When gastric bleeding occurs, symptoms may vary in severity depending on the underlying disease and its severity. This phenomenon is considered a serious complication of a number of diseases, requiring urgent measures. Large blood losses can be life-threatening, and therefore knowledge of first aid techniques will help to avoid tragic consequences. It is important to strictly observe prohibitions on the consumption of a number of foods, since it is poor nutrition that often provokes pathology.
Signs of intestinal bleeding and ways to help the patient
The leakage of blood from the upper and lower parts of the digestive system is called intestinal bleeding.
It occurs due to injuries, diseases of the abdominal organs and other pathological processes. The phenomenon is harmful to health and dangerous to human life. The symptom in question occurs due to the following diseases:
- Thinning of the walls of blood vessels.
- Crohn's disease.
- Diverticulosis.
- Tumors, adenocarcinoma.
- Acute intestinal inflammation.
- Ulcerative lesions of the stomach and duodenum.
- Polyps.
- Haemorrhoids.
Types of stomach bleeding
| Classification sign | Types of bleeding |
| Due to the occurrence | Ulcerative (most common) |
| Non-ulcerative | |
| According to the nature of bleeding | Acute |
| Chronic | |
| According to clinical manifestations | Explicit |
| Hidden | |
| By flow and duration | One-time |
| Recurrent |
Types of bleeding
The phenomenon is classified according to its localization and the nature of the flow.
- Intense (profuse) bleeding. They are characterized by the fact that biological fluid is released in large quantities. Blood loss is life-threatening.
- Weak. They have mild symptoms and lead to the development of anemia.
Sources of bleeding can be organs of the upper and lower gastrointestinal tract.
Provoking factors for bleeding are gastric ulcers, polyps, Meckel's diverticulum and inflammatory processes of the digestive system. In addition, they arise due to:
- Recurrence of ulcerative lesions.
- After an operation during which part of the stomach was removed.
- Benign tumors. These include lipoma, leiomyoma.
- Malignant neoplasms: adenocarcinoma, rectal cancer.
- Multiple polyps originating from the rectal mucosa.
Non-ulcer pathologies provoke bleeding from the intestines. These include:
- Inflammatory process in external and internal hemorrhoids.
- Cracks in a hollow organ.
- Intestinal diverticula.
Feces with blood are found in infectious lesions of the organ. Acute intestinal infections such as salmonellosis, typhoid fever, dysenteric enterocolitis are causes of blood loss.
The clinical picture of the disease depends on its nature and location. In this case, the following general signs of internal bleeding appear:
- Marked weakness.
- Frequent dizziness, tendency to faint.
- Blurred consciousness.
- Low blood pressure.
- Hyperhidrosis.
- Delirium.
- Visual and auditory hallucinations.
- Pale coloration of the skin.
- Perioral cyanosis (blue discoloration of the skin around the mouth).
- Dry mouth, feeling thirsty.
- Vomiting, with blood.
- Bloody feces, melena.
The presence of these signs requires urgent hospitalization. Delay can be fatal.
Blood from the intestines appears due to diseases of the stomach and duodenum.
Aortic aneurysm is a serious illness that causes bleeding. The disease is a consequence of portal hypertension, which occurs due to liver cirrhosis and acute heart failure. The walls of the blood vessel become thinner, which leads to its rupture and blood loss.
- High blood pressure.
- Heavy sweating.
- Cardiopalmus.
- Dizziness, loss of consciousness.
Gastroenterological pathologies are accompanied by the following symptoms:
- Heartburn.
- Belching with an unpleasant odor.
- Vomit.
- Aversion to food, poor appetite, weight loss.
- Unpleasant taste in the mouth.
- Pain in the abdominal area.
- Diarrhea.
- Dehydration.
Symptoms of stomach bleeding
The type of signs that occur in the presence of open blood flow in the stomach and the power of their manifestation are determined by the size of the open wound and the duration of the process.
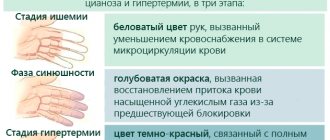
Common symptoms of stomach bleeding are associated with a decrease in blood supply to the organs. Nonspecific signs characteristic of internal hemorrhage into any cavity of the body:
- weakness, sluggish response to what is happening, up to fainting with massive bleeding;
- pale skin, cyanosis (blue discoloration) of fingers, nose, nasolabial triangle;
- excessive sweating – hyperhidrosis;
- dizziness, unsteady gait;
- flickering “flies”, tinnitus.
The pulse rate increases, filling and tension drop, and the tonometer records a decrease in pressure.
Vomiting with blood, as well as changes in stool, are the most characteristic external manifestations of the described traumatized state of the circulatory system of the gastrointestinal tract.
Vomiting is often with clotted blood - “coffee grounds”, as it is affected by hydrochloric acid of the stomach. The appearance of scarlet blood may indicate either bleeding from the esophagus or profuse (profuse) gastric bleeding.
Patients' stool becomes black or very dark in color - melena, due to coagulated and partially digested blood.
In addition to the listed symptoms, manifestations of a disease or condition that lead to blood loss are observed.
Features of the phenomenon
Blood coming out of the anus is the main symptom. The stool is dark in color. It should be remembered that this color is also caused by taking medications that contain iron, activated carbon, bismuth . Blueberries, black currants, and pomegranate also cause darkening of the color of stool.
Some diseases have specific symptoms that help identify the cause of bleeding.
Adenocarcinoma, colorectal cancer
The bleeding is slight. The patient develops anemia. Feces mix with blood and mucus. These signs indicate the presence of a tumor of the left parts of the large intestine.
Crohn's disease
Signs of colitis are observed. A complication occurs due to damage to a hollow organ.
Nonspecific ulcerative colitis
The patient complains of a constant urge to defecate. Feces contain impurities of mucus, blood, and pus.
The blood is scarlet. It comes out in a stream during bowel movements.
Rectal fissure
The stool is bright red in color. Severe pain occurs during and after defecation. A spasm of the anal sphincter occurs.
Causes
Provoking factors for bleeding are gastric ulcers, polyps, Meckel's diverticulum and inflammatory processes of the digestive system. In addition, they arise due to:
- Recurrence of ulcerative lesions.
- After an operation during which part of the stomach was removed.
- Benign tumors. These include lipoma, leiomyoma.
- Malignant neoplasms: adenocarcinoma, rectal cancer.
- Multiple polyps originating from the rectal mucosa.
Non-ulcer pathologies provoke bleeding from the intestines. These include:
- Inflammatory process in external and internal hemorrhoids.
- Cracks in a hollow organ.
- Intestinal diverticula.
Feces with blood are found in infectious lesions of the organ. Acute intestinal infections such as salmonellosis, typhoid fever, dysenteric enterocolitis are causes of blood loss.
Intestinal bleeding in a child
Blood loss from the lower parts of the digestive system can also occur in children under 3 years of age. This is how congenital pathology of newborns manifests itself. This phenomenon occurs in the presence of the following diseases:
- Volvulus, intestinal obstruction.
- Duplication of the small intestine.
- Ulcerative necrotizing enterocolitis.
Symptoms of the complication manifest themselves in the form of bloating, constant belching, regurgitation, vomiting and stool with mucus, which has a green tint and a watery consistency.
Main reasons
In recent years, despite the development of medicine, the frequency of gastric bleeding has not decreased. At the same time, the incidence of the main provoking factor, namely ulcerative lesions, has decreased somewhat, but other reasons related to the lifestyle and profession of patients, the presence of various background diseases and the need to regularly take certain groups of medications are beginning to play an increasingly important role.
Non-steroidal anti-inflammatory drugs have a negative effect on the gastrointestinal mucosa
All causes of gastric bleeding are very diverse and numerous, but they can be combined into the following groups:
How to diagnose a stomach ulcer
- the formation of ulcerative lesions of the mucous membrane and deeper layers of the stomach, caused by various factors (“aggression” of hydrochloric acid of gastric juice, rupture or thrombosis of blood vessels, exposure to acute or chronic stress, the influence of medications, especially non-steroidal anti-inflammatory drugs);
- malignant and benign neoplasms (stomach cancer with tumor disintegration, polyposis accompanied by trauma or ischemia of polyps);
- gastric diverticulosis, that is, the presence of “outgrowths” on the stomach wall into its lumen (bleeding is possible due to injury or inflammation of the diverticula);
- Mallory-Weiss syndrome, characterized by rupture of blood vessels in the mucous membrane of the upper part of the stomach and esophagus, which leads to severe bleeding. This phenomenon is provoked by a sharp increase in intra-abdominal pressure, for example, during vomiting, severe coughing, or with a blow to the stomach;
- diaphragmatic hernia, that is, protrusion of the upper stomach into the chest cavity through an incompetent diaphragm (damage to blood vessels and further bleeding occur as a result of the action of gastric juice on the lower part of the esophagus or the formation of ulcers);
- vascular pathologies (varicose veins, systemic vasculitis, hypertension, atherosclerosis);
- blood pathologies affecting, first of all, indicators of its coagulation (leukemia, hemophilia, thrombocytopenia, hemorrhagic diathesis).
It should be noted that vascular or blood pathologies often become consequences of many diseases. For example, varicose veins of the esophagus, which quite often lead to bleeding, can form due to liver pathologies (tumors, cirrhosis), thrombosis or compression of the portal vein. Often, hemorrhage begins with cardiovascular and endocrine diseases, sepsis, and chronic renal failure. Reduced blood clotting can be hereditary or acquired, which leads to bleeding in the stomach even in childhood.
A drop in blood pressure may indicate significant blood loss
First aid
Activities that help stop bleeding can be done at home.
Emergency aid algorithm:
- The patient is ensured the correct position of the body. He is placed on his back. The legs are raised at an angle of 15˚.
- They are not allowed to eat or drink.
- Ice is applied to the abdominal area. It causes vasoconstriction and reduces blood flow. The procedure takes 15 minutes. Take a 5-minute break. The manipulation is repeated.
- The patient is given a Dicinone tablet. It is pre-crushed.
Injections of Papaverine and Atropine are given in case of acute bleeding.
The windows in the room are opened for normal circulation of fresh air. It is forbidden to wash the intestines. Clears the airways of blood, vomit, and mucus. Ammonia is used if the patient loses consciousness.
First aid will help prevent unwanted, dangerous consequences.
Consequences and complications
The greater the volume of blood loss, the more dangerous the consequences. Acute bleeding can lead to hemorrhagic shock and rapid death. Loss of small volumes leads to the development of persistent anemia. If the cause of intraintestinal hemorrhage is not identified in time, the disease can progress to the stage when doctors are powerless.
Therefore, the first thing to do in case of gastrointestinal bleeding is to consult a doctor. Internal bleeding is dangerous because it is difficult to assess the extent of blood loss and the likelihood of certain complications.
Diagnostics
Blood in the stool and during vomiting helps in making a diagnosis. The diagnostic program includes such examination methods as:
- General, biochemical blood test.
- Urine examination.
- Coagulogram.
- Fibrogastroduodenoscopy.
- Sigmoidoscopy.
- Fecal occult blood test.
- Ultrasound examination of the abdominal cavity.
- Mesentericography, scintigraphy of mesenteric vessels.
- Radiography.
The choice of tactics depends on the cause of bleeding. Treatment is not carried out at home. A specialist knows how to stop intestinal bleeding and provide adequate therapy.
Hemostatic measures are carried out using instrumental methods. They include:
- Clipping.
- Ligation.
- Surgery.
Therapeutic measures are carried out using drugs such as:
- Aminocaproic acid.
- Hemostatic drugs Fibrinogen, Etamzilat.
- Reopoliglyukin.
- Erythrocyte mass.
- Frozen blood plasma.
- Calcium chloride.
- Vitamin K
- Medicines that restore the volume of intercellular fluid.
The choice of specific minimally invasive treatment depends on the clinical picture:
- Coagulation of damaged vessels using an endoscope is used for frequently recurring hemorrhages.
- Vessel ligation and sclerotherapy are used in cases of injury to varicose veins of the esophagus.
- A colonoscopic electrocoagulator is used for severe, prolonged bleeding from the lower segments of the digestive tube.
For moderate blood loss, the main goal of therapy is to eliminate the underlying cause.
Bleeding from the colon, which occurs against the background of complicated diverticular disease, is eliminated by infusion of Vasopressin. This is done using a catheter, which is not removed for 48 hours, since the complication recurs.
Necrosis of the intestinal wall, local or diffuse peritonitis requires emergency surgical assistance. This involves resection of the affected part of the intestine .
Hemorrhoidal damage to the organ is treated with sclerosis and bandaging.
If signs of bleeding do not stop or intensify, the patient undergoes an autopsy of the abdominal cavity. Surgery allows you to detect the source of bleeding. Subsequent treatment is carried out according to the examination.
Classification
There are several varieties of such a symptom or complication, ranging from the nature of its occurrence to possible sources. Thus, two types of gastrointestinal bleeding are distinguished:
- acute – divided into voluminous and small. In the first case, there is a sudden appearance of characteristic symptoms and a significant deterioration in the person’s condition, which can occur even after ten minutes. In the second situation, the symptoms of blood loss gradually increase;
- chronic – characterized by the manifestation of anemia, which is recurring in nature and continues for a considerable time.
In addition to the main forms, there are also obvious and hidden, single and recurrent hemorrhage.
According to the location of the source of blood loss, it is divided into:
- hemorrhage from the upper gastrointestinal tract - the appearance of the disorder occurs against the background of damage to the esophagus, stomach or duodenum;
- bleeding from the lower zones of the gastrointestinal tract, which includes organs such as the small and large intestines, as well as the rectum.
Severity of gastrointestinal tract infections
Classification of gastrointestinal bleeding according to the severity of its occurrence:
- mild degree - the person is conscious, blood pressure and pulse indicators deviate slightly from the norm, the blood begins to thicken, but its composition does not change;
- moderate degree - characterized by a more pronounced manifestation of symptoms, decreased blood pressure and increased heart rate, blood clotting is not impaired;
- severe – characterized by the patient’s serious condition, a significant decrease in blood pressure and an increase in heart rate;
- coma – observed with significant blood loss, which can reach three liters of blood.
Traditional medicine recipes
Folk remedies include the use of hemostatic herbs. Recipes:
- Viburnum common. Grind 4 teaspoons of plant bark and add 250 mg of water. Put the mixture on the fire and boil for half an hour. Infuse the decoction. It should be drunk 10 g three times a day, before meals.
- Yarrow. The plant is indicated for blood loss of any etiology. 2 teaspoons of dry plant are poured with boiling water. The infusion is taken 4 times a day.
- Burnet. The root of the plant is filled with water. The mixture is boiled over low heat for 30 minutes. Leave for 2 hours. A tablespoon of decoction is taken 5 times a day.
- Highlander. The plant is brewed with a glass of boiling water. The infusion is drunk 4 times a day before meals.
- Geranium. 20 g of the plant is added to 1 liter of water. Boil for 20 minutes.
- Cucumber stems. The plant is useful to take for bleeding from the intestines.
- Immortelle pink. A tablespoon of the plant is infused for 1 hour in 250 ml of boiling water. Drink 1 tbsp. spoon every 2 hours.
Signs of gastrointestinal tract
Emergency care for gastric bleeding should be provided immediately after the first symptoms are recognized. In addition to the specific symptoms that appear in different diseases, there are general manifestations.
The patient exhibits:
Thick, coffee-colored vomit begins.
- weakness, skin turns pale;
- there is a chill throughout the body, cold sweat appears;
- heart rate and blood pressure readings decrease;
- the patient becomes lethargic and may lose consciousness;
- with ulcerative disorders, thick, coffee-colored vomit begins;
- the color of the stool becomes intensely dark, blood appears in the stool.
As the intensity of the hemorrhage increases, the symptoms become more pronounced, so first aid for gastric bleeding must be provided quickly. The death of the patient can occur in a few minutes. To save the patient, timely diagnosis and treatment of bleeding is required.
Rehabilitation
Intestinal bleeding requires a fasting diet for 1 to 3 days. Nutrients, glucose and protein preparations are supplied to the body using a dropper.
Raw eggs, milk, and fruit jelly are introduced into the patient’s diet. By the end of the week, the patient eats boiled eggs, mashed porridge, meat soufflé, and jelly. All dishes must be cold.
Intestinal restoration requires a long time for healing of ulcers and scars. Proper nutrition is maintained for 6 months. Physical activity is prohibited.
Acute bleeding always poses a danger to human life, since a lot of time passes from the first manifestations to the adoption of urgent measures and surgical intervention.
An acute hemorrhagic attack ends in death in a third of cases. This happens due to large blood loss and untimely contact with specialists. Bleeding cannot always be stopped. In addition, there is a high risk of relapse.
Types of housing and communal services
Before treating hemorrhage, it is important to know the classification of gastrointestinal bleeding. Considering the part of the digestive system that serves as the source, bleeding is distinguished from the upper parts of the gastrointestinal tract (duodenal, esophageal, gastric), as well as from the lower parts (colon and small intestine, hemorrhoidal).
For gastrointestinal bleeding, the classification takes into account ulcerative and non-ulcerative nature. There are acute and chronic gastrointestinal tract diseases. Depending on its severity, the condition can be hidden or obvious. Regarding the number of episodes, a distinction is made between recurrent and single GIB.
Gastrointestinal bleeding of non-ulcer etiology occurs when:
- erosion of the gastric mucosa, hemorrhoids;
- anal fissures and bacterial colitis;
- diaphragmatic hernia, Mallory-Weiss syndrome;
- malignant, benign tumors of the gastrointestinal tract (sarcoma, cancer, lipoma and polyps);
- presence of parasites and infections.
Considering the severity of blood loss, there are 3 degrees of gastrointestinal tract disease. A mild degree is characterized by a heart rate of 80, systolic blood pressure of at least 110, satisfactory condition and consciousness, dizziness, and normal diuresis. Indicators of moderate acute gastrointestinal bleeding: heart rate - 100 beats per minute, systolic blood pressure - 100-110 millimeters Hg. Art., consciousness and pallor of the skin, cold sweat remain, and diuresis decreases. If such signs occur, it is necessary to call emergency doctors.
Severe gastrointestinal bleeding is manifested as follows: heart rate - more than 100 beats, systolic blood pressure - less than 100, adynamia and lethargy, anuria or oliguria. The composition of the blood changes significantly.
Stomach and intestinal bleeding - symptoms and first aid
When stomach bleeding occurs, the signs are quite easy to recognize. The main thing in this situation is to make adequate decisions and competently provide first aid, since with heavy blood loss every minute is valuable.
In this case, you should not wait idly for the doctors to arrive: you must try to stop or at least reduce the intensity of blood loss. Even if the bleeding in the stomach is not severe, you should also provide the person with minimal assistance and consult a doctor.
This condition occurs quite often, especially in patients with chronic diseases of the stomach and intestines. According to medical statistics, 8-9% of patients in surgical departments who are admitted by ambulance have this diagnosis.
More than half of the cases occur due to internal bleeding of the stomach, with the duodenum in second place. Approximately 10% are due to bleeding from the rectum. In the midgut, blood loss rarely occurs.
Treatment
Acute hemorrhage or exacerbation of chronic hemorrhage can occur anywhere at the most unexpected moment, which is why it is necessary to know the rules of emergency assistance to the victim. First aid for gastrointestinal bleeding includes:
- providing a person with a horizontal position so that the lower limbs are higher than the rest of the body;
- applying a cold compress to the area of the suspected source. This procedure should last no more than twenty minutes, after which they take a short break and apply cold again;
- taking medications by mouth only if absolutely necessary;
- exclusion of food and liquid intake;
- a complete ban on gastric lavage and cleansing enema.
Treatment of gastrointestinal bleeding in a medical facility consists of:
- intravenous injections of blood replacement drugs - to normalize blood volumes;
- transfusion of donor blood - in cases of massive hemorrhages;
- administration of hemostatic medications.
In cases of ineffectiveness of drug therapy, endoscopic surgical interventions may be necessary, which are aimed at:
- ligation and sclerosis of damaged vessels;
- electrocoagulation;
- puncture of bleeding vessels.
Often they resort to open surgery to stop hemorrhages.
How and why does gastrointestinal bleeding occur?
There are three main mechanisms for the development of this condition:
- Damage to a blood vessel in the lining of the stomach or intestines. The main causes are mechanical or chemical damage, inflammation, peptic ulcer, excessive stretching of the stomach walls.
- Reduced blood clotting.
- Leakage of blood through the walls of blood vessels.
There are more than two hundred reasons that can cause stomach bleeding . And although most cases are associated with the presence of pathologies of the upper digestive tract, other diseases can also lead to this condition.
- Directly peptic ulcer of the esophagus, stomach or duodenum, caused by the bacterium Helicobacter pylori or arising as a complication of gastritis or duodenitis.
- Ulcer due to chronic stress.
- Destruction of the mucous membrane as a result of taking certain medications (hormones, non-steroidal anti-inflammatory drugs, salicylates, etc.)
- Erosive gastritis.
- Triggered by disturbances in the functioning of the endocrine system.
- Tumors (benign and malignant).
- Varicose veins in the stomach and intestines, which often occur in conjunction with liver diseases.
- Anal fissures.
- Haemorrhoids.
- Diverticulitis.
- Diseases of the liver and gall bladder.
Systemic lupus erythematosus.
Hypertension is an acute state of crisis.
Tuberculosis or syphilitic damage to the stomach, burns, ischemia of the gastric mucosa can also lead to the development of such a pathology - but these cases are rare.
An increased tendency and greater risk exists in people who abuse alcohol: due to changes in the vessels of the digestive organs.
Risk factors also include:
- Vitamin deficiencies, especially vitamin K deficiency, can cause mild bleeding.
- State of shock.
- Blood poisoning.
- Old age and the presence of a large number of chronic diseases.
- Esophageal hernia.
- Traumatic brain injury.
- Low blood pressure in combination with tachycardia.
Typically, gastric and intestinal bleeding occurs in the presence of several factors from the list given in the table.
Etiology of the phenomenon
Most often, the causes of gastric bleeding are associated with the development of peptic ulcers in the organ itself or the duodenum. They are recorded in almost every fifth sick person with this pathology. In this case, direct damage to the blood vessels by gastric juice occurs or complications develop in the form of the formation of a blood clot, leading to rupture of the vessel.
The problem under consideration can also be caused by reasons not related to peptic ulcer:
- erosion of the gastric mucosa;
- ulcers provoked by injuries, burns, surgery (so-called stress ulcers);
- ulcers caused by a long course of treatment using potent drugs;
- Mallory-Weiss syndrome, i.e. damage to the mucous membrane due to intense vomiting;
- ulcerative colitis;
- tumor formations, polyps;
- Gastric diverticulum, caused by a protrusion of the stomach wall;
- diaphragmatic hernia associated with protrusion of part of the stomach into the abdominal cavity.
Causes due to disruption of the structure of blood vessels are also recorded:
- the formation of atherosclerotic plaques in the vascular walls;
- vascular aneurysms;
- venous expansion in portal hypertension due to liver dysfunction;
- connective tissue diseases: rheumatism, lupus erythematosus;
- systemic vasculitis: periarteritis nodosa, Henoch-Schönlein purpura.
Sometimes the cause of bleeding is a bleeding disorder. The main pathologies of this type include thrombocytopenia and hemophilia. In addition, blood loss can be caused by mechanical trauma when a solid body enters the stomach, as well as infectious lesions - salmonellosis, dysentery, etc.
Types of internal bleeding of the digestive system
Intragastric bleeding can occur once and not bother a person anymore, or it can recur from time to time. In the second case, we can talk about a recurrent condition. In this case, the patient needs a thorough examination , which will help identify the whole range of reasons that each time lead to blood loss.
Acute disease develops suddenly and rapidly, leading to the loss of large volumes of blood and a sharp deterioration in general condition. The person requires emergency medical attention because there is a risk of losing a large amount of blood. Signs include vomiting red blood, confusion, low blood pressure (high reading below 100) and loss of consciousness.
Chronic can last for several days or even weeks. The patient often goes unnoticed, but iron deficiency anemia develops over time. You should not hope that this condition will go away on its own over time: examination and medical care are necessary to stabilize the condition.
Depending on the volume of blood loss, it can be:
- Light - practically does not manifest itself. A person may notice a small amount of blood in their stool or vomit. Usually small vessels are affected and blood loss is negligible.
- Moderate mild dizziness and slight decrease in blood pressure.
- Severe, in which a person may lose consciousness and not respond to the environment.
A patient with intestinal bleeding should be provided with rest and consultation with a doctor. The more severe the condition, the faster medical help is needed. If you feel satisfactory, you still need to see a therapist or gastroenterologist.
Types of pathology
Depending on the etiological mechanism, there are 2 main types of gastric bleeding: ulcerative (occurring from a stomach ulcer) and non-ulcerative. According to the nature of the pathology, acute and chronic forms are distinguished. In the first case, internal bleeding develops very quickly with intense blood loss, which requires urgent medical measures. The chronic clinic is characterized by a long course with small constant leaks of blood into the gastric lumen.
Taking into account the severity of the phenomenon, 2 types are distinguished: obvious and hidden bleeding. In the first option, all signs of gastric bleeding are intense and easily detected. A latent course is characteristic of a chronic process, while the definition of the disease is hampered by the absence of pronounced symptoms, and the presence of pathology, as a rule, is indicated only by indirect signs, in particular the pallor of a person. According to the severity of the manifestation, the following degrees are distinguished: mild, moderate and severe.
The clinical picture of intestinal bleeding also depends on the location of the source of hemorrhage. The following main options are distinguished:
- Bleeding in the upper part of the gastrointestinal tract: esophageal, gastric, duodenal.
- Bleeding in the lower parts: small, large and rectal.
Symptoms of bleeding in the stomach and intestines
The patient may not notice any signs if the lesion is not large-scale.
In later stages and with serious illnesses, the following may occur:
- Dizziness.
- Pallor.
- Chills, clammy sweat.
- Weakness, fatigue.
- The dark color of the stool is almost black. The blood in the intestines has time to be partially digested, so it turns black. If the vessels of the rectum are damaged, feces do not mix with blood.
- Nausea.
- Vomiting - scarlet blood with large and rapid blood loss or with damage to the esophagus. When vomiting is slow but voluminous, it resembles coffee grounds - the blood coagulates under the influence of gastric juice.
- Decreased heart rate.
- Ringing in the ears, darkening of the eyes.
Pain does not necessarily accompany this condition. Perforation of an ulcer is usually accompanied by acute sensations. If bleeding occurs when an ulcer damages a vessel or it bleeds periodically without breaking through the stomach wall, the pain, on the contrary, subsides.
Symptomatic manifestations
There are several groups of signs of bleeding in the stomach. With any internal bleeding in the human body, general symptoms develop:
- pale skin;
- general weakness and apathy;
- cold sweating;
- arterial hypotension;
- the appearance of a rapid but weakened pulse;
- dizziness;
- noise in ears;
- confusion and lethargy.
With intense blood loss, a person may lose consciousness.
Pathognomonic signs of the phenomenon under consideration include vomiting and defecation with blood. Bleeding can be determined by the characteristic appearance of the vomit: it resembles “coffee grounds.” In this case, blood is released that was affected by acid in the stomach. At the same time, in case of bleeding from the esophagus or severe damage to the gastric arteries, scarlet, unchanged blood may be released in the vomit. Blood impurities in the stool give it the appearance of a tarry substance.
The severity of a sick person’s condition with gastric bleeding is assessed according to 3 degrees:
- A mild degree is determined when the patient’s general condition is satisfactory. Slight dizziness is possible, pulse is up to 76–80 beats per minute, pressure is not lower than 112 mm Hg.
- The average degree is established in the presence of pronounced pallor of the skin with cold sweating. The pulse may increase to 95–98 beats, and the pressure may drop to 98–100 mmHg.
- Severe severity requires emergency assistance. It is characterized by such a sign as obvious inhibition. The pulse exceeds 102 beats, and the pressure drops below 98 mm Hg.
If treatment is not carried out or carried out incorrectly, the pathology progresses quickly.
Why is there bleeding from the stomach?
Bleeding in the intestines, stomach or other digestive organs can develop for the following reasons:
- mechanical damage to the stomach due to foreign body entry;
- abdominal injuries;
- burn of the gastrointestinal mucosa;
- inflammation of the mucous membrane and reflux disease of the esophagus;
- erosive gastritis;
- peptic ulcer of the stomach and duodenum;
- nonspecific ulcerative and bacterial inflammation of the large intestine;
- Crohn's disease;
- endocrine and enzymatic disorders (dysfunction of the parathyroid glands, gastrinoma);
- long-term use of NSAIDs (especially salicylic acid compounds), glucocorticoids, Butadione and other drugs, violations of the rules for using medications;
- complications of operations on the gastrointestinal tract;
- damage to the mucous membrane at the junction of the esophagus and stomach with frequent and intense vomiting (Mallory-Weiss syndrome);
- benign and malignant neoplasia of the digestive tract;
- protrusion of the walls of the gastrointestinal tract (diverticulosis);
- tuberculosis and other chronic inflammatory bowel diseases;
- intestinal infections of bacterial and parasitic origin (dysentery, helminthiasis, etc.);
- volvulus;
- damage to hemorrhoids and intestinal polyps during the passage of feces;
- anal fissure;
- aortointestinal fistula;
- Hirschsprung's disease and other pathologies leading to acute fecal obstruction;
- thrombosis of the portal and hepatic veins;
- compression of the portal vein or large vessels associated with it by neoplasms or large scars;
- severe liver pathologies (cirrhotic lesions, chronic hepatitis);
- varicose veins of the esophageal and gastric veins;
- atherosclerosis of gastrointestinal vessels;
- diseases of autoimmune and inflammatory origin that affect blood vessels (systemic lupus erythematosus, scleroderma, hemorrhagic vasculitis, periarteritis nodosa, etc.);
- congenital vascular anomalies (Rendu-Osler-Weber disease);
- atherosclerosis and aneurysms of the arteries of the digestive tract;
- blockage of blood vessels in the intestinal mesentery;
- congenital (hemophilia) and acquired disorders of the blood coagulation system (acute deficiency of vitamins C and K, hypoprothrombinemia, etc.);
- hemorrhagic diathesis (thrombocytopenic purpura, radiation thrombocytopenia, chronic and acute leukemia);
- DIC syndrome;
- aplastic anemia and other pathologies of the hematopoietic system;
- cardiovascular diseases (inflammation of the valve system of the heart and cardiac sac, insufficiency of cardiac function, arterial hypertension, etc.).
Etiology
Currently, there is a wide range of predisposing factors that cause the occurrence of such a serious complication.
Bleeding that occurs against the background of damage to the gastrointestinal tract is often caused by the following ailments:
- ulcer of the duodenum or stomach;
- malignant or benign tumors;
- diaphragmatic hernia;
- chronic form of esophagitis;
- GERD;
- ulcerative colitis;
- pathological influence of helminths, parasites and other pathogenic bacteria;
- hemorrhoids;
- formation of cracks in the anal area;
- Crohn's disease;
- Mallory-Weiss syndrome.
Mallory-Weiss syndrome
Hemorrhages of the digestive tract associated with a violation of the integrity of blood vessels are often caused by:
- varicose veins of the gastrointestinal tract, in particular the stomach or esophagus;
- systemic lupus erythematosus;
- atherosclerosis;
- the formation of plaques of atherosclerotic nature;
- scleroderma;
- aneurysm or dilation of the vessel, which is accompanied by thinning of its wall;
- periarteritis nodosa;
- rheumatism;
- diverticula of the gastrointestinal tract;
- septic endocarditis.
Often, hemorrhages in the gastrointestinal tract are the result of blood diseases, for example:
- leukemia of any form;
- lack of platelets, which are responsible for blood clotting;
- hemophilia - is a genetic pathology, against the background of which there is a violation of the blood clotting process;
- hemorrhagic diathesis and other ailments.
Bleeding in the gastrointestinal tract due to portal hypertension often occurs when:
- chronic hepatitis;
- liver damage by cirrhosis;
- compression of the portal vein by tumors or scars;
- the formation of a blood clot in the veins of the liver.
In addition, it is worth highlighting other causes of gastrointestinal bleeding:
- a wide range of injuries and injuries of the abdominal organs;
- penetration of a foreign object into the gastrointestinal tract;
- uncontrolled use of certain groups of medications, for example, glucocorticoid hormones or non-steroidal anti-inflammatory drugs;
- the influence of stress or nervous strain over a long period of time;
- traumatic brain injuries;
- surgical intervention on the organs of the digestive system;
- housing and communal services;
- arterial hypertension.
Gastrointestinal bleeding in children is caused by the following factors:
- hemorrhagic disease of newborns is the most common cause of such a disorder in infants under one year of age;
- volvulus - often causes gastrointestinal hemorrhages in children from one to three years old;
- colon polyposis – explains the appearance of this symptom in preschool children.
Children of the older age group are characterized by similar etiological factors inherent in adults.
Intestinal bleeding
Bleeding in the intestines is caused by the release of blood from the digestive tract. This disease occurs due to pathological processes in the gastrointestinal tract or mechanical damage. If such a symptom is not paid attention to, there will be a serious danger to human life.
Since internal bleeding occurs due to damage to a vessel or capillary, the intensity will depend on its diameter.
This disease is divided into 2 types:
Hidden bleeding is the bleeding that occurs when the capillary walls are damaged. Most often they occur due to a decrease in hemoglobin in the blood, which is why anemia develops.
Overt bleeding is a sudden pathology that provokes a sudden loss of a large amount of blood. A patient with this diagnosis needs urgent medical attention.
Intestinal bleeding is caused by ulcerative lesions of the gastrointestinal tract, this category includes:
- secondary ulcers after surgery to remove a fragment of the stomach;
- ulcerative colitis of nonspecific type;
- accumulation of a large number of ulcers in the cavity of the large and small intestines.
Sometimes this phenomenon occurs due to the formation of polyps in the colon. Blood is released as a result of damage to formations by feces.
In addition, the disease is provoked by other abnormalities:
- chronic hemorrhoids;
- oncological diseases;
- damage to the veins of the esophagus, resulting in bleeding;
- tuberculosis;
- diaphragmatic hernia.
Bleeding also occurs due to poisoning with heavy metals or any chemical components. Blood is released due to a burn of the mucous membrane.
In rare cases, psychogenic injuries lead to such a phenomenon. The appearance of bleeding from the intestines is sometimes preceded by blows to the abdominal area.
The following symptoms of intestinal bleeding are distinguished:
- general weakness;
- strong feeling of thirst;
- short-term loss of consciousness;
- dizziness;
- a sharp decrease in blood pressure;
- excessive sweating;
- increased heart rate;
- labored breathing;
- convulsive attacks causing vomiting;
- Sometimes when bleeding from the intestine there is tarry stool.
Diagnosing the disease with heavy bleeding is not difficult. In some patients, this condition causes a neurological disorder, fear or sudden euphoria.
Patients also experience a decrease in hemoglobin levels in the blood. Moreover, this indicator does not appear immediately, but only 2–3 days after bleeding. During this period, it is necessary to carefully monitor changes in blood pressure. It is important in this matter to establish the cause of pathological changes.
Ulcerative lesions of the gastrointestinal tract are characterized by the following symptoms:
- pain occurs periodically;
- there is a decreased body temperature;
- discharge of blood with feces is the main sign of a latent ulcer.
With stomach cancer, vomiting with blood may occur. In this case, the patient quickly loses body weight.
Other gastroenterological abnormalities also cause symptoms:
- heartburn, belching, bad breath;
- nausea, vomiting;
- pain in the area of localization of inflammation;
- loss of appetite;
- diarrhea with particles of undigested food;
- watery stools;
- dehydration of the body.
If there is heavy bleeding from the rectum, then the veins in the intestinal tract may have dilated. This condition is caused by cracks that appear due to constant constipation or the presence of a foreign object in the intestine. In some cases, the disease occurred in people after radiation damage to the body.
If there are liver pathologies, then the disease occurs along with a change in the color of the skin. Most often, the patient's face acquires a jaundiced tint, and discomfort also occurs in the area of the right hypochondrium.
Sometimes the cause of such disorders is sexually transmitted diseases, and in particular syphilis.
With such a pathology, the following symptoms are observed:
- intestinal obstruction;
- gas formation;
- periodic constipation and diarrhea;
- during the process of defecation, unpleasant sensations arise;
- dysfunction of the genitourinary system.
If assistance is not provided to the patient in a timely manner, severe consequences for the patient’s health cannot be avoided. Heavy bleeding sometimes causes the death of the patient.
Symptoms
Depending on the rate of blood loss, bleeding is usually divided into obvious and hidden; the latter can only be determined during a stool test for occult blood. Obvious acute ones are manifested by bloody vomiting and melena, and hidden hemorrhages cause manifestations of anemia. Early signs of intestinal hemorrhage include weakness, dizziness, fainting, and palpitations, which are associated with anemia.
If the hemorrhage is severe, bloody vomiting (due to the stomach being full of blood) or melena (black, semi-liquid stool with an unpleasant odor, which is formed from blood and intestinal contents) may occur. With minor blood loss, there will be no bloody vomiting, since the blood has time to be evacuated from the stomach into the intestinal tract.
Blood appears in the vomit if the bleeding ulcer is located in the duodenum and duodenal contents are refluxed into the stomach. Repeated vomiting and melena occurs with massive bleeding. If vomiting is frequent, then this indicates ongoing bleeding in the high parts of the gastrointestinal tract, and if the intervals between urges are long, then most likely the bleeding resumes.
If the bleeding is not massive or chronic, then melena and vomiting can occur only a few days after the start of bleeding from the mucosal wall. Intestinal bleeding is often manifested not by vomiting, but by the presence of blood in the stool. It can also be determined during a digital rectal examination, and the redder the blood, the closer to the anus the location of the damage.
If the blood loss is more than 100 ml, then, against the background of accelerated passage of feces, the stool will contain dark liquid blood, and if the intestinal contents have been moving for more than 6 hours, then tarry stools (melena) appear. The strength of the outpouring can be determined by the consistency of the stool. When the small intestine is affected, the stool is liquid, black, and foul-smelling.
If bleeding occurs above the rectosigmoid colon, the blood has time to mix with the feces. If blood is released unchanged and not mixed with feces, hemorrhoidal bleeding or damage to the perianal area is suspected.
The most common cause of intestinal bleeding is intestinal diverticulosis.
Often, before acute bleeding, patients report increased pain in the epigastric region, and as soon as the ulcer begins to bleed, the pain becomes less intense or disappears altogether. This is because the blood dilutes the hydrochloric acid contained in the stomach. During gastrointestinal bleeding, the skin becomes pale, cyanotic, cold, and moist. The pulse is increased, and blood pressure (blood pressure) is normal or low.
Intestinal bleeding is rarely acute; in most cases, patients only report the appearance of blood in the stool. If a lot of blood is poured out, it irritates the intestinal walls and leads to an acceleration of the passage of feces through the digestive tube. Hence the loose, black, foul-smelling stool.
Acute blood loss (more than 0.5 liters of blood) leads to the following symptoms:
How to take a stool occult blood test?
- weaknesses;
- dizziness;
- noise and ringing in the ears;
- tachycardia;
- shortness of breath;
- darkening of the eyes;
- heartache;
- pallor;
- heavy sweating;
- drowsiness;
- limbs become cold;
- confusion;
- weak pulse;
- low blood pressure.
Young patients more often have bleeding from duodenal ulcers, and in patients over 40 years of age, the pathology is more often localized in the stomach.
Signs of chronic hemorrhage:
- pallor of the skin and mucous membranes;
- glossitis, stomatitis;
- decreased performance;
- dizziness;
- anemia;
- There is rarely tarry stool.
Inflammatory bowel pathologies cause pain in the lower abdomen, diarrhea, tenesmus (painful false urge to defecate). The blood is usually mixed with the stool because the source is superior to the rectosigmoid region. Inflammation of the colon, which is caused by a bacterial infection, can also cause bloody diarrhea, but blood loss is not significant.
Typhoid fever, for example, is manifested by intestinal bleeding, fever, increasing intoxication, rashes that turn pale when pressed, and cough. The diagnosis is confirmed by sigmoidoscopy with biopsy and stool analysis. With ischemia of the colon, colicky pain appears in the abdomen, often on the left side. Bloody diarrhea occurs throughout the day.
Blood loss is usually minimal, but can be massive. The diagnosis is established after X-ray examination and colonoscopy with biopsy. If hemorrhage occurs against the background of long-term low-grade fever, weight loss, chronic diarrhea and symptoms of intoxication, then intestinal tuberculosis can be assumed. If the effusion of blood into the intestines is combined with systemic lesions of the skin, joints, eyes and other organs, then there is a high probability of nonspecific colitis.
Diagnostics
The following diagnostic measures are carried out:
- general and biochemical blood test;
- Analysis of urine;
- stool examination;
- Ultrasound of the abdominal organs.
With a complicated course of the disease, there is a need for urgent surgical intervention. Before the procedure, fluoroscopy is performed. Using this method, you can determine the type of operation. It is worth noting that ulcerative lesions rarely occur in people under 20 years of age.
After diagnosis, further treatment methods include the use of the following methods:
- conservative therapy;
- surgical intervention.
Identification of the source of bleeding involves gastrofibroscopy. Such a study is more accurate; with the help of a special probe, the doctor has the opportunity to examine the condition of the organs from the inside. However, this procedure is carried out after complete gastric lavage or before meals.
When identifying the source of bleeding, symptoms are important. If there is vomiting with blood, then the cause is a pathology of the stomach, but when there is stool mixed with blood, there are obvious disturbances in the functioning of the intestines.
Diagnosis and treatment of gastrointestinal bleeding
The most informative diagnostic method for gastrointestinal bleeding is endoscopic gastro- and colonoscopy . During these procedures, doctors can detect the source of bleeding and immediately carry out therapeutic procedures, for example, cauterizing the damaged vessel. For chronic bleeding from the stomach or intestines, patients are shown contrast radiography, angiography and computed tomography of the digestive tract.
Special immunochemical tests are used to detect occult blood in stool. In European countries and the United States, all older people are recommended to undergo such tests annually . This makes it possible to identify not only chronic bleeding, but also to suspect tumors of the gastrointestinal tract, which can begin to bleed even when small in size (before intestinal obstruction appears).
To assess the severity of bleeding, patients must undergo a general blood test, biochemical study and coagulogram. If the blood loss is serious, there will be changes in all these tests.
Treatment tactics for patients with gastrointestinal bleeding are determined by the location and causes of this syndrome. In most cases, doctors manage to manage with conservative methods, but surgical intervention is not excluded. Operations are carried out plannedly, if the patient’s condition allows, and urgently, when it is impossible to delay.
General recommendations for patients with gastrointestinal bleeding with moderate blood loss are as follows:
- Bed rest.
- Hunger until the bleeding stops, and then a strict diet that is as gentle as possible on the digestive tract.
- Injections and oral administration of hemostatic drugs.
After stopping the bleeding, the patient is treated for the underlying disease and anemia, which almost always develops after blood loss. Iron supplements are prescribed by injection, and subsequently - orally in the form of tablets.
In case of massive blood loss, patients are hospitalized in the intensive care unit. Here doctors have to solve several problems: stop bleeding and eliminate its consequences - infuse blood substitutes and red blood cells to restore the volume of blood circulating in the body, administer protein solutions, etc.
Features of providing assistance to children
The main feature of gastrointestinal tract in children and adolescents is the specific etiology of gastrointestinal bleeding, which is usually caused by pathologies in the development of organs - ulcerative processes are diagnosed only in every tenth child. Also, a common cause of gastric bleeding between the ages of 3 and 10 years is a clinical complication of portal hypertension.
A sick child with suspected gastrointestinal bleeding must urgently call a medical team, reporting by telephone about the possible presence of gastrointestinal bleeding.
The basis of emergency care for gastrointestinal bleeding in children before the arrival of medical specialists is ice and rest, monitoring vital signs and a ban on drinking water with food. In emergency cases and pronounced symptoms of gastrointestinal tract, it is necessary to administer calcium gluconate (10 percent solution) and 2 cubes of Vikasol intravenously to the child. As a supplement, take 2 tablets of Dicynone in dry form without drinking water, and also make an intravenous drip based on aminocaproic acid (or a similar systemic hemostatic agent, if possible) in a chilled form.
Diet
The patient should follow an individually selected diet so that the hemorrhage does not recur and help the body recover from stress and blood loss. For the first 9 days after surgery, the patient should follow the following nutrition plan:
- Day 1: absolute hunger. Prohibition on the consumption of food and liquids.
- Day 2: You are allowed to take half a glass of liquid per day. Liquid intake should be taken with a teaspoon.
- Day 3: let’s take 500 ml of broth/water/tea.
- Day 4: allow 4 glasses of liquid per day. Soups, jelly and yogurt are allowed.
- Day 5: unlimited fluid intake. It is acceptable to make liquid soup, cottage cheese, semolina porridge for the patient.
- Days 6-7: boiled meat is introduced into the diet.
- Days 8-9: transition to proper nutrition.
During the recovery period and to avoid recurrence of bleeding, you will need to follow a diet
Basic rules for further diet:
- Maintain temperature control at every meal. It is forbidden to eat excessively hot or cold food; it should be at room temperature.
- Drink plenty of fluids.
- Fractional meals. Meals should be small and repeated every 2-3 hours (as required). During the day, the patient should consume from 4 to 6 servings.
- Use vitamin complexes and biological supplements to speed up the recovery of the body.
- Avoid drinking sugary drinks and foods with lots of sugar. You can make juices or baked goods with a sugar substitute (stevia) at home.
- Avoid eating fatty, carbohydrate, smoked, and pickled foods.
- Limit the consumption of alcoholic beverages and tobacco products.
Where is the outbreak located?
The length of the large intestine in adults is approximately 150 cm. Bleeding can appear in different parts of the absorption organ. The mesenteric arteries provide high-quality blood supply. Blood is drained through mesenteric veins. Varicose veins lead to slow and prolonged bleeding in the cavity of the large intestine.
The lower the source of blood leakage is located, the more of it will be in the stool. Resinous pigmentation of decay products indicates the presence of bleeding in the upper parts of the organ. Pain usually occurs with injuries. To establish the source of injury, a targeted diagnostic study is required.
Symptoms of internal bleeding
How to recognize internal bleeding?
With low blood loss, there is often a slight increase in heart rate and a slight decrease in blood pressure. However, such internal bleeding may sometimes not be accompanied by any symptoms at all.
With moderate internal bleeding, systolic pressure drops to 80-90 mmHg. Art., the pulse quickens to 90-100 beats per minute. The skin becomes pale, the extremities become cold, and increased breathing may occur. Also in such a situation, dry mouth, fainting and dizziness, adynamia, nausea, slow reaction, and weakness are possible.
In severe cases, systolic pressure drops to 80 mmHg. Art. and even lower, the pulse increases to 110 beats per minute and above. Sticky cold sweat appears on the body, there is a strong increase in breathing, yawning, nausea and vomiting, apathy, hand tremors, increased drowsiness, painful thirst, a decrease in the amount of urine excreted, severe pallor of the skin and mucous membranes.
With massive internal bleeding, systolic pressure drops to 60 mmHg. Art., the pulse rate can reach 140-160 beats per minute. Characteristic features of massive internal bleeding are periodic breathing (Cheyne-Stokes breathing), delirium, confusion or lack thereof, cold sweat, severe pale skin. The gaze becomes indifferent, the facial features become sharpened, the eyes become sunken.
With fatal blood loss, systolic pressure decreases to 60 mmHg. Art. or is not determined at all. Coma develops, breathing becomes agonal, severe bradycardia, convulsions, dilated pupils, and involuntary release of feces and urine are observed. The skin becomes dry and cold, acquiring a characteristic “marble” shade.
Signs of internal bleeding also depend on which cavity the blood is bleeding into. For example, nausea and vomiting of dark blood may indicate bleeding into the cavity of the stomach or esophagus; coughing with bright pulmonary blood is an unambiguous sign of pulmonary hemorrhage.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Treatment of internal bleeding is carried out in a hospital; the choice of department depends on the source of internal blood loss: it can be the department of general surgery, gynecology, neurosurgery, and so on.
In this case, specialists solve three problems:
- stopping internal bleeding;
- compensation for blood loss;
- improvement of microcirculation.
In some cases, in order to stop the bleeding, it is enough to cauterize the bleeding area, but most often surgical intervention under anesthesia is necessary. The specific actions of the surgeon, again, depend on the type of internal bleeding.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Acute bleeding
If intestinal bleeding is observed, help should be provided very quickly. Otherwise, complications are likely. A prolonged phenomenon can lead to human death.
For minor chronic bleeding, special care is not needed. In this case, the underlying disease is treated. Typically, sclerotherapy with laser or liquid nitrogen is used. Electrical thermocoagulation is also used.
Severe massive blood loss requires blood transfusion, plasma and intravenous administration of large amounts of fluid. This is done after the cause has been eliminated. Usually, an emergency surgery is required, in which a ligature suture is placed on the painful vessels and mucosal tissue.
Therapy and patient care
Treatment of the patient depends on a list of factors (primarily on signs of psychological health and physical indicators). If the patient’s condition is not critical, before starting treatment, a comprehensive diagnosis is carried out, which helps determine the general condition of the patient’s body, subsequent therapy, possible complications and consequences. If there is no time for preparatory actions, the only effective treatment method is surgery.
Conservative treatment
Conservative treatment of the disease consists of drug therapy.
Conservative treatment consists of drug therapy without resorting to surgery. Treatment consists of bed rest, which will help reduce blood loss. The victim should be provided with complete emotional and physical rest (muscle contractions can increase blood flow). The abdominal cavity is fixed, a cold object is applied to it, which slows down the outflow of blood and promotes vasoconstriction.
After carrying out the required diagnostic measures, gastric lavage is performed (blood in the stomach, food debris, dead tissue must be removed from the organ). The procedure is carried out with cold water through the mouth or nasal passage using a special tube. After lavage, a probe is inserted into the stomach, through which a medicinal substance is introduced into the body - adrenaline, norepinephrine. The medication causes muscle contraction, constriction of blood vessels and helps stop bleeding. It is possible to administer intravenously medications that promote rapid blood clotting.
Surgical intervention
Surgical intervention is used in the following cases:
- it is impossible to stop blood loss;
- serious condition of the patient, risk of death;
- severe decrease in blood pressure;
- disruption of normal blood flow in the body;
- constant resumption of blood loss.
An operation to stitch up an open area where blood loss has begun.
Surgical interventions can be divided into several types:
- suturing the open area where blood loss has begun;
- removal of a section of the stomach that has begun to bleed;
- puncture of the groin area, which is performed remotely under ultrasound guidance. After the puncture, the bleeding vessel is blocked.
One of the most important preparatory actions before surgery is to notify the patient's close relatives. After the operation, specialized rehabilitation of the victim will be required, compliance with strict rules of nutrition and physical development, of which relatives and the patient himself must be notified in advance.
Postoperative therapy
Postoperative therapy of the patient depends on the psycho-emotional state, the nature of the operation, its success, and other things. The time frame for rehabilitation depends on the individual characteristics of the patient’s body and the impact of external factors. Basic rehabilitation scheme:
- on the first day after surgery, the patient is allowed to make slight forward movements of the limbs;
- introduction of breathing exercises from the second day;
- removal of sutures on the eighth day, provided the patient’s condition is normal;
- discharge from the medical center on the fourteenth day after surgery;
- performing physical therapy;
- a ban on vigorous physical activity for 30 days or more after discharge from the hospital;
- timely contact your doctor if signs of the disease appear.
About the intestines
This is an important human organ. The intestine is a digestive and excretory organ. It is located in the abdominal space and consists of 2 segments:
- Thin. It is supplied with blood from the superior mesenteric artery and the celiac trunk.
- Tolstoy - from the superior and inferior mesenteric arteries.
The intestines begin with the stomach and end with the anus. This organ is in constant activity, its length is approximately 4 meters. The intestines grow with the body. Its main functions include the following:
- Ensuring that hydrochloric acid enters the stomach to process food.
- Participation in the digestive process, breaking down foods into components and taking the necessary microelements and water.
- Formation and excretion of feces.
- Impact on the hormonal and immune systems.
Various diseases appear in the intestines. Bleeding from it is common. The causes, symptoms and treatment methods are described below.
What are the signs and symptoms
Early symptoms of bleeding in the gastrointestinal tract include:
- general weakness, adynamia;
- dizziness, fainting, confusion and loss of consciousness;
- ringing in the ears, flickering spots in the eyes;
- nausea, vomiting;
- change in color of gastric and intestinal secretions (vomit and feces);
- sweating;
- strong thirst;
- increased heart rate;
- pallor of the skin, cyanosis of the lips, blue discoloration and decreased temperature of the fingertips.
The severity of the symptoms of the pathology depends on the intensity of bleeding, the volume of blood volume and the amount of blood lost. Due to the larger initial volume of circulating blood, signs of bleeding in adults may manifest later and less clearly than in children. Even minor blood loss in a small child may require immediate resuscitation.
Symptoms of internal bleeding in the stomach often appear simultaneously with signs of massive blood loss and a decrease in circulating blood volume. Against the background of manifestations of blood loss, pain may be observed in the affected part of the gastrointestinal tract, an increase in the volume of the abdomen due to the accumulation of fluid (ascites), fever caused by intoxication, loss of body weight, a sharp change or loss of taste and other pathological phenomena indicating the cause of the gastrointestinal tract.
The main symptom of gastric bleeding is bloody vomiting, the nature of which may indicate the cause of the pathology and the duration of the bleeding.
| The cause of bleeding is in the stomach, esophagus or duodenum | Color and consistency of vomit |
| Varicose veins and erosions of the esophagus, profuse bleeding due to rupture of the mucosa | Scarlet blood in vomit |
| Ulcers of the duodenum and stomach, volvulus, cancerous neoplasia of the upper tract, rupture of the gastric mucosa | "Coffee grounds" (dark vomit with a grainy texture) |
“Coffee grounds” are a product of treating blood from the stomach with hydrochloric acid.
With ulcerative lesions, stomach pain is reduced during vomiting. Bleeding is not accompanied by irritation of the peritoneum and tension of the muscles of the anterior abdominal wall. With massive blood loss and stomach cancer, the color of the stool also changes.
Repeated vomiting with blood 1-2 hours after the first episode indicates continued bleeding, and vomiting after 4-6 hours indicates its relapse.
With gastric bleeding, the symptoms of blood loss in most cases are more pronounced than with bleeding in the intestines. This is due to the fact that common causes of damage to the walls of the small, large and rectal intestines are injuries to hemorrhoids, polyposis and small cracks in the mucosa. They can provoke prolonged but insignificant blood loss, which is accompanied by a slight decrease in hemoglobin concentration and the development of compensatory tachycardia while maintaining normal blood pressure and the patient’s well-being.
Symptoms of intestinal bleeding, accompanied by massive blood loss, may include:
- black feces;
- discharge of melena (unformed, tarry stool with a strong unpleasant odor);
- weakness, loss of consciousness, pale skin and other manifestations of acute blood loss.
Visual changes in the color and structure of stool are visible only with blood loss of more than 100 ml/day and damage to the rectum and colon (cracks, polyps, bleeding hemorrhoids). In case of a one-time leakage of blood (with a stomach ulcer and pathologies of the lower parts of the digestive tract), the blood is excreted unchanged in the stool. With prolonged massive bleeding, a few hours after it starts, tarry stools (dark stool with small clots) are released.
| Disease | Type and consistency of discharge | Bleeding pattern |
| Anal fissures, hemorrhoids | Stool with scarlet streaks of blood | Chronic blood loss that occurs during and after defecation and during physical activity. |
| Nonspecific ulcerative colitis, Crohn's disease | Watery mucous discharge with purulent and bloody impurities | Most often, mild bleeding occurs over a long period of time, but massive blood loss also occurs. |
| Oncological diseases of the intestine | Dark stool mixed with mucus | The discharge is long-lasting and low-intensity. Blood mixes with the stool, turning it dark. |
In the chronic course of the pathology, symptoms of anemia may occur:
- weakness, fatigue;
- decreased performance;
- frequent dizziness;
- inflammation of the mouth and tongue;
- pallor of the mucous membranes and skin.
How to treat
For gastrointestinal bleeding, treatment is aimed at stopping it, eliminating the root cause of the pathology, restoring hemostasis of the body and normal blood volume.
The danger for the patient is not only the loss of red blood cells that carry oxygen, but also a sharp decrease in blood volume, which leads to massive thrombosis of small vessels and the development of disseminated intravascular coagulation syndrome.
Conservative treatment of gastric bleeding and intestinal blood loss is carried out as an adjunct to surgery. As the main method of therapy, it is used for the following indications:
- hemorrhagic syndromes;
- cardiovascular diseases;
- inoperable malignant tumors;
- congenital pathologies of the hematopoietic system.
Therapy may include hemostatic agents, cytostatics, anti-inflammatory and other drugs.
If a large volume of blood is lost, the patient is prescribed IVs with saline solutions and transfusions of blood components.
Surgery
If bleeding in the gastrointestinal tract is suspected, the patient is taken to the surgical department of the clinic, where diagnosis and treatment tactics are determined.
Depending on the diagnosis, the patient may undergo the following operations:
- endoscopic sclerosis, electrocoagulation and ligation of dilated vessels of the intestine, esophagus, etc.;
- suturing of the ulcer and partial resection of the stomach;
- suturing duodenal ulcer;
- subtotal resection of the large intestine with stoma.
Treatment tactics using diet therapy depend on the underlying disease. For pathologies of the stomach, the patient is prescribed table No. 1, No. 1a (immediately after stopping the bleeding), No. 1b or No. 2. For intestinal diseases, diet No. 3 or No. 4 is recommended.
If bleeding is a complication of liver pathology, the patient is prescribed table No. 5 and its variations.
Diagnostic manipulations
Diagnosis of gastrointestinal bleeding is usually not difficult. Doctors begin examining the patient by studying the clinical history, medical history, examine the patient, palpate the epigastric area and abdominal space. Other diagnostic methods are:
- laboratory tests: blood, urine, feces to determine blood impurities;
- celiacography to determine the condition of the celiac trunk of the aorta and its branches;
- irrigoscopy to assess the condition of the intestines;
- vascular angiography to determine the state of blood flow;
- MRI of the abdominal cavity.
Endoscopic examinations play a great role in the diagnosis of blood loss in the digestive system. Carrying out colonoscopy simultaneously with gastroscopy increases the accuracy of the diagnosis and makes it possible to stop the bleeding site when its volume is insignificant.
What causes blood loss?
Severe bleeding (over 300 ml of blood) leads to:
- a decrease in blood volume without changing the diameter of blood vessels;
- elimination of blood pressure on the walls of blood vessels - the speed of blood circulation decreases;
- a decrease in the speed of blood flow in the center of the body - slow movement of blood in capillaries and small vessels;
- slowing down blood flow in the microvasculature, which causes stagnation;
- gluing of red blood cells in the microvasculature;
- complicating the exchange between clogged glued cells, capillaries and tissues;
- disruption of microcirculation in the liver, so it will not neutralize toxins from the blood.
Consequently, blood loss, especially large ones, leads to negative consequences. Therefore, it is better to prevent it, and for this you need to take the necessary measures in a timely manner.
Specific signs
If the integrity of the gastrointestinal tract is violated, a specific symptom is the appearance of blood in the stool and a change in its color. It can be present in feces or mixed with them. The shade depends on the location of the microtrauma:
- if the upper sections are damaged, it becomes almost black.
- with changes in the large intestine and rectum, a person notices blood in the form of drops on toilet paper or red streaks in the discharge.
Changes in stool color are associated with hemoglobin oxidation. They can be caused by dietary habits and certain medications. Bleeding due to pathological changes in the gastrointestinal tract is complemented by other unpleasant signs: 1. With inflammation of the mucous membrane (colitis, Crohn's disease), abdominal pain and prolonged diarrhea with mucus and pus appear. 2. During intestinal infections, high fever and muscle pain are added to the main symptoms. 3. With intestinal tuberculosis, in addition to periodic hemorrhages, rapid weight loss, severe weakness and frequent diarrhea are observed. 4. Malignant neoplasms are manifested by severe pain, loss of appetite, and the gradual development of anemia.
The intensity of bleeding affects the time it takes for symptoms to develop. For minor injuries, it may take several weeks or months before a person notices a change in their condition. Severe injuries cause rapid changes in condition: the victim turns pale, loses consciousness, and the heart rate slows down.
Is it possible to cope with stomach bleeding at home?
Any bleeding is life-threatening. It requires medical attention. Even mild but prolonged bleeding leads to serious consequences in the form of anemia. Along with medication prescribed by a doctor, you can help yourself with folk remedies.
Herbs - pepper knotweed, viburnum bark, horsetail, pink immortelle - will help prevent and stop mild stomach bleeding. They not only have a hemostatic effect, but also affect the cause of bleeding.
Prevention
Prevention of gastrointestinal bleeding includes timely diagnosis and treatment of pathologies of the digestive system. If an ulcer or other disease is detected, they undergo a full course of treatment. This prevents complications. The patient must monitor their lifestyle - stick to a diet, eliminate alcohol and reduce the amount of nicotine consumed.
The prognosis of gastric bleeding depends on the severity of the pathology and the speed of treatment. Chronic low-intensity hemorrhages have a favorable outcome. And in the case of profuse release of blood into the stomach cavity, one should wait for the outcome of the surgical intervention. Acute massive blood loss has a high mortality rate.
What is needed for normal bowel function?
Monitoring the functioning of this organ allows you to prevent bleeding. For its normal operation, the following rules must be observed:
- Diet is important. Do not overload your body with heavy foods. This especially applies to overeating throughout the day and contamination with harmful products - cookies, chips and candies. You need to have breakfast. The calorie content of this meal should be 25-30% of the daily value. It is advisable to eat whole grains and protein foods, which provide satiety and strength for a long time. And for snacks you need fruit and protein products. This could be dried fruits, nuts, yogurt, fresh fruits.
- You need to add foods that are valuable for digestion to your diet. To maintain intestinal activity, you need whole grain foods - cereals, muesli, legumes, nuts, fresh vegetables and fruits. The last 2 products are especially important for digestion and cleansing, as they contain fiber. This component helps prevent constipation, intestinal dysbiosis and excess weight.
- It is necessary to drink enough water. You need to drink at least 2 liters per day. Water ensures the swelling of fiber fibers, which increases the volume of masses in the intestines and enhances peristalsis. It is useful to drink water in the morning. This habit helps the organ start working.
- It is necessary to increase physical activity. To maintain the normal position of internal organs, including the intestines, the work of the abdominal muscles is required. If your lifestyle is sedentary, then the muscles of the anterior abdominal wall are weak, which aggravates the work of the gallbladder and intestines. Therefore, in the morning you need to do simple exercises.
- It is useful to take vitamins and herbal complexes. These are great helpers during the cold season. They are accepted as a course. If you have difficulty bowel movements, it is advisable to choose herbal preparations with dietary fiber.
Thus, bleeding in the intestines is considered dangerous. If it occurs, you should consult a doctor as soon as possible to get help.
Urgent Care
If symptoms of gastrointestinal tract appear, you should immediately call an ambulance. Since it will take about 15 minutes for a doctor to arrive, you should provide emergency assistance to the patient yourself to prevent complications. The algorithm is as follows:
- Place the patient on a bed or couch with the legs elevated above the body level, which ensures blood flow to the head and prevents repeated fainting.
- Provide access to fresh air for normal oxygen supply to tissues and organs.
- Place a cloth or gauze soaked in cold water on your forehead.
- Apply a heating pad with ice or a regular plastic bottle with cold water to the stomach in the area where the intestines and stomach are projected. This will help slightly reduce bleeding and reduce blood loss.
- Do not give the patient any medications, food or water, so as not to aggravate the situation. It is only allowed to give a few ice cubes for the patient to swallow. Children should not be given ice; a heating pad or bottle is sufficient.
After providing first aid, you must wait for specialists to arrive. It is important not to leave the patient alone. This can provoke panic, which will increase bleeding and worsen symptoms.
Treatment Options
To relieve symptoms, the patient is prescribed medications from different groups. In addition, quite often surgical intervention is required when seeking help was late. Additionally, the patient can stop bleeding using endoscopic methods, which involve instant coagulation of blood vessels (“adhesion” of small ones into larger ones).
Medicines: table of essential ones
If blood loss is insignificant and there are no complications, the specialist decides to carry out conservative treatment to stop the bleeding and promote the healing of erosions and ulcers.
| Drugs | Action |
| Agents to stop bleeding: aminocaproic acid, Dicinone, Etamzilate, Tranexam | They help increase the number of platelets and blood clotting factors to form a clot in the area of damaged vessels. Thanks to this effect, you can stop or significantly reduce the amount of blood, improve the patient’s condition |
| Preparations for eliminating toxins and purifying the blood: Reosorbilact, Reamberin | Help cleanse the body, prevent complications, fill the vascular bed, helping to maintain stable blood pressure levels |
| Proton pump inhibitors: Contrikal, Omez, Nolpaza | Reduces the acidity of gastric juice, eliminating the cause, which most often becomes a predisposing factor to the development of gastrointestinal tract |
| Medicines to replenish missing blood volume: sodium chloride, glucose 5% | Always used, they play the role of means to prevent dehydration of the body |
If necessary, medications to normalize blood pressure and painkillers are added to the course of treatment. In each specific case, the doctor draws up an individual scheme.
Operation
Significant bleeding with the release of not dark, but scarlet blood is almost impossible to stop with medications, so the patient is immediately sent to the operating table. The operation is performed urgently in case of a critical decrease in pressure and the impossibility of increasing it with drugs, in patients with repeated gastrointestinal tract bleeding, in the development of complications associated with significant blood loss.
For pain relief, general anesthesia is used, the surgeon opens the abdominal cavity and removes the part of the stomach in which the ulcer and damaged vessels are located. This allows you to quickly fix the problem. Sometimes suturing is required not only of the stomach, but also of part of the intestine. The operation is dangerous, takes a long time, and is followed by a long recovery period.
After resection, the wounds are sutured, and special drains are removed from four places in the abdominal cavity to drain serous fluid. A double probe is also inserted into the patient's nostril, the end of which is in the stomach. From one part of the tube, accumulated blood is removed from the stomach, and nutrition is introduced into the other.
Others
Sometimes severe bleeding can be stopped using endoscopic methods. The most effective will be the following:
- The thermal method involves the use of an endoscope (a special tube for examining the stomach). It is introduced into the organ cavity and the vessels are soldered using electric current. The bleeding stops and the rehabilitation period is reduced.
- The injection method also involves the use of an endoscope, after the introduction of which the doctor injects the site of the ulcer and damaged vessels with hemostatic drugs.
- Vessel ligation allows you to quickly stop gastrointestinal bleeding through the use of a laparoscope and endoscope. The method is considered a mini-operation, when several incisions are made in the abdominal cavity to insert laparoscopic instruments, an endoscope is inserted through the nose or oral cavity, and the damaged area is sutured.
The use of any of the methods is indicated for minor blood loss and the absence of complications.