Ocular uveitis is a pathological inflammation of the vascular network of the eye. The choroid (uveal) membrane must nourish the entire eyeball and the inflammatory process can begin anywhere in the uveal tract or eye. This includes: the iris, blood vessels and ciliary body.
Uveitis of the eye has a serious impact on a person's vision. If this is a severe or advanced form of uveitis, then the consequences will be noticeable. The patient may lose part of his vision or become completely blind. Even if eye uveitis has even the slightest symptoms, you should urgently consult an ophthalmologist. The disease can occur in both adults and children.
The causes of the disease are so diverse that it makes no sense to describe them all. We will tell you the main symptoms and causes of the development of ocular uveitis. What is ocular uveitis, and what treatment is needed?
What is uveitis?
Uveitis is a general concept that refers to inflammation of various parts of the choroid (iris, ciliary body, choroid). This disease is quite common and dangerous. Often (in 25% of cases) uveitis leads to visual impairment and even blindness.
The appearance of this disease is facilitated by the high prevalence of the vascular network of the eye. In this case, blood flow in the uveal tract is slowed down, which can lead to retention of microorganisms in the choroid. Under certain conditions, these microorganisms are activated and lead to inflammation.
Watery eyes as one of the signs of uveitis
The development of inflammation is also influenced by other features of the choroid, including different blood supply and innervation of its different structures:
- the anterior section (iris and ciliary body) is supplied with blood by the anterior ciliary and posterior long arteries, and is innervated by the ciliary fibers of the first branch of the trigeminal nerve;
- the posterior section (choroid) is supplied with blood via the posterior short ciliary arteries and is characterized by the absence of sensory innervation.
These features determine the location of the lesion in the uveal tract. The anterior or posterior region may be affected.
Causes of uveitis
A variety of reasons can lead to the development of an inflammatory process in the choroid of the eyes:
- Metabolic disorders;
- Infections;
- Decreased general immunity;
- Autoimmune diseases.
Uveitis can also be caused by a penetrating eye injury.
With the infectious nature of the disease, its causative agents are a variety of pathogenic microorganisms - viruses (cytomegalovirus, herpes virus), bacteria (Koch bacillus, Brucella), fungi, protozoa (toxoplasma, chlamydia). In this case, infectious uveitis can be primary (inflammation is initially localized in the tissue of the choroid) or secondary.
In the latter case, the pathogen penetrates into the eye tissue from any other source of infection present in the patient’s body through the bloodstream (hematogenous route). Secondary infectious uveitis can become a complication of diseases such as septic endocarditis, sinusitis, meningitis, purulent forms of tonsillitis, etc.
Uveitis can also occur against the background of a number of systemic diseases, for example, diabetes mellitus, Reiter's syndrome, rheumatoid arthritis, systemic lupus erythematosus. But it is not possible to establish the exact cause of the development of uveitis even with a very thorough examination of the patient in all cases.
Classification
The anatomy of the eye predisposes the disease to be localized in different locations of the uveal tract. Depending on this factor, there are:
- Anterior uveitis: iritis, iridocyclitis, anterior cyclitis. Inflammation develops in the iris and vitreous body. This variety is the most common.
- Median (intermediate) uveitis: posterior cyclitis, pars planitis. The ciliary or vitreous body, retina, and choroid are affected.
- Posterior uveitis: choroiditis, chorioretinitis, retinitis, neurouveitis. The choroid, retina and optic nerve are affected.
- Generalized uveitis – panuveitis. This type of disease develops if all parts of the choroid are affected.
Symptoms of uveitis
The insidiousness of uveitis lies in the fact that this disease can go unnoticed by the patient for quite a long time, without causing any painful or other unpleasant symptoms. This is due to the fact that the choroid of the eye is devoid of nerve endings, the irritation of which could indicate the onset of a pathological process.
Subsequently, the symptoms of uveitis largely depend on the cause of the disease, the pathogenicity of the microflora that caused it, the extent of the lesion, the general health of the patient and many other factors.
In the initial stages of anterior uveitis, many patients complain of the appearance of a slight “fog” or “veil” before the eyes, which is accompanied by rapid fatigue. At the same time, visual acuity often decreases. As a result, the usual contact lenses or glasses no longer satisfy the user.
If the patient does not see a doctor, the inflammatory process continues to progress. The symptoms listed above include redness and pain in the eyes, increased intraocular pressure, lacrimation and photophobia. Vision progressively decreases until it is completely lost.
For posterior uveitis, redness of the eyes and the appearance of pain in them are not typical. The decrease in visual acuity gradually progresses. Patients often experience “spots” or “fogginess” in front of the affected eye. In advanced stages, dull pain often occurs in the very depths of the orbit. The appearance of this symptom is unfavorable, as it indicates the involvement of optic nerve fibers in the inflammatory process.
Causes of inflammation
Uveitis can develop due to a wide variety of reasons, the main ones being:
- infections;
- allergic reactions;
- injuries;
- systemic and syndromic diseases;
- metabolic and hormonal regulation disorders.
Infectious uveitis is the most common: they occur in 43.5% of cases. Infectious agents in this case are mycobacterium tuberculosis, streptococci, toxoplasma, treponema pallidum, cytomegalovirus, herpesvirus, and fungi. As a rule, such uveitis is associated with infection entering the vascular bed from any source of infection and develops with sinusitis, tuberculosis, syphilis, viral diseases, tonsillitis, sepsis, dental caries, etc.
Increased specific sensitivity to environmental factors plays a role in the development of allergic uveitis - drug and food allergies, hay fever, etc. Serum uveitis often develops with the introduction of various serums and vaccines.
Uveitis can occur against the background of systemic and syndromic diseases, such as:
- rheumatism;
- rheumatoid arthritis;
- psoriasis;
- spondyloarthritis;
- sarcoidosis;
- glomerulonephritis;
- autoimmune thyroiditis;
- multiple sclerosis;
- ulcerative colitis;
- Reiter's, Vogt-Koyanagi-Harada syndromes, etc.
Post-traumatic uveitis occurs due to eye burns, penetrating or contusion injuries to the eyeball, and foreign bodies entering the eyes.
The following diseases also contribute to the development of uveitis:
- metabolic disorders and hormonal dysfunction (diabetes mellitus, menopause, etc.);
- diseases of the circulatory system;
- diseases of the visual organs (retinal detachment, conjunctivitis, keratitis, blepharitis, scleritis, perforation of corneal ulcer).
And this is not the entire list of diseases as a result of which uveitis can arise and develop.
Treatment of uveitis
Uveitis has no standard treatment regimen.
Therapy includes a number of drugs from different groups; their action is aimed at eliminating the etiological factor and relieving pathological symptoms, they use:
- antiviral and immunomodulators;
- vasodilators;
- antibiotics;
- non-steroidal anti-inflammatory drugs (NSAIDs);
- hormones: topical and systemic corticosteroids;
- immunosuppressants;
- antihistamines;
- mydriatics and cytoplegics;
- vitamins;
- enzymes, etc.
Additionally, physiotherapy is used.
Cycloplegic and corticosteroid drops are initially prescribed to relieve pain and reduce inflammation.
Important
Before treatment, intraocular pressure must be assessed and the herpetic nature of uveitis excluded.
In patients with severe cases who do not respond to steroids or who have complications with conventional therapy, immunosuppressants may be used. They are also considered as first-line therapy for the treatment of uveitis in Behçet's disease, Wegener's granulomatosis and necrotizing scleritis. These diseases are often associated with life-threatening systemic vasculitis.
Necrosis factor inhibitors
Immunomodulatory therapy is used in situations where long-term treatment with systemic corticosteroids is necessary. New treatment approaches are drugs that target specific mediators of the immune response. Although these drugs have been studied primarily in patients with rheumatoid arthritis, psoriasis, and Crohn's disease, the similarities in disease pathogenesis have stimulated interest in using these drugs to treat various inflammatory eye diseases. Tumor necrosis factor alpha blocking molecules (eg, adalimumab, infliximab) have been found to effectively modulate the immune response in patients with uveitis.
In June 2019, the FDA approved adalimumab (Humira) for the treatment of noninfectious intermediate uveitis, posterior uveitis, and panuveitis in adults. The basis is the results of two pivotal phase 3 studies: VISUAL-I and VISUAL-II, which showed that adult patients with active and controlled non-infectious intermediate uveitis, posterior uveitis and panuveitis had a significantly lower risk of treatment failure with adalimumab.
Intraocular implants and intravitreal injections
Another new treatment option is the use of intraocular pharmacotherapy through injections and surgical placement of implants. Cataract formation and increased intraocular pressure are common side effects, and the risk of endophthalmitis (usually sterile) is approximately 0.1%.
Cycloplegics
Symptoms and complications of inflammation can be reduced by topical cycloplegic agents. Short-acting drops (cyclopentalate) and long-acting drops (atropine) can be used to reduce photophobia caused by ciliary spasm and to break up or prevent the formation of posterior synechiae (adhesions).
Cyclopentolate causes mydriasis after 30-60 minutes and cycloplugia after 25-75 minutes. The effect lasts up to 24 hours.
Corticosteroids
Corticosteroids slow the release of arachidonic acid from phospholipids, inhibit transcription and cytokine action, and limit the activity of B and T cells. They are indicated for inflammatory diseases of non-infectious causes. Three routes of administration are available: local, periocular and systemic, which is determined individually in each case. Because of serious side effects, especially with high doses and long-term use, immunosuppressants are commonly used for chronic or sight-threatening uveitis.
note
For anterior uveitis, steroid drops are used. Prednisolone acetate 1% is preferred. Sometimes steroids can cause ocular hypertension; therefore, you need to monitor intraocular pressure once a month.
Intravitreal implants of dexamethasone and fluocinolone may be considered as an option to provide prolonged treatment.
Periocular corticosteroids are used to treat posterior uveitis.
In the presence of a systemic disease that additionally requires ophthalmological treatment; For uveitis that does not respond well to other treatments, systemic oral or intravenous therapy is necessary. Prednisone is the most used oral corticosteroid.
Prednisolone ophthalmic (Pred Forte) treats acute inflammation after eye surgery or other types of eye injury. It reduces inflammation and neovascularization of the cornea, inhibits the migration of polymorphonuclear leukocytes and reduces capillary permeability. In cases of bacterial infections, the use of antibacterial agents is mandatory.
Other drugs:
- Dexamethasone (Ozurdex implant for chronic non-infectious uveitis),
- Fluocinolone ophthalmic (Retisert implant),
- Triamcinolone for intravitreal administration,
- Prednisone, etc.
Immunosuppressive agents
Immunosuppressants: antimetabolites, T-cell suppressors and cytotoxic agents. Antimetabolites include azathioprine, methotrexate, and mycophenolate mofetil. T-cell inhibitors include cyclosporine and tacrolimus. Cytotoxic agents: cyclophosphamide and chlorambucil. Most drugs take several weeks to be effective and are initially given in combination with oral corticosteroids.
Symptoms and diagnosis
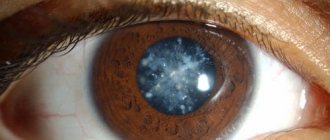
At the initial stage of the disease, the color of the iris changes and adhesions appear. The lens of the eye becomes cloudy. Further, uveitis can manifest itself in different ways, depending on the type and form of inflammation. Common symptoms are:
- redness of the eye;
- photophobia;
- chronic lacrimation;
- aching or sharp pain;
- pain and discomfort;
- deformation, constricted pupil;
- the appearance of a slight “fog” before the eyes;
- deterioration of visual acuity, up to blindness;
- unclear perception;
- increased intraocular pressure (heaviness in the eye is felt);
- transition of inflammation to the second eye.
Diagnostics
During the diagnostic period, the main role is played by the patient’s medical history and all information about his immunological status. Thanks to an examination by an ophthalmologist, it is possible to clarify the location of inflammation in the area of the choroid.
Uveitis of the eye is determined by skin testing for any allergens. These may include: staphylococcus, streptococcus or toxoplasmin. If we touch on tuberculous etiology, then an important symptom of uveitis will be damage to the conjunctiva of the eye and the appearance of conflicts (specific pimples) on the skin.
Inflammatory processes of a systemic nature and existing infections when diagnosing ocular uveitis can be confirmed through blood serum analysis.
Treatment
The effectiveness of uveitis treatment depends on how accurately the diagnosis is made and the causes of the disease are established. Treatment should be carried out by an ophthalmologist, taking into account the causes of the disease and the individual characteristics of the body. Self-medication can only make the situation worse.
As a rule, the doctor carries out local antibacterial, anti-inflammatory and immunostimulating therapy. In parallel, physiotherapeutic treatment, enzyme therapy and physioreflexotherapy are also carried out.
Drugs are prescribed in the form of ointments, drops, injections and tablets. Sometimes hormonal and vasodilator drugs are prescribed. And at the initial stage of the inflammatory process, it is necessary to take medications that dilate the pupil. This is especially true for anterior uveitis. Sometimes the doctor recommends the use of homeopathic medicines. But only an experienced specialist should select them.
If the disease causes an increase in intraocular pressure, antiglaucoma drugs are used. In complex cases, surgery may be required, including the use of a laser.
Treatment is usually carried out in a hospital. Patients who have suffered inflammation of the choroid are under medical supervision for another two years.
Traditional methods of treating uveitis are also known. But they need to be treated with caution so as not to complicate the situation. Traditional medicine advises washing your eyes with a decoction of chamomile, calendula, rose hips, sage, and marshmallow. Aloe juice diluted with water and rubbed over the eyes also helps. Before using these recipes, you should definitely consult your doctor.
Nature of the disease
There are several forms of ocular uveitis:
– Acute uveitis of the eyes. Begins suddenly, duration is limited;
– Recurrent uveitis. Has periods of remission. In most cases, at least 3-4 months if no treatment;
– Chronic uveitis of the eye. Recurrence of episodes of illness, even after treatment. May recur in less than three months.
As a rule, treatment for ocular uveitis is purely individual. Everything will depend on the diagnostic results and additional thorough examinations. In the treatment of uveitis, both local and systemic therapy can be used. If uveitis has complications, surgical intervention will be required.
Classification of ocular uveitis
In medicine, there is a certain classification of the disease. It all depends on its location:
– Peripheral. With this disease, inflammation affects the ciliary body, choroid, vitreous body, and also the retina.
- Front. A type of disease that is much more common than others. Accompanied by damage to the iris and ciliary body.
- Rear. The optic nerve, choroid, and retina become inflamed.
– When there is inflammation throughout the entire choroid of the eyeball, this type of disease is called “panuveitis.”
As for the duration of the process, an acute type of the disease is distinguished, when the symptoms intensify. Chronic uveitis is diagnosed if the pathology worries the patient for more than 6 weeks.
Complications
Comprehensive and timely treatment of acute anterior uveitis usually leads to recovery within 3-6 weeks. Chronic uveitis is prone to relapse due to exacerbation of the primary disease. Complicated uveitis can lead to the following consequences:
- formation of posterior synechiae;
- development of angle-closure glaucoma, cataracts, retinal dystrophy and infarction, optic disc edema, retinal detachment;
- significant decrease in visual acuity.
Structure of the eye
Symptoms of uveitis development
Inflammation of the vascular part of the eye has various manifestations. This depends on the location of the lesion, the severity of the infectious process and the resistance of the body as a whole. Clinical forms have the following characteristic features:
- acute – pain in the eye, redness with a purple tint, intolerance to bright light, constricted pupil, high pressure inside the eye;
- chronic – few symptoms, slightly reddened eyes, moving dots in the field of vision;
- the anterior one occurs with an accumulation of cells on the cornea; due to adhesions with the lens capsule, cataracts, swelling of the optic nerve head, and glaucoma are formed.
- peripheral – both eyes are affected, vision is reduced, spots before the eyes;
- posterior - vision is blurred, the contours of objects are unclear, there is swelling or ischemia in the fundus, blockage of blood vessels, retinal detachment;
- generalized - more common in sepsis and causes inflammation of all layers of the eyeball, characterized by an extremely severe course and rapid loss of vision.
Watch the video about the causes of red eyes:
Prevention
To prevent relapse of autoimmune uveitis, it is important to maintain eye hygiene and avoid hypothermia and overwork. If there are various allergic diseases, then during the acute period it is very important to monitor the general condition of the body in order to avoid the transition of uveitis to a chronic form that cannot be treated.
Retinal angiopathy or dystrophy is a dangerous disease that can lead to blindness.
Episcleritis of the eye: treatment with folk remedies:
How to choose contact lenses without a doctor, read this article.
Types of uveitis
The broad classification of uveitis can lead to difficulties in diagnosis. The inflammatory process varies in symptoms, causes, and location. Depending on where the source of inflammation is located, the following uveitis is distinguished:
- Front. Detected in 70% of cases. Characterized by damage to the ciliary body (cyclitis) or the iris (iritis). If the inflammation has spread to both the iris and the ciliary body, it is called iridocyclitis.
- Peripheral (intermediate). Inflammation affects that part of the visual organs that is located behind the ciliary body. This process is rarely diagnosed.
- Rear. An uncommon occurrence in which the choroid is affected. If the development of inflammation is not stopped, it will spread to the optic nerve and retina (choriotenitis). Damage to the posterior portions of the choroid is called choroiditis. Damage to the entire uveal tract is called panuveitis.
Based on the nature of inflammation, scientists gave uveitis the following classification:
- Serous inflammation.
- Fibrinous lamellar uveitis.
- Purulent process.
- Hemorrhagic inflammation.
- Uveitis of mixed type.
The characteristics of the course of the disease give grounds to distinguish the following types of uveitis:
- Spicy. It develops against the background of a surge in the activity of microorganisms that cause infection. In this case, the symptoms of inflammation are clearly expressed. There is overflow of the blood vessels of the eyeball with blood. My eye hurts. Visual functions deteriorate.
- Chronic. Uveitis turns into this form if it is not treated. The cause of its development also includes autoimmune diseases. The symptoms of the disease periodically worsen.
- Sluggish. Symptoms of the disease are poorly expressed. Their manifestation is observed within 2 months. After which the acute stage of inflammation is revealed.
There are also primary and secondary pathologies. In the first case, it is caused by general diseases of the body. In the second – diseases of the visual organs.
conclusions
So, uveitis is a complex disease that can occur due to many reasons. Bacterial conjunctivitis, a common condition, can also lead to uveitis. The most important thing is for the doctor to identify the true cause of the disease and prescribe treatment as early as possible. Chronic uveitis is very dangerous and can lead to incurable eye diseases, including blindness. You should not expect the disease to go away on its own. The first symptoms should be a signal that you urgently need to run to an ophthalmologist. Because Since the symptoms of eye diseases are mostly similar, you should not hope that you can cure the manifestations of this disease at home. Moreover, similar symptoms can also manifest as cataracts, which you can read about here.
Diagnostic measures
After talking with the patient, the doctor makes the first conclusions about a possible disease. To create a clear clinical picture, he conducts the following studies:
- Determining the degree of visual acuity.
- Measuring intraocular pressure.
- Checking the reaction of the pupils to a light stimulus.
- Examination of the anterior chamber of the eye (gonioscopy).
- Ophthalmoscopic examination.
- Ultrasound of the eyeball.
- Tomography of the visual organs.
- Assessing the condition of the blood vessels of the eyes using x-rays (angiography).
- Checking blood circulation indicators in the choroid (rheoophthalmography).
The uveitis treatment regimen is based on the identified results.
Reasons for development
The disease can develop for many reasons, but most often it occurs due to infection - streptococcus, herpevirus, fungi, toxoplasma, cytomegalovirus, tuberculosis bacillus.
Often the disease develops against the background of:
- Sinusitis.
- Caries.
- Tonsillitis.
- Tuberculosis.
- Syphilis.
- Viral infection.
- Sepsis.
The listed diseases can lead to the spread of infection to the blood vessels of the eyes.
In addition, the cause of pathology can be:
- Allergies caused by food or medications.
- Injury to the organs of vision (burn, foreign body, bruise, etc.).
- Eye diseases (for example, conjunctivitis, keratitis, scleritis, etc.).
- Blood diseases.
- Glomerulonephritis, ulcerative colitis, rheumatism, etc.
Uveitis in children
When ocular uveitis occurs in a child, the cause is most often trauma to the eye tissue.
Children lead a very energetic, active lifestyle. And bruises, scratches, abrasions are a common occurrence in childhood. Most often, microtraumas heal quickly and do not cause much discomfort to the child, but more serious injuries can cause complications.
Another cause of eye inflammation is an exacerbation of an existing infection. Often infection occurs in the womb. A child can acquire cytomegalovirus and toxoplasmosis.
And also in the body of almost every person there is a herpes virus, which, due to a combination of various factors (decreased immunity, unfavorable environmental conditions), can be activated.
The causes of infections and uveitis of the eyes are:
- impaired metabolism;
- weakened immune system;
- complication after psoriasis;
- weakening of the body due to tuberculosis, diabetes.
Symptoms of ocular uveitis in a child are practically absent:
- the eyeball may turn red;
- the pupil reacts worse to light;
- the child sees worse in the distance with one eye;
- swelling appears around the eyes.
In this case, pain may be completely absent.
Note! Without treatment, eye inflammation can move to the second eyeball, and after two months the retina will detach. The last complication can only be corrected through surgery; drugs cannot cure retinal detachment in the eye.
Etiology of the disease
Uveitis is characteristic of autoimmune diseases, when damage to the eye structures occurs by pathological immune complexes. It often develops against the background of diseases such as ankylosing spondylitis, rheumatoid arthritis, multiple sclerosis, systemic lupus erythematosus, sarcoidosis, and vitiligo.
The pathology is observed against the background of leukemia, retinoblastoma, and oncology in advanced stages.
The disease can be caused by various pathogens:
- viruses (HIV, herpes simplex virus, cytomegalovirus);
- bacteria (syphilis, brucellosis, tuberculosis, leprosy);
- parasites (toxoplasma, causative agents of cistercecosis, amoebiasis);
- fungi (candidiasis, cryptococcosis and other mycoses).
The genetic factor plays a major role: almost 70 out of 100 patients produce the HLA-B27 antigen. As a rule, these patients are observed for systemic diseases of the joints and connective tissue.
The disease has age-related characteristics:
- in children it often develops against the background of infectious diseases;
- in older people – against the background of systemic diseases, cancer pathology, reduced immunity.
Classification of the disease and its symptoms
The main morphological forms of pathology: anterior uveitis, median, posterior, peripheral and diffuse. The anterior one, in turn, is divided into iritis, cyclitis and iridocyclitis. The posterior one is called choroiditis, and the diffuse one is called panuveitis or iridocyclochoroiditis. Depending on the nature of the course, acute, chronic and recurrent uveitis are distinguished. Each form of uveitis has a number of its own characteristics. The following symptoms are characteristic of anterior uveitis:
- redness of the pupils;
- fear of light;
- chronic lacrimation;
- constriction of the pupils;
- Pain in the eyes;
- increased intraocular pressure.
Peripheral uveitis of the eye, symptoms:
- eye damage that is symmetrical in nature;
- the appearance of “floaters” before the eyes;
- noticeable deterioration in visual acuity and quality.
With posterior uveitis, symptoms appear later. A person will have the following symptoms:
- vision becomes very blurred;
- everything visible around is distorted;
- impaired color perception;
- the patient constantly sees “spots” floating in front of his eyes, and there may often be peculiar flashes;
- visual acuity sharply decreases.
The severity of the inflammatory process also differs in different forms of the disease. It is most intense with anterior uveitis. The iris of the eye becomes greenish or rusty-brown, the pupil narrows greatly and almost does not react to light. Tiny plaques appear on the cornea and move freely in the eye fluid. They arise as a result of the appearance of a large number of pigment proteins along with lymphocytes. The acute form lasts up to 1.5-2 months. If left untreated, it goes into a chronic stage, which begins to recur with the onset of cold weather. Peripheral uveitis is sluggish and has the most vague symptoms, so it is difficult to diagnose. It affects structures of the eye that are very difficult to examine. But if the necessary measures are not taken, serious complications and the development of secondary eye diseases may occur.
Symptoms
Pathology manifests itself depending on the location, the presence of pathogenic microflora, and the reactivity of the body as a whole. In the acute form, the following appear:
- Pain in the eyes;
- Redness;
- Irritation;
- lacrimation;
- Photophobia;
- Constriction of the pupil;
- Deterioration of visual function.
The pericorneal injection becomes purple in color, and intraocular pressure begins to increase with the acute nature of the pathology. But the chronic form often occurs either asymptomatically or with minor manifestations such as redness of the eyes, as well as the presence of moving spots in front of the eyes.
During diagnosis, an indicator of the acute phase of anterior uveitis is accumulation of precipitated cells in the area of the corneal endothelium, as well as a cellular reaction in the fluid of the anterior chamber. A complication of this type of pathology is often synechiae, which are areas of fusion between the iris and the lens, as well as keratopathy, glaucoma, and so on.
Important! The symptoms of uveitis are quite vague. Each type of pathology requires its own type of treatment. Don't self-medicate!
Peripheral uveitis affects both eyes at once. Cloudy areas appear before the eyes, and central vision decreases. With posterior uveitis, blurred vision, distortion of objects and spots in front of the eyes may appear. Complications of the posterior type of the disease include retinal detachments, macular ischemia, macular edema, and so on.
The most severe form of pathology is iridocyclochoroiditis. It develops most often due to sepsis. Accompanied by panophthalmitis or endophthalmitis. If uveitis is associated with certain pathologies, then headaches, baldness, vitiligo, enlarged lymph nodes, vasculitis, arthritis, skin rashes, shortness of breath, increased salivation, and so on may additionally make themselves felt. It all depends on what kind of disease caused inflammation in this area.
Causes
The following reasons can lead to the appearance of uveitis::
- depressed state of immunity;
- infection in the eyes;
- disturbance in the body's autoimmune processes;
- metabolic problems;
- penetrating eye injuries.
Sometimes uveitis is not an independent disease, but is a consequence of other infectious diseases: sinusitis, tonsillitis, chlamydia, herpes, rheumatoid arthritis and even diabetes.
Sometimes the cause of uveitis cannot be determined even after a thorough diagnosis, but most often doctors are able to find out what was the provoking factor for the development of the disease and prescribe the correct treatment.
Peripheral (median) uveitis
Description
This uveitis was identified as a separate nosological group in 1967.
The primary inflammatory focus is localized in the pars plana of the vitreous and the peripheral part of the choroid in the form of retinal perivasculitis
. As a result of inflammation, a preretinal cyclic membrane is formed, which can cause rupture and retinal detachment.
This is an inflammatory disease with a vascular factor. Most often, the first symptom is decreased vision due to clouding of the vitreous.
, as well as edema and degeneration of the macular area. It is more common in young people and occurs after the flu, acute respiratory infections and other infections. The first complaint with this disease is decreased vision. When the ciliary body is captured by the process, there may be clouding of the moisture in the anterior chamber. If the exudate settles on the trabeculae, secondary uveitis may occur.
If vascular phenomena predominate (periphlebitis, perivasculitis), hemorrhages may appear in the retina and vitreous body
.
The iris is usually not clinically changed, and posterior synechiae are not formed. Changes in the anterior layers of the vitreous body first take the form of small powdery opacities, which after various periods (from 6 months to 2 years) accumulate in the area of the flat part of the ciliary body and on the extreme periphery of the retina in the form of snow-like opacities or exudative masses. Peripheral exudate
is the most significant and permanent sign of parsplanitis.
It is white or grayish-white, dense, well circumscribed, localized near the dentate line, spreading into the region of the ciliary body. Snow-like foci of peripheral exudate can be single or numerous. Their presence in the area of the flat part of the ciliary body can be determined by examination with a three-mirror Goldmann lens and indentation of the sclera. The most common localization of such changes is in the zone between 3 and 9 o'clock in the lower part of the anterior segment of the eye. By their nature, snow-like masses lying on the flat part of the ciliary body refer to inflammatory, exudative changes or condensed areas of the vitreous body. Their predominant localization in the lower zone of the flat part of the ciliary body may be associated with the attraction of opacities of the vitreous body to its inflammatory changes at its base or with the fact that the largest number of vitreous cells are located in the lower ocular part. In some cases, especially in young patients, posterior vitreous detachment
. Wrinkling of the vitreous caused by inflammation leads to tractional tension of the retina, and sometimes to ruptures of the internal limiting membrane. The development of complex cataracts, starting at the posterior pole, is also noted. Sometimes gradually, and sometimes quite quickly it becomes full. The process is often complicated by the development of secondary glaucoma.
Cystic macular edema
and mild papilledema are typical symptoms accompanying parsplanitis. Sometimes changes in the retinal vessels such as vasculitis or perivasculitis appear. After partial resorption of the exudate, pigmentation appears in the atrophy zone, characteristic of choroidal damage. The percentage of complications of peripheral uveitis according to the literature is as follows:
- cataract - 60.7%,
- maculopathy - 42.8%,
- papilledema - 17.8%.
Less common complications include retinal detachment and retinal hemorrhages. Thus, with peripheral uveitis, three stages of the process are noted:
- early stage - decreased visual acuity, external accommodation, cellular reaction in the aqueous humor of the anterior chamber and small corneal precipitates, the appearance of cells in the vitreous body;
- an intermediate stage, characterized by further deterioration of vision and the appearance of strabismus, simultaneously with increased inflammatory phenomena in the vascular tract, expressed in photophobia, pain and the formation of exudate in the vitreous body;
- late stage, which is characterized by sudden loss of vision due to cystic macular degeneration, the formation of posterior subcapsular cataracts and sometimes atrophy of the eyeball.
In the clinical manifestation of parsplanitis, forms of diffuse and focal inflammation are distinguished. Diffuse form
corresponds to the described picture of the disease.
With focal inflammation,
granulomatous foci appear around the entire circumference of the flat part of the ciliary body without localization in any meridian. Initially, the granulomas have a grayish color and are not clearly demarcated. After their resorption, atrophic pigmented scars remain. In acute inflammatory processes during the recovery stage, infiltration in the lower part of the base of the vitreous disappears.
Chronic inflammatory processes that exist for a long time lead to secondary changes in the form of scarring. Primarily affecting the vitreous cortex and inner layers of the retina, they cause fibrous degeneration of the base of the vitreous.
and diffuse thickening of the retinal periphery. Scarring may be widespread with the formation of cysts. Sometimes newly formed vessels and retinal tears appear, leading to retinal detachment. An important sign is noted that makes it possible to distinguish the disease from parsplanitis: scarring occurs only in the lower zone of the periphery of the retina, without affecting the flat part of the ciliary body. The sources of peripheral deposits of exudate are all inflammatory processes that involve the vitreous cortex. Such deposits can quickly dissolve in focal chorioretinitis. In patients with disseminated peripheral chorioretinitis, exudate can cover the entire periphery of the retina, simulating the picture of posterior cyclitis. However, the flat part of the ciliary body remains free of exudative deposits.
Analysis of clinical signs allows us to identify three criteria for differentiating anterior and posterior uveitis with parsplanitis:
- exudate is located in the lower periphery;
- it is always intravitreal;
- the flat part of the ciliary body does not show signs of inflammation in the initial phase of the disease, when certain morphological changes have not yet formed.
The etiology of the disease has not been established. The involvement of the herpes virus and immunological factors is possible.
—-
Article from the book: Eye diseases. Complete Guide | Perederiy V.A.
Choroid: structure and its functions
The uveal membrane has a rather complex structure. It occupies the space between the retina and the sclera and looks like grapes. This is where its name comes from - “uvea”, which in Russian means “grape”. It has 3 main departments:
- iris;
- ciliary body;
- choroid - the choroid itself (located directly under the retina, lining it on the outside).
The important functions assigned to the choroid include:
- Regulating the flow of sunlight. This protects the eyeball from excess light.
- Transport of nutrients throughout the retina.
- Removing decay products from the eye.
- Participation in the adaptation of the eyeball, i.e. changing the refractive power of the optical system of the eye for a clearer and clearer perception of different objects that are distant from it at different distances.
- Production of intraocular fluid.
- Normalization of pressure inside the eye.
- Thermoregulation.
The most important function of this membrane is to supply the organs of vision with blood. Thanks to the anterior, posterior short, and long ciliary arteries, blood is transported to all areas of the eye. However, due to the fact that each part of the eyeball is supplied with blood from its own source, infection also occurs separately.
Lifespan
How long do people live with uveitis? The disease does not affect life expectancy, but it causes significant complications if left untreated:
- Partial or complete loss of vision.
- Cataract.
- Retinal disinsertion.
- Vasculitis.
- Glaucoma.
- Panuveitis.
- Damage to the optic nerve.
- Loss of an eye.
In order not to lead to such complications and not to suffer from uveitis at all, you should adhere to prevention:
- Don't overwork and don't get too cold.
- Do not injure your eyes.
- Maintain eye hygiene.
- Avoid allergic reactions.
- Treat all infectious diseases of both the eye and other organs.
- Contact an ophthalmologist if symptoms appear.