Italian company Recordati, Framinazine is a cheaper analogue produced in Belarus. | |
| Albucid (sulfacyl sodium) | The drops are intended for use in ophthalmology and contain an active substance from the sulfonamide group - sodium sulfacetamide. Instillation into the nose together with a vasoconstrictor is allowed. | |
| Protargol (Sialor), Nozosept | The drug contains a silver compound, due to which it has some antiseptic and astringent effect. Not an antibiotic. |
Etiotropic treatment of bacterial sinusitis
If there is no effect from local antibacterial drugs, clinical manifestations increase and the condition worsens, it is necessary to prescribe systemic antibiotics. The range of antibacterial drugs on the pharmaceutical market is very large; the doctor (therapist or ENT specialist) decides which drug to choose.
How to properly treat rhinosinusitis with antibiotics? The choice of antibacterial agent depends on the age of the patient, previous treatment, and the suspected pathogen. There are drugs for initial therapy, “second-line” drugs and reserve antibiotics.
The antibacterial agents of the starting group are:
| Amoxicillin | Amoxicar, Flemoxin, Ospamox |
| Amoxicillin clavulanate | Amoxicar plus, Augmentin, Flemoklav, Amoxiclav |
Oral cephalosporins:
|
|
Parenteral cephalosporins:
|
|
In outpatient settings, it is advisable to use oral cephalosporins to improve adherence and avoid pain.
Modern oral forms of antibiotics are an alternative to painful injections
If treatment is not effective, or the patient is allergic to beta-lactam drugs (cephalosporins or protected penicillins), second-line drugs are used.
These include:
| Macrolides: Clarithromycin | Claricar, Fromilid, Lekoklar |
| Fluoroquinolones: Levofloxacin | Tavanik, Lebel, Leflox |
Other macrolides (Azithromycin, Rovamycin) and fluoroquinolones (ciprofloxacin, ofloxacin) have less activity against pathogenic microorganisms that cause rhinosinusitis. Newer drugs from these groups (Moxifloxacin, Josamycin) are considered reserve drugs.
Fluoroquinolones are contraindicated for use in childhood.
Reserve drugs are reserve antibiotics that are used when previous drugs are ineffective or complications develop. This group can include some fluoroquinolones (moxifloxacin, gatifloxacin), macrolides (josamycin, midecamycin), carbapenems (meropenem, imipenem, Tienam). Reserve drugs are prescribed to severely ill patients, mainly in a hospital setting.
Do not self-medicate, do not prescribe antibiotics for yourself or your loved ones without a doctor’s recommendation! An antibacterial agent that remains from a previous treatment in a home medicine cabinet may be ineffective, toxic, or completely contraindicated for use in a particular case of the disease.
Pathogenetic treatment
To interrupt the development of the disease, it is necessary:
- Ensure sufficient drainage of discharge from the sinus. For this purpose, antihistamines are prescribed.
- Reduce the volume of pathological discharge;
- Reduce swelling of the tissues in the nose and paranasal sinuses. For this purpose, antihistamines, vasoconstrictor nasal drops, and nasal steroids are used.
Antihistamines
Antiallergic drugs reduce swelling of the mucous membrane in the nose and sinuses, reduce the amount of discharge, and promote the opening of natural anastomoses between the nasal cavity and paranasal sinuses.
| Loratadine | Claritin |
| Desloratadine | Erius, Lordes |
| Hifenadine | Fenkarol |
| Cetirizine | Tsetrin |
Rhinoscopic picture of swelling of the inferior turbinates
Secretolytics
Medicines that have a secretolytic effect dilute the discharge in the sinuses and facilitate its removal. The most commonly used herbal preparations are: Sinupret (in the form of syrup, drops or dragees), Cinnabsin, Sinustrong. In addition to them, you can use medications based on carbocysteine (Fluditec, Fludicaf) or acetylcysteine (ACC, Acetsex).
Vasoconstrictor nasal drops
On the pharmaceutical market, nasal drops are represented by a huge variety of medicines. Most of them have naphazoline/oxymetazoline/xylometazoline as the active ingredient, for example Nazol, Nazivin, Xylin, Snoop and others.
The advantage of these drops is their rapid action, the disadvantage is the rapid addiction and development of medicinal rhinitis. It is not recommended to use these drops for more than 5 days; in addition, they are not recommended for use in children under one year of age and in pregnant women.
With prolonged use of vasoconstrictor drops, the nasal mucosa “gets used to the drops”, becomes dry, and may often bleed. First, drug-induced rhinitis develops, and then true hypertrophic rhinitis.
There are known cases of overdose and poisoning with vasoconstrictor drops from the naphazoline/oxymetazoline/xylometazoline group.
The harmless drug Naphthyzin (Naphazoline) can cause serious drug poisoning in children
Phenylephrine has a more gentle effect. It is contained in Vibrocil, Rinocil, Adrianol, Nazol Baby and Nazol Kids drops. Phenylephrine constricts blood vessels and has virtually no systemic effect. Phenylephrine drops are allowed to be used for up to 7 days.
Nasal steroids
There is an international document that regulates the treatment of rhinosinusitis, called EPOS (European Position Paper On Rhinosinusitis and Nasal Polyps). According to him, the most effective use of nasal steroids is the basis for the treatment of viral and bacterial rhinosinusitis.
It is quite difficult for domestic ENT doctors to abandon antibacterial therapy in favor of exclusively nasal steroids, therefore, in their practice, otolaryngologists often use a step-by-step treatment regimen: first antibiotics and other drugs, then nasal steroids as an option for “follow-up treatment.”
Among nasal glucocorticosteroids, preference is given to mometasone preparations: Nasonex, Maurice and others. Unlike earlier generation drugs, mometasone causes less dryness and bleeding of the nasal mucosa.
Symptomatic therapy
Symptoms of rhinosinusitis are varied:
- Nasal congestion, difficulty breathing through the nose;
- Nasal discharge;
- Facial pain;
- Fever, general malaise, weakness.
Many of the previously mentioned drugs have both pathogenetic and symptomatic effects, for example, antihistamines, nasal steroids and nasal drops not only relieve swelling in the nasal cavity, but also facilitate nasal breathing and reduce the amount of nasal discharge.
To relieve headaches, drugs from the group of NSAIDs - non-steroidal anti-inflammatory drugs - are used.
Most often used:
- Ibuprofen: Nurofen, Ibufen, Brufen;
- Paracetamol: Panadol, Efferalgan, Cefekon;
- Nimesulide: Nise, Nimesil, Nisit;
- Analgin and others.
Analgin is not used in some countries due to the possible development of agranulocytosis; Aspirin is undesirable to use as an analgesic due to its ulcerogenic effect. Aspirin can cause nonsteroidal ulcers of the gastric and duodenal mucosa. In addition, Aspirin is contraindicated for use in children due to the risk of Reye's syndrome.
Helper Methods
This group of therapeutic measures includes physiotherapy and various methods of removing discharge from the sinuses.
Physiotherapeutic methods can be used:
- Inhalations - alkaline, phytoinhalations - facilitate the passage of secretions, reduce cough;
- UFO (quartz tube) in the nose - is bactericidal;
- Magnet/Magnetic Laser - relieves swelling, reduces inflammation and pain;
- Bioptron - has an anti-inflammatory effect.
In the photo - treatment of acute rhinosinusitis using the Bioptron device
Thermal procedures for acute rhinosinusitis are contraindicated! You should not warm your nose with salt/egg/hot water bottle, as this may worsen the patient’s condition.
Non-invasive methods are used to remove discharge:
- Sinus rinsing according to Proyets (cuckoo);
- Sinus catheter “YAMIK”;
- Rinsing the nasal cavity using the drugs “Dolphin”, “Humer”, “Aqualor”, Aquamaris devices and others.
The video in this article demonstrates how to properly rinse your nose during acute rhinosinusitis: