Parenchymal or hepatic jaundice is a symptomatic complex expressed in the yellowness of the skin and mucous membranes. The reason for this is the excessive accumulation of bile pigment (bilirubin) in the body, which is a signal of liver dysfunction.
In addition, there is the concept of “false jaundice”. It occurs when not bilirubin accumulates in the body, but carotene, a naturally occurring dye found in vegetables and fruits. For example, pumpkin, carrots, oranges and even beets. Yellowness of the skin and mucous membranes can also be associated with long-term consumption of picric acid or a number of medications.
Causes of hemolytic jaundice
Prehepatic jaundice is not associated with liver damage. It occurs when red blood cells are destroyed and a large amount of free bile pigments is released. At the same time, hepatocytes are not able to utilize a huge amount of the substance, so bilirubin accumulates in the bloodstream and tissues of the body, which provokes the appearance of a yellow tint to the skin and mucous membranes.
The process of transformation of bile pigments in the body of a healthy person
Free bilirubin has a toxic effect on cells of the central nervous system. This condition is especially dangerous for newborns. The accumulation of bile pigments under the skin, their appearance in free form in the bloodstream, and their excretion in urine in the form of urobilin are the main reasons for the brightness of the symptoms of the pathological condition.
Prehepatic jaundice can be congenital or acquired. In newborns, hemolytic disease is a hereditary pathology. The reasons for its appearance are as follows:
- congenital hemoglobin disorders;
- the presence of high levels of bilirubin in the blood, which is accompanied by icterus of the skin and sclera, but liver parameters remain within normal limits;
- the action of chemical compounds of arsenic, hydrogen sulfide, phosphorus, which provokes increased breakdown of red blood cells.
Also, suprahepatic jaundice can be the result of pneumonia, aseptic conditions, endocarditis, Addison's disease and some types of oncological processes. It is important to carry out a differential diagnosis of the types of pathology, as well as to evaluate the possibility of the appearance of non-hemolytic jaundice, which has a hereditary predisposition and is manifested by a deficiency of a certain enzyme in the patient’s body.
What is jaundice
Hyperbilirubinemia or jaundice is a pathological condition that occurs when the content of bilirubin in the blood plasma increases. Bilirubin easily reacts chemically with proteins, forming yellow compounds. It is for this reason that the skin and whites of the eyes become stained. First of all, jaundice is detected on the sclera, since the white membrane of the eyes contains a lot of elastin, a protein that has the greatest affinity for bilirubin. The skin with jaundice turns yellow later because the protein collagen, which is abundant in the skin, has less affinity for bilirubin.
The mechanism of pathology development
The bile pigment bilirubin is found in the human body in several forms: free and bound. Free bilirubin (or indirect, as it is also called) appears in the bloodstream during the breakdown of red blood cells. It is insoluble in water and is toxic to the body.
If metabolic processes occur under normal conditions, bilirubin combines with blood proteins and enters the liver cells, where, through a series of chemical transformations, it becomes a direct (bound) substance. Next comes the connection with glucuronic acid. The pigment becomes low-toxic and begins to dissolve in water. It is this substance that is usually determined during a biochemical blood test.
In this form, the pigment combines with bile, enters the intestinal tract, and becomes urobilinogen. A certain amount binds to bile acids, the rest becomes part of the feces and is excreted from the body. A disruption of physiological processes in adults and children, which is characterized by the appearance of large amounts of toxic bilirubin in the blood, is hemolytic jaundice.
Causes of hepatic jaundice
- Parenchymal jaundice occurs due to liver damage by bacteria, viruses, and toxins of various origins. Most often, this disease can be associated with syphilis, malaria and toxoplasmosis.
- If we are talking about a specific damage to toxins, then it can be caused by organic and inorganic poisons. For example, alcohol, poisonous plants and mushrooms, exposure to hazardous production conditions, contact with poisonous reptiles and insects.
- Uncontrolled use of certain medications can also provoke hepatic jaundice. For example, drugs of the “antibiotics” class or the banal “Paracetamol”.
- Hereditary predisposition also plays a role in the occurrence of hepatic jaundice. Some people have a genetic defect in the form of a deficiency of liver ligandin proteins or an enzymatic deficiency of UDP-glucuronyl transferase.
- Also, the cause of parenchymal jaundice can be Wilson-Konovalov disease - excessive accumulation of copper in the liver, which causes its further dysfunction.
Hemolytic disease
One of the causes of hemolytic disease of newborns is considered to be incompatibility of the mother and fetus with regard to the Rh blood factor (very rarely - blood group incompatibility). Pathology can occur both during pregnancy and after the baby is born.
The presence of Rh conflict is diagnosed throughout pregnancy, starting from the second trimester
The main symptoms and signs are anemia and jaundice, which tend to progress. A high level of indirect bilirubin is observed in the patient's blood. More often, a similar problem occurs when a woman has Rh-negative blood, but her man has an Rh-positive factor. The result may be hemolytic disease in their child.
If rhesus positive red blood cells (in a baby) enter a pregnant woman’s body, her defense system reacts to them as if they were foreign bodies. Own antibodies begin to be actively synthesized to destroy fetal red blood cells. In this condition, the child's blood is considered hostile to its mother.
If a similar situation is observed during the first pregnancy, the pathology is resolved positively, since so far a small amount of antibodies is observed, but with each subsequent pregnancy the risk of a Rh conflict, which results in hemolytic disease of the newborn, increases several times.
Provoking factors for the development of pathology can be:
- ectopic pregnancy that occurred earlier;
- history of abortions and miscarriages;
- blood transfusion with incorrect determination of the patient's Rh factor.
Nutrition correction
After a diagnosis of obstructive jaundice is made, the patient must adhere to a strict diet. Doctors recommend table No. 5B, which provides for the exclusion of any irritants of the gastric tract. The main requirements for nutrition correction are:
- Cooking without using salt or oil.
- The diet includes boiled lean meat.
- Soups should be slimy and based on easily digestible grains.
- Meals are divided up to 8 times a day.
- Crackers and dried bread are consumed in limited quantities.
- Fat per day should not exceed 40 g.
- The diet is enriched with fiber.
- Spicy or high-calorie foods, flour products, and store-bought sweets are excluded.
Constant adherence to a diet allows you to improve your well-being, reduce the risk of stone formation, and prevent their movement. Proper nutrition should become part of a person’s life to support the body in the fight against disease.
Classification
Hemolytic disease has several types:
- hydropic,
- anemic,
- icteric.
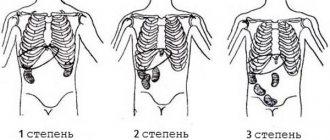
Depending on the severity of the pathological condition, there is a mild degree, which occurs in 10% of patients, a moderate degree of severity (in every third patient) and a severe degree of damage (in every fifth patient).
As a rule, mild degrees of pathology have minor changes in blood tests. The average degree is characterized by increased levels of bilirubin. The clinical picture may be present, but the symptoms of intoxication, as well as complications, are mild. Typically, the quantitative indicators of bilirubin are above 60 µmol/l, and the hemoglobin level is less than 140 g/l. The condition occurs during the first two days after the baby is born. Accompanied by an increase in the size of the spleen.
Important! A severe degree of pathology is accompanied by edema of the entire body, damage to brain structures, and serious heart and pulmonary failure.
Reasons for development
Hemolytic or suprahepatic jaundice is caused by excessive formation of bilirubin due to hemolysis of red blood cells and the inability of the liver to eliminate it.
Pathogenesis of suprahepatic jaundice in adults:
- Infectious causes - sepsis, malaria.
- Immune. Jaundice occurs due to the oversensitivity of the immune system to antigens.
- Toxic - poisoning with lead, phenylhydrazine, arsenic hydrogen, sulfonamide drugs, as well as due to the bite of poisonous snakes.
- Hereditary causes (hemoglobinopathies, enzymopathies). Hemolytic jaundice occurs against the background of sickle cell anemia, thalassemia, Minkowski-Choffard disease and others.
With hereditary hemolytic anemia, abnormalities in the structure of red blood cells are observed against the background of the appearance of abnormal lipids and proteins in the membrane. They change visually and also have low resistance to changes in temperature and pressure.
The main factor in the occurrence of prehepatic jaundice is the destruction of red blood cells, which provokes the release of a large amount of indirect bilirubin, which does not have time to combine with hepatocytes. The following causes of hemolytic jaundice can be distinguished:
- Hereditary predisposition to self-destruction of red blood cells. Among genetic risk factors, there are hereditary defects of erythrocyte membranes (acanthocytosis, hemoglobinuria, ovalocytosis, microspherocytosis and others), deficiency of enzymes such as pyruvate kinase, which catalyzes the penultimate reaction of glycolysis with the help of magnesium and potassium and glucose-6-phosphate dehydrogenase, necessary for binding active forms oxygen at the last stage. Also, hemolytic jaundice can occur against the background of sickle cell anemia or thalassemia.
- Exposure to foreign antibodies during transfusion of isoincompatible blood. Also, similar factors are characteristic of a number of diseases - sepsis, malarial plasmodium, rubella, measles, leptospirosis, etc. A separate group includes poisons that purposefully destroy the structural elements of the blood - snake venom, aniline, arsenic, hydrogen sulfide, nitrobenzene, lead, phosphorus and others. It is worth noting that hemolytic jaundice can be caused by taking drugs from the groups of quinines, antipyretics and sulfonamides.
- Interruption of normal blood circulation as a result of hemorrhage, hematoma or myocardial infarction, mild, hemorrhagic stroke, dissecting aneurysm, hemothorax, gastric or intestinal bleeding. This is due to the fact that large accumulations of blood in problem areas are resolved in tissues, cavities or parenchymal organs. At the same time, free bilirubin is actively released.
- Certain types of diseases provoke mechanical damage to red blood cells. This often occurs when blood passes through peripheral vessels close to bony prominences. In science this is called marching hemoglobinuria.
The risk group for the disease includes:
- Patients fighting malignant tumors, regardless of their location. This is especially true for patients with acute radiation sickness and those undergoing radiotherapy, since the powerful ionizing effect provokes the destruction of the erythrocyte membrane;
- Newborns with low activity of liver enzymes who do not have time to take part in internal metabolic processes;
- Patients with systemic connective tissue pathologies.
Symptoms of the disease
The most severe degree of damage is the edematous form. Often the baby dies in the womb of the mother, but if he is still born, the birth is accompanied by significant swelling of the entire body. There is no jaundice, but pronounced anemia is observed. Symptoms of the condition:
- blue-gray skin;
- increase in the size of the liver and spleen;
- muscle tone is sharply reduced;
- reflexes are impaired or completely absent;
- the fetus is motionless.
The presence of the disease can be diagnosed during the period of intrauterine development, which depends on the timing of the development of the pathology
The baby's body weight can be several times higher than normal. This is due to significant swelling of the body. On examination, there is pronounced pastiness, bruising on the skin, and the presence of pathological fluid in the abdominal cavity.
If an anemic type of disease is present, the child is born with signs of anemia and icterus of the sclera, skin, and mucous membranes. During the first weeks of the baby's life, the symptoms of anemia intensify, the size of the liver and spleen increases, and intoxication increases.
The icteric type of hemolytic disease occurs if the Rh conflict appears at the end of pregnancy. The severity of the symptoms of the pathological process reaches its peak development on days 4-5 from the moment of birth. The main symptom is significant jaundice. In parallel, bleeding, decreased reflexes, convulsions, and severe drowsiness are observed. The higher the bilirubin levels in the blood, the more severe the manifestations of the pathology.
Diet for jaundice
Diet therapy plays an important role in the treatment of liver and biliary tract diseases. The goal of the diet is to reduce the load on the liver. Refractory and animal fats are the most difficult to digest. For this reason, it is recommended to reduce the consumption of fatty, fried foods. It is prohibited to consume fatty meats and fish, confectionery and sausages, smoked meats, other deli meats and products containing trans fats.
The consumption of protein foods and “slow carbohydrates”, cereals, vegetables and fruits, and cereals is not limited.
It is recommended to increase fluid intake if there are no contraindications (edema, abdominal hydrops, liver cirrhosis with portal hypertension). Meals are fractional, in small portions, but frequent, 5-6 times a day. Alexander Ni
Diagnostics
Even during the period of bearing a baby, a woman must undergo tests to determine the presence of Rh conflict. If the attending physician notices abnormalities in the blood data, then another ultrasound examination is prescribed, during which the following indicators are determined:
- thickness of the placenta, the rate of its increase in size;
- presence of polyhydramnios;
- the presence of free fluid in the child’s abdominal cavity;
- condition of the baby's spleen and liver.
Cardiotocography is mandatory, during which the fetal heart rate and the possible risk of hypoxia are assessed. If necessary, amniocentesis and cordocentesis are prescribed - methods for examining the amniotic fluid and blood of the baby. As a rule, differential diagnosis of the condition is not accompanied by difficulties. The type of jaundice should be determined. This is important for choosing further treatment tactics.
Diagnosis of jaundice
The appearance of parenchymal jaundice indicates the development of a serious disease. And this is a good reason to see a doctor and conduct a comprehensive examination.
Laboratory tests are performed to identify the cause of the syndrome.
If jaundice is suspected, patients are prescribed the following tests:
- Clinical blood test.
- Biochemistry of blood.
- General urine analysis.
- Physical, chemical, microscopic examination of stool.
- Ultrasound of the liver, abdominal organs.
If the methods described above do not help establish an accurate diagnosis, then the doctor prescribes a biopsy (sampling of fragments of liver tissue). This diagnostic method is used if the pathology has a hidden course.
Hepatic jaundice is an important syndrome in liver diseases, so it is necessary to determine the type of pathology in order to draw up a treatment regimen.
Differential diagnosis of jaundice, taking into account the mechanism of origin, development of the disease and its individual symptoms:
| Symptoms and indicators | Hemolytic jaundice | Hepatic jaundice | Obstructive jaundice |
| Development factors | Destruction of red blood cells inside cells or vessels, infarctions of various organs (usually lungs), large hematomas | Hepatitis, cirrhosis, familial non-hemolytic jaundice, etc. | GSD (gallbladder stones), tumors or narrowing of the area in the area of the porta hepatis, neoplasms on the pancreas or major duodenal papilla, etc. |
| Color of the skin | Pale yellow | Yellow-orange | Greenish |
| Itchy skin | No | Moderate itching in some patients | Severe itching |
| Liver dimensions | Normal | Hepatomegaly | Hepatomegaly |
| Bilirubin level | Increased concentration of unconjugated bilirubin | Increased amount of bound and unbound bilirubin | High concentration of conjugated bilirubin |
| ALT, AST levels | Fine | Promoted | Normal or slightly elevated |
| Cholesterol concentration | Normal | Low | Increased |
| Alkaline phosphatase activity | Normal | Normal or slightly increased | Significant increase |
| Gamma-glutamitranspeptidase level | Normal | Slightly increased | Increased |
| Urine color | Dark | Dark | Dark |
| Presence of urobilin in urine | Promoted | Promoted | No |
| Bilirubin in urine | No | Promoted | Increased |
| Shade of feces | Dark | Light lightening | Discolored |
| Presence of stercobilin in feces | Promoted | Low level | Absent |
Differential diagnosis is important, as it helps determine the treatment regimen, as well as avoid dangerous complications.
Possible consequences
Dangerous complications include:
- premature death (while still in the womb);
- disability combined with muscular dystrophy;
- strabismus;
- severe impairment of hearing and visual acuity;
- tendency to allergic reactions;
- liver inflammation;
- Cerebral palsy.
Severe jaundice is an important diagnostic sign
How does the disease manifest itself?
Hemolytic jaundice is characterized by symptoms observed in many liver lesions:
- liver enlargement detected by palpation or ultrasound;
- dilation of the veins of the esophagus;
- yellow coloration of the whites of the eyes and skin;
- sharp pain in the right side under the rib;
- changes in the color and composition of feces and urine;
- the appearance of a venous network on the skin of the abdomen.
Hemolytic jaundice is differentiated by symptoms that are characteristic only of this type - enlarged spleen (splenomegaly), yellowness of the skin against a background of general pallor, increased process of red blood cell synthesis in the bone marrow.
A characteristic symptom is also intense coloration of stool. The liver cannot cope with the large volume of bilirubin that is formed during the active breakdown of red blood cells (this condition is called hemolytic crisis). In this case, chills, nagging pain in the spleen area, and a decrease in hemoglobin levels may be added to the main symptoms.
Treatment
The specialist prescribes complex therapy, which can combine the use of medications and surgery. When choosing, be sure to take into account the quantitative indicators of bile pigment in the blood and the severity of the pathology itself. The main goal of therapy is to carry out detoxification measures.
Surgical treatment is manifested in the form of replacement blood transfusion. Used for severe hemolytic disease, as well as for the progression of intoxication symptoms. Hemosorption and plasmapheresis are often used. Among medications, antibacterial drugs and hormones are widely used; to reduce signs of intoxication, saline solution, glucose solution, and albumin are administered intravenously.
Important! Choleretic drugs, hepatoprotectors, adsorbents and vitamins will help maintain the condition of hepatocytes.
A serious condition is an indication for replacement blood transfusion. Direct transfusion is not used at this stage due to the fact that the risk of contracting hepatitis and HIV infection is quite high, so transfusion of red blood cells, as well as fresh frozen plasma, is used.
Hemosorption is carried out to cleanse the blood of toxic substances. In parallel, phototherapy is carried out, which makes it possible to convert indirect bilirubin fractions into low-toxic ones. The child’s body is irradiated with fluorescent lamps, as a result of which the breakdown products of bile pigment are excreted from the body with urine and feces. Thanks to the use of phototherapy, the frequency of the need for blood transfusion and the development of complications of hemolytic disease decreased by more than 40%.
Special conditions are required for the procedure
Treatment of jaundice
Hyperbilirubinemia is most often just a consequence of a particular disease. To eliminate jaundice, treatment of the underlying pathology is necessary. Due to the large number of possible causes of increased bilirubin levels in the blood, doctors of several specialties treat this problem.
Hemolytic jaundice mainly refers to diseases of the blood system and is treated by hematologists. Cases of poisoning with hepatotropic toxins, drugs and poisons require consultation with a toxicologist. Treatment of liver diseases is the specialty of a hepatologist. Liver tumors are treated by oncologists. Subhepatic jaundice, regardless of the cause, requires consultation with a surgeon (surgeon-oncologist).
Etiotropic therapy of hyperbilirubinemia
Etiotropic therapy is treatment aimed directly at the cause that caused the pathology. For example, if a gallstone blocks the outflow of bile, the etiotropic treatment for mechanical hyperbilirubinemia will be surgical intervention aimed at removing the foreign body. Causal therapy is not possible in all cases. Although the cause of hemolytic bilirubinemia in hereditary hemolytic anemias is known, there are no treatments that can eliminate the defect in the genes that lead to the premature destruction of red blood cells.
Pathogenetic therapy of hyperbilirubinemia
Pathogenetic therapy is aimed at individual parts of the mechanism leading to the disease or contributing to the deterioration of the patient’s condition. For example, infusion therapy, which uses intravenous infusions of saline or other detoxifying agents, helps remove excess bilirubin through the kidneys.
Prevention
Preventive measures consist of carrying out specific and non-specific measures. The procedure for proper blood transfusion and carrying a child throughout pregnancy with adequate registration and carrying out all the necessary tests are nonspecific.
Specific prevention consists of administering anti-D immunoglobulin during the first two days after the baby is born. This is necessary if the mother has Rh-negative blood and the fetus has Rh-positive blood. The administration of immunoglobulin is also indicated after an abortion.
If during pregnancy the antibody titers steadily increase, it is necessary to detoxify the blood by purifying it with sorbents. It is also possible to use an exchange intrauterine blood transfusion: washed red blood cells are infused at the 27th week of pregnancy + further delivery is carried out after the 29th week of gestation.
Direct and indirect bilirubin
For proper exchange of bilirubin, it must be bound to the protein albumin. Bilirubin can be direct or indirect.
Indirect (in analyzes it can be designated as ID-BIL) – one that has not yet undergone connections. This fraction of bile pigment usually increases significantly in jaundice of the hemolytic and parenchymal type.
Direct (D-BIL) – bound to a protein, also called bound. It increases with mechanical hyperbilirubinemia, however, with some hereditary pathologies, hepatic jaundice also leads to this. In parenchymal jaundice, an increase in D-BIL may be observed, but will be minor.
Features of therapy
Conservative therapy is recommended for the treatment of jaundice. It is aimed at eliminating the causes and symptoms of pathology. Patients are recommended to undergo detoxification treatment for jaundice. It is necessary if the pathological process occurs in an acute form. Patients are recommended to use it if there is severe intoxication of the body. For the treatment of jaundice, it is recommended to use infusion techniques in accordance with diagnostic data.
If the cause is infection or bacteria, jaundice is treated with antibiotics. Patients are recommended to first test for the sensitivity of microorganisms to the active components of the prescribed drug. When treating jaundice, the patient must strictly follow the treatment regimen. Patients are simultaneously prescribed antifungal therapy.
Treatment of jaundice is carried out with hepatoprotectors if it occurs against the background of damage to hepatocytes. With the help of medications, liver tissue is protected and restored. If the pathological process develops against the background of anemia, then patients are given hematotherapy. Treatment for jaundice involves blood plasma transfusion. Blood substitutes can also be used for this purpose.
If an oncological process occurs in the organ, then the use of chemotherapy, radiotherapy or surgery is recommended for the treatment of jaundice. During the course of the pathology, a decrease in the body’s defenses is observed, so patients are prescribed immunotherapy. If there is an accumulation of a large number of stones in the patient’s gallbladder, then treatment of jaundice requires surgery to remove them. The progression of pathology in an advanced state requires the use of hormonal medications.
For the treatment of jaundice, it is recommended to use folk remedies that are safe. They belong to the category of auxiliary techniques. During treatment of jaundice, the patient must adhere to a dietary diet. It consists of eliminating foods from the diet that have a destructive effect on the liver.
Treatment of jaundice should be comprehensive. The choice of technique and certain drugs is carried out by the doctor in accordance with the type of pathology, as well as the individual characteristics of the patient.
Why is jaundice dangerous?
This pathology, as an independent and separate entity, does not become a threat to human life or health. However, in the absence of proper treatment and if it worsens (the addition of a secondary infection or complications of the main diagnosis), serious problems may arise that significantly worsen the patient’s quality of life. They can cause serious disorders in the functioning and structure of the liver, gallbladder and most internal organs. Pure bilirubin has a toxic effect on the body, so an increase in its concentration leads to significant intoxication, which has a detrimental effect on the nervous system. The brain is especially sensitive to the effects of toxic substances. When jaundice is diagnosed in a child, it can cause delayed intellectual development.
Causes
Jaundice is a sign indicating disturbances in the functioning of the body in adults and children. The effect of the prescribed therapy will be noticeable only if the cause is discovered. Most often, jaundice affects the body due to disruption of the following organs and systems:
- The circulatory system, the function of which is to produce bilirubin from waste blood cells.
- The liver, which serves as a place for the accumulation and transfer of bilirubin to part of the bile.
- The gallbladder, in which bile heats up and affects the large intestine.
Causes and symptoms of the obstructive form of the disease
Mechanical or subhepatic jaundice got its name due to the fact that the causes of the pathological process are located below the liver - in the bile ducts. If a mechanical obstacle arises in the way of secretion, cholestasis develops.
When this type of pathology occurs, an increase in bilirubin in the direct fraction is detected.
This type of disorder is not accompanied by damage to the liver tissue; for this reason, liver tests do not change.
Direct bilirubin enters the bloodstream and is excreted by the kidneys as part of the urine, which leads to its coloration in a darker color. Bilirubin, excreted from the body through the kidneys, does not enter the intestines, which leads to lightening of the stool.
The main causes of the superior and inferior mechanical forms of jaundice are different. In addition, there are certain features of the manifestation of clinical symptoms.
The causes of hyperaural jaundice are as follows:
- Formation of metastatic foci in the area of the liver hilum.
- Formation of lymphogranulomatous nodes in the area of the liver hilum.
- Formation of syphilitic gumma.
- Formation of tumor formations in the right or left hepatic duct.
- Development of liver echinococcosis.
When the processes of bile outflow from the liver are disrupted, the vena cava is compressed, while the icteric bladder is not able to absorb the changes that occur. This form of the disease is characterized by:
- accelerated progression;
- increasing feeling of skin itching;
- the patient experiences a gradual yellowing of the skin, and this symptom intensifies over time and the skin acquires a yellow-green or gray-yellow tint;
- obligatory development of ascites;
- the manifestation of pain is moderate.
The main causes of subjacent jaundice are:
- Development of cholelithiasis.
- Oncological processes affecting the head of the pancreas, the common bile duct and the outlet of the pancreatic duct.
During palpation, if obstructive jaundice is detected, the patient feels attacks of pain, the doctor during the procedure reveals an increase in the size of the gallbladder.
Obstructive jaundice provoked by a neoplastic process is characterized by a gradual increase in characteristic signs and pain.
Features during pregnancy
During gestation, the liver experiences excessive stress associated with toxicosis, hormonal changes, and decreased immunity. Causes of Gospel disease during pregnancy include:
- malnutrition;
- excess sex hormones;
- vitamin deficiency;
- exacerbation of chronic pathologies;
- psycho-emotional stress;
- cholestasis (cessation of the flow of bile into the small intestine).
Jaundice is detected in the first or third trimesters. Women complain of bitterness in the mouth, severe nausea, itchy skin, vomiting, lack of appetite, and weight loss. In the last stages of pregnancy, jaundice is caused by gestosis, that is, late toxicosis. Its manifestations:
- headache;
- yellowing of the skin;
- convulsions;
- bone pain;
- discomfort in the liver area;
- Digestive problems.
Gospel disease has dangerous negative consequences for both the mother and the fetus. Severe bleeding after childbirth, osteoporosis, hyperbilirubinemia in a child and other pathologies of the hepatobiliary system cannot be excluded.
How to identify jaundice: characteristic symptoms
Signs of jaundice in an adult are determined by the form and stage of the underlying disease. More than 93% of possible pathologies are accompanied by characteristic yellowness of the skin. Malfunctions in the functioning of the bile, liver and bile ducts are indicated by the following symptoms:
- elevated temperature;
- skin itching;
- loose stools;
- discolored stool;
- bitterness in the mouth;
- yellow skin color;
- pain in the right hypochondrium;
- yellowed eyes;
- lack of appetite;
- dark urine;
- yellowness of the mucous membranes (especially noticeable on the tongue).
Jaundice syndrome is not a specific manifestation of a particular disease. To recognize pathology in an adult, you need to determine the characteristic symptoms. For example, when the liver is damaged (hepatic jaundice), the skin becomes yellow with a red tint, but if the color is greenish, this indicates a malfunction of the bile ducts.
A person with Gospel disease appears tired, lethargic, or irritable. Due to an increase in bilirubin levels, nerve endings in the skin are irritated. Therefore, adults complain of itching, which intensifies in the evening hours. With obstructive jaundice caused by obstruction (narrowing) of the bile ducts, there are complaints of spastic pain in the side. Sometimes they worsen after heavy physical work, eating or drinking.
Causes of pathology
There are a huge number of reasons why jaundice develops in an adult. The pathological process develops with neoplasms in the liver, which are benign and malignant. The causes of jaundice are the appearance of parasitic microorganisms in the liver. If a patient has abnormalities in the structure of the biliary tract, this can lead to the onset of the disease.
Among the causes of jaundice are viral hepatitis of an infectious nature. The disease appears against the background of hepatitis, which has a different etiology. It develops against the background of cirrhotic changes in the liver, which is caused by the effects of alcohol and other toxic substances on the body. The cause of jaundice is Gilburne syndrome. Often the pathological process develops with infectious monoculosis.
Often the cause of jaundice is liver cancer. It is diagnosed in a patient with autoimmune diseases that damage the liver tissue. The disease can develop with monoculosis of an infectious nature. It is observed against the background of leptospirosis. Pathology can manifest itself as a postoperative complication.
What jaundice is and why it appears can only be determined by a doctor. That is why, when the first signs of the disease appear, you need to contact a specialist.
Basic principles of treatment
Since jaundice is a syndrome that accompanies various diseases, it should be treated symptomatically, focusing on treating the underlying disease.
Etiotropic therapy. If the cause of jaundice is known, then etiotropic treatment is carried out: treatment of viral hepatitis, removal of stones, tumor resection, withdrawal of hepatotoxic drugs, deworming, surgical, endoscopic restoration of bile drainage (balloon dilatation of strictures, endoprosthetics, biliodigestive anastomoses).
Diet. Limiting the consumption of neutral fats (up to 40 g per day for steatorrhea), medium-chain triglycerides (up to 40 g per day).
Enzyme preparations. Creon is prescribed, which is the gold standard among this group of drugs.
Fat-soluble vitamins.
- Vitamins are prescribed internally: K - 10 mg/day, A - 25 thousand IU/day, D - 400–4000 IU/day.
- Vitamins are administered intramuscularly: K - 10 mg per month, A - 100 thousand IU 3 times a month, D - 100 thousand IU per month.
- For hypovitaminosis D, replacement therapy is prescribed at a dose of 50 thousand IU orally 3 times a week or 100 thousand IU intramuscularly once a month (higher doses can also be used). If serum vitamin D levels are not controlled, the parenteral route of administration is preferable to the oral route. For severe bone pain, slow intravenous administration of calcium is prescribed (calcium gluconate 15 mg/kg for several days), if necessary, in repeated courses. Vitamins are indicated for the prevention of hypovitaminosis and hepatic osteodystrophy in jaundice and prolonged cholestasis. It is necessary to take calcium supplements of 1.5 g per day and stay in scattered rays of sunlight for the synthesis of vitamin D.
- diet, or table No. 5, “liver table” with limitation of fatty, smoked and fried foods;
- drinking plenty of mineral waters for the purpose of detoxification;
- taking enterosorbents (SUMS, Polyphepan, Enteros-gel). They contribute to a general improvement in well-being;
- prescribe vitamin complexes that have pronounced detoxifying activity, for example, vitamin C, alpha-tocopherol, and others;
- in the absence of cholestasis, mild choleretic drugs (holosas, allochol) can be used.
Medication
It involves the use of adsorbents, antiviral, anti-inflammatory and antibacterial drugs. Hepatoprotectors can be used.
Vitamin K is prescribed to restore blood clotting. If skin itching occurs, then topical topical preparations are used.
Vitamin complexes containing amino acids and B vitamins promote recovery. Glucocorticoids are used in the presence of oncological changes.
Diet therapy
To reduce the level of bilirubin in the blood, a diet is recommended in complex therapy. Limited, fractional meals are recommended with the exception of aggressive and heavy foods.
Mandatory for overweight patients. It consists of eliminating fatty foods from the diet.
It is necessary to completely eliminate the consumption of alcoholic beverages.
Phototherapy
It is used to treat parenchymal jaundice in newborns. For phototherapy, special incubators with ultraviolet lamps are used. Such lamps have a wavelength of 400 - 550 nm. The duration of the course is about 90 hours.
Continuous irradiation is indicated for children whose bilirubin levels significantly exceed the permissible norm. In order to avoid adverse reactions, regular monitoring of the child’s body temperature and blood biochemistry is carried out.
With jaundice, it is important for newborns to eat their mother's breast milk. Its regular use helps to significantly reduce the level of bilirubin in the child’s blood.
If continuous phototherapy is indicated, then mother's milk is expressed and the baby is fed with a bottle or pipette.
Traditional methods
All patients with jaundice should be hospitalized because they may be contagious. Perhaps the exception is Gilbert's disease, but the patient knows about his disease and does not worry, since the bilirubin level will decrease on its own. In all other cases, the following principles of therapy should apply to the patient:
You should know that usually the liver itself copes well with the hepatocellular type of jaundice. To do this, she only needs a little help. The most important rule is to completely spare her work. This especially applies to those people who, due to the development of jaundice, cannot refuse to continue drinking alcohol or intravenous drugs.
In such patients, hepatocellular jaundice often occurs latently, since the body’s immune status is unable to cause “bright” inflammation, for example, in the fight against the hepatitis virus, or a sufficient immune response. Therefore, it is precisely these “sluggish” forms of viral hepatitis that can lead to the appearance of hepatocellular carcinoma, or liver cancer.
Provoking factors
The described disease can occur as a result of eating foods or water that contain pathogenic microorganisms. In addition, blood and sexual transmission are possible.
To avoid contracting viral hepatitis, it is recommended to minimize contact with people who:
- Are already infected or are carriers of a viral infection;
- Have had sexual contact with infected persons;
- Are planning a trip to or have returned from a country where there are outbreaks of disease;
- Abuse alcoholic beverages or use drugs.
The direct etiological factor, which theoretically becomes a trigger for the development of jaundice, can be:
- Obstruction of the bile ducts and bile ducts;
- The presence of congenital anomalies in the structure;
- Liver diseases (various types of hepatitis or cirrhosis);
- Premature destruction of red blood cells;
- The presence of neoplasms in the liver;
- Penetration of pathogenic microorganisms into the body;
- Complications after surgery;
- Use of certain groups of drugs.
Diagnostic methods
Before prescribing an adequate course of therapeutic measures, the doctor conducts a whole range of diagnostic examinations to determine the causes of the malfunction.
For this purpose, laboratory and instrumental examination methods are used.
Carrying out a general and biochemical blood test allows us to detect the presence of an inflammatory process in the patient’s body; in addition, an increased concentration of bilirubin in the blood is detected, and a decrease in the resistance of erythrocytes is also determined.
Urine analysis makes it possible to determine the increased content of urolibin in it, which is a characteristic sign of the development of a malfunction in the patient’s body.
The presence of a hemolytic form of the disease is indicated by an increased content of stercobilin in the stool.
An abdominal ultrasound is performed to detect changes in the size and structure of the liver and spleen. The use of ultrasound examination allows us to identify changes in the structure of the parenchymal tissue of the liver.
If necessary, the doctor may prescribe additional examination using CT and MRI.
Hepatic or parenchymal jaundice
We have already examined the mechanisms of occurrence and clinical manifestations of types of jaundice, and now we will continue to consider liver-type diseases. It develops due to significant damage to organ cells. As a result, their structure is disrupted and they cannot perform their functions. Naturally, one of them is the processing of bilirubin. Because of this, the whole system goes astray.
This type of jaundice indicates serious liver disease. When conducting differential diagnosis, the doctor must necessarily exclude the possibility of infection of other patients.
Why does this type of jaundice occur? The reasons may lie in infectious mononucleosis, cirrhosis, or cancer. The disease can also manifest itself due to alcohol, drug or toxic liver damage. Many people know that there is another factor that can cause this type of jaundice. What type of hepatitis can cause the disease? This, of course, is chronic aggressive hepatitis or acute viral.
Forecasts and warning methods
Prevention of parenchymal jaundice consists of preventing damage from viral hepatitis and intoxication with all kinds of chemicals. A person should be careful about personal hygiene and visit only proven salons for manicure procedures. You should always consult a doctor before purchasing and taking weight loss medications and other medications on your own. The prognosis for jaundice is positive, but with fibrosis and sclerosis that accompany severe stages of the disease, prognostic criteria worsen.
Forecast
The prognosis of jaundice detected at the beginning of development can be considered favorable if the main cause can be eliminated by conservative or surgical methods.
Its reappearance is possible with cholelithiasis, so correction of metabolism and compliance with diet and other doctor’s instructions is necessary.
Surgery should not be performed at the peak of icteric syndrome, but resection (excision) of difficult-to-reach tumors or cysts will be almost as harmful as no treatment. The best tactics are considered to be reducing the volume of the tumor before surgery or applying bypass anastomoses.
Prehepatic jaundice and its features
Modern medicine knows several basic mechanisms for the development of such a disorder as jaundice. Symptoms in adults are mostly the same, but the reasons may be different. As you know, bilirubin is released during the destruction of red blood cells. Increased hemolysis of red blood cells leads to an increase in the amount of yellow pigment - it simply does not have time to be metabolized in the liver.
A similar picture, for example, is observed with sickle cell anemia and malaria. Causes include autoimmune diseases, as well as some genetic disorders, including spherocytosis. Sometimes this form of the disease develops due to drug use.
Symptoms
Differential diagnosis of jaundice is based on a combination of certain signs and laboratory results. It is convenient to compare them using a table:
| Sign | Suprahepatic | Hepatic | Subhepatic |
| Color of the skin | Lemon yellow | Yellow-orange | Yellow-gray or greenish |
| Itching | No | Sometimes | Constantly |
| Urine | Normal color | Dark | Dark |
| Feces | Normal color or dark | Discolored | Discolored |
| Liver | Rarely enlarged | From reduced to increased | increased |
| Heaviness in the right hypochondrium | No | At the beginning of the disease | Rarely |
| Pain on the right | No | Not always | Available for cancer and stones |
| Spleen | Increased | Increased | Fine |
| Symptom intensity | Weak | Moderate | From weak to strong |
Instrumental studies are necessary for obstructive jaundice. They establish the location of the obstacle and its origin. Only after this is an individual treatment plan for the patient drawn up.
Kinds
Jaundice is a collective syndrome, the manifestations of which are characteristic of a number of diseases of the hepatobiliary system. It includes changes in the color of the skin, mucous membranes, urine and feces. Bile acids, which irritate the nerve endings, provoke severe itching, which is why scratch marks can be seen on the patient’s skin. This is true for all types of jaundice except hemolytic.
Based on the etiological factor, the following types of disease are distinguished:
- Mechanical.
- Parenchymatous.
- Hemolytic.
- Physiological.
- Conjugation.
- Congenital.
Mechanical type of jaundice
This variety is a pathogenic process that appears due to mechanical obstruction of the biliary tract. As a result, bile outflow or total blockage of the lumen is disrupted. Due to impaired outflow, stretching of the blood vessels of the microvasculature occurs, compression of the liver cells, as well as an increase in the amount of unbound and bound bilirubin in the blood in the tests.
Often, with this disease, it is possible to detect bilirubin molecules in the urine. With a partial reduction or complete disappearance of pathological components in the tests, they indicate a complete cure, which is achieved by clearing the lumen of the vessel. The mechanical type of jaundice is the most common because it affects both adults and children equally. In addition to the symptoms listed above, it is characterized by headaches, gastrointestinal upset, skin problems, general fatigue and drowsiness.
Characteristics of hemolytic jaundice
The pathogenesis of this type of pathology is based on the synthesis of large amounts of bilirubin. The liver is unable to process and remove bilirubin from the body into the external environment. Diagnosis of such a disorder most often occurs in childhood as a result of a conflict with the mother’s immunity. In this case, the process of destruction of the child’s red blood cells is observed.
Very often, this type of pathology appears as a result of hereditary anemia, toxic poisoning or long-term progression of the inflammatory process. When hemolytic jaundice occurs, the patient's nervous system is damaged. The result of such damage is irritability and headaches.
The etiology of the disease is associated with increased breakdown of hemoglobin in the spleen, for this reason this type of jaundice is called adrenal.
The most common causes of the hemolytic form of the disorder are:
- transfusion of incompatible blood group;
- development of infarctions of large organs, such as the lungs and spleen;
- intoxication with hemolytic poisons - arsenic and phosphorus;
- malaria infection;
- liptospirosis;
- the presence of congenital and acquired defects of erythrocytes - sickle cell anemia, enzymatic deficiency and microspherocytosis.
The symptoms characteristic of this type of disease develop very quickly. The main manifestation of the disease is yellowing of the skin and its acquisition of a lemon-yellow hue. In addition, the patient has an enlarged spleen, while the liver enlarges slightly.
Parenchymal jaundice
The mechanism of the pathological process in the hepatocyte can be different, depending on which there are 3 types of hepatic jaundice: hepatocellular, cholestatic and enzymopathic. Hepatic jaundice occurs with infectious and non-infectious damage to liver cells. The functional ability of cells to secrete bilirubin from the blood into the bile ducts decreases; they do not secrete bile into the bile ducts, and it begins to enter the blood through the lymphatic vessels. Most often, this process is typical for hepatitis of a viral and bacterial nature, during pregnancy with severe toxicosis, as well as for newborns for reasons of heredity.
The characteristic coloring of the skin may have a red or ruby tint. The study reveals an increased content of free and bound bilirubin in the blood. Bilirubin and bile acids appear in the urine. A characteristic feature of this type of jaundice is a change in all functional liver tests. Hepatic jaundice caused by viral hepatitis can be contagious and, depending on the type, transmitted through household, sexual contact or blood.
In addition to the main forms of jaundice listed above, the hepatic form can be divided into several more types. These include:
- Hepatocellular;
- Cholestatic;
- Enzymopathic.
The causes of hepatocellular jaundice can be various types of hepatitis, exacerbation of chronic hepatitis, alcoholic cirrhosis of the liver, exposure to toxic substances due to uncontrolled use of medications.
The main symptoms of hepatocellular jaundice are:
- Pronounced yellowing of the skin and mucous membranes;
- Complete absence of skin itching;
- The presence of spider veins in the upper part of the body and sharp redness of the skin of the palms;
- Enlarged liver;
- In laboratory tests, the blood serum will have a yellowish tint.
For specialists, making an accurate diagnosis of hepatocellular jaundice is difficult at the initial stage of the disease (especially in newborns).
If hepatocellular jaundice is caused by the presence of viral hepatitis in the patient’s body, then the symptoms will include chills, increased body temperature, fever, diarrheal disorders, pain on palpation of the liver;
In the case of cholestatic jaundice, the manifestation of the disease will be characterized by the following symptoms (depending on the neglect, more or less pronounced):
- Increased levels of direct and indirect bilirubin in the blood;
- Darkening of urine;
- Discoloration of stool.
The causes of cholestatic hepatic jaundice can be drug-induced liver damage, biliary cirrhosis, and hepatosis in pregnant women. The principle of cholestatic jaundice is a metabolic disorder in the components of bile.
In the case of enzymopathic jaundice, the patient at any stage of the disease will experience reduced activity of the necessary enzymes that are responsible for the fixation of bilirubin in liver cells.
Stages of development of the pathological condition and their main signs
Hepatic jaundice is a warning sign of functional problems with the liver. Such jaundice in its progression has three stages of development. Each stage of the disease differs from the others in its complex of characteristic signs and symptoms.
The first stage is called pre-icteric. At this stage, characteristic signs are a significant decrease in the activity of liver enzymes and damage to hepatocyte membranes.
At the same time, a decrease in the formation of free bilirubin is recorded. The external manifestations of this stage are a change in the color of urine, it becomes dark, as well as discoloration of feces.
The second stage is icteric. This stage of the disease is characterized by the development of hyperfermentation, which consists of increased production of bile acids and increased permeability of the cell membrane of hepatocytes and compression of the vascular system of the gland.
The second stage is externally manifested by the following signs:
- The appearance of skin itching on the body in the area where the organ is located.
- Formation of yellowness of the skin and mucous membranes.
- The appearance of discomfort and pain in the area of the right hypochondrium.
- Intoxication – attacks of nausea and vomiting occur, and body temperature rises.
- The appearance of a nodular rash on the skin.
- An increase in blood pressure.
- The appearance of pain in muscle structures and joints.
The third stage is the exodus. This stage is characterized by an intensification of the existing set of symptoms. The itching of the skin becomes unbearable, the skin acquires a greenish tint, and there is increased pain in the area where the liver is located. In the absence of qualified medical care, signs of the development of hepatic coma are observed, resulting in death.