≡ November 2, 2019 Category: Types and forms
Suppuration is the cumulative result of the activity of infectious agents and cells of the immune system aimed at their elimination. Purulent otitis is always difficult. Despite the approximate similarity of symptoms, variants of purulent otitis within one local area (middle, internal or external) can differ significantly from each other depending on the pathogen that caused the inflammation.
If we talk about the localization of purulent otitis media, then the tympanic region of the middle ear is the leader in this regard. The greatest danger is the purulent lesion of labyrinthitis. Finally, purulent inflammation localized in the external auditory canal is the simplest type of otitis that does not require serious medical care.
Causes of the disease
In most cases, purulent otitis media is a complication. Consequently, the main cause of the disease is ignorance or improper treatment of inflammation, usually of the middle ear.
However, there are other causes of suppuration. The disease develops when an infection gets into one of the ear cavities against a background of weakened immunity and decreased body resistance. The main representatives of pathogenic microflora that provoke the development of purulent otitis are pneumococci, Haemophilus influenzae and Staphylococcus aureus.
Suppurative external otitis media, the mildest form, can develop when germs from contaminated water or unwashed hands enter the ear. In this case, the inflammation is localized in the outer ear, which facilitates the course of the disease and its treatment.
Suppurative otitis media, the most common form, is usually the result of infection with mucus from the nasopharynx. Bacteria can also enter the middle ear through the eardrum or mastoid process (if they are perforated). Some diseases, such as measles, typhus and influenza, can provoke purulent otitis media: the infection in this case enters the cavity with contaminated blood.
Untimely treatment of otitis media leads to internal purulent otitis: pathogenic microorganisms penetrate into this area from the middle ear.
If the ears fester on both sides, a diagnosis of “bilateral purulent otitis media” is made; This is not uncommon - it is one-sided in 1 out of 10 cases.
Causes and symptoms of the disease
Purulent otitis is an otolaryngological disease of an infectious nature, in which the epithelium of the inner and middle ear becomes inflamed. Then purulent, unpleasant discharge from the auricle appears. The causes are pathogens that have entered the ear and reduced immunity.
The main routes of infection into the ear cavity during purulent otitis media.
- Tubogenic - through the auditory tube.
- Traumatic - through a damaged eardrum.
- Retrograde - from the cranial cavity: with sinusitis and rhinitis.
- Hematogenous - with blood flow: due to such serious diseases as scarlet fever, tuberculosis, measles.
Symptoms of the disease are severe ear pain, which can be throbbing or aching, congestion and noise in the ears, and pus comes from the ear, and the discharge smells unpleasant. Decreased hearing, increased temperature, dizziness, nausea, vomiting, and headache are also possible.
With purulent otitis, the mucous membranes of all parts of the middle ear are affected: the auditory tube, the eardrum, the mastoid process.
Symptoms
From the name of the disease it becomes clear that inflammation of the ear - otitis media - is accompanied by suppuration. However, there are several other signs that will prompt the doctor to diagnose “purulent otitis media”:
- Intense ear pain
- Hearing loss
- Redness, swelling in the ear area
- Heat
- Headache
- Weakness
Unfortunately, most people prefer self-medication to qualified therapy and consult a doctor in the later stages of the disease. This is dangerous due to complications that can cause irreparable harm to health. The first symptoms of purulent otitis require an immediate visit to an otolaryngologist.
It is difficult not to pay attention to the signs of purulent otitis media in adults. Young patients are unable to complain of hearing loss and a feeling of congestion. Parents should be wary if a child refuses to eat, rubs his ears and cries for no reason, and the thermometer indicates an elevated temperature. Do not wait until pus flows from your ear; consult a doctor as soon as possible.
Symptoms
It is difficult to confuse purulent otitis in a child with another pathology, since its symptoms are obvious.
The main manifestations of the disease are:
- ear pain;
- hearing loss;
- fever;
- purulent discharge from the ear.
Babies cannot explain that their ears hurt or they cannot hear anything. The baby becomes irritable, restless, does not sleep, and often cries for no apparent reason. There is a way for parents to check their suspicions about otitis media. The outer ear has a cartilaginous projection (tragus). When a baby has purulent otitis media, pressing on this cartilage will lead to a significant increase in pain and, accordingly, to screaming or crying.
Development of the disease
There are four stages of development of purulent otitis media:
- Catarrhal stage. At this stage, suppuration has not yet begun, but ear pain and fever indicate an inflammatory process. If left untreated, the condition worsens - the disease becomes purulent.
- Preperforative stage. The pain in the ears increases, pus appears in the eardrum and puts pressure on the membrane, hence the feeling of stuffiness, pain and hearing loss. Most patients at this stage seek help from a specialist.
- Perforated stage. Perforation is a rupture of the eardrum, which occurs due to the pressure of purulent masses. This stage is characterized by suppuration: at first the substance is liquid and light in color, later the discharge becomes thicker and denser until it stops altogether.
- Post-perforation, or recovery, stage. The patient no longer complains of pus from the ear, as well as pain, fever and weakness. The damaged eardrum heals, and hearing gradually returns to normal.
It is extremely important to visit an otolaryngologist at the first stage of the disease, since with the appearance of pus, perforation of the eardrum cannot be avoided. If it does not break through on its own, the surgeon intervenes to empty the cavity of pus. Otherwise, current purulent masses can enter the brain and provoke meningitis, encephalitis and hydrocephalus.
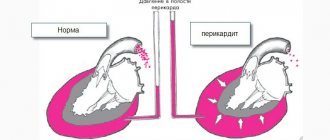
How does the middle part of the ear work?
The middle ear is located in the middle of the human hearing organ, on the right and left sides. The main part is the tympanic cavity. This is the name given to a small, air-filled space that is located at the base of the pyramid of the temporal bone between the inner and outer parts of the hearing organ.
The walls of the tympanic cavity are covered with mucous membrane. They also have membrane-covered openings leading to different parts of the hearing organ. The most famous of them is the eardrum, which separates the eardrum from the auditory canal of the outer ear (through which sound waves captured by the auricles penetrate into the ear).
The auditory ossicles are located inside the tympanic cavity. These are the hammer, incus and stirrup. They transmit the signal received from the ear drum to the inside of the ear. There it is transformed into an electrical impulse, which travels along the auditory nerve to the parts of the brain that are responsible for sound recognition.
The middle part of the ear is surrounded by a huge number of blood and lymphatic vessels and nerve fibers. It is connected to the nasopharynx by thin eustachian tubes, through which air enters the tympanic cavities. It resists the pressure of air, which, together with sound waves, enters the hearing organ through the auditory canals and rests on the eardrums, creating pressure on them. Thanks to the air in the tympanic cavities, they do not bend under external air pressure, but only vibrate under sound waves, transmitting a signal in the form of vibration to the auditory ossicles.
Possible complications of purulent otitis media
The development of the above dangerous diseases occurs rarely. Despite this, it is unacceptable to neglect the symptoms, since the complications of the disease are not limited to intracranial ones, but also include:
- significant hearing loss (in rare cases, complete deafness)
- destruction of the mastoid process of the temporal bone as a result of filling its cells with pus - mastoiditis
- bone caries, or osteitis
- facial paralysis
- cholesteatoma – growth of tissue behind the eardrum
- chronic purulent otitis
How does the disease progress?
Otitis media begins with inflammation of the mucous membrane of the Eustachian canals. Due to the fact that they swell, the flow of air into the middle ear deteriorates. Pathogens, once in the tympanic cavity, begin to actively multiply, inflaming its mucous membrane. After some time, the middle ear fills with exudate. This is the name given to the fluid released from blood vessels during inflammation.
After some time, the exudate becomes viscous and purulent. At the same time, the mucous membrane of the tympanic cavity thickens greatly, ulcers and scars form on its surface. Due to the disruption of the natural removal of fluid in the middle ear (which happens with very swollen Eustachian tubes), there is too much exudate and it completely fills the middle ear. When pus fills the tympanic cavity, all that remains is for it to break through the tympanic membrane and come out. The hole is usually small, but with tuberculosis, scarlet fever, and measles, the gap is larger.
After the membrane ruptures, thick purulent discharge appears from the ears, sometimes with elements of blood. As inflammation decreases, their number decreases and the flow of pus stops. The membrane, after some time, tightens itself and heals. If the gap was not more than one millimeter, there is usually no trace left of it, although congestion is felt for at least some time. With a strong breakthrough, scars and adhesions can form in the middle ear and on the tympanic membrane, which will lead to a decrease in the mobility of the auditory ossicles, which is why hearing acuity is not fully restored.
In the worst situation, pus breaks through the membranes that separate the tympanic cavity from the inside of the hearing organ. This causes extremely serious consequences: if the structures of the inner ear are damaged, this can cause hearing loss or deafness. In addition, the vestibular apparatus is located here, and pus can damage it, which will negatively affect coordination of movements. Also, purulent exudate can go further and reach the brain. This will lead to dangerous complications, including death.
Chronic purulent otitis media
The above symptoms and stages are characteristic of the acute form of the disease. However, in the absence of proper therapy, acute purulent otitis media can become chronic . In this case, pus periodically flows from the ear, the eardrum does not heal, which leads to complete or partial hearing loss. There are two forms of the disease:
- Mesotympanitis is a milder form, usually not complicated by complications.
- Epitympanitis is a severe form of the disease; threatens destruction of the mastoid process, sepsis, brain abscess, meningitis and osteitis.
What are the complications?
If a patient's temperature remains high after a rupture of the tympanic membrane and he continues to feel unwell, this may indicate inflammation in the mastoid process, which is located in the temporal bone behind the ear. That is, about the appearance of mastoiditis. In this situation, urgent medical intervention is necessary, including surgery. Treatment for this disease is not always successful; relapses are possible, especially if the infection has spread to neighboring areas. The disease can cause irreversible hearing loss, loss of coordination, and paralysis. If purulent otitis media in adults and children spreads to the brain tissue, the membranes of the brain may become inflamed (meningitis), a brain abscess and other diseases may develop that can cause death.
After a tympanic membrane rupture, it also happens that the patient’s temperature drops, the pain subsides, and he feels better. But after some time, my ears began to hurt again, and my temperature began to rise. This indicates problems with the outflow of purulent fluid and its retention in the tympanic cavity. The reason for this may be grains (granulations) that have formed in the mucous membrane, or incipient mastoiditis.
Mastoiditis is also indicated by a situation where pus flows from the ear for 3-4 weeks and constantly fills the ear canal after cleaning. Abundant flow of pus from the ear, especially if it is accompanied by pulsation, may indicate the development of an extradural abscess. This is the name given to the accumulation of pus between the bones of the skull and the dura mater. This can lead to various problems, including:
- headache;
- nausea;
- vomit;
- vision problems;
- slow pulse;
- impaired sense of smell;
- damage to the facial, glossopharyngeal, vagus, abducens nerves.
The main cause of complications is lack of treatment or improper therapy. Weak immunity, the high pathogenicity of the pathogen and its resistance to antibiotics also contribute.
Treatment of the disease
Taking into account the various stages, severity and possible complications of the disease, with the question “How to treat purulent otitis media?” It is better to consult a doctor than to use the Internet. The otolaryngologist will make a diagnosis based on a survey and examination and prescribe a comprehensive treatment for acute and purulent otitis media, which will be aimed at:
- suppression of pathogenic microorganisms
- vasoconstriction
- pain relief
The doctor will also determine the stage of the disease, and the therapy will correspond to it:
- At the pre-perforation stage, the main attention is paid to pain relief: Paracetamol or Diclofenac in tablets are prescribed, as well as Otipax or Anauran (contains an antibiotic) in the form of ear drops. Drugs are instilled into the nose to help narrow blood vessels and relieve swelling, such as Otrivin, Naphthyzin and others. An important component of treatment are antibiotics - Amoxicillin (most often), Augmentin (for intense pain and suppuration), Ampicillin, Ceftriaxone (extremely rare, in the absence of effect from the above drugs) and others.
- If the patient seeks help at the perforated stage, that is, when pus appears in the ears, therapy is supplemented with mucolytic drugs - ACC, Fluimucil - to reduce the amount of discharge. If possible, ultraviolet irradiation, ultra-high-frequency and ultra-high types of therapy are prescribed. It is necessary to clean the ear canal from pus every day using cotton swabs. A 3% solution of hydrogen peroxide will help soften too thick discharge. The ear drops used at this stage should not contain alcohol.
- At the final, recovery stage, in the absence of complications, the course of treatment is completed. Now the patient is recommended to focus on strengthening the immune system and improving the body's resistance in order to prevent relapse. To prevent adhesions, massage of the eardrums with air currents and the use of enzyme medications may be prescribed.
The diagnosis of “purulent otitis media” does not exclude surgical treatment:
- If pus accumulates in the tympanic cavity and there is no perforation of the membrane, paracentesis is performed, i.e. an incision made under local anesthesia.
- Ear blowing is carried out in order to cleanse the tympanic cavity from residual purulent masses.
- Severe mastoiditis requires a procedure called an anthrotomy. The cells of the mastoid process are opened and cleaned of pus using antiseptics.
Acute purulent otitis media
Causes
There are three ways for infectious agents to enter the middle ear cavity:
- through the Eustachian tube;
- through a rupture in the eardrum;
- with blood flow.
Of these, the first option accounts for up to 98% of all infections of the tympanic cavity.
The main causes of purulent otitis:
- The presence of a focus of infection in the upper respiratory tract: sinusitis, tonsillitis, scarlet fever, pharyngitis or any other disease.
- Decreased local immunity of the mucous membrane of the nasopharynx and Eustachian tube.
- A general immunodeficiency condition that can occur, for example, during chemotherapy.
Acute purulent otitis is often a consequence of chronic catarrhal otitis.
Symptoms
1. The most typical pain symptom in acute purulent otitis media is:
- Extremely severe pain in the depths of the ear, mainly in the evening and at night.
- Nature of pain: throbbing, shooting.
- The pain radiates to other areas of the head: to the temple, to the eye, to the back of the head, and can affect the entire half of the head.
- During the day, the nature of the pain becomes dull and less pronounced. The feeling of heaviness in the head persists.
- The pain intensifies when coughing, sneezing, or pressing on the ear.
2. Against the background of pain, such classic symptoms as hearing loss, ear congestion, noise and distortion of sounds fade into the background.
3. Feverish state. In the purulent phase, body temperature rises to 39.5°C, in children – above 40°C.
4. Suppuration. Occurs after deformation and rupture of the eardrum under the influence of pus pressure. The pain symptom at this stage is significantly reduced.
Treatment
1. Antibiotics are indicated for all patients with acute purulent otitis, including children under 2 years of age, patients with diabetes, immunodeficiency and other diseases for which antibiotic therapy is contraindicated.
The following drugs are most effective:
- Amoxicillin
- Sparfloxacin
Not prescribed:
- Tetracycline (ineffective)
- Gentamicin (toxic to the auditory system)
2. To relieve pain caused by the pressure of purulent contents on the eardrum, turundas moistened with boric acid and glycerin are placed in the ear.
In the pre-perforation stage, Otipax is used, which has anti-inflammatory and analgesic effects. The alcohol included in its composition makes it impossible to use these drops in case of open suppuration.
To reduce pain, take ibuprofen-based medications.
3. In order to restore the functionality of the auditory tube, vasoconstrictor drops and drugs that relieve local irritation (for example, Tavegil) are used.
4. The result of pus formation is ultimately a rupture of the eardrum. If this does not happen, and the pain becomes unbearable, forced perforation is indicated.
After perforation, the entire complex of drug therapy that was used at the pre-perforation stage is continued.
Significant attention is paid to ear hygiene: pus must be removed 2-3 times a day. Hydrogen peroxide is used to clean and disinfect the external auditory canal. After cleaning, Tsipromed is instilled into the ear.
Treatment of purulent otitis in children
Children are more susceptible to inflammation of the middle ear than adults due to the development of the ear-nose-throat system. Unfortunately, it is children who most often experience relapses, and again parents notice that pus is flowing. In most cases, treatment requires the insertion of a special catheter into the ear, which allows for the following therapeutic manipulations:
- cleansing the middle ear cavity by blowing out the passages
- introduction of antibacterial, anti-inflammatory, antiseptic and analgesic drugs
- restoration of auditory tube functions
Treatment of children should be carried out strictly under the supervision of an experienced specialist, since, firstly, unpleasant symptoms and the danger of complications do not allow experimentation with the child’s health, and secondly, there is a risk of harming the fragile body with medications inappropriate for age, because the treatment of purulent otitis in Adults and children are treated using different techniques and medications.
Treatment
Today, antibacterial therapy is a priority in the treatment of purulent otitis for the following reasons:
- when using antibiotics, the risk of developing complications of otitis media decreases;
- the use of antibacterial drugs improves treatment outcomes for patients at early and late stages of the disease.
Other pharmacological agents are also used in the treatment of purulent otitis media. Painkillers and antipyretics will relieve the child of pain and reduce fever.
Antihistamines help reduce inflammation of the ear mucosa. To reduce the swelling of the Eustachian tube and restore its functioning, you can use nasal vasoconstrictor drops.
Systemic steroids have not demonstrated any effect in the acute phase.
Antimicrobial therapy must be carried out in accordance with the rules.
- Choice of antibiotic.
In the absence of culture results, the choice of antibiotic should have the following two goals:
- the antibiotic should be effective against most common bacterial pathogens;
- the drug must be individualized for the child with regard to allergies, tolerance, previous exposure to antibiotics, cost and level of resistance of the microbial community.
- First choice drugs.
Amoxicillin remains the first choice drug for uncomplicated suppurative otitis in most cases due to its excellent safety record, relative effectiveness, and low cost. Amoxicillin is the most effective oral antimicrobial agent available against S. pneumoniae strains. However, amoxicillin may not be effective against some strains of H. influenzae and most strains of M. catarrhalis. This factor is becoming increasingly important with data showing an overall increase in the frequency of H. influenzae as the primary causative agent of suppurative otitis.
For children with an allergy to penicillins, the first choice of antibiotics will be cephalosporin class antibiotics, for example, cefdinir. If a child has hypersensitivity to cephalosporins, azithromycin is a suitable alternative first-line drug.
- Duration of treatment.
The duration of treatment for otitis suppurativa has historically been set at 10 days, and most efficacy studies examining antimicrobial treatment of the disease have used this duration as the reference. But 10 days may be too long for some children, although not long enough for others. Studies comparing shorter durations of treatment with longer durations of treatment show that short courses of therapy are often insufficient in children under 6 years of age and especially in children under 2 years of age. As a result, for most episodes, in the vast majority of children, treatment for at least 10 days seems appropriate. Treatment for more than 10 days may be necessary for very young children, for severe episodes of suppurative otitis, or if a previous episode of the disease was problematic.
- Unsatisfactory response to treatment with first-line drugs.
Healing from suppurative otitis depends on the eradication of the causative pathogen and the restoration of middle ear ventilation.
Factors contributing to poor response to first-line treatment include:
- ineffectiveness of the selected antibiotic;
- poor adherence to treatment;
- concomitant viral infection;
- persistent dysfunction of the auditory tubes;
- repeated infection of the middle ear;
Despite these many potential factors, switching to an alternative drug is prudent when there is insufficient improvement in the middle ear.
- Second line drugs.
When first-line treatment of purulent otitis media has failed, there are a number of second-line alternatives. These drugs should be effective against strains of H. influenzae and M. catarrhalis, and the most resistant strains of S. pneumoniae. Only 4 antimicrobial agents meet these requirements: Augmentin (amoxicillin-clavulanate), cefdinir , cefuroxime axetil and ceftriaxone (injection).
Since high concentrations of amoxicillin in the body are effective against most strains of S. pneumoniae, and the addition of clavulanate increases the effective antibacterial spectrum of amoxicillin, Augmentin is especially suitable as a second-line drug.
Cefdinir has demonstrated broad therapeutic efficacy, is generally well tolerated, and can be taken once daily.
Ceftriaxone and cefuroxime axetil have important limitations for use in young children. Currently, cefuroxime axetil suspension has an unpleasant taste. Treatment with ceftriaxone entails pain from intramuscular injection. However, the use of ceftriaxone is acceptable in severe cases of suppurative otitis when oral treatment is not possible.
Clarithromycin and azithromycin have only limited activity against resistant strains of S. pneumoniae and strains of H. influenzae. Clindamycin is effective against many strains of S. pneumoniae, including resistant strains, but is not active against H. influenzae or M. catarrhalis. Therefore, it should be prescribed for patients who have an infection caused by penicillin-resistant pneumococci.
The remaining antimicrobial agents traditionally used in the treatment of otitis media have such a significant lack of effectiveness against resistant organisms that their benefits rarely outweigh potential side effects or complications. These include cefprozil, cefaclor, loracarbef, cefixime. Cefpodoxime has shown reasonable effectiveness in some studies, but is generally poorly accepted due to its taste.
Prevention of purulent otitis media
The manifestation and treatment of the disease causes significant discomfort to patients. Therefore, it is worth thinking about preventing the occurrence of a disease such as purulent otitis media.
To avoid the development of purulent otitis, factors leading to the disease should be excluded. Preventive measures include:
- Regular ear hygiene. Please note that cotton swabs should not be inserted into the ear canal - they are intended to clean the corners of the auricle from accumulations of wax!
- Strengthening the immune system. This can be done through hardening, proper nutrition and a healthy lifestyle. This measure will protect you not only from purulent otitis media, but also from a number of other diseases.
- Avoid places with high noise levels, as well as very dusty rooms.
- Before visiting the pool, use special plugs to prevent infection from getting into your ears with water.
- Avoid overcooling your ears: warm scarves and hats will come to the rescue.
Suppurative otitis media is a most unpleasant disease: its symptoms are pronounced and cause severe discomfort. Everyone needs to know what purulent otitis is in order to take action in time: do not self-medicate, but contact a specialist who will decide how to treat the disease. It is important to remember that purulent otitis media in adults and children is treated in different ways due to age-related characteristics.
The site contains exclusively original and author's articles. When copying, place a link to the original source - the article page or home page.
Where does the inflammation come from?
In the international classification system ICD 10, acute purulent and unspecified otitis media are coded H66. In this disease, inflammation affects all parts of the middle ear. This is manifested by a feeling of congestion, pain, noise and ringing, loss of hearing acuity, migraine, and other unpleasant feelings. Manifestations can be either mild, barely noticeable, or severe. But even if the tympanic and other membranes remain intact, purulent otitis media of the middle ear can leave scars, which will reduce hearing acuity. If the disease is not treated, acute purulent otitis media progresses to the chronic stage.
The cause of the disease is a decrease in immunity and the penetration of pathogens into the tympanic cavity, where microflora usually does not live: if pathogenic microorganisms enter here through the Eustachian tube, the immune response quickly destroys them. But with good immunity, they do not cause inflammatory processes and are quickly destroyed. In addition, the mucous membrane of the Eustachian tube produces a secretion that has antimicrobial properties, and the epithelial hairs constantly move the mucus towards the nasopharynx.
When an infection affects the upper respiratory tract, the mucous membranes of the Eustachian canals lose their protective properties, which is why pathogens not only leak into the tympanic cavity, but also develop. This causes an inflammatory response.
Pathogens penetrate into the tympanic cavity in other ways:
- Through a damaged drum membrane.
- Through the injured mastoid process, which is located at the bottom of the temporal bone.
- Through the blood - rare, possible with influenza, tuberculosis, scarlet fever, measles, typhoid.
- From the cranial cavity.
- From an inflamed inner ear.
Most often, acute purulent otitis media affects children under three years of age: their Eustachian tube is wider and shorter than that of older people. In this case, otitis in a child begins sluggishly, but if the disease is not cured in time, it is prone to relapses.
Complications
Acute purulent form of otitis entails negative consequences if left untreated. They appear a month after the onset of the disease. Acquired difficulties are much more difficult to eliminate than the disease itself. The most common complications after ear pathology:
- deafness (temporary or permanent);
- perforation of the tympanic membrane;
- transition of the disease to a chronic course;
- growth of specific tissue behind the membrane;
- destruction of the incus, stapes, malleus in the middle organ of hearing;
- transition of the inflammatory process to the bone;
- meningitis.
The consequences are fraught with inflammation of the brain, which can be fatal. Deafness is also one of the most dreaded forms of complications. If hearing loss has not resolved after 3 weeks from the moment of recovery, you need to sound the alarm. Additional examination, therapeutic measures, including surgical intervention are indicated. Most often, these consequences develop in children due to the structural features of the tympanic membrane.
Causes of the disease
Otitis media occurs when an infection enters the middle ear. The causative agents are various bacteria: streptococcus, staphylococcus, pneumococcus. Most often, those who suffer from the disease are those who often suffer from sinusitis, rhinitis, and have chronic pathologies of the nasopharynx.
With other infections, local immunity is weakened, and bacteria easily penetrate from the nose to the ear. Severe sneezing and pressure on the eardrum increase the risk of developing the disease.
Sometimes the disease begins after an acute respiratory viral infection caused by the influenza virus, scarlet fever, or measles. In this case, otitis media is considered a complication of another disease. When water gets into the ears and hypothermia, the infection develops faster, so in the autumn-winter period you should wear a hat.
See also
How to properly warm the ear during otitis, if it hurts, and is it possible at home?
Read
The development of otitis due to bacteria entering the bloodstream or due to injury is rare.
Consequences
What are the consequences of purulent otitis media?
Although the pain is mainly in the ears, if the infection is severe enough, the infection can also affect other organs. If the treatment was inadequate, this can lead to very dire consequences. When suppuration spreads to the lower jaw and affects the salivary gland, this will lead to disability.
But no less dangerous is the fact that such a disease is not so easy to identify. There are cases when the disease may not be accompanied by ear pain. There are often cases when otitis media disrupts the functioning of the gastrointestinal tract. All this happens because our ears and abdomen are connected by the same nerve. Therefore, often during otitis media, especially in children, vomiting, constipation, and bloating may occur. In this case, you will be suspected of appendicitis and referred to a surgeon. But it is better to diagnose inflammatory diseases in children by involving an otolaryngologist in the procedure.
If suddenly the child’s mother thinks that he just has an upset stomach and does not seek help from the appropriate specialist, then as a result the correct diagnosis will not be made, and in the meantime otitis media will develop into a more serious disease.
Chronic otitis media is very difficult to treat, and the quality of life is greatly reduced - hearing is impaired, and an inflammatory process occurs in the ears and pus appears. Often conventional treatment is not enough and surgical methods must be resorted to.
Diagnostics
There are practically no difficulties in diagnosing chronic mesotympanitis. The entire necessary list of diagnostic tests is carried out both in the district clinic and in the ENT clinic or center.
When diagnosing chronic epitympanitis, otomicroscopy or video microscopy plays an important role - examination of the ear using special instruments - otoscopes and microscopes, i.e. diagnostic and surgical ENT optics. When diagnosing a purulent-carious process and cholesteatoma, an important role is played by: an x-ray of the temporal bone, which is performed in the Schüller and Mayer projection, and a computed tomographic examination of the temporal bones, which today is much more informative compared to x-rays.
Therapeutic measures
You should consult a doctor if ear pain lasts more than 2 days and does not go away. Treatment of otitis media is carried out only after examining the patient. Diagnostics includes collecting a medical history and life history, a general blood and urine test, determining the mobility of the eardrum, otoscopy, and audiometry. To assess the condition of the cavities and structures of the skull, X-ray examination, MRI or CT can be performed. When purulent contents are detected, tympanocentesis (puncture of the eardrum and drainage) is often performed. After the fluid is removed, the patient's condition improves.
Complicated forms of the disease (in the presence of mastoiditis or meningitis) should be treated in a hospital setting. For otitis media, treatment depends on the form of the disease. Treatment of acute otitis involves taking antibiotics, bed rest, taking painkillers, lowering the temperature (if it is above 38.5 degrees), and periodically removing pus. Ears should be washed with disinfectant solutions. Chronic otitis media should be treated by rinsing the ear cavity and instilling boric alcohol. If conservative therapy is ineffective, surgical treatment may be performed.
In the case of non-purulent chronic inflammation, blowing, pneumomassage, and physiotherapy are indicated. Currently, laser treatment in combination with other methods is increasingly used to treat acute otitis media. In order for a person to recover faster, it is necessary to eliminate the main cause of inflammation (eliminate foci of chronic infection and strengthen the immune system).
Pus in the ear: symptoms and treatment of acute purulent otitis
Purulent otitis is a fairly common disease characterized by inflammation of the mucous membrane of the middle and inner ear. Against the background of this pathology, purulent discharge appears in the ear cavity. Some symptoms of this disease resemble the common cold. For example, purulent otitis is also characterized by fever and headaches. And this pathology occurs almost simultaneously with colds.
But there are also specific signs by which the disease is diagnosed . If a cold can be tolerated without seeking help from a doctor, then the appearance of signs of purulent otitis should be the reason for a mandatory visit to the clinic. Otherwise, the lack of proper and timely treatment can lead to significant hearing loss, and in severe cases, to the development of meningitis.
Chronic form
Chronic purulent otitis is determined by inflammation of the middle ear. Its main characteristic feature is the flow of purulent exudate from the ear cavity. Other signs include hearing loss and perforation of the eardrum. This disease, it is worth noting, can manifest itself as chronic rhinitis and sinusitis.
Typically, chronic otitis media can appear in childhood. It can be caused by staphylococci, pneumococci and pseudomonas. This form of otitis may also appear as epitympanitis. In addition to the mucous membrane, the pathological process includes the bone structures of the mastoid process. Its localization is in the upper part of the membrane. This form is dangerous because it progresses to dangerous complications, such as meningitis, sepsis, osteitis and brain abscess.
Purulent otitis in a child usually occurs in an acute form.
Ear treatment
To reduce pain, the doctor may prescribe topical osmatic drugs and general pain medications. Ear drops for purulent otitis should be used carefully: if the pus has ruptured the tympanic membrane, many medications should not be dripped into the ears. If an ototoxic agent ends up in the middle ear, it can cause serious damage and cause hearing loss.
Since pus is usually caused by bacteria, the doctor will prescribe antibiotic therapy. If you know you are allergic to any type of antibiotic, you should definitely tell your doctor. Otherwise, instead of treating with an antibiotic, you can cause serious damage to the body, even death.
Treatment of purulent otitis with one type of antibiotic should not exceed ten days. If the medicine does not work during this time, it means that it is ineffective, and you need to look for an alternative option. If the antibiotic helps, it will be noticeable before ten days. Sometimes the doctor may decide that it is necessary to cut the eardrum to release the purulent exudate. This operation is called paracentesis. They resort to it in extreme cases, if symptoms appear that indicate damage to the inner ear or meningitis. These include dizziness, severe migraines, and vomiting. Also, this operation is more often prescribed to children than adults, since their tympanic membrane is thicker, and therefore better resists the pressure of pus from the middle ear. In this case, otitis symptoms in children make themselves felt more strongly and require immediate intervention.
Once healing occurs, once the eardrum has healed, the focus is on restoring the eustachian tube and improving immunity . The doctor prescribes various physiotherapeutic procedures (pneumatic massage of the drum membrane), vitamin complexes. After recovery, the patient must remain under medical supervision for about six months. If during this time problems are discovered with the hearing aid, additional procedures are prescribed.
Clinical signs of the acute form of the disease
The acute course of the disease is characterized by severe pain, abundant purulent accumulations in the ears, and swelling. Doctors distinguish right-sided and left-sided acute purulent otitis media. Ear inflammation is divided into 3 stages. Each of them is accompanied by a number of signs.
initial stage
At the first stage of the disease, the main complaints are pain, noise and congestion in the ear. Painful spasms are usually shooting, pulsating, stabbing, they are quite painful, and often prevent the patient from sleeping. Unpleasant sensations radiate to the jaw, temples, and intensify when chewing, sneezing, coughing. Patients experience hearing loss. Hyperthermia, a general weakness in the body, is also present. Upon examination, the doctor observes a reddened and swollen membrane. Pain is noted on palpation.
Acute period
During the acute purulent stage, holes appear in the tympanic membrane, from which pus flows. Perforation occurs on the 2-3rd day of illness. At this stage, pain decreases, the patient’s condition improves, and the temperature drops to normal levels. Acute purulent otitis media in children sometimes resolves without perforation of the membrane because it is too thick. This slows down the healing process and requires surgery. Patients are prescribed puncture of the eardrum. During the operation, a small hole is made in the membrane through which the purulent accumulation is sucked out. After the intervention, the patient feels much better. If it is done on time, recovery will come and deafness will go away.
Recovery stage
The recovery stage of ear pathology is characterized by the cessation of suppuration, the inflammatory process subsides, and the tympanic membrane heals.
The medical history of acute purulent otitis media helps the doctor to reliably establish a diagnosis; the doctor studies this paper and takes into account the necessary information. It should be noted that the signs of the disease are felt more strongly in some people, while in others they are mild. Often, the manifestations are most clearly felt at the middle stage of the disease.
Treatment of acute purulent otitis media involves the use of antibacterial, anti-inflammatory and painkillers. After recovery, hearing is completely restored, on average after a month, differently for each patient. If this does not happen, you need to consult a doctor.
Treatment of chronic otitis media
Chronic otitis - the purulent form of middle ear disease can be treated using various methods. With the conservative method, both local and general treatment methods are used simultaneously. They include cleaning the external auditory canal and partially the tympanic cavity using antiseptic agents, after which desensitizing and antibacterial drugs are administered in the form of drops or by injection to relieve swelling. It is effective to catheterize the auditory tube on the affected side in order to relieve its swelling and administer vasoconstrictor and desensitizing medications. The next stage of treatment is also carried out - they act on the mucous membrane of the middle ear using drugs such as 0.5% dioxidine solution, 0.01% miramistin solution and some other drugs that are effectively impregnated into the mucosa through ultrasonic medicinal irrigation. Therapeutic laser is also used. When stable clinical remission is achieved, the patient is sent to an ENT hospital for myringoplasty - a surgical operation to restore the integrity of the eardrum using a graft.
Patients with epitympanitis generally need to be treated through ear surgery. After the necessary preparation and conservative treatment of the diseased ear, patients are sent to an ENT hospital along with the results of X-ray and computed tomography studies.
Causes
The cause of acute otitis media is an infection, most often nasopharyngeal. The cause of chronic otitis media is an acute illness that is not fully cured. What can cause infection of the eustachian tube and middle ear?
- chronic inflammatory diseases of the nasopharynx (sinusitis, tonsillitis, adenoids, frequent runny nose);
- improper nose blowing, too strong and through both nostrils at the same time;
- injuries with infection entering the ear cavity - this is how otitis externa is complicated
Folk remedies for the treatment of otitis
Traditional methods are used as a complement to traditional medicine. The greatest therapeutic effect is achieved by using herbs, but they do not relieve pain and swelling quickly.
A few drops of wild garlic into the ear canal will help fight infection, and chamomile will reduce inflammation and pain. Kalanchoe juice, diluted with water in equal proportions, will have an antimicrobial and anti-inflammatory effect. Apply 3 drops 2 times a day.
Using a swab soaked in hydrogen peroxide and placed in the ear for 5 minutes will help remove discharge and bacteria.
Propolis tincture helps destroy microbes, relieves pain, and speeds up the healing process. Apply 5 drops to each ear 3 times a day.
Warming a sore ear at home is prohibited. As the temperature rises, bacteria begin to multiply intensively, which leads to increased secretion of pus and provokes inflammation in other places.
Treatment methods
Of course, the question arises: if pus is found in the ears, what to do? It is absolutely not recommended to attempt self-treatment if a person has purulent otitis in the acute stage. This pathology can lead to meningitis. Therefore, it is extremely important to contact an ENT specialist in a timely manner.
The doctor will prescribe the patient a course of antibiotic therapy. The most commonly used drug is Amoxicillin. If there is pus, it is strictly forbidden to apply warm compresses to the sore ear. You should not use any drops yourself.
In the case of chronic otitis media, the doctor will initially clear the cavity of pus. The patient will be recommended special antibacterial drops. And further treatment methods depend on the size of the hole in the membrane. For small sizes, use a film made of artificial fabric. Under it, the wound completely heals within 2-3 weeks. If the hole is large enough, then tympanoplasty is performed (surgical restoration of the membrane).