Dorsopathy is a pathological condition of the back and muscular frame of the spine, accompanied by pain and characteristic changes in the tissues. According to clinical symptoms, the disease is similar to osteochondrosis, which is why they are often confused. However, dorsopathy has a number of signs and properties that distinguish it from dystrophic processes in cartilage and intervertebral discs.
The most significant of its symptoms is severe pain in the body and limbs, not related to damage to internal organs. Dorsopathy is defined and what it is according to the established formulation
International Classification of Diseases (ICD-10). According to official statistics, the incidence of this type of pathology ranges from 15 to 25% among the adult population aged 30-45 years. The disease is treated with a conservative method. In uncomplicated forms, the disease goes away on its own.
Classification
Dorsopathies can be systematized into several types. Classification depends on which structures are affected by the pathological mechanism.
Table. Classification of dorsopathies.
| Name | Description |
| Deforming dorsopathy | First of all, the disease affects the intervertebral discs, which play the role of shock absorbers of the spinal column. Degeneration of intervertebral cartilage is associated with dystrophic processes due to impaired local circulation. The flow of nutrients and oxygen decreases, and collagen delivery is disrupted. The disc becomes thinner, loses its shock-absorbing properties and regeneration rate under conditions of lack of resources. Due to the reduced height of the cartilage, the vertebrae move closer together and compress the nerve endings. Associated with this are radiculopathy (compression of the nerve roots at the site of their exit from the intervertebral foramina), intercostal neuralgia (pain in the chest area caused by compression of the roots that give rise to the intercostal nerves), sciatica (a symptom complex caused by compression of the sciatic nerve), radiculitis ( inflammation of the roots) and all combinations of pain syndromes (for example, dorsalgia (pain in the chest), cervicalgia (in the neck area), lumboischialgia (in the lower back and in the zone of innervation of the sciatic nerve). The convergence of the vertebrae and degenerative-dystrophic processes initiate anatomical changes, in in particular, various pathological curvatures of the spine: pathological scoliosis, kyphosis; as well as displacements and subluxations of the vertebrae - spondylolisthesis. |
| Spondylopathy | This group of diseases is associated with pathological changes in bone tissue and ligaments of the spine. Both inflammatory and dystrophic processes are involved in the pathogenesis. Spondylopathies include the following diseases: spondylosis, osteoporosis, Scheuermann-Mau disease (dorsal pathological kyphosis, characteristic of young males), ankylosing spondylosis (chronic alteration processes of the spine and joints, the pathogenesis of which is based on inflammation), uncovertebral arthrosis (partial destruction of intervertebral cartilage as a result of chronic degenerative processes), etc. |
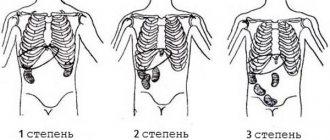
| Discogenic dorsopathy | This group of dorsopathies includes intervertebral hernias and protrusions. With protrusion, only the fibrous rings of the intervertebral discs protrude. Unlike protrusions, with a hernia the nucleus pulposus comes out through the fibrous rings, the integrity of which is broken. |
There are several types of dorsopathies
Dorsopathies can be classified according to the volume of structures that diseases of this group involve. If only one intervertebral disc is damaged, then dorsopathy is limited, and if several are damaged, then it is polysegmental.
Important! Dorsopathies can affect all parts of the spine.
Causes
Dorsopathy syndrome is a consequence of degenerative-dystrophic changes in the spinal column, which accompany the following diseases:
- osteochondrosis;
- intervertebral hernia;
- osteoporosis;
- spondyloarthrosis;
- infection of the spine;
- rachiocampsis;
- fibromyalgia.
The following factors can provoke the development of dorsopathy:
- hypodynamic lifestyle;
- being overweight;
- weak immune system;
- excessive physical activity;
- mechanical damage to the back;
- presence of bad habits;
- poor nutrition;
- exposure to vibration waves;
- staying in one position for a long time;
- hereditary predisposition;
- metabolic disorder.
People suffering from heart pathologies, endocrine diseases or psychological disorders are most susceptible to back pain.
Etiopathogenesis
The most common etiological factors of dorsopathies are diseases leading to degeneration in intervertebral cartilage (osteochondrosis) with spondylosis, facet joints (spondyloarthrosis), ligaments, and also causing myofascial pain syndrome.
Factors contributing to the initiation and progression of dorsopathies include:
- physical inactivity (sedentary lifestyle);
- postural disorders (pathological scoliosis, kyphosis);
- heredity (biochemical, biomechanical, anthropological and other human constitution);
- uneven and inadequate load on the spine;
- improper diet (for example, a predominance of spices, baked goods, fried foods);
- smoking and drinking alcohol;
- constant exposure to vibration or a combination of humidity and low temperatures;
- thyrotoxicosis;
- diabetes;
- diseases of the cardiovascular system;
- long-term and systematic stay in an uncomfortable position;
- congenital anomalies (eg, spina bifida);
- psychological and mental disorders.
The causes of dorsopathies are most often improper load on the spine, consumption of “harmful” foods, and curvature of the spine.
Important! The lumbosacral spine is most often affected, as it experiences more stress than other parts. The thoracic region is least likely to be damaged.
Symptoms of dorsopathy of the thoracic spine
The vertebrae in the thoracic region are connected to the ribs, and through them to the sternum. The thoracic region has less mobility compared to the cervical and lumbar regions, and therefore some pathologies are relatively rare here. Possible symptoms of thoracic dorsopathy:
- Back pain.
- Pain in the heart, “in the internal organs.” This can be misleading: a sick person believes that he has problems not with the spine, but with the heart, stomach, and other organs.
- The pain may worsen during deep breaths. Sometimes it can be very strong, it feels as if “a stake has been driven into the chest.”
Over time, damage to the thoracic spine leads to limited mobility of the chest. Because of this, breathing and heart function are impaired.
Clinical picture
Clinical manifestations of dorsopathy are:
- chronic low-grade pain on the affected side;
- increased discomfort during sudden movements, when lifting weights, during involuntary reflex movements such as coughing and sneezing.
- paresis (absence of a certain voluntary movement due to a violation of the motor tract of the nervous system), hyporeflexia, atrophic changes in the muscles;
- muscle spasms;
- trophic changes in soft tissues or neuromyofibrosis and neuroosteofibrosis.
Neuroosteofibrosis
Neuromyofibrosis and neuromyostenosis are myofascial syndromes. The first is overexcitation of the muscular-fascial zone, which is accompanied by dystrophic or fibrotizing processes and conducting pain when pressing trigger points of the body. Neuroosteofibrosis is characterized by fibrosis at the points of attachment of muscle to bone. The pain is also conductive and is also associated with pressing on certain pain points.
Spasms, chronic pain and paresis are obvious symptoms of dorsopathy
The symptoms of dorsopathies largely depend on the localization of pathological processes.
With cervical spine dorsopathy, the patient complains of:
- pain in the arms, neck;
- migraine;
- dizziness;
- spots before the eyes.
A complication of such dorsopathy may be “vertebral artery syndrome,” characterized by a combination of the above symptoms. The headache is intense and throbbing. The patient may faint.
Thoracic dorsopathy is characterized by:
- intercostal neuralgia;
- radiating back pain;
- fluctuations in heart rate.
Important! May mimic serious cardiovascular disease. Differential diagnosis is necessary, which should be carried out by a specialist.
With lumbosacral dorsopathy, pain is localized in the lower back and radiates to the area of innervation of the nerves that originate from the sacral and lumbar plexuses.
Symptoms may vary depending on which part of the spine is affected
You should immediately consult a doctor if you have cauda equina syndrome (the cauda equina is a bundle of spinal nerves located at the terminal part of the spinal canal). Characterized by tingling and numbness in the groin area and along the inner thigh, disturbances in urination and defecation, weakness of the legs, and sexual dysfunction.
Pain may occur due to compression of the nerve root by protrusions and intervertebral hernias. In this case, the sensation will be sharp and paroxysmal. May be accompanied by hypotrophy (decrease in the volume of muscle tissue) and hypotension (decreased tone) of the innervated muscles. Constant pain, alternating with a corresponding change in posture, is local pain; and spreading in a direction similar to the direction of the branches of the affected nerve - projection. Pain due to muscle spasm and hypertonicity is classified as non-radicular - psychogenic. The pathogenesis of muscular-tonic syndrome is characterized by the presence of a vicious circle. This pathophysiological mechanism, in this case, is as follows: the muscles are spastic in response to pain, and the pain itself intensifies with muscle spasm.
Important! Symptoms are characterized by intensification at night and during sudden movements, including involuntary ones (sneezing, coughing).
Rehabilitation and preventive measures
- Maintaining a healthy lifestyle with physical activity;
- Doing therapeutic exercises, sports exercises without overloading the spine, swimming, stretching the spinal column on a tourniquet, etc.;
- Protecting yourself from carrying or lifting heavy objects;
- Carrying out special small warm-ups for the back during the day;
- Proper and nutritious nutrition;
- Controlling body weight and avoiding weight gain;
- Rejection of bad habits.
Compliance with therapeutic and preventive recommendations will allow you to forget about dorsopathy forever.
Diagnostics
If you have complaints that are typical for dorsopathies, you should contact a vertebrologist. The doctor will first take a medical history. This is an integral part of diagnosis. The patient must answer questions related to the duration and frequency of symptoms; the presence of limited mobility of the limbs, numbness; impairment of performance; a history of spinal surgery and trauma. The specialist palpates the muscles and structures of the spine to identify painful points and spasms; conducts tests to assess range of motion and to identify postures that change the intensity of symptoms. A neurological examination is required at the appointment. Reflexes and motor sensory functions are tested.
Diagnosis of dorsopathies must be comprehensive, since the causes of this phenomenon can be various factors
The following are used as instrumental methods for diagnosing dorsopathies.
- Radiography. The picture is taken in several planes. X-ray is effective for assessing the condition of spinal structures in spondylosis and compression fractures. Allows you to determine the presence of osteophytes and protrusions.
- MRI is the gold standard for soft tissue assessment.
- CT together with MRI is used to diagnose intervertebral discs and pathologies affecting soft tissues and ligaments. These methods allow layer-by-layer assessment of the condition of tissues.
- Bone scintigraphy is a radionuclide diagnostic method and is used to exclude bone tumors and compression fractures associated with osteoporosis.
- EMG is electromyography, which is used to measure electrical impulses coming from the nerves that innervate muscles. The muscle response to nerve impulses is also assessed. An electromyogram will show an altered picture in the presence of radicular syndrome.
- Thermography. The method shows the picture of the distribution of thermal zones, which changes, for example, in radicular syndrome due to a violation of the innervation of the walls of the feeding vessels.
- Ultrasound examination, which is used to detect tears in soft tissues.
Depending on the diagnosis, it may be necessary to consult with a neurosurgeon and orthopedist.
Tumors
Neoplasms affect the vertebrae and can spread into the cavity of the spinal canal. Such structures are benign and malignant, arise directly from the bone or vascular tissue of the vertebra or grow into it from other organs. Tumors produce different symptoms depending on the type and location and the general health of the patient.
The most common symptom is pain, as well as loss of muscle strength, sensation, loss of bowel and bladder control, and scoliosis.
Cancers that affect the vertebrae include osteosarcoma, Ewing's sarcoma, and multiple myeloma.
Benign neoplasms – osteomas, osteoblastomas and hemangiomas.
Regardless of the type, tumors cause prolonged pain, spinal deformation, and neurological disorders.
Malignant formations destroy the body and processes of the vertebrae, exert mechanical pressure on the spinal cord and nerves
Treatment
For dorsopathies, doctors and patients themselves prefer conservative methods. They are aimed at slowing the progression of dystrophic processes, eliminating pain and other symptoms associated with a decrease in the patient’s quality of life. Treatment tactics depend on what kind of dorsopathy the patient has, but in any case he should be provided with rest. For cervical dorsopathy, it is necessary to wear a special Shants collar. The collar is hypoallergenic; consists of a variety of materials, the edges for support are always soft. The collar relieves stress on the neck and limits the range of motion of the neck. Orthoses and corsets are used for a similar purpose. The Shants collar is used as prescribed by a doctor. The specialist determines the required dimensions of this device.
Treatment of dorsopathies is most often conservative
The following means are mainly used.
- Non-steroidal anti-inflammatory drugs (NSAIDs) - which are used to relieve pain and relieve inflammation characteristic of periods of exacerbation of a particular dorsopathy.
- Opioids (such as codeine or morphine). It is prescribed for a short period of time for unbearable pain that is not relieved by analgesics and non-steroidal anti-inflammatory drugs. The patient is under the supervision of medical staff.
- Muscle relaxants and antispasmodics to relieve muscle spasms and pain associated with muscle tone.
- Traction (mechanical traction using special tools) of the spine to increase the distance between the vertebrae. Effective in relieving symptoms associated with compression of blood vessels and nerve roots. Relieves pain and improves trophism.
- Antioxidants.
- Antihypoxants (drugs that reduce tissue oxygen demand and improve its utilization by the body).
- Lidocaine/novocaine blockades.
- Dexamethasone blockades (dexamethasone is a hormonal steroid drug with powerful anti-inflammatory and immunosuppressive properties. A systemic drug).
- Antidepressants and anxiolytics to improve the patient’s general condition and to reduce psychosomatic symptoms.
- Vitamin and mineral complexes, anabolic steroids and physiotherapy to improve the effect of treatment, as well as as rehabilitation measures.
Important! The last point is started only after pain has been relieved. Each remedy is prescribed after consultation with a doctor. Each remedy has contraindications.
Blockades are conservative, but at the same time complex invasive procedures. Carrying out requires an experienced specialist.
Surgical methods are switched to when conservative therapy is ineffective; with the proliferation of bone tissue, leading to stenosis of the vertebral canal and neurological symptoms, as well as with “cauda equina syndrome”.
Alternative methods can also effectively relieve symptoms and causes of dorsalgia.
Alternative methods of treating dorsopathies include the following.
- Acupuncture. Used at all stages of treatment. The method involves inserting needles into bioactive points paravertebrally, on the neck, etc. A variation of this method is hot acupuncture. At the same time, the needles heat up. Acupuncture is used to relieve inflammation and pain. Effective for restoring sensitivity and relieving swelling.
- Acupressure. Acupressure is based on intense pressure on painful and biologically active points. As a result, muscle tension is relieved, local circulation is improved, and therefore the flow of oxygen, nutrients and the supply of structural proteins.
- Moxibustion therapy. In other words, thermotherapy. The method is effective for relieving muscle spasms and quickly restoring intervertebral cartilage. There are two types of moxotherapy: non-contact and contact. In the first case, the procedure is carried out using special miniature cigars, and in the second - with cones. Non-contact therapy is used more often and is based on remote exposure to a heat source until the skin area reddens. Contact therapy may cause burns.
- Manual therapy, in other words, manual pulling. The effect is the same as with mechanical traction. Most effective for deforming dorsopathies.
- Osteopathy. Osteopathy is based on the use of hands on the spine. Moreover, the manipulations themselves are carried out not only locally, but also affect structures that affect the biomechanical properties of the spine. This method is less controversial from the point of view of classical medicine compared to manual therapy. It is characterized by an almost complete absence of contraindications.
- Vacuum therapy, otherwise known as cupping massage. Helps improve local blood circulation and relax muscles. Slows down processes associated with trophic disorders. A variation of this method is used - magnetic vacuum therapy with a combination of acupuncture.
- Hirudotherapy. Use of medicinal leeches. Their placement in the spine area to change the rheological properties of blood. Hirudotherapy is effective for eliminating congestion and improving blood circulation. Has anti-inflammatory and analgesic effects.
- Stone therapy - warming up the back and massage with hot stones. Improves blood circulation, relaxes muscles, accelerates metabolism in muscles and other tissues.
- Therapeutic massage and physical education, herbal medicine are used as additional therapeutic methods.
- Cryotherapy is a physiotherapeutic therapy that is based on the response of the skin surface to cold.
Before resorting to alternative medicine, you should consult your doctor.
Important! Before using any alternative method, you should consult your doctor.
Symptoms of dorsopathy of the cervical spine
Characteristic manifestations of damage to the cervical spine:
- Headaches, pain in the neck, shoulders, arms.
- Dizziness.
- Noise, ringing in the ears. “Floaters” and colored spots flash before your eyes.
- Feeling of numbness, weakness in the arms.
- Tension in the muscles of the neck and shoulder girdle, a feeling as if “someone was riding on your shoulders.”
Forecast
As with other diseases, the prognosis for dorsopathies is favorable if you immediately consult a doctor for any of the symptoms listed above. You can contact a neurologist, vertebrologist, orthopedist, neurosurgeon, or a local doctor, who will refer you to the right specialist.
The treatment will be successful and without complications if you seek help in time
Fortunately, in most cases, surgical intervention is not required for dorsopathies. Conservative therapy is sufficient. But you cannot prescribe medications yourself. Self-medication can lead to a poor prognosis, including disability. Moreover, it should be remembered that there are many diseases that are classified as dorsopathies. First of all, they need to be differentiated. The result of treatment largely depends on the correct diagnosis, which must be determined by experienced specialists.
Dorsopathy
Diagnosis of Dorsopathy? Translated from Latin as back disease (dorsopathy disease). It is not considered an independent disease, since it includes a number of pathological conditions. Their common feature is damage to the spine and all adjacent physiological structures (nerve endings, ligaments, muscles). For this purpose, a comprehensive diagnosis of dorsopathy is performed.
dorsopathy
Dorsopathy - clinics in
Choose among the best clinics based on reviews and the best price and make an appointment
Family
Oriental Medicine Clinic "Sagan Dali"
Moscow, prosp.
Mira, 79, building 1 Rizhskaya
+7
- Consultation from 1500
- Diagnostics from 0
- Reflexology from 1000
0 Write your review
Family
Center for Chinese Medicine "TAO"
Moscow, st.
Ostozhenka, 8 building 3, 1st floor Kropotkinskaya
+7
- Consultation from 1000
- Massage from 1500
- Reflexology from 1000
0 Write your review
Family
Clinic "Your Health Plus"
Moscow, Orekhovy pr., 11, entrance from the yard (from the children's playground)
Shipilovskaya
+7
- Consultation from 1850
- Reflexology from 2000
- Neurology from 500
0 Write your review
Show all Moscow clinics
Symptoms
The symptoms of dorsopathy, regardless of the specific disease that caused the deviation from the norm, are in principle quite similar. When the spine is affected, dorsopathy makes itself felt as follows:
- a person complains of periodically occurring, very acute pain (relapses occur up to 20 times a year, and sometimes more often);
- signs of the disease appear at any time, may or may not be related to exercise, if the disease is widespread, the limbs will be involved;
- In order for the pain to subside, it is often necessary to take a horizontal position;
- dorsopathy is accompanied by degeneration of the spine, limitation of its mobility in the affected area;
- in some cases, muscle weakness and dry skin may be observed at the level of the lesion.
Separately, many doctors distinguish vertebrobasilar insufficiency syndrome. With VBI, not only the vertebrae are dystrophically affected, but also the vessels supplying blood to the brain. As a result, vertebrobasilar syndrome leads to decreased brain activity.
Dorsopathy - specialists in Moscow
Choose among the best specialists based on reviews and the best price and make an appointment with
Therapist
Batomunkuev Alexander Sergeevich
Moscow, prosp.
Mira, 79, building 1 (Oriental Medicine Clinic “Sagan Dali”) +7 0 Write your review
Masseur
Zakrevskaya Natalya Alekseevna
Moscow, 1st Lyusinovsky lane, 3 B. (Medical)
+7
0 Write your review
RheumatologistTherapist
Forms
Doctors distinguish several forms of the disorder, not only by type, but also by form. The following forms of the disease are distinguished:
- deforming dorsopathy, in which primarily the intervertebral discs change, due to which the normal processes of depreciation of the spinal column do not occur and, as a result, its functions are disrupted;
- spondylopathy, in which changes directly affect bone structures;
- other types of disease in which the root cause of the disorders is not always amenable to accurate diagnosis.
Additionally, widespread and limited dorsopathy are distinguished. In the first case, the pathology is characterized as polysegmental, i.e., several segments are affected within one department. In the second case, only one segment is affected. It is important to clarify what form of dorsopathy the patient has by collecting all documents regarding disability.
Dorsopathy of pregnancy is also distinguished separately. When carrying a fetus, the load on the spinal column increases, which can lead to the development of various diseases. Usually, exercises selected by your doctor help prevent pathology during pregnancy.
Prevention
To prevent the development of spinal dorsopathy, a careful attitude towards oneself is recommended: people who are forced to sit or stand for a long time are recommended to take short breaks, and should not lift heavy objects.
It is useful to go swimming and give preference to moderate physical activity.
If you find an error, please highlight a piece of text and press Ctrl Enter. We will definitely fix it, and you will suffer karma
Traditional methods
It is important to understand that the use of alternative medicine recipes does not exclude the need to seek qualified help. Such methods can be used, but only after prior consultation with a doctor. This is due to the fact that some medicinal plants and remedies can reduce the effectiveness of medications or cause unwanted reactions in the patient.
Using traditional methods will not cure the disease. Their task is to relieve pain.
The most effective recipes:
- Take a cabbage leaf and make several shallow cuts on it. Lubricate it with honey. Apply a cabbage leaf to the affected area. Secure the compress on the body with a warm scarf.
- Pour 0.5 liters of sunflower oil into a container. Add 7 tablespoons of chopped sage herb to it. Place the container in a water bath for about half an hour. Let the product sit for 3 hours. The container must first be covered. After the specified time, strain the product and lubricate the affected areas with it.
- Chop a few cloves of garlic. The resulting pulp must be placed on a piece of natural fabric. Apply a compress to the body. After 5 minutes, remove the fabric and treat the skin underneath with vegetable oil. Then you need to wrap yourself in a warm blanket.
Regular use of these methods will help increase the effectiveness of medications and quickly relieve an acute attack of pain.
Dorsopathy in the acute period
Treatment during this period is planned literally day by day to achieve the desired result:
- From the moment of onset to the third day of the disease, bed rest is required. You need to lie on a hard, straight surface, and wear an orthopedic corset to reduce pain. The patient is prescribed injections of muscle relaxants, non-steroidal anti-inflammatory drugs, and also undergoes a blockade to relieve pain.
- From the fourth day the patient is allowed to get up little by little. Until the tenth day of illness, continued use of muscle relaxants and the inclusion of physiotherapeutic methods of treatment (a simple complex of exercise therapy) are indicated.
- From the eleventh to the twentieth day of the disease, physiotherapy procedures are carried out as prescribed, massage and the patient’s motor activity is slightly increased. During this period, it is recommended to seek the help of a chiropractor.
- From the twenty-first day of illness, moderate physical activity and therapeutic exercises are allowed. Until the thirty-first day of illness, painkillers are used as needed.
Development mechanism
The human spine is a complex structure that can withstand significant loads. Until about 30 years of age, the processes of tissue synthesis and restoration in the body prevail. Due to this, the spine copes with significant loads. After 30 years, the process of involution begins in the body. First of all, degenerative changes begin to occur in the cartilage of the intervertebral discs.
Under the influence of various unfavorable factors, the severity of the process intensifies, the spinal roots are pinched, and the surrounding tissues become inflamed. This condition is called dorsopathy. There are several types of it. It is customary to talk about deforming dorsopathy when intervertebral discs are initially involved in the pathological process. In most cases, the development of the disease is irreversible and can lead to disability.
Deforming dorsopathy codes in ICD-10 are assigned the following: M40 - M43.
Methods of diagnosis and treatment of dorsopathy
Dorsopathy can be identified in the first stages of development. To do this, it is enough to make an appointment with a neurologist, talk about the symptoms and undergo a series of instrumental examinations. One of the main diagnostic methods is radiography. In addition, if there is a suspicion of more serious pathologies, the patient is sent to:
- electroneuromyography;
- computed tomography;
- magnetic resonance imaging.
If the diagnosis is confirmed, and the person is actually diagnosed with the development of dorsopathy of the lumbar spine, the doctor’s task is to develop an effective course of treatment. It may include the following techniques:
- physiotherapy;
- physiotherapy;
- folk remedies;
- drug treatment.
Doctors always advise patients not to self-medicate, as this can lead to serious complications.
Diagnosis of dorsopathy
As a rule, the detection of lumbar dorsopathy does not cause problems - the pathological condition has clear and rather specific symptoms. Despite this, the diagnostic process must be comprehensive.
The patient is prescribed:
- X-ray of the lumbar area in two projections;
- spondylography;
- and MRI;
- electroneuromyography.
The use of the term “lumbar dorsopathy” is possible only as a preliminary diagnosis. For a doctor, such a phrase only means that the patient has certain problems with the integrity of the bone and connective tissue structures in the lumbar region. This condition a priori implies the appointment of more serious studies in order to identify the cause of the disease.
What is dorsopathy?
Spinal dorsopathy is a complex of all degenerative-dystrophic diseases affecting intervertebral discs, cartilage and paravertebral tissue.
Often the development of dorsopathy is caused by a characteristic “overload” of the spine, which occurs due to prolonged physical activity.
Dorospathy of the spine has its own varieties depending on the location (cervical, thoracic, lumbar and lumbosacral) and is manifested by a pain syndrome that is not related to inflammatory processes and diseases of the internal organs.
When the disease worsens, the person feels severe pain followed by limited mobility. It is these symptoms that should lead to a decision to seek help from a specialist.
Reasons for the development of dorsopathy
- Hereditary predisposition - often children suffer whose parents have already been diagnosed with the disease with a positive verdict.
- Static load on the spine - prolonged standing in a standing position due to one's professional activities - often leads to pinching of the nerve roots of the spinal cord - the development of osteochondrosis and other serious diseases.
- A sedentary lifestyle also leads to partial atrophy of the back muscles, resulting in a violation of the “support” and elasticity of the spine.
- A one-time load on the spine - a sudden lifting of a heavy object can lead to the development of osteochondrosis with subsequent formation of a hernia.
- Curvature of the spine, both congenital and acquired, leads to pinched nerve roots.
- Impaired metabolism provokes a violation of the integrity of cartilage tissue and the intervertebral disc.
- Excessive consumption of alcohol and tobacco smoking leads to “depletion” of cartilage and muscle tissue.
- The presence of chronic infections leads to inflammation and provokes the development of spinal diseases.
- An unbalanced diet also causes depletion of cartilage and muscle tissue in beneficial microelements.
All of these aspects gradually lead to a change in the height of the intervertebral discs, a change in the shape of the vertebra (a kind of grinding occurs due to loss of height), inflammation of the paravertebral tissues and pinching of nerve fibers.
Changes in the integrity of the vertebrae are accompanied by severe pain and partial loss of previous activity. Irreversible processes that have begun can lead to disability.
Consequences and complications
Each dorsopathy has its own complications. If the patient does not seek medical help, then with a formed intervertebral hernia, the development of vertebral artery syndrome, discogenic myelopathy, and radicular syndrome is possible. And any degenerative-dystrophic pathology can cause fusion of the bone structures of the spine, immobilizing the affected part.
If you are diagnosed with “dorsopathy” and do not take the necessary measures in time or interrupt treatment, this will lead to tragic consequences. Such as incessant pain, progressive paralysis, decreased sensitivity, cerebral circulatory disorders, and subsequently disability.
How to treat spinal dorsopathy
An integrated approach to the treatment of dorsopathies is practiced. Pharmacological drugs are used, physiotherapeutic and massage procedures are carried out. During exacerbations, patients are recommended to rest in bed or semi-bed rest, excluding stress on the spine.
Corseting
Orthopedic correction allows you to fix the vertebral elements in an anatomically correct position, prevent their displacement, and reduce the severity of pain. For patients with cervical dorsopathy, it is recommended to wear Shants collars, and for thoracic and lumbar patients, elastic orthoses with stiffening ribs are recommended.
To eliminate acute pain, injectable solutions of non-steroidal anti-inflammatory drugs (NSAIDs) are used - Meloxicam, Xefocam, Diclofenac. If they are ineffective, blockades with glucocorticosteroids (Diprospan, Triamcinolone) and anesthetics (Novocaine, Lidocaine) are performed. You can cope with moderate pain by taking NSAID tablets - Ketorol, Naiza, Nurofen. You can get rid of mild discomfort with the help of ointments and gels. These are Voltaren, Fastum, Dolgit.
Physiotherapy
In the treatment of dorsopathies, magnetic therapy, UHF therapy, laser therapy, shock wave therapy, and ultraviolet irradiation are used. In the acute, subacute period, electrophoresis or ultraphonophoresis with glucocorticosteroids, anesthetics, B vitamins, and chondroprotectors is performed.
Immediately after the acute pain is relieved, the physical therapy doctor creates an individual set of exercises. Their daily implementation helps improve blood circulation in the spine, strengthen the muscles of the neck and back, and accelerate tissue repair processes.
The doctor is present at the first classes and tells you how to dose the load correctly. In the future, you can train at home.
Massage
In the complex treatment of dorsopathy, acupuncture, vacuum, connective tissue, and segmental massage are used. But the most popular is the classic one, aimed at strengthening the muscular frame of the back, eliminating spasms, and increasing range of motion. During the procedure, the massage therapist acts only on the muscles, performing vibrations, rubbing, and kneading.
Osteopathy
Sometimes you can avoid spinal surgery by contacting a chiropractor - a doctor with a narrow specialization (orthopedist, traumatologist). After studying the radiographs, he examines the part of the spine affected by dorsopathy using superficial and deep palpation. The chiropractor then adjusts the displaced discs and performs muscle traction to increase the distance between the vertebrae.
Operation
If the pain cannot be eliminated with medication, the patient is prepared for surgery. Indications for it include complications that arise and rapid progression of the pathology. Surgery usually involves decompressing the spinal canal or removing a hernia. It is performed in various ways - laminectomy, open or endoscopic discectomy, microdiscectomy.
Products made according to traditional medicine recipes are not used to treat dorsopathies of any origin. Doctors allow their use only after basic therapy. At the stage of stable remission, folk remedies are used to get rid of mild discomfort that occurs after hypothermia or lifting heavy objects.
Specificity of pain sensations
Lumbosacral dorsopathy in most clinical cases manifests itself as a specific symptom, and only occasionally diagnosis can be difficult due to a number of nonspecific symptoms.
Manifestations of lumbar dorsopathy are characterized by such syndromes as:
- Reflex. In medical circles it is called lumbago, and among the people - “lumbago”. It is characterized by the occurrence of sudden and sharp pain in the lower back during physical activity or against the background of intense movements. The appearance of the syndrome indicates the initial degree of a pathology such as osteochondrosis. From the outside, the manifestation of the syndrome looks like a person is frozen in one position from pain, and subsequent movements only intensify it. Then muscle tension in the lumbosacral region is added to the pain.
- Compression syndrome. Because of the focus of formation, it is called radicular. The syndrome is distinguished by an uncharacteristic set of manifestations that develop against the background of compression of the nerve roots of the spinal cord. Painful sensations are localized in different places, which greatly complicates the diagnosis of the disease.
Causes
Degenerative changes in the structure of cartilage over time extend to the vertebrae, ligaments and intervertebral discs. The severity of the condition depends on the duration and nature of the negative impact.
There are many reasons for this pathology, however, the main ones are considered to be:
- Irregular loads;
- Physical inactivity (inactivity);
- The presence of scoliosis, kyphosis, lordosis;
- Injuries and neoplasms of the spine;
- Tuberculosis;
- Obesity.