Nephrosclerosis of the kidneys
Every urologist knows the causes of kidney nephrosclerosis, what it is, the outcome of the disease and the signs of this pathology. Nephrosclerosis (wrinkled kidney) is a disease that occurs in a chronic form and is characterized by the growth of coarse scar tissue. Mostly adults are affected. If this condition is not treated correctly, it can be fatal.
Causes and pathogenesis
There are two phases of the disease:
- Pathological changes in the functioning of the kidney and the onset of the sclerotic process caused by specific reasons;
- The development of nephrosclerosis and the manifestation of pathological changes associated with the replacement of healthy parenchyma with connective scar tissue.
A wrinkled kidney is the final stage of the process, when almost all healthy parenchyma is replaced by connective tissue adhesions. At the same time, the surface of the kidney is uneven, and the organ itself is compacted, and its size is smaller than normal. Histological signs of nephrosclerosis differ, depending on the causes of the disease:
- If nephrosclerosis has developed due to arterial hypertension or glomerulonephritis, the surface of the kidney will be fine-grained.
- With pyelonephritis, the kidney will be affected asymmetrically.
- If the disease is caused by atherosclerotic vascular lesions, the surface will be large-nodular with cicatricial extensions of irregular shape.
Depending on the speed of the flow, two forms of the disease are distinguished:
- benign – certain groups of nephrons are affected;
- malignant - hemorrhages, dystrophic changes in the renal tubules and necrosis of the entire parenchyma develop.
In the pathogenesis of renal vascular sclerosis, two stages are distinguished. The first is due to the fact that pathogenic factors have a negative effect on the kidneys, leading to the death of nephrons. At the second stage, the sclerotic process develops independently, covering increasingly large areas. The organ can be affected evenly or unevenly, its surface becomes fine- or coarse-grained, and becomes covered with scars.
According to the mechanism of development, renal sclerosis can exist in two forms:
- Primary. Associated with a failure of the blood supply to the renal nephrons as a result of various systemic vascular diseases (for example, hypertension).
- Secondary. Develops against the background of an existing kidney disease (for example, glomerulonephritis complicated by sclerosis).
Primary renal sclerosis has the following classification:
- Hypertensive nephrosclerosis. A prolonged increase in pressure leads to spasm and stenosis of the renal vessels; they become less elastic and cannot resist blood flow.
- Sclerosis due to thromboembolism in the renal vessels during renal infarction. Blockage of the artery lumen by a thrombus or embolus leads to a decrease in blood flow to the kidney tissue, as a result of which part of the organ dies from lack of oxygen. Repeated kidney infarctions or extensive infarctions are especially dangerous.
- Atherosclerotic nephrosclerosis. As in other arteries of the body, fatty plaques can be deposited in the renal vessels, so the blood supply to the organs is disrupted. Over time, poorly nourished areas of the renal parenchyma undergo nephrosclerosis. Most often, nephrosclerosis of this type covers the areas where the renal artery enters the kidney, as well as the places where it divides into small branches.
- Involutive nephrosclerosis. After 50 years, the walls of blood vessels begin to thicken, their lumens narrow. This is due to the deposition of calcium inside the vessels and the replacement of some muscle fibers with connective tissue. By the age of 70, the number of healthy nephrons is 40% lower than at a young age, so nephrosclerosis is diagnosed more often in older people.
- Renal sclerosis against the background of chronic venous congestion. Prolapse of the kidneys, narrowing of the renal veins or varicose veins gradually provoke a violation of the outflow of blood from the kidney. As a result, collagen fibers grow in it, the elasticity of the vessel walls decreases, and sclerosis develops.
Causes of nephrosclerosis
Nephrosclerosis is not an independent disease. It develops most often against the background of hypertension, atherosclerosis and other diseases of the blood vessels or the kidneys themselves, which causes disruption of the normal blood supply to the organ. According to the mechanism of development, the following types of nephrosclerosis are distinguished: primary, or hypertensive, and secondary.
The main cause of nephrosclerosis is a violation of the blood supply to the organ, which ultimately leads to its dysfunction.
Reasons for development
Renal nephrosclerosis is divided into two types:
- Primary. This nephrosclerosis is caused by a disruption in the blood supply to the kidney tissue due to vascular diseases.
- Secondary. This form of the disease is the outcome of various diseases of the urinary system, in particular, an infectious process in the kidneys (glomerulo- and pyelonephritis).
There are two forms of this pathology: primary and secondary wrinkled kidney.
Among the causes of primary nephrosclerosis, several are mentioned at once:
- Age-related changes. Many elderly people suffer from venous congestion and atherosclerosis. This is precisely what becomes one of the reasons for the development of the disease.
- High cholesterol content. The appearance of plaques on the walls of blood vessels reduces the amount of blood and impairs renal function.
- Hypertension. This cause causes spasms and sclerotic changes in tissues.
The appearance of secondary renal sclerosis is provoked by other reasons:
- diabetes;
- nephrotic diseases (glomerulonephritis and pyelonephritis);
- injuries of various types;
- syphilis;
- kidney tuberculosis;
- MBC;
- amyloidosis.
- Causes
- Mechanism of disease development
- Symptoms
- Treatment
Renal nephrosclerosis is a pathological process characterized by the death of nephrons and the replacement of functional renal tissue (parenchyma) with connective tissue. It can be a consequence of various diseases of the kidneys or renal arteries and veins, as a result of which the normal blood supply to the organ is disrupted.
As the disease progresses due to significant proliferation of connective tissue in the affected kidney, dysfunction and characteristic structural and morphological changes are noted.
The buds decrease in size, become dense and wrinkled.
Nephrosclerosis predominantly develops as a complication of diabetes mellitus, hypertension, atherosclerosis, glomerulonephritis or pyelonephritis and gradually leads to chronic renal failure (CRF).
Types and causes of the disease
Primary nephrosclerosis
Primary sclerosis of the kidney often occurs with a heart attack, atherosclerosis of the renal arteries, arterial hypertension and chronic congestion of the organ. Elderly people over 70 often face this problem. This is due to the natural processes of aging and the death of nephrons. Older people experience thickening of the arteries, calcium deposits, and proliferation of connective tissue. The renal cortex becomes thinner, and the inner layer of the tubules atrophies. Symptoms of primary nephrosclerosis may appear in a child.
Etiology
As mentioned earlier, the causes of nephrosclerosis are varied. Thus, the primary factors for the onset of the disease include:
- disturbance of blood supply;
- high blood pressure;
- the formation of blood clots that block the flow of blood to the entire kidney or to certain areas of it, which can cause an organ infarction;
- atherosclerosis - in which the lumen of the arteries narrows through the formation and deposition of fats on them;
- patient's age;
- decreased elasticity of renal vessels.
https://youtu.be/UiWFSrOCB7Y
Why does kidney shrinkage occur?
With a prolonged increase in blood pressure (BP), vascular spasms develop. They narrow and lose elasticity. As a result, the pressure increases even more, and resistance to blood flow increases. Organs are deprived of normal blood supply and experience oxygen starvation.
As a result, areas of ischemia appear in paired organs, which leads to the replacement of parenchymal connective tissue. Secondary kidney shrinkage can also occur due to the following diseases:
- amyloidosis;
- diabetes mellitus;
- tuberculosis of renal tissue;
- history of systemic lupus erythematosus;
- nephrolithiasis;
- glomerulonephritis;
- nephropathy in pregnant women;
- injuries;
- pyelonephritis.
Clinical picture
https://youtu.be/hcgpvW9kwhk
Nephrosclerosis, also known as “shrunken kidney,” is quite difficult to identify in the initial stages, since there are no characteristic symptoms. The patient does not experience any discomfort. Only when you consult a doctor with other complaints and after a diagnostic examination does it become possible to identify abnormal processes.
When the disease becomes stable, the following signs appear:
- swelling of the face and limbs;
- the number of urges to urinate increases, but the volume of urine produced decreases;
- pain in the lumbar area;
- strong thirst;
- high blood pressure;
- fatigue, weakness;
- itching of the skin.
The listed symptoms of kidney nephrosclerosis should be a reason to undergo a more in-depth medical examination. Only after receiving its results can you begin therapy.
The further the process of kidney cell death has progressed, the more pronounced the signs of the disease will appear. At the earliest stage, a person can only feel the symptoms of the underlying pathology, but not always (for example, vascular atherosclerosis gives practically no symptoms).
As cell death progresses, the following symptoms appear:
- Polyuria (more than 2 liters of urine per day), which is later replaced by oliguria (with the death of more than 70% of nephrons) and anuria (with the death of more than 90% of nephrons).
- Increased urge to urinate, especially at night.
- The appearance of blood in the urine.
- Anemia (decrease in the level of hemoglobin and red blood cells in the blood).
When kidney tissue is replaced to a high degree by connective fibers, organ function is severely affected. Waste and toxins accumulate in the blood, swelling appears on the face and body, including in the abdominal cavity.
A person’s body weight increases, and the entire appearance becomes puffy. Blood pressure changes towards a persistent increase. Further, visual acuity decreases, and sensations of fog appear before the eyes due to the development of retinopathy.
Symptoms of nephrosclerosis
Every tenth inhabitant of the Earth has kidney damage, namely nephrosclerosis at one stage or another of the disease. But many of them are not even aware of their illness. The insidiousness of nephrosclerosis is that at its initial stage there are practically no symptoms. The disease is discovered by chance during urine and blood tests. If at this moment you do not pay due attention to the developing disease, then over time it progresses up to terminal renal failure. At this stage, serious complaints appear and symptoms are pronounced. But the moment when the disease could be defeated or the patient’s condition could be stabilized at this stage has already been missed.
This is what the face of a patient with nephrosclerosis looks like in the stage of developed renal failure
Clinical symptoms of nephrosclerosis appear when renal function is impaired:
- specific swelling on the face and legs;
- pain and discomfort in the lumbar region;
- high blood pressure, accompanied by severe headaches that are difficult to relieve with analgesics;
- change in the appearance of urine (reddish, brown, foamy, with flakes, cloudy sediment);
- frequent urge to urinate, especially at night;
- decrease in the volume of urine excreted per day (less than 500 ml);
- constant feeling of thirst;
- intolerance to meat food (a feeling of disgust appears);
- general weakness, loss of appetite;
- shortness of breath, rapid heartbeat;
- skin itching;
- weight loss.
If these symptoms or some of them occur in a child or an adult, then you should immediately undergo a nephrological examination.
Stages of nephrosclerosis
There are 2 periods in the development of this pathology:
- In the first phase, there are no manifestations of nephrosclerosis, however, the patient has and may progress one or more diseases leading to the replacement of normal renal parenchyma with connective tissue. During this period, changes characteristic of kidney damage already appear in urine and blood tests.
- Symptoms characteristic of nephrosclerosis, and, accordingly, renal failure, appear in the second stage of the process, when changes in the structure of the kidneys can be detected using ultrasound and other instrumental research methods.
Also, depending on the course of the pathological process, malignant and benign forms of nephrosclerosis are distinguished.
https://youtu.be/2CznUi0EQkc
Fortunately, in the vast majority of patients, the second form of the disease occurs, in which the process progresses slowly; with successful treatment of the underlying disease, the progression of nephrosclerosis can be slowed down.
In a malignant course, nephrosclerosis progresses quickly and within a few years can lead to complete loss of kidney function, severe renal failure and doom the patient to lifelong hemodialysis. Such an unfavorable outcome can be observed with malignant arterial hypertension and eclampsia in pregnant women.
Diagnostic measures
Diagnosis of pathology begins with a visual examination of the patient and collection of data about the patient’s complaints, his habits and lifestyle, past and concomitant diseases.
At the next stage, a set of diagnostic studies is carried out:
- general clinical analysis of urine and blood;
- biochemical study of blood plasma;
- CT scan;
- urography;
- ultrasonography;
- scintigraphy;
- vascular angiography;
- radionuclide renography;
- Doppler examination of blood vessels;
- biopsy.
Symptoms
The disease can last for decades, with the deterioration of kidney function occurring gradually, and the symptoms initially do not bother patients much. A doctor is often consulted when edema appears, urination problems and signs of arterial hypertension appear. With such symptoms, changes in the kidneys are often irreversible, and the function of the organ is already significantly reduced.
Urinary dysfunction
Most people over forty suffer from a benign form of nephrosclerosis, which means that the blood vessels in the kidneys gradually change, but these changes do not occur as quickly and do not require treatment.
For patients with benign nephrosclerosis, all that is required is to monitor their condition and take measures to prevent the progression of the disease.
Other patients have a malignant form of nephrosclerosis, in which case damage to the kidney vessels occurs so quickly that drug treatment or even surgery is necessary.
Definition
Nephrosclerosis is the process of replacement of the renal parenchyma with connective tissue, which leads to thickening of the walls of arteries and arterioles in the kidneys.
Such arteries cannot normally supply blood to the kidney, the nutrition of the glomeruli and tubules is disrupted, and subsequently their death and replacement with connective tissue.
The kidney decreases in volume (primarily shriveled kidney) and begins to lose its functions.
Pain in the lower back indicates possible kidney problems
Renal nephrosclerosis or hypertensive nephropathy is the replacement of organ parenchyma with connective tissue, which leads to a decrease in the size of organs and disruption of their functions, and therefore their functionality may cease.
The following types of disease are distinguished:
- 1Primarily wrinkled bud. Appears as a result of impaired blood supply to the organ as a consequence of arterial hypertension. Changes of this kind can cause a serious functional disorder - renal failure.
- 2Secondary wrinkled bud. It develops against the background of damage to the organ parenchyma due to various diseases that have a negative impact on the human urinary system.
https://youtu.be/ppwFKY8uUBw
The causes of the pathology of the disease lie in many factors.
- Expert opinion: Today it is one of the most effective remedies in the treatment of kidney diseases. I have been using German drops in my practice for a long time...
For example, hypertension. Increased blood pressure over a long period disrupts the structure of the kidney vessels, after which they become less elastic.
Hypertensive nephrosclerosis has the following 2 types:
- 1Benign nephrosclerosis is a decrease in the elasticity of the arteries of the kidneys due to an increase in the amount of connective tissue in their walls. This type of nephrosclerosis develops over a long period.
- 2Malignant nephrosclerosis is a consequence of severe arterial hypertension. With this form of nephrosclerosis, it is very important to carry out hemodialysis on time. Otherwise, irreversible changes begin to occur in the organ, leading to kidney failure. This could result in death.
- An effective way to cleanse your kidneys at home
Another reason for a primarily shriveled kidney is its infarction. The lumen in the renal artery is blocked by a blood clot, as a result of which the living tissues of the organ atrophy.
Atherosclerosis is also a common cause of pathology. The presence of atherosclerotic plaques on the walls of the arteries leads to a decrease in the lumen in them and to the death of organ cells.
Age-related changes also lead to this disease. By the age of 45-50, calcium is deposited on the inner walls of the arteries, and the number of muscle fibers increases. In this regard, the walls of the arteries become thicker, and the openings in them narrow.
The reason may lie in chronic venous congestion of the kidneys. The outflow of venous blood from these organs is disrupted, protein grows in the walls of blood vessels, and therefore their elasticity decreases.
These processes occur over a long period and are associated with the presence of venous diseases and nephroptosis in the patient.
The causes of the pathology are as follows:
- 1Pyelonephritis is an inflammatory disease of the kidneys of bacterial origin, characterized by damage to the renal pelvis (pyelitis), calyces and parenchyma of these organs. In children, pyelonephritis often goes unnoticed, since there are few symptoms for diagnosis. In this case, the disease develops, developing into nephrosclerosis and renal failure. To prevent an unfavorable outcome of this disease in children, it is necessary to diagnose it in the early stages of the disease and begin treatment on time.
- 2Kidney tuberculosis is an infectious disease caused by the microbacterium tuberculosis bacillus. The disease negatively affects almost all body systems.
- 3Nephrolithiasis or kidney stones is the most common kidney disease, which is characterized by the presence of stones in these organs.
- 4Diabetes mellitus is a chronic disease that develops as a result of insufficient production of insulin by the patient’s body. Without the necessary treatment, the disease progresses rapidly, leading to atrophy of both kidneys. The result of this is death.
- 5Nephropathy in pregnant women. During pregnancy, significant changes occur in the hormonal system of a woman—the expectant mother: the brain begins to work somewhat differently, as a result of which the capillaries spasm, blood circulation in the kidneys decreases, and salts accumulate in the body. Against the background of such an imbalance, swelling appears and blood pressure increases.
- 6Chronic glomerulonephritis. Impaired blood flow in the kidneys due to untreated throat diseases (sore throat, pharyngitis).
Changes in the kidneys with nephrosclerosis
The kidneys are two small organs located in the abdominal cavity at the lumbar level. They are bean-shaped, equipped with a network of vessels and pathways for excreting the resulting urine. The kidney consists of many identical structures - nephrons. This is where the blood is purified through a special filter. It is located inside the glomerulus - small intertwined vessels. The filter is so thin that it retains blood cells - red blood cells, white blood cells and platelets, as well as large proteins.
The nephron is the basic unit of the kidney
The resulting filtrate is not immediately sent to the pelvis and ureter - the main urinary tract, since it still contains a mixture of waste and useful chemicals. Separating them is a task for the tubules, which are also part of the nephron and originate from the vascular glomeruli. In appearance they resemble thin curved tubes. Inside these tubes, the final separation of the filtrate into its component parts occurs. All useful substances return to the bloodstream, waste products enter the final composition of urine and are sent further to the pelvis and ureter.
The kidney is closely related to the urinary organs
The nephrons are held together by a strong foundation of the organ - the stroma, consisting of connective tissue. It is located in the form of a layer between the nephrons. Nephrosclerosis is not an independent disease. It represents the proliferation of the connective tissue layer against the background of various diseases. These changes lead to the progressive death of nephrons and chronic poisoning of the body with toxins - renal failure. The number of such cases in the world is steadily growing every year. In European countries, kidney failure occurs in six hundred cases per one million inhabitants.
Synonym for the disease: wrinkled kidney.
Sclerosis is not a process that occurs exclusively in the kidneys. In fact, it is a logical outcome of many diseases of the liver, lungs, and brain. A typical representative of sclerosis is cirrhosis of the liver. Pulmonary tuberculosis in the final stage is also called cirrhosis.
Diagnostics
The diagnosis of “wrinkled kidney” is made on the basis of a number of studies:
- Ultrasound examination of the kidneys. The size of the organ, the degree of atrophy of the cortex and the thickness of the renal parenchyma are determined.
- Urography. Determine the decrease in organ volume and the degree of degradation of the cortical layer. In some patients, calcified areas of tissue can be found.
- Angiography. Vascular examination allows us to identify pathologies of small blood vessels.
- Radionucleotide radiographic examination. The drug, which contains nucleotides, is distributed in the kidney tissue and is gradually eliminated from the body. When studying this process, areas of the kidney are identified that are not involved in drug excretion - these are sclerotized areas. In severe forms of the disease, the entire kidney may become sclerotized.
To identify the disease, laboratory tests are performed, the patient is examined using ultrasound and x-ray examination. Urography and angiography are performed, with the help of which a decrease in the size of the organ and a decrease in the rate of urine excretion from the kidneys are detected.
Since the symptoms of a shriveled kidney appear in the later stages, it is very important to identify this pathology with the help of an examination as early as possible, since the effectiveness of treatment in this case will be much higher. Taking the patient's medical history plays an important role.
- General urine analysis. Any examination of the kidneys, of course, begins with a urine test; with initial nephrosclerosis, the following abnormalities can be detected: a decrease in the relative density of urine, the appearance of protein, single red blood cells and casts.
- Blood tests. In a clinical blood test, a decrease in the level of hemoglobin and platelets is possible. In biochemical – a decrease in the amount of total protein, an increase in the level of urea, creatinine, uric acid and sodium. An increase in glucose and cholesterol levels should alert you.
Such changes in urine and blood tests are very nonspecific and can be observed not only in kidney diseases. However, the combination of such deviations in the results of laboratory tests, in the presence of a history of factors that can lead to kidney damage, forces the doctor to think about further diagnosis.
For examination, many instrumental methods are used, such as ultrasound, excretory urography (x-ray of the kidneys with a contrast agent), angiography, computed tomography, radioisotope studies, etc. All of them reveal a decrease in the kidney in size, the presence of calcium deposits, impaired blood flow in the renal vessels, and others changes indicating the proliferation of connective tissue.
A biopsy can give an accurate answer about the condition of the renal parenchyma.
Renal sclerosis is an extremely serious disease that requires urgent treatment.
https://youtu.be/Umocifp9T1M
To achieve effectiveness, the doctor must make a correct diagnosis - a thorough diagnosis will help with this. All methods and types of patient examination are divided into laboratory and instrumental.
Laboratory methods include:
- general blood test - low levels of hemoglobin and platelets are considered a manifestation of pathology;
- biochemical blood test - here the signals of the development of kidney disease will be high levels of uric acid, creatinine and urea, and the amount of protein, on the contrary, will decrease;
- general urinalysis - renal sclerosis is accompanied by an increase in the amount of protein and the presence of red blood cells in the urine (in the normal state there are none).
If clinical tests only indicate the presence of pathology in the body, then instrumental tests make it possible to accurately determine the location and extent of organ damage. For this purpose the following are assigned:
- ultrasound examination (ultrasound);
- angiography of renal vessels;
- excretory renal urography;
- vascular doppler;
- computed tomography (CT);
- radionuclide renography;
- scintigraia;
- kidney biopsy.
First you need to correctly collect anamnesis and analyze the clinical picture. Laboratory methods are also used for diagnosis, including:
- biochemical blood test, which reveals increased levels of urea, creatinine and uric acid, a decrease in total protein, and in the final stages an increase in potassium, magnesium, phosphorus and sodium;
- a general urinalysis, which reveals an increased amount of protein, a decrease in the relative density of urine, as well as the presence of red blood cells and casts that are absent normally;
- a general blood test, which shows a decrease in hemoglobin and platelet levels.
Among the instrumental research methods that are effective are:
- ultrasound examination, which reveals a decrease in the size and function (atrophy) of the renal cortex, as well as the presence of calcifications in the renal parenchyma;
- excretory urography of the kidneys, which allows you to identify a decrease in the volume of the kidney and its cortex;
- angiography of the renal vessels, which determines the narrowing and deformation of small renal arteries, uneven contour of the kidney, thinning of the renal cortex;
- kidney scintigraphy, which reveals uneven distribution of the radioisotope in nephrosclerosis;
- renal vascular Doppler, which detects slowing of blood flow in the renal vessels and nephrons;
- radionuclide renography, which detects delayed accumulation and excretion of a radiopharmaceutical drug by the kidneys;
- computed tomography of the kidneys;
- kidney biopsy.
Using the Zimnitsky test, you can evaluate the concentrating ability of the kidneys; any deviations may indicate a disruption in their functioning, and, consequently, the development of sclerosis.
To confirm the correct diagnosis, it is necessary to evaluate the results of x-ray, ultrasound and radionuclide studies.
Ultrasound examination reveals changes in the size of the kidney, the thickness of the parenchyma, atrophy of the cortex and its relationship with the medulla.
Urography shows an increase in kidney volume, thickening of the cortical layer of the parenchyma and calcium deposition. On an angiogram, specialists can detect narrowing of small arteries, uneven contours of the affected kidney, and a decrease in the cortex.
During a radionuclide study, slow accumulation and elimination of the radiopharmaceutical are observed.
Scintigraphy reveals an uneven distribution of radionuclide in the tissue of the affected kidney.
The nonspecificity of the signs of the disease significantly complicates diagnosis. Typically, such issues are dealt with in specialized nephrology centers. Organ transplant operations of varying degrees of complexity are also performed here.
If you suspect an illness, you should seek help from such a center or a local physician. The latter, after studying the clinical picture, can give a referral to a specialist.
Diagnosis of the disease begins with a study of the patient’s complaints, his medical history and physical examination. During the consultation, the nephrologist may also palpate the abdominal cavity. The listed manipulations allow us to suggest a preliminary diagnosis and outline further examination tactics.
At the next stage, the patient is prescribed laboratory tests. For example, blood biochemistry may indicate the following symptoms of kidney dysfunction:
- increased levels of urea and creatinine;
- reduction in quantitative protein content;
- a decrease in potassium levels, and an increase in phosphorus and magnesium.
https://youtu.be/4dGvDJKyWrE
A urine test reveals protein and red blood cells, but its density is significantly reduced. When examining a blood test, it turns out that the level of platelets and hemoglobin falls, and the quantitative content of leukocytes increases.
To more accurately assess the functioning of organs, they resort to instrumental methods of examining patients diagnosed with nephrosclerosis. Ultrasound of the kidneys, for example, allows you to assess their size and the condition of the cortex. Urography is mandatory. Angiography gives a complete picture of the condition of the vessels in the affected organ.
Based on the examination results, the doctor confirms or refutes the preliminary diagnosis and makes recommendations for further treatment.
Diagnostic measures begin with collecting anamnesis, identifying the main complaints and conducting an external examination of the patient. Collecting complete information will allow us to assume the presence of nephrosclerosis and find out its causes.
Laboratory diagnostics play a major role in the early detection of problems:
- Blood chemistry. Reflects an increase in creatinine, urea, uric acid, and a decrease in protein levels. In the early stages of the disease, the amount of potassium decreases, but later it increases greatly, as does the amount of magnesium, phosphorus, and sodium.
- General blood analysis. Protein appears in the urine, red blood cells and casts appear in small quantities, and the density of urine decreases.
- General urine analysis. In the later stages of renal sclerosis, hemoglobin and platelets decrease, and leukocytosis is observed.
Ultrasound of the kidneys provides fairly accurate data on the condition of the renal tissue. The patient's ultrasound shows signs of atrophy of the cortical layer; sometimes it can merge with the medulla (does not have a clear boundary).
Calcifications appear in the kidney parenchyma, reflecting the death of its individual sections. To assess information about the vessels of the kidneys, angiography is performed with the introduction of a contrast agent - the method will show all areas of vascular narrowing, obstructions to blood flow, etc. To clarify the diagnosis, CT and MRI of the kidneys, scintigraphy, excretory urography are recommended, and occasionally a kidney biopsy is performed.
Symptoms and manifestations of a wrinkled kidney
Symptoms of a shriveled kidney are caused by the death of most of the nephrons. The organ ceases to control the fluid balance in the body, salt exchange, maintain hematopoiesis and the proper level of blood pressure. The nature of urination and the volume of urine released per day changes.
Kidney failure affects all organs
Symptoms of nephrosclerosis - table
| Manifestation of a wrinkled kidney | Mechanism of symptoms |
| Decrease in the amount of urine excreted per day | Death of renal nephrons |
| Predominant urine output at night | Failure of active nephrons to concentrate urine |
| High blood pressure | Lack of blood in a shriveled kidney due to nephrosclerosis |
| Swelling of the eyelids and face | Inability of a shriveled kidney to control fluid content in the body |
| Pale skin, weakness | Lack of hemoglobin in the blood |
| Blood in the urine | Changes in blood flow inside the kidney |
Treatment options
For neurosclerosis, treatment should be comprehensive. First of all, therapy is aimed at eliminating the causes that caused sclerotic changes in the renal tissue. If the cause of the disease is hypertension, medications that lower blood pressure are taken. However, these drugs should be taken with caution, since a decrease in blood pressure can lead to a decrease in blood flow to the kidney and a worsening of the patient's condition.
https://youtu.be/k8seM8oovig
In addition, a wrinkled kidney requires following a diet and taking diuretics. The patient's diet should not contain salt. In some cases, you should also limit the amount of fluid you drink.
Drinking should be limited only to patients at a late stage of the pathological process. In this case, the amount of liquid consumed per day (including soups, juices and fruits) should be half a liter higher than the volume of urine excreted over the previous day. For patients in the early stages of nephrosclerosis, there is no need to limit drinking. On the contrary, they are recommended to drink up to two liters of clean water per day.
If normal kidney function is disrupted, it is important to limit the consumption of protein foods, primarily meat. Such a restriction will reduce the degree of toxicity from nitrogenous bases. However, the restriction in protein intake must be compensated by other foods. The diet of a sick person should be varied and sufficiently high in calories.
Treatment of renal sclerosis depends on the causes of the disease and the symptoms of the pathology. Diuretics, vitamins, anabolic drugs, enterosorbents, and antihypertensive drugs can be used. A diet is also used as treatment, which can be aimed at reducing the amount of protein consumed, table salt and fluid intake.
If complications develop, surgery and donor organ transplantation may be required.
tvoipochki.ru
There is no specific therapy aimed at treating nephrosclerosis. It is necessary to treat the disease, which has led to kidney damage and death of nephrons, followed by their replacement with connective tissue. That is why not only a nephrologist, but also a specialized specialist treats patients with nephrosclerosis.
In addition to therapy aimed at treating the underlying disease, patients must follow a diet. It is recommended to limit the amount of protein and table salt; the diet should contain enough vitamins and mineral salts. In the absence of arterial hypertension and edema, fluid and protein restriction is not required.
In end-stage renal failure, when both kidneys have lost their functions, patients are advised to undergo hemodialysis. The only way out in this situation is kidney transplantation; in recent years, this operation has been successfully carried out in Russia, and for citizens of our country it is free.
Based on the data obtained during the diagnosis, the doctor prescribes medications and selects the most effective dosage. The difficulty is that therapeutic treatment of renal sclerosis is at an early stage. Only at this stage can the process be corrected with medications.
Depending on the course of the disease and the patient’s condition, anticoagulants, antiplatelet agents (help restore blood supply to the kidneys), drugs that lower blood pressure and potassium preparations (to restore salt balance) are prescribed.
In later stages of the disease, hemodialysis is performed. This is a special procedure for purifying blood outside the kidney. Hemodialysis is carried out using a special artificial kidney apparatus, which eliminates metabolic end products and toxins from the body.
First you need to determine the cause and begin treatment of the causative disease. Therapy in the early stages involves drugs such as anticoagulants (heparin, warfarin), antiplatelet agents (pentoxifylline, trental, dipyridamole), which help improve renal blood supply.
Drugs are also used to lower blood pressure, but in the later stages of nephrosclerosis they should be used with caution. These include ACE inhibitors (captopril, enalapril), calcium antagonists (verapamil, nifedepine), β-adrenergic receptor blockers (atenolol, propranolol), diuretics (furosemide, hypothiazide).
Potassium preparations (asparkam, panangin) are also prescribed in order to eliminate salt imbalances. No less important are multivitamin preparations, iron supplements, and sorbents.
With the development of stage III-IV chronic renal failure, when it is impossible to restore kidney function with drug treatment, hemodialysis or kidney transplantation are used. During hemodialysis, the blood of a patient with nephrosclerosis is passed through a special membrane in an artificial kidney apparatus, which cleanses the body of toxins and metabolic end products and normalizes the water-salt balance.
The frequency of hemodialysis procedures depends on the patient’s condition and the degree of functional activity of the kidneys. During hemodialysis, the patient is prescribed antihypertensive drugs, vitamins, potassium supplements and other medications.
Carrying out hemodialysis procedures for nephrosclerosis
To prevent the disease from continuing to progress, it is necessary to regulate the amount of table salt consumed in the patient’s diet. Another important factor in the treatment and prevention of nephrosclerosis is the use of hypertensive drugs. Intensive hypertensive therapy can cause a decrease in renal blood flow and an increase in azotemia.
During the period of development of azotemia, specialists prescribe a diet with restrictions in the consumption of protein, vitamin D2, diuretics, enterosorbents and anabolic agents.
In case of a malignant course of hypertension, which contributes to the development of nephrosclerosis, they resort to embolization of the renal arteries. In such cases, patients are advised to undergo hemodialysis or transplantation of the affected organ.
Preventive measures are aimed at timely detection and treatment of pathologies contributing to the development of renal sclerosis.
Treatment methods
For renal sclerosis, treatment should be comprehensive. It includes:
- Following a salt-free diet. Patients should reduce their protein intake and eat small meals 5-6 times a day.
- Use of medications (anticoagulants, antiplatelet agents, antihypertensive drugs, potassium and iron supplements, bisphosphonates, sorbents, Canephron or Cyston). In case of nephrosclerosis against the background of hypertension, ACE inhibitors (Perindopril, Capoten, Enap), calcium channel blockers (Amlodipine, Verapamil) and beta-blockers (Egilok, Betalok, Concor) can be prescribed.
- Taking microelements.
- Blood purification using hemodialysis.
Treatment of kidney nephrosclerosis
In severe cases, a kidney transplant is required.
Surgery
At stages 3-4 of the pathological process, drug treatment is usually ineffective. In such cases, the patient is indicated for hemodialysis or a donor kidney transplant.
The essence of the first procedure is to cleanse the blood of toxic substances. For this purpose, a special artificial kidney filter is used.
https://youtu.be/ycU7KB1MqWs
The frequency of hemodialysis is determined by the patient’s condition and the severity of the pathological process. The procedure must be accompanied by drug therapy.
Surgical treatment involves transplantation of a donor kidney. This is one of the few types of operations where an organ can be removed from both a living person and a corpse. During the recovery period, the patient is prescribed serious medication support and complete rest.
Types of disease
Depending on the cause, there are two types of kidney nephrosclerosis:
- primary, which occurs as a result of impaired blood supply to the kidneys in diseases and conditions such as atherosclerosis, hypertension, renal infarction, venous congestion in the kidneys, etc. Primary nephrosclerosis also often occurs due to senile changes in the body;
- secondary, which develops against the background of existing kidney diseases (glomerulo- and pyelonephritis, kidney stones, tuberculosis, syphilis, renal amyloidosis, diabetes mellitus), as well as as a result of their injury, or exposure to ionizing radiation on the body.
Primary nephrosclerosis, in turn, is further divided into the following forms:
- atherosclerotic;
- involutive;
- hypertensive.
Also, depending on the course of the process, there are:
- benign nephrosclerosis, in which there is a gradual and long-term deterioration in the functions of the renal arteries. First, the inner layer of the walls of smaller vessels thickens and gradually this thickening spreads to the entire wall, sometimes blocking the central channel of the vessel. Fat is then deposited in the degenerated wall tissue. Large arteries have excess elastic tissue, which can block their channels. Both of these conditions cause disruption of blood flow to vital areas in the kidneys, which in turn leads to poor functioning of the kidney tissue;
- malignant nephrosclerosis, in which the above changes develop much faster.
Use of medications
This disease is treated in specialized nephrology centers. It comes down to eliminating the main provoking factor. Attempts to restore lost kidney function without the first step are usually unsuccessful.
Treatment is always comprehensive and long-term. Depending on the clinical picture and general condition of the patient, the following medications may be required:
- Anticoagulants (Heparin) to prevent blood clots.
- Medicines to lower blood pressure.
- ACE inhibitors (Diroton, Berlipril) to dilate the blood vessels of the kidneys.
- Diuretics, which remove excess fluid from the body.
- Calcium antagonists that promote dilation of arteries (Falipamil).
- Multivitamin complexes.
For other disorders caused by kidney dysfunction, medications are selected individually.
Stages of the disease
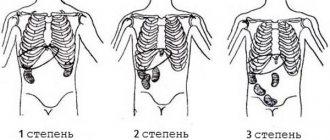
Kidney nephrosclerosis, regardless of its form, develops over several years. It is characterized by gradual formation. The main stages of nephrosclerosis:
- First. Vivid symptoms of nephrosclerosis of the hypertensive type have not yet appeared. The disease can be detected by determining the filtration rate of creatinine or insulin or by low albumin levels.
- Second. This is the pre-nephrotic stage. At this stage, microhematuria develops - a small amount of red blood cells in the urine.
- Third. Accompanied by high blood pressure and swelling.
- Fourth. It begins a couple of years after the onset of proteinuria. Chronic renal failure develops.
Prevention
There is no specific prevention of renal nephrosclerosis. The main methods to prevent the progression of the disease are to follow a diet, avoid physical and mental stress, get enough rest, constantly monitor blood pressure, and lead an active lifestyle.
Kidneys are vital organs; without them, our body would not be able to function. Therefore, you need to remember that when you take care of them, the frequency of exacerbations of the underlying disease that caused nephrosclerosis is reduced.
Secondary nephrosclerosis
If hypertensive nephroangiosclerosis occurs primarily, then the secondary form is a complication of infectious and non-infectious pathology. It is necessary to consider what diabetic sclerosis is. Kidney damage is a late complication of diabetes types 1 and 2 (occurs on average 15-20 years after the onset of the disease). The glomeruli are predominantly affected.
Forms of kidney nephrosclerosis
Forecast
Nephrosclerosis is a chronic disease that lasts a long time with alternating periods of exacerbations and remissions. Therefore, with good compensation for the underlying disease, following the diet and doctor’s prescriptions, the patient will be able to reduce the number of periods of exacerbations and lead an active life.
But a malignant course of nephrosclerosis is also possible, in which kidney function quickly deteriorates, nephrons die and chronic renal failure sets in, which in the future can only be compensated with the help of hemodialysis or kidney transplantation.
Renal nephrosclerosis is a chronic disease. In the initial stages of its development, it is possible to maintain organ functions, but for this it is necessary to follow the doctor’s recommendations and adhere to certain restrictions.
For example, for patients with this diagnosis, it is important to minimize the consumption of table salt and constantly monitor calcium and phosphorus levels in the blood. With each exacerbation of the pathology, it is necessary to seek medical help and undergo a course of therapy each time.
https://youtu.be/odZoRLEy-I4
A “wrinkled kidney” identified at stages 3-4 requires a slightly different approach. In this case, all restrictions are much stricter. It is no longer possible to restore lost organ tissue. Therefore, in such situations, therapy comes down to ensuring the functionality of the remaining nephrons. Sometimes this is not enough.
Disease Prevention
Unfortunately, no one is immune from the development of nephrosclerosis. You can prevent the occurrence of pathologies that can provoke renal dysfunction by following a healthy lifestyle:
- dose physical activity and proper rest;
- adhere to the principles of dietary nutrition;
- avoid nervous tension and stressful situations;
- give up nicotine and alcohol addiction;
- monitor your blood pressure and undergo regular routine examinations;
- Strengthen your immune system and closely monitor your well-being; if unusual symptoms appear, you should consult a doctor in order to diagnose the disease in time and begin treatment.
Stopping the pathology at the beginning of development will prevent the occurrence of complications and the formation of nephrosclerosis.
Dietary requirements
Positive results from the recommended treatment can only be expected if you follow a diet. It is necessary to limit the consumption of protein foods, especially if kidney failure begins to form.
At the initial stages of the development of pathology, it is necessary to compensate for the lack of potassium in the body by eating dried apricots, baked potatoes, bananas and dried apricots. In the final stages, the consumption of such products is reduced.
At the beginning of the disease, you need to drink at least 6-7 glasses of water daily, but if edema develops and blood pressure frequently increases, this dose is reduced and two glasses of water are drunk more than the daily volume of urine excreted.
It is necessary to limit dairy products in the diet to a minimum, replenishing the calcium deficiency with whole grain bread, legume dishes and plenty of green vegetables.
Salt also requires restrictions. With minor kidney damage, no more than 10 g of salt per day is allowed; in later stages, the amount is reduced to 5-7 g.
https://youtu.be/pCg9PsiKugc
Symptoms
In the first stages, the symptoms of renal sclerosis are practically absent. Diagnosis of pathology occurs after preventive testing or during the diagnosis of another disease. In the absence of measures taken, the pathology develops and with each subsequent stage of development the severity of symptoms increases.
With nephrosclerosis, the main clinical picture relates to functional disorders of the organ, which provides symptoms:
- Swelling of the face and lower extremities.
- Lumbalgia.
- Hypertension associated with headaches. The pain syndrome is practically not overcome by painkillers.
- Changes in the physical properties of urine, as well as the presence of various inclusions in it - flaky sediment, changes in color to reddish, turbidity.
- Nocturnal enuresis.
- A sharp decrease in diuresis.
- Dry mouth and thirst.
- Apathy, weakness, lack of appetite. Also, patients with nephrosclerosis experience an aversion to meat foods.
- Dermatological disorders.
- Losing weight.
- Tachycardia, shortness of breath.
Symptoms and manifestations of nephrosclerosis
Such symptoms in adults and children require immediate diagnosis.
Therapy
Treatment of nephrosclerosis is based on two principles. The first is drug therapy, the second is surgical intervention.
If high blood pressure is diagnosed, drugs are selected that reduce blood pressure at a general level. The approach to the selection of funds is individual. Therapy is prescribed only by the attending physician. The choice of medications is based on the characteristics of the patient’s body and the possibility of using combinations of drugs.
There are several main groups of drugs:
- ACE inhibitors.
- Angiotensin receptor blockers.
A fundamentally important point is the correct diet. Salt is completely excluded. In some cases, carbohydrates are contraindicated.
Timely diagnosed first stage of the disease implies a classical approach to treatment:
- Hormonal therapy. Prednisolone, methylprednisolone. Dosages are determined by the doctor based on the functionality of the kidney.
- Cytostatic agents.
- Drugs that improve the functional abilities of the urinary system.
If the main cause is atherosclerosis, then medications from the statin group are prescribed. This allows you to reduce cholesterol levels in the blood, which has a beneficial effect on the functioning of the cardiovascular system. It also helps stop nephrosclerosis.
If the disease is diagnosed at one of the last stages, when the patient is experiencing serious problems, then the following methods are indicated:
- Blood dialysis . An effective procedure that cleanses the blood of toxins that are not filtered by the kidneys due to illness. Usually up to five procedures are performed. Already by the third procedure the patient feels much better.
- Peritoneal dialysis . It is also an effective method that can be carried out even at home.
- Nephrectomy or transplantation . It includes a whole range of procedures for adaptation of a new organ in the patient’s body. Consequences of surgery include the possibility of rejection by the patient's immune system.
Knowing the dangers of nephrosclerosis, the patient must strictly follow the doctors’ instructions.
Treatment with folk remedies
Treatment of kidney nephrosclerosis with folk remedies includes a set of measures aimed at reducing blood cholesterol levels and improving the functional abilities of the kidneys. And also, additional to the main anti-inflammatory and antiseptic therapy of renal diseases with herbal medicines.
Ayurveda is an Indian herbal medicine that is very popular. The main drug that is often used by patients and prescribed by doctors is Cyston. Treatment with this remedy is long-term and ensures normalization of renal pressure, alleviation of inflammatory processes and increased diuresis.
In addition to the Indian method, the use of herbs and plant extracts is recommended:
- Birch buds.
- Lingonberry extracts.
- Mixtures of flax seeds, strawberry leaves, birch buds, nettle leaves, knotweed, horsetail.
- Licorice root infusion.
Pelvic and calyx stones and hydronephrosis:
the kidney is either increased (a) or decreased (b) in size, the cavities of the pelvis and calyces are sharply expanded. The pelvis contains dense, oval-shaped stones with a smooth or rough surface, grayish-white in color. The mucous membrane of the pelvis and calyces is thickened. The cortex and medulla of the kidney are sharply thinned, compacted, and the kidney, when cut, resembles a thin-walled bag filled with stones and urine
Rheumatic heart disease:
the heart is enlarged in size and weight (the features of hypertrophy of its parts depend on the location of the defect and the degree of its compensation, for example, hypertrophy of the left atrium and right ventricle - “mitral configuration of the heart” with mitral disease). Sclerosis, hyalinosis, foci of calcification, deformation, fusion of the cusps of the mitral (a, c) and aortic (b) valves. Fusion, thickening and shortening of the mitral valve chords. The predominance of insufficiency (b) and stenosis (a, c) of the valves. In rheumatic mitral stenosis, the mitral valve opening resembles a button loop or fish mouth
Which doctor should I contact?
A nephrologist treats kidney diseases and their complications, in particular nephrosclerosis and renal failure. If necessary, consultations with other specialists are prescribed: a cardiologist (for high blood pressure), an endocrinologist (for diabetes), a vascular surgeon (for atherosclerosis of the renal artery), a urologist (for urolithiasis), an infectious disease specialist (for suspected kidney tuberculosis). You can get a referral for a kidney examination by contacting your general practitioner with relevant complaints.
myfamilydoctor.ru
Pathological anatomy
Sclerotic pathology develops in 2 phases. At the first stage, it is important to determine the disease, which is the cause of sclerotic processes in the organ. At this point, the relationship is quite easy to find. At the second stage, this is much more difficult to do, sometimes unrealistic. Wrinkling occurs very quickly, covering more and more kidney tissue. In this case, the organ increases slightly, its surface becomes granular, many irregularities form, and tissue scarring begins. Sometimes the organ shrinks evenly, sometimes not.
The disease can develop in benign and malignant forms. With benign sclerosis of the kidney, individual groups of nephrons shrink, the process develops slowly. Connective tissues first replace the intermediate space, and then the atrophied zones. With malignant wrinkling, pathological changes occur faster, which worsens the prognosis. Necrosis of arterioles and capillary glomeruli develops, and many complications arise. Death due to late diagnosis is common.
Prevention and prognosis
If pathological replacement is detected in a timely manner, the process is considered reversible, so the prognosis is relatively favorable. Carrying out adequate therapy makes it possible to achieve a long stage of compensation for nephrosclerosis. However, extensive changes in the kidney tissues that have begun lead to a deterioration in the functioning of the nephrons, their gradual death and the development of renal failure.
With malignant nephrosclerosis of the kidneys, a positive outcome of the disease is impossible. As a rule, symptoms of the disease appear in the later stages, when most of the nephrons are already damaged, which leads to total renal dysfunction. Due to the inability of the organ to remove decay products, they accumulate, which leads to intoxication and deterioration of well-being. If a kidney transplant is not possible, the patient's life expectancy is no more than a year.
https://youtu.be/cPyyMOK72uc
Measures to prevent kidney shrinkage involve, first of all, timely and adequate treatment of diseases: pathologies of the genitourinary system, as well as infectious and inflammatory processes. The development of nephrosclerosis is determined by the condition of blood vessels and blood pressure indicators. There are no special preventive measures, however, doctors suggest following the most common rules. As practice shows, a healthy lifestyle, diet, moderate physical activity, lack of overexertion, and proper rest can easily prevent the occurrence of kidney problems.
Classification
Atherosclerotic vascular lesions and the presence of blood clots are the main causes of the formation of the first stage of the pathology: primary nephrosclerosis.
Primary nephrosclerosis
With this type of renal sclerosis, the trophic capabilities of the organ tissues are severely impaired. This causes ischemic conditions. And in the absence of proper medical care, they provoke a kidney infarction. The potential risk of this pathology is that if the blood supply is completely inhibited, the excretory system stops functioning. This entails a state of renal failure. Such complications are life-threatening for the patient.
The main consequence of primary nephrosclerosis is primary kidney shrinkage. This is typical for acute hypertension.
In turn, nephroangiosclerosis is divided into several types:
Atherosclerotic nephrosclerosis
A pathological condition that develops as a consequence of atherosclerotic disease affecting the arterial vessels and arterioles of the kidney. As a result, the lumen of the vessels is greatly narrowed or completely blocked. Degenerative conditions of the organ arise as a result of decreased permeability due to thickening of the arterial walls.
The early stage is asymptomatic, while a characteristic complication of renal sclerosis is ischemia, as a result of which changes occur on the surface of the organ and scars form. The prognosis for this type is positive, because not all kidney tissue is affected by destruction, continuing to perform its functions normally.
Hypertensive nephrosclerosis
This type of pathology owes its name to the etiological factor that caused spastic conditions of the blood vessels. As with the previous form, pathogenesis includes ischemic damage to the organ, as well as the replacement of normal tissues with connective tissue.
In turn, the hypertensive type of pathology is divided into:
- Arteriolosclerotic nephrosclerosis. This is a malignant disease.
- Arteronecrotic nephrosclerosis. Benign course.
Involutive form
This form of renal sclerosis occurs in older patients. This is mainly due to calcium deposits on the walls of blood vessels. When the lumen narrows, the pathological condition develops according to the standard pattern.
https://youtu.be/HFm1XxcSadI
Secondary nephrosclerosis
The development of this form of the disease is due not only to atherosclerosis, but is also a consequence of other pathologies. Various infectious and inflammatory processes in the kidney system lead to this disease.
Main reasons:
- Chronic glomerulonephritis.
- Chronic pyelonephritis.
- Severe forms of kidney stones.
- Tuberculosis.
- Amyloidosis.
- Diabetic nephropathies.
- Nephropathy in pregnant women.
- Consequences of injuries and surgical interventions.
Atherosclerosis of the aorta with mural thrombus:
aortic intima with pronounced changes - with lipid (yellow) spots, fibrous (atherosclerotic) plaques rising above the surface of the intima, dense consistency, yellowish-white color, complicated lesions are visible - multiple ulcerations of atherosclerotic fibrous plaques, parietal thrombi (1), calcification (petrification). Thrombi are tightly or loosely attached to the wall of the aorta, with their heads in the area of ulceration of the atherosclerotic plaque; the surface of the blood clots is dull, uneven, often corrugated, the thrombotic masses have a dense consistency and crumble when cut.
Preventive measures
Among the preventive measures are:
- Dietary recommendations. Doctors do not advise neglecting fruits and vegetables. It is also not recommended to abuse meat.
- Body weight control.
- Maintaining proper water regime.
- Playing sports and giving up bad habits.
- Exclusion of self-medication.
- Periodic diagnostic procedures.
- No poisoning or intoxication by chemicals.
https://youtu.be/mrxWvaakJuk
Types and reasons
Nephrosclerosis is a dangerous disease, leading in some cases to death.
This disease can be provoked by a variety of reasons, among which a fairly common disease is hypertension, as well as atherosclerosis.
They are the ones who cause primary nephrosclerosis, which in medical practice is still interpreted as vascular, because the vessels of the kidneys are primarily affected.
Primary nephrosclerosis is a consequence of narrowing of the renal arteries and the formation of thrombosis. The cause may also be stagnation of venous blood in the kidneys, which is not uncommon for older people.
Ischemia provokes renal infarction and also contributes to the formation of scars.
Insufficient blood circulation and hypoxia lead to irreversible changes, as a result of which connective tissue begins to actively grow (fibrosis), and the kidney becomes wrinkled.
Secondary nephrosclerosis is a consequence of kidney diseases, which include:
- pyelonephritis;
- kidney tuberculosis;
- glomerulonephritis;
- amyloidosis;
- kidney injuries.
Diabetes mellitus also makes its negative contribution to the development of secondary renal sclerosis. It has been proven that the appearance of such a pathology could be provoked by radiation exposure.
https://youtu.be/q9-G-whNUjs
In pregnant women, renal sclerosis can be caused by severe forms of nephropathy.
Clinical manifestations
Clinical manifestations of primary nephrosclerosis can be detected in the late stages of hypertension. One of the early signs is polyuria and nocturia; protenouria and gross hematuria are also common. A decrease in the concentrating ability of the kidney is also considered a clinical manifestation of sclerosis. With severe vascular damage, an increase in pressure is observed, up to manifestations of arterial hypertension.
It is important! Also characteristic is a rapid increase in diastolic pressure, which contributes to the development of coronary insufficiency, cerebral hemorrhage, swelling of the optic nerve papilla or retinal detachment.
Manifestations of secondary nephrosclerosis can range from very minor to very severe, for example, conditions accompanied by edema, severe arterial hypertension or acute renal failure.
Gallstones (cholelithiasis):
the gallbladder is enlarged in size, its cavity is expanded, it contains multiple or faceted, ground to each other (faceted) or rounded stones of dark brown, gray or yellow color. The wall of the bladder is thickened, of dense consistency (on the side of the serous membrane there are often fragments of adhesions), whitish when cut, the mucous membrane is smooth, losing its velvety quality. Deposition of multiple yellowish-brown dense small granules may be observed in the mucous membrane (cholesterosis of the gallbladder, “strawberry” gallbladder)
studfiles.net
Diagnostic procedures
If the first symptoms of pathology appear, then biochemical studies of blood, urine, and instrumental studies of the organs of the urinary system are carried out.
Since the risk of developing the disease increases in the presence of chronic pathologies, patients suffering from diabetes mellitus, hypertension, atherosclerosis, and pathological weight gain are recommended to undergo tests once a year and undergo a full functional diagnosis.
This includes:
- Blood analysis. General and biochemical. Particular attention is paid to creatinine clearance.
- Analysis of urine. The density of urine is important.
- Ultrasonography.
- X-ray procedures, including contrast ones.
Nephrosclerosis
Nephrosclerosis (nephrosclerosis; Greek nephros kidney + sclerosis) is the replacement of the kidney parenchyma with connective tissue, leading to their compaction, wrinkling and dysfunction.
“Nephrosclerosis” is a clinical and anatomical concept. The process can develop as a result of various diseases of the kidneys and their blood vessels. In 1872, Gull and Sutton (WW Gull, Nephrosclerosis G. Sutton) first suggested that the cause of nephrosclerosis is damage to the vessels of the kidneys, and called it arteriolocapillary fibrosis. In 1914, Volhard and Far (F. Volhard, Th. Fahr) identified arteriolosclerotic changes in the kidneys as an independent nosological form of diffuse bilateral kidney disease and associated them with hypertension; They also proposed to distinguish between simple renal sclerosis - in a benign form of hypertension and its combined form - in hypertension with a malignant course.
Etiology and pathogenesis. Replacement of the renal parenchyma with connective tissue can be observed in advanced hypertension (see full body of knowledge) and is most often associated with narrowing of the renal arteries - primary Nephrosclerosis (angiogenic Nephrosclerosis), primary shriveled kidney. Due to insufficient blood supply and increasing hypoxia, dystrophic and atrophic changes in the renal parenchyma occur, followed by the proliferation of connective tissue. Depending on the nature of the process leading to narrowing of the renal arteries, nephrosclerosis is distinguished between hypertensive, or arteriolosclerotic, and atherosclerotic. In the pathogenesis of primary nephrosclerosis, chronic venous congestion is also important, in which the proliferation of connective tissue in the kidneys is associated with increased synthesis of tropocollagen under conditions of oxygen deficiency. Primary Nephrosclerosis includes post-infarction Nephrosclerosis, which develops with scarring of multiple renal infarctions (see full body of knowledge).
The growth of connective tissue in the kidneys can occur secondaryly, as a result of various diseases (secondary Nephrosclerosis, secondary wrinkled kidney). Secondary Nephrosclerosis is the outcome of inflammatory and degenerative processes that occur in the kidneys during chronic glomerulonephritis, pyelonephritis (pyelonephritic shrinkage of the kidneys, pyelonephritic shrinkage of the kidneys), kidney stones (calculous Nephrosclerosis), tuberculosis (tuberculous Nephrosclerosis), syphilis (syphilitic Nephrosclerosis), rheumatism ( rheumatic Nephrosclerosis), systemic lupus erythematosus (lupus nephrosclerosis), amyloidosis (amyloid scarring of the kidneys, or amyloid-shrinking kidneys), diabetes mellitus (diabetic nephrosclerosis).
Secondary Nephrosclerosis can develop after such adverse effects as trauma (including after repeated kidney surgeries), exposure to ionizing radiation, as well as in severe forms of nephropathy in pregnant women - preeclampsia and eclampsia. Spasm of the arteries, inflammation of the renal glomeruli and degeneration of the tubules characteristic of nephropathy after delivery in some cases transforms into chronic glomerulonephritis, which, slowly progressing, leads to shrinkage of the kidneys.
Acute infectious diseases such as hemorrhagic nephrosonephritis, leptospirosis, typhoid and typhus, scarlet fever, measles, as well as sepsis, are accompanied by changes in the parenchyma, interstitium and renal vessels that vary in mechanism of injury and severity - from focal glomerulonephritis without impaired renal function to tubular necrosis and acute renal failure. After these inflammatory and necrotic changes, nephrosclerosis of varying severity develops, which usually does not progress.
There is also involutive Nephrosclerosis, which is caused by age-related changes in the vessels of the kidneys, as well as atherosclerosis or hypertension, often observed in elderly and senile people.
Pathological anatomy. Of the primary nephrosclerosis, the most common is hypertensive, or arteriolosclerotic, nephrosclerosis. Far (Th. Fahr), depending on the nature, prevalence, severity of changes and characteristics of the course, distinguishes two forms - benign and malignant.
The benign form is characterized by arteriolosclerosis (Figure 1), often in combination with atherosclerosis of the renal artery and its large branches, atrophic changes in groups of nephrons with secondary hyalinosis of the glomeruli (Figure 2), an increase in the connective tissue stroma, hyalinosis of the papillae of the pyramids. Macroscopically, the surface of the kidneys is fine-grained, and when combined with atherosclerosis, it becomes coarsely lumpy. As arteriolosclerotic changes increase, combining plasmorrhagia (see full body of knowledge) and hyalinosis (see full body of knowledge), and the shutdown of new groups of nephrons, renal failure develops (see full body of knowledge).
The malignant form is characterized by fibrinoid necrosis of arterioles (arteriolonecrosis) and capillary loops of the glomeruli (Figure 3, a), edema of the stroma, hemorrhages, protein degeneration of the tubular epithelium. Very quickly, in response to necrotic changes, renal sclerosis develops (Figure 3, b). Similar changes can occur with eclampsia (malignant post-eclamitic nephrosclerosis).
| Rice. 1. Electron diffraction image of the afferent vessel of the renal glomerulus in a benign form of nephrosclerosis: accumulation of hyaline masses under the endothelium (indicated by an arrow); × 6000. | ||
| Rice. 2. Microscopic specimen of a kidney for a benign form of nephrosclerosis: sclerosis and hyalinosis of the renal glomerulus, CHIC reaction; × 750. | ||
| Rice. 3. Microscopic specimens of the kidney in a malignant form of nephrosclerosis: a - in the center the renal glomerulus is visible with fibrinoid necrosis of the afferent vessel (1) and glomerular blood capillaries (2); hematoxylin-eosin staining; × 310; b — glomerulus with severe sclerosis of the loops of blood capillaries and a decrease in the number of endothelial cells; hematoxylin-eosin staining; × 525. | ||
| Rice. 4. Macroscopic specimen of a kidney in a malignant form of nephrosclerosis: on the left - general view (the kidney capsule has been removed, the surface of the kidney is uneven, fine-grained, mottled due to numerous hemorrhages); on the right is a sagittal section of the kidney (the pattern of the structure is disturbed, numerous hemorrhages of various sizes are visible). | ||
Macroscopically, the surface of the buds is motley, fine-grained (Figure 4); the buds are not much different from the “great motley”. kidneys" for glomerulonephritis (see full body of knowledge). Arteriolonecrosis of the kidneys leads to renal failure.
According to Lelein (M. Lohlein), the benign form of arteriolosclerotic Nephrosclerosis corresponds to the first stage of Nephrosclerosis (initial Nephrosclerosis), which occurs clinically without manifestations from the kidneys, and the malignant form corresponds to the second stage of Nephrosclerosis (progressive Nephrosclerosis), which is characterized by a rapid course with the development of renal failure .
However, this sequence of the process is not recognized by everyone.
According to N.N. Anichkov, K.G. Volkova, M.A. Zakharyevskaya, the morphology of arteriolosclerotic nephrosclerosis reflects the features of the course of hypertension.
Atherosclerotic Nephrosclerosis occurs when there is a narrowing (caused by an atherosclerotic plaque) of the renal artery at the site of its origin or division into first and second order branches.
More often this process is one-sided, less often two-sided. In the kidney, wedge-shaped areas of parenchymal atrophy develop with collapse of the stroma and replacement of these areas with connective tissue or infarctions with their subsequent organization and scar formation (atherosclerotic wrinkled kidney, atherosclerotic nephrocirrhosis). Macroscopically, the kidney becomes coarsely tuberous, and it is often difficult to distinguish it from a kidney with nostrinfarction Nephrosclerosis. The function of such a kidney (kidney) suffers little, since most of its parenchyma remains intact. As a result of ischemia of the renal tissue, in some cases with stenotic atherosclerosis of the renal arteries, symptomatic (renal) hypertension develops.
Secondary Nephrosclerosis, which most often develops in chronic glomerulonephritis, is associated not only with glomerulonephritis as such (fibroplastic transformation of glomerular changes), but also with those changes in the vessels of the kidneys that constantly occur in this disease, reflecting the state of renal allergy (proliferative endarteritis), arterial hypertension (arteriolosclerosis, arteriolonecrosis), adaptation of the vascular system to switch off the “peripheral bed” of the kidneys (progressive elastofibrosis of the arteries with secondary lipoidosis). part o., secondary Nephrosclerosis always has angiogenic features.
Therefore, the morphological criteria for the differential diagnosis of primary (hypertensive) and secondary (nephritic) renal shrinkage are usually unclear.
Involutive changes in the kidneys are detected starting from 40-50 years of age and by 70 years of age lead to a reduction in the mass of active nephrons by approximately 40%.
Age-related renal atrophy is accompanied by a gradual thinning of the cortical layer of both kidneys, atrophy of the tubular epithelium until death and replacement of the tubules with scar tissue. The glomeruli undergo hyalinosis, and their number gradually decreases. Vascular resistance, which increases with age, leads to emptying of the glomerular capillaries and the formation of anastomoses between the afferent and efferent arteries, bypassing the glomeruli.
Nephrosclerosis in old age is associated primarily with age-related changes in the vessels of the kidneys, so it approaches the primary mechanism of development.
Main clinical signs. Clinical manifestations of primary nephrosclerosis usually occur in the late stages of hypertension, both benign and malignant. One of the early signs of kidney damage may be polyuria (see full body of knowledge) and nocturia (see full body of knowledge), however, nocturia is not always a consequence of polyuria and may indicate a disturbance in the circadian rhythm of kidney function. Proteinuria (see full body of knowledge) observed with nephrosclerosis is usually small and inconsistent.
Often with nephrosclerosis, microhematuria is observed, in some cases there may be macrohematuria (see full body of knowledge Hematuria). A decrease in renal clearance (see full body of knowledge) with a relative increase in the filtration fraction is manifested by a decrease in the concentrating ability of the kidneys (hyposthenuria), which is detected using the Zimnitsky test. Accordingly, the specific gravity of urine and its osmolarity decrease. In the case of severe vascular damage to the kidneys, leading to a significant decrease in renal blood flow, their pressor effect on blood pressure levels increases, which stabilizes at a high level and is difficult to correct with medication (see full body of knowledge Arterial hypertension).
Particularly characteristic is an increase in diastolic blood pressure, which is always above 120-130 millimeters of mercury.
In this regard, phenomena of overload and insufficiency of the left ventricular myocardium, coronary insufficiency, cerebral hemorrhages, swelling of the optic nerve papilla, retinal detachment, and in some cases progressive renal failure may occur.
Survey photographs reveal a reduction in the affected kidney (all or part) and unevenness of its contours.
With urography (see full body of knowledge), a decrease in the volume of the kidney and the size of the cortical layer is noted. On angiograms (see the full body of knowledge Renal angiography) there is a convergence and deformation of small arterial vessels (in the nephrogram phase, a decrease in the cortical layer and the unevenness of the outline of the affected kidney are clearly visible).
With radioisotope renography (see full body of knowledge Radioisotope renography) there is a slow accumulation, as well as a slow elimination of the radiopharmaceutical drug from the kidneys.
Scintigraphy (see full body of knowledge) determines the uneven distribution of the radionuclide in the tissue of the affected kidney; in some cases, its image may be absent or certain areas of the parenchyma may be preserved.
Manifestations of secondary nephrosclerosis can vary from minor renal dysfunction (not clinically expressed) to conditions accompanied by severe arterial hypertension, edema, nephrotic syndrome, a significant decrease in renal function, and the development of severe renal failure.
General principles of treatment and prevention. For nephrosclerosis without signs of renal failure and an unstable increase in blood pressure, treatment consists mainly of limiting the consumption of table salt (up to 0.5 grams per day) and the use of antihypertensive drugs (rauwolfia derivatives, ganglion blockers, dopegit, saluretics).
With the development of renal failure due to nephrosclerosis, the use of antihypertensive drugs is also indicated, however, intensive antihypertensive therapy can lead to a drop in renal blood flow and an increase in azotemia; They use a diet with limited salt and protein, anabolic agents, lespenefril, saluretics.
In the malignant course of hypertension with the rapid development of nephrosclerosis and progression of renal failure, in order to turn off the reninangiotensive mechanism, they resort to embolization of the renal arteries or nephrectomy (see full body of knowledge), patients are transferred to hemodialysis (see full body of knowledge) or undergo kidney transplantation (see full body of knowledge) Body of knowledge Kidney transplantation).
Prevention of nephrosclerosis consists of timely treatment of diseases leading to its development.
Radiation nephrosclerosis refers to the long-term consequences of ionizing radiation on the body (see full body of knowledge) and is detected many months or years after irradiation.
Morphologically, radiation nephrosclerosis is expressed by atrophy of the renal tubules, interstitial fibrosis and sclerosis of the renal vessels. There is no single view on the development of radiation nephrosclerosis. The dominant hypothesis is about primary damage to the renal glomeruli, which, according to a number of researchers, can be caused by immunological factors. There is a point of view that radiation nephrosclerosis develops as a result of primary damage to blood vessels by ionizing radiation. It is possible that this process is based on damage to the genetic apparatus of the renal vascular endothelium. It is also assumed that the cause of radiation nephrosclerosis is primary damage to the renal tubules. Sometimes radiation nephrosclerosis is considered as a result of simultaneous damage to the renal parenchyma and the vascular system. There is an opinion that the basis of radiation nephrosclerosis is interdependent vascular disorders and changes in the interstitial substance of the kidneys.
Basic information about radiation nephrosclerosis was obtained in experiments on animals, as well as as a result of observations of victims of atomic bomb explosions in Hiroshima and Nagasaki and patients exposed to local irradiation for tumors in the lumbar region. The severity of radiation nephrosclerosis depends on the type of ionizing radiation, its dose and the nature of the dose distribution in time and space (see Doses of ionizing radiation, Time factor of irradiation). After acute irradiation in absolutely lethal doses, radiation nephrosclerosis does not occur, since in the short period preceding the death of the organism, sclerotic processes in the kidneys do not have time to develop. Acute radiation sickness of mild and moderate severity in the long term can result in the development of radiation nephrosclerosis. With total irradiation, the development of radiation nephrosclerosis in at least 50% of animals, according to most researchers, occurs when exposed to a dose close to 500 rad. There is information about the occurrence of radiation nephrosclerosis after total exposure to ionizing radiation in doses of 100-300 rad. Under conditions of local irradiation of the kidneys, the development of nephrosclerosis can be observed in the dose range of ionizing radiation from 1000 to 2500 rad.
In radiol practice, the kidneys are considered as critical organs (see full body of knowledge) during radiation therapy for cancer metastases in the paraortic lymphatics, nodes, ribs or vertebrae from ThXI to LIV, as well as for tumors of the intestine, uterus, cardiac esophagus and some other organs. The greatest caution should be observed when carrying out neutron and proton therapy, since these types of ionizing radiation have a more pronounced effect in relation to radiation Nephrosclerosis Alpha radiation is also characterized by high efficiency in this regard. Experiments have shown that when affected by polonium, which is mainly excreted through the kidneys, in the long term, radiation nephrosclerosis is formed against the background of developing chronic radiation sickness.
Clinically, radiation nephrosclerosis in mild cases is manifested by proteinuria, slight hypertension; renal function is not impaired. In severe cases, hypertension develops, which cannot be treated with medication, and renal failure.
Treatment is symptomatic (salt restriction, antihypertensive drugs).
| Vepkhvadze R.Ya.; Serov V.V. Tareev E.M. |
⇐ Go to the main page of the site ⇐ | ⇑ Return to top of page ⇑ | Ordo Deus Library ⇒ ⇒ |
⇐ Nephroptosis | ⇓ Complete body of knowledge. Volume one A. ⇓ |
Renal sclerosis
Nephrosclerosis (renal sclerosis) is a disease accompanied by the replacement of healthy renal parenchyma by connective tissue. This causes the walls of the arterioles and arteries to thicken, so the vessels can no longer fully supply blood to the kidney. Subsequently, with sclerosis, the nutrition of the tubules and glomeruli is disrupted, the kidney gradually decreases in size and shrinks.
Since nephrons are replaced by connective tissue cells, the latter are not able to perform the main function of the kidneys - filtration. The patient's chronic renal failure progresses, and various disorders of other organs develop.
Diagnosis of the disease
Using the Zimnitsky test, you can evaluate the concentrating ability of the kidneys; any deviations may indicate a disruption in their functioning, and, consequently, the development of sclerosis.
To confirm the correct diagnosis, it is necessary to evaluate the results of x-ray, ultrasound and radionuclide studies.
Ultrasound examination reveals changes in the size of the kidney, the thickness of the parenchyma, atrophy of the cortex and its relationship with the medulla.
Urography shows an increase in kidney volume, thickening of the cortical layer of the parenchyma and calcium deposition. On an angiogram, specialists can detect narrowing of small arteries, uneven contours of the affected kidney, and a decrease in the cortex.
During a radionuclide study, slow accumulation and elimination of the radiopharmaceutical are observed.
Scintigraphy reveals an uneven distribution of radionuclide in the tissue of the affected kidney.
Clinical signs
Symptoms of nephrosclerosis and patient complaints are as follows:
- swelling of the face, especially the area around the eyes
- swelling of the legs and hands
- increasing weakness and fatigue
- nausea, loss of appetite, especially aversion to meat and other protein foods
- dry, pale skin and itchy skin
- nagging pain in the lower back
- high blood pressure, which is difficult to treat, is accompanied by persistent headaches
- decrease in the amount of urine excreted
Prognosis for recovery
The diagnosis of nephrosclerosis implies different outcomes. Since this is a chronic pathology in which remissions and exacerbations constantly occur, by compensating for the pathology of one kidney, dietary nutrition and following the recommendations of the attending physician, the number of attacks can be reduced. In this case, the patient will lead a normal life and will not lose his ability to work. The prognosis for the outcome of malignant shrinkage of the kidney is not so favorable, since the nephrons die and renal failure develops. Usually the patient awaits permanent hemodialysis or transplantation. Failure to do this leads to death.
Symptoms of the disease
In the initial stages, shriveled organs do not make themselves felt at all or the symptoms are mild. The problem can only be diagnosed by blood and urine tests, which show small changes in the functioning of the organ. The main symptoms appear at a late stage. The first symptoms are:
- increased urination;
- frequent urination;
- the presence of protein in the urine;
- high blood pressure;
- swelling.
In addition, there are:
- symptoms of damage to the heart and blood vessels;
- Iron-deficiency anemia.
Nephrosclerosis of the kidneys: symptoms, treatment (including folk remedies), diet and other aspects
Diet for kidney nephrosclerosis is a prerequisite. You should eat food in small portions, but often.
It is advisable to limit protein foods. Porridge, potatoes, and bread should be excluded from the diet.
It is better to get protein from eggs, dairy products, and meat. It is recommended to eat fish dishes, as fish contains a lot of phosphorus.
To prevent swelling, it is necessary to limit the consumption of salty foods and salt itself. However, it is not advisable to completely give up salt.
The diet must be balanced - contain the necessary vitamins and microelements. You can eat nuts, buckwheat, seaweed, and drink mineral waters high in magnesium. With secondary nephrosclerosis, you need to drink a lot of water (up to 3 liters per day), but if you have heart or vascular diseases, you should not do this.