Keratitis is a general name for a number of diseases of the visual analyzer, the distinctive characteristic of which is inflammation of the cornea of the eye.
Due to the accumulation of infiltrate, cloudiness occurs, which in the case of purulent infection is accompanied by necrosis of the corneal tissue.
Pathology can occur either as an independent disease or as a consequence of existing disorders in the body.
Keratitis of the eye leads to decreased visual acuity, glaucoma and even loss of the eyeball. The sooner the patient receives medical assistance, the greater the chance of avoiding undesirable consequences.
This article will help you understand what keratitis is, describe its symptoms and treatment.
Causes of keratitis
Keratitis has a varied etiology. But in most cases (about 70%) the causative agents of the disease are herpes simplex and herpes zoster viruses (shingles). Other reasons include:
- infections: viral (causative agents are: adenoviruses , varicella zoster virus , measles);
- bacterial. Causes purulent keratitis of the eye (pathogens: streptococci , staphylococci , Pseudomonas aeruginosa and Escherichia coli , pathogens of tuberculosis , diphtheria , syphilis);
- fungal (candida, aspergillus, fusarium mushrooms);
- chlamydial infection (chlamydia);
- parasitic (amoeba, leishmania, worms).
Provoking factors for the development of the disease
Factors that favor the development of pathology include:
- vitamin deficiencies;
- decreased immunity;
- disruption of the trigeminal nerve;
- diabetes;
- history of gout.
Keratitis of unknown etiology
This group of keratitis includes diseases for which the main cause of development cannot be identified. These include: rosacea keratitis, corrosive Moraine ulcer and filamentous keratitis.
Rosacea keratitis is a chronic disease that affects the facial skin and cornea. The disease is progressive. Often seen in older people. Factors that provoke the appearance of the disease are: hormonal imbalance, lack of vitamin B12, impaired peripheral circulation, allergic reactions.
Filamentous keratitis is a chronic disease that is a manifestation of hypofunction of the lacrimal gland (Sjögren's syndrome).
Morena's ulcer is a rare disease of autoimmune origin. It occurs in the following forms:
- Unilateral corrosive ulcer;
- Bilateral corrosive ulcer;
· Chronic bilateral corrosive ulcer.
Symptoms of keratitis
The main and common symptom for all keratitis is corneal syndrome. It is characterized by:
- photophobia (photophobia);
- excessive tear production;
- reflex closure of the eyelid (blepharospasm).
Corneal syndrome occurs due to the pressure of the infiltrate on the nerve endings. The accumulation of leukocytes, plasma cells and histiocytes leads to a decrease in the transparency of the cornea, disruption of its shape and clouding.
Against this background, sensations of a foreign body in the eye, discomfort and pain occur. The cornea of the eye becomes rough and turns red (see photo above). Patients note worsening vision.
Symptoms
Main signs of pathology:
- sharp cutting pain in the eye;
- secretion of tear and purulent fluid;
- photophobia (fear of light);
- uncontrolled contraction of the orbicularis oculi muscles;
- swelling of the conjunctiva.
With bacterial keratitis, clouding of the cornea, its swelling, and infiltrates (accumulations of cellular elements with blood and lymph) of a gray-yellow hue appear in its tissues. Within 24 hours, deep ulcers with a purulent bottom form at the site of corneal infiltrates. On one side, the border of the formation is smooth, and on the other, it has a progressive yellow tint. The progressive side increases within 3 days and covers a larger area of the cornea.
The inflammatory process also involves the choroid (choroid) - this is a soft pigmented tissue dotted with vessels, which is located between the sclera (tunica albuginea) and the retina. Bacterial keratitis progresses, pain in the eye intensifies, the choroid turns yellow-green, swells, and the shape of the pupil changes.
The space between the cornea and iris is filled with purulent exudate, which consists of white blood cells and fibrin (protein). After the protein folds, the liquid turns into an elastic film, which is connected to the cornea. In some cases, the cornea dissolves and a through hole appears. If bacteria penetrate this hole, an acute inflammatory process will occur on the retina.
Classification of keratitis
Viral keratitis
Parenchymal keratitis in late congenital syphilis
Keratitis is classified according to several criteria.
- Due to the occurrence: bacterial keratitis (congenital parenchymal keratitis, the development of which is caused by the causative agent of syphilis, is separately distinguished);
- viral keratitis;
- allergic;
- fungal keratitis;
- caused by protozoa, most often amoebas;
- photokeratitis;
- traumatic keratitis;
- neuroparalytic keratitis, occurs due to damage to the trigeminal nerve;
- unknown etiology (idiopathic keratitis).
- endogenous, or developed due to internal reasons (vitaminosis, rheumatism, allergic reactions, etc.);
- superficial (inflammation is localized in the upper layer);
- central (at the pupil);
Congenital keratitis
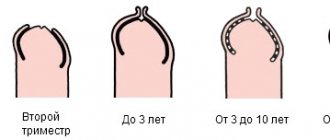
Parenchymal keratitis is the extreme stage of congenital syphilis. It manifests itself even after several generations. People under 20 years of age are especially susceptible to it.
The pathology is characterized by cyclicality, bilateral lesions, redness of the choroid and the absence of corneal lesions.
What is this?
Often patients come to me with red eyes, who for some time have been independently and unsuccessfully treated for what they believed was conjunctivitis. Upon examination, it may turn out that this is a more serious disease that requires immediate qualified help.
Let's figure out what keratitis is. Essentially, keratitis is any inflammation of the cornea, the front layer of the eye that protects and separates the deeper structures of the eye from the external environment. Correct initial diagnosis and treatment are critical to limiting the amount of residual damage and scarring on the cornea. Preserving the transparent properties of the cornea is necessary to restore and maintain the patient's vision.
Due to its transparency and shape, the cornea is involved in the process of vision, so a violation of the transparency of the cornea can lead to decreased vision.
The cornea consists of five layers:
- Anterior epithelium;
- Anterior limiting membrane (the so-called Bowman's layer);
- Corneal (stromal) substance, making up 90% of the thickness of the cornea;
- Posterior limiting membrane (Descemet's membrane);
- Endothelium.
The cornea is lubricated on the outside by the tear film, which is very important for refracting light over it and therefore providing clear vision. It is permeated with many sensitive nerve endings that perceive stimuli and transmit them further. Any irritation of the nerve endings, including inflammation of the cornea, causes pain, increased lacrimation and photophobia. Inflammation of the cornea is a reaction of the immune system of the eye to pathogenic microorganisms, injuries or other irritations. Inflammation can occur in different layers of the cornea individually or in combination. Symptoms depend on which layer of the cornea is affected and what is causing the inflammation.
Inflammation of the outermost layer of corneal cells, the epithelium, often results in cloudy corneas. If the lower layer, the endothelium, is affected, corneal edema may occur. If the thickest layer between them (the stromal layer) becomes inflamed, white corneal deposits may appear.
At the first symptoms of keratitis, you should immediately consult an ophthalmologist, as serious complications are possible.
Diagnostics
Corneal syndrome is the first sign that will help the ophthalmologist diagnose inflammation of the cornea in a patient.
To conduct further research, the specialist instills anesthetic drops into the patient. This will help relieve spasm and open the eyelids.
The next step will be collecting anamnesis, general examination and checking visual acuity.
To clarify the diagnosis, ophthalmologists resort to such additional research methods as:
- biomicroscopy (study of the structures of the visual analyzer using a slit lamp);
- ophthalmoscopy (allows you to evaluate changes resulting from the inflammatory process);
- staining corneal tissue with fluorescein for better visualization of structural changes;
- Ultrasound.
Pathogens of inflammation
Viral keratitis of the eye is provoked by:
- herpes;
- get excited by chicken pox;
- adenovirus;
- measles virus;
- endemic mumps;
- flu.
The risk of keratitis especially increases if, when infected with one of the listed infections, the integrity of the cornea is disrupted or the permeability of its surface layer increases. This usually occurs after injury, foreign body entry, or other impacts.
Also increasing the likelihood of viral keratitis is a decrease in immune function against the background of constant stress and shock, hypothermia, physical overload and hormonal changes (in women).
Treatment of keratitis
Treatment of eye keratitis must be carried out in a hospital and lasts five days. Continues at home if necessary. If a patient has keratouveitis in parallel with keratitis, the symptoms of the disease can persist for up to several months.
Drug treatment
To achieve a speedy recovery, local and systemic therapy is used.
Systemic therapy necessarily implies:
- taking medications designed to destroy pathogens. For purulent inflammation, antibiotics are prescribed (Ciprofloxacin , Ceftriaxone , Moxifloxacin). For viral nature of keratitis - Acyclovir. Fungal keratitis is treated with Voriconazole, Fluconazole, Itraconazole;
- detoxification measures (droppers with saline or Rheosorbilact, drinking plenty of fluids);
- prescribing antihistamines to reduce swelling (Zyrtec, Zodak, Desloratadine).
Additionally, the patient is prescribed aloe extract to improve the trophism of the affected tissues and multivitamin complexes.
Keratitis of any nature requires local treatment. For this purpose, use:
- eye drops containing antibiotics (Tobrex, Floxal);
- eye drops with an antiseptic (Oftamirin, Okomistin, Albucid), which will not only have a detrimental effect on pathogenic microorganisms, but will also prevent the addition of a secondary infection;
- Okoferon drops, if the cause of the disease is a virus;
- Zovirax (ointment), if the causative agent of keratitis is the chickenpox virus or herpes;
- drops with corticoids (Maxidex, Sofradex, Tobradex), which prevent damage to the deep layers of the cornea;
- ointments or gels that accelerate regeneration processes (Lakropos, Korneregel, Vidisik).
Drug treatment of ocular keratitis is usually supplemented with physiotherapy (phonophoresis, electrophoresis, magnetic therapy).
Parenchymal keratitis requires specific treatment. The first stage is preparation - taking iodine preparations, then administering Bioquinol intramuscularly.
The second stage is treatment with penicillin for 14 days. Along with the antibiotic, mydriatics (Atropine, Irifrin, Cyclomed), yellow mercury ointment, dionine solution and corticosteroid drugs are prescribed locally.
Surgery
The indication for surgery is the presence of ulcers on the cornea of the eye. To eliminate tissue defects, modern microsurgery methods are used: laser coagulation and cryoapplication. If a scar has formed, keratoplasty is performed.
Prevention
Patients who have suffered keratitis are often interested in preventive measures. I usually list the following:
- Frequent hand washing;
- Use of separate towels;
- Use of selected personal care products
- Elimination of exposure to allergens;
- Wearing closed-sided safety glasses to reduce exposure to external irritants;
- Rinsing the conjunctival sac with a 0.9% saline solution or artificial tears without preservatives, which helps reduce the concentration of various allergens and irritants present on the surface of the eye;
- Elimination of exposure to adverse environmental factors: cold, dry air, strong wind, smoking, smoke, staying in air-conditioned rooms;
- When working on a computer, the monitor should be located approximately 10-20 degrees below the line of sight (if the monitor is too high, the eyes open wider and the mucous membranes dry out);
- If you wear contact lenses, pay special attention to their disinfection - never use lenses after the wearing period has expired, always put on lenses with clean hands;
- Pay attention to nutrition. For eye health, include Omega-3 (fatty fish) and antioxidants (green vegetables) in your daily menu;
- Wear swimming goggles in the pool to minimize the risk of getting chlorinated water in your eyes;
- In spring and summer, wear sunglasses with UV filters.
Forecast
The outcome of the disease mainly depends on the nature of tissue damage, the location of the infiltrate and the complications that arise.
Therapy at the initial stages of the pathology shows good results - the infiltrate resolves without consequences or minor opacities occur.
If treatment is not provided on time, the outcome of the disease may be:
- thorn;
- glaucoma;
- optic nerve atrophy;
- atrophy of the eyeball;
- loss of visual function.
Physiotherapy and surgery
If ulcers are present, cryoapplication and laser coagulation procedures are performed. In the first case, pathological tissues are removed using low temperatures, in the second - under the influence of a laser beam.
Electrophoresis, diathermy procedures, and stimulation of eye tissue with a helium-neon laser help improve blood supply and trophism of corneal tissue.
If the above methods do not give a positive result, surgery is prescribed. In the superficial form, the surgeon scrapes off the affected corneal tissue. This is a fairly simple and easy operation. If the inner layers are damaged, a layer-by-layer or through operation is performed. This is the removal of tissue affected by keratitis, followed by the application of thin suture material.
Additional rehabilitation therapy in a hospital is required.
Herpetic keratitis
This type of keratitis is caused by herpes. In this case, even several types of herpes can develop. Then the disease takes a long time to be treated and often returns.
Herpetic keratitis develops on the surface or inside the clear outer layer of the eye. If only the upper part is affected, ulcers and erosions will become noticeable. The patient will have something in the eye that is bothering them. Tear production increases. The eye looks red. Often in this type, damage to the blood vessels of the eye occurs. And this contributes to the penetration of the disease deeply.
Vision decreases, the cornea is cloudy. Even, possibly, the formation of a cataract, which often leads to complete loss of vision in that eye. In very severe forms of herpetic keratitis, there may be indications for organ removal.
Positive dynamics during treatment are guaranteed, but only with early contact with a specialist. Therapy consists of the use of antibiotics, antiseptics, and steroids.
What are the types of keratitis?
The rarest form is fungal keratitis. A pathological condition can develop as a result of injury to the organs of vision, when debris or foreign bodies enter the eye. Most often, this problem occurs in patients living in rural areas. If you do not seek medical help in a timely manner, you can provoke a significant spread of the infection, in which the entire eye will be affected.
Signs of infection may appear two to three days after the infection occurs. If debris is not removed from the eye, the condition may worsen, with keratitis turning into an ulcer that gradually invades nearby tissue. The presence of fungal keratitis can be suspected if the following signs are noted:
- The source of inflammation is quite large in size;
- The color of the inflamed area is white or yellow;
- Dryness appears in the area of inflammation, sometimes the areas become covered with a curd-like coating;
- The inflamed area is fenced off with a roller - it determines the boundary of infiltration.
Symptoms do not change within several days.
The disease itself can continue to develop. The resulting cushion begins to disintegrate, and the corneal cells die. Sometimes the focus of inflammation moves away from the cornea, forming a depression, which then becomes a cataract. Viral keratitis can be triggered by pathogens present inside the body. The disease is most often observed in adolescents. The source of inflammation can be localized in the upper part of the cornea, sometimes it penetrates into the depths. At the same time, the cornea loses transparency and vision decreases. If the disease becomes particularly severe, the corneal tissue gradually becomes dead.
Keratitis can be caused by herpes simplex or herpes zoster. The viral variety of the disease is divided into several subtypes:
- Bacterial. Caused by bacteria of various origins. Often occurs as a result of injury or in people using contact lenses;
- Amebic. This type of lesion is very dangerous and can lead to blindness;
- Viral – the cause may be the herpes virus present in the body;
- Fungal. This form is also very dangerous. May lead to the appearance of ulcers on the cornea and its perforations;
- Allergic keratitis. It represents the so-called vernal keratoconjunctivitis, in which inflammation begins due to an allergic reaction. Another type is onchocerciasis keratitis;
- Purulent keratitis is an ulcer, the condition is quite severe;
- Photokeratitis - appears as a result of burns on the cornea due to excess ultraviolet rays.
The signs of the disease are quite pronounced; frequent recurrences and a long course of the disease are characteristic. Small bubbles form on the cornea, sensitivity gradually disappears, and sometimes a more serious condition develops - trigeminal neuralgia. The affected eye turns red and pain begins. The blisters burst after some time, after which ulcers appear. With subsequent relapses, visual acuity decreases.
If ulcerative keratitis occurs, there is a danger of losing all vision. Scars appear on the cornea, the edges and sometimes the center are affected. The shape of ulcers and sizes may vary. At first, the patient may feel a slight pain, which becomes more obvious when blinking. The eyes become sensitive to light, tears may flow, and purulent discharge occurs.
Traumatic keratitis can occur due to damage to the cornea due to contusion, burn, or when a foreign body penetrates under the eyelid. With further development of the disease, the vessels may grow into the cornea.
The superficial variety is characterized by the appearance of branching vessels. With severe injuries, they may begin to grow into the cornea. The result is erosion forms, pain appears, and uncontrolled flow of tears begins. Among the main symptoms of the disease is a twitching eyelid.
In punctate keratitis, the lesions appear as small dots that create defects in the cornea. When this happens, the eyes turn red and vision deteriorates, and tears begin to leak. There is a feeling of roughness and slight tingling in the eyes.
Diagnosis of keratitis
Any unpleasant symptoms in the eye area are a reason to urgently consult an ophthalmologist. Keratitis can progress quickly and lead to irreversible consequences, so it is dangerous to hesitate and wait for everything to resolve itself. The diagnosis is made based on the medical history and objective symptoms discovered by the doctor during the examination. To determine the disease, the following information is important:
- the patient has chronic infectious and non-infectious diseases;
- recent illnesses (flu, ARVI);
- use of any medications;
- all complaints about the organ of vision;
- any other health and well-being problems;
- eye injuries, exposure to other adverse factors.
During a visual examination, a specialist can immediately notice the symptoms of keratitis. To determine the safety of eye functions, visual acuity is checked, a biomicroscopic examination of the eyes is performed (assessment of the state of media and tissues using contrast lighting), algesimetry or estensiometry (study of the sensitivity of the cornea using special devices or electronic devices). To assess the production of tear fluid, a Schirmer test is performed. Culture of a smear from the surface of the cornea allows you to identify the causative agent of inflammatory changes and correctly prescribe medications.
To collect additional information and determine the causes of keratitis, a general examination is prescribed, which includes general blood and urine tests, a biochemical test, and rheumatic tests.
In the process of differential diagnosis, it is important to correctly determine the type of keratitis and its etiology. This depends on the treatment tactics and prognosis.
Table - Differences between the main types of keratitis
| View/ Index | Corneal syndrome | Infiltrate | Corneal sensitivity | Laboratory diagnostics |
| Fungal | Moderate | Spilled, fuzzy edges | Saved | Bakposev |
| Acanthamoeba | Expressed | Ring-shaped | M.b. reduced | — |
| Herpetic | Pronounced or absent | Tree-shaped, disc-shaped | May be missing | ELISA |
| Bacterial | Sharply expressed | Different | Saved | Bakposev |
| Endogenous | Moderate | Deep penetration | Saved | Tests for specific infections, allergy and immunoassays |
| Neurotrophic | May be missing | Different | Absent | — |
Clinical manifestations
Marginal keratitis occurs with a clear clinical picture. Patients complain of excessive tearing, photophobia, and blepharospasm.
A feeling of a foreign body in the eyes develops, which causes the patient to blink frequently.
A characteristic symptom is clouding of the iris , which loses its shine and transparency.
Visually, the affected eye differs from a healthy eye not only in the cloudy iris, but also in the redness of the conjunctiva with visible vascular mesh, the presence of grayish-white spots on the cornea - infiltrates and ulcers.
Attention! With marginal keratitis, pain also occurs - pain in the eyeball appears during the process of opening the eyes.
Classification
Doctors divide viral keratitis into two main types:
- Primary type. This problem is most often noticed between the ages of 6 months and 5 years. Symptoms of primary type viral keratitis include a visculous rash on the skin, as well as enlarged lymph nodes. The disease is quite easy, and complications practically do not arise.
- Secondary type. This type of disease occurs at any age. The disease may be accompanied by complications in the form of keratopathy, in which the strength of the cornea is impaired. Additional symptoms include: slight discharge of gray or white fluid from the eyes, pain, and swelling.
Fungal keratitis
Pathomorphology
Changes in the tissues of the cornea during keratitis consist in the occurrence of the following processes. The cornea of the eye becomes infiltrated and swells due to the formation of a large number of polynuclear leukocytes and lymphoid cells.
Infiltrates have vague boundaries, different sizes and shapes. After acute processes subside, vascularization of the cornea is observed (formation of new vessels).
This phenomenon is twofold: it improves the trophism of the cornea, but, at the same time, helps to reduce its transparency. With prolonged keratitis, areas of necrosis, abscesses, and corneal ulcers may develop. Large ulcerations after scarring form an eyesore.
ethnoscience
Keratitis is very widely treated with traditional medicine. The most common ones are listed below:
- Sea buckthorn oil will help with light intolerance and soothe pain. First, 1 drop is instilled every hour, then (after a couple of days) the interval is increased to 3 hours. Using this remedy, you can feel noticeable relief even in advanced cases.
- If there is suppuration, then 2 drops of celandine juice (freshly squeezed) are instilled before bedtime, it is diluted with aqueous propolis extract in the ratio of 1 part juice to 3 parts propolis extract. If irritation occurs, the propolis extract must be increased.
- Clay lotions that are applied to the eyes, forehead and back of the head help a lot. To do this, put a 3 cm layer of clay in a napkin. The clay should be soft, not flowing, smooth and dense. Such compresses should be kept for about an hour or two. It is recommended to do 2-3 lotions per day.
- The juice from an aloe plant that is more than 3 years old must first be kept in the refrigerator for 10 days, then strained and diluted with mumiyo (about the size of a match head). Instill 1 drop of the resulting mixture once a day into one or both eyes. After a month, you can no longer add mumiyo, but only drip juice.
- In freshly baked rye bread you need to make a depression in which you need to place the glass upside down. Drops will form on the walls of the glass, which must be carefully collected and dripped 2-3 drops into both eyes once a day.
Additional symptoms of keratitis
Prognosis and prevention
Deep keratitis of a viral nature, which is accompanied by severe ulceration and persistent clouding of the cornea, often results in a sharp deterioration in vision. Therefore, it is very important to prevent inflammation.
Prevention of viral keratitis:
- prevention of primary infection;
- vaccination;
- protection against microtraumas;
- increasing stress resistance;
- no hypothermia.
Each person should pay increased attention to factors that may contribute to the activation of the latent virus (weakened immunity, poor diet, etc.). A healthy lifestyle and infection prevention will help avoid keratitis and its complications.
Keratitis: prevention
Prevention of this disease is quite simple and requires compliance with the following rules:
- Carrying out work in which the eyes may be injured, wearing special safety glasses;
- Strict adherence to hygiene rules when using contact lenses;
- Work with welding in a protective mask, avoiding prolonged exposure to the sun;
- Timely treatment of eye diseases such as: conjunctivitis, blepharitis, dacryocystitis;
- Timely treatment of common pathologies that stimulate the development of keratitis.
If you still notice the first signs of developing this disease, immediately seek professional medical help! Remember: the key to successful treatment is its timeliness!
How is viral keratitis treated?
Comprehensive treatment of the disease increases the chances of a favorable outcome. For this purpose, medications are used that directly affect the pathogen itself, increase the body’s defenses, and drugs that help restore damaged tissues. The basic treatment of the disease is the prescription of antiviral drops (Interferon, Acyclovir) and ointments (Zovirax, Florenal). If the disease is severe, it would be advisable to use internal antiviral drugs in large doses, especially if it is viral keratitis.
The activity of the immune system is increased with the drugs Timalin or Levomesol. To treat pain and alleviate the patient's condition, analgesics (Analgin), antiallergic drugs (Tavegil, Diphenhydramine), non-steroidal anti-inflammatory drugs (Diclofenac, Indomethacin), proteolytic enzyme inhibitors (Kontrikal), pupil dilatants (Atropine, Cyclomed), antioxidants (Emoxipine) are used. and vitamins.
Herpetic ulcers can be treated using cryoapplication or laser coagulation. If treatment with conservative methods is found to be ineffective, and corneal ulceration continues to develop, then the next step will be surgical intervention.
Treatment of contagious forms of viral keratitis requires isolation of the patient at home or in a hospital with mandatory observance of personal hygiene rules.
Features of the viral nature of keratitis
Viral keratitis is a manifestation of general infection. Most often, this diagnosis is made to children and young people when the body is infected with the herpes simplex or herpes zoster virus. These filtering neurodermotropic viruses significantly aggravate the course of viral keratitis.
There are primary viral keratitis of herpetic etiology and post-primary, when the latent virus is activated. Herpetic infection is characterized by a long-term inactive state; during this period, the pathogen accumulates in the epithelium of the conjunctiva and trigeminal ganglion.
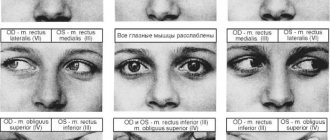
Types of keratitis according to the clinical picture:
- point;
- tree-like;
- vesicular;
- discoid;
- metaherpetic;
- diffuse.
Viral keratitis can be superficial or deep. Superficial affects the epithelium and upper layers of the base of the cornea, and deep affects the entire stroma. Common complications of viral keratitis include abscess, necrosis, and corneal ulcers. This condition is characterized by significant deterioration in visual function and clouding of the cornea.
Diagnosis of the disease
To more accurately determine the form that keratitis takes, a detailed examination by an ophthalmologist is necessary. Research for this can be carried out as follows:
- A general assessment of visual acuity is carried out using a table;
- The lesion is examined using a special slit lamp;
- The doctor will interview the patient to find out if there are any complaints;
- A hardware examination of the cornea is performed.
In addition to the listed procedures, in order to more accurately assess the situation, a scraping may be prescribed. This helps to find out the reason why inflammation developed. When it is determined, the doctor, based on the information received, will select medications and prescribe a regimen for taking them.
Paying attention to treatment will help prevent significant problems.
Preventive measures
Prevention of keratitis involves strict adherence to hygiene standards, which are usually provided for review in the ophthalmologist's office. They are similar to those required when wearing contact lenses. It is imperative to protect your eyes from the influence of chemicals and prevent injury. You should contact a specialist in time to cure ailments such as blepharitis and dacryocystitis, conjunctivitis, and other diseases if their signs are detected. Working on boosting your immunity also helps improve the situation.
If there are any problems with the organs of vision that make it possible to suspect an infectious disease, it is recommended to quickly consult an ophthalmologist and carefully follow his recommendations. This helps prevent the disease from developing and prevents relapses. When suffering from keratitis, there are no special changes in the patient’s daily life. But you should be more attentive to your condition, follow the advice of your doctor, do not linger in dusty rooms, smoky rooms, and try to avoid hypothermia.
Regional type of keratitis - what kind of disease is it?
Marginal keratitis of the eye occurs as a result of complications of other infectious diseases of the organs of vision (eyelids or conjunctiva). This is how the body reacts to pathogenic microbes or chronic inflammation of the mucous membrane of the eye, eyelids and glands of the cartilage of the eyelids.
The main feature of this disease, which affects the periphery of the cornea, is the development of an inflammatory process that leads to degeneration of the superficial corneal layers.
Penetration of pathogens into the cornea occurs exogenously. Under the influence of pathogenic bacteria, the eyelids shrink, as a result of which the nutrition of the cornea is disrupted. This also leads to the formation of bloody infiltrates, due to which it becomes cloudy.
If treatment is not started in time, after the infiltrates resolve, ulcers will form, in place of which scars will remain in the future.
In the chronic form of the disease, a superficial marginal type of keratitis develops, characterized by the accumulation of small infiltrates. In some cases, they can resolve on their own, but as soon as the pathological process affects the anterior cornea, an ulcer forms, leading to its clouding.
Complications and prognosis
If a person neglects the disease or does not follow the doctor’s recommendations, the cornea becomes completely cloudy. Visual acuity decreases. To prevent infection and complications, it is necessary to avoid eye injury, stress, and hypothermia.
When the immune response decreases, the infection easily spreads deep into the cornea. With timely treatment, viral keratitis goes away within a month.
Viral keratitis is a frequently diagnosed disease among ophthalmological pathologies. Usually the causative agent is a herpes infection. It is important to consult a doctor promptly at the first signs of illness.
Have you suffered from viral keratitis? Tell us your medical history. Share the article with your friends on social networks. Be healthy.
What causes keratitis to develop?
The reasons why the disease appears may be:
- Past colds;
- There is a herpes virus in the body;
- Decreased immunity;
- The presence of adenovirus, measles pathogens;
- Fungi that have received an impetus for development due to the use of antibiotics;
- The appearance of allergies;
- Staphylococcus, other bacteria, Escherichia coli and Pseudomonas aeruginosa;
- Corneal burns;
- Injuries leading to eye infection.
Symptoms
Symptomatically, the disease manifests itself in two forms - primary and post-primary. Main symptoms of primary infection:
- photophobia;
- lacrimation;
- blepharospasm;
- mixed infection with a predominance of pericorneal infection.
The patient complains of severe pain and purulent discharge from the eyes. The iris is dotted with dilating vessels, as a result of which ciliary pain intensifies. The disease does not go away on its own - it can only “fade out” temporarily.
Post-primary herpetic keratitis does not have as severe symptoms as primary one.
Post-primary herpetic keratitis is not so acute, the discharge from the eye is quite scanty. Corneal syndrome is not very pronounced. Exacerbations of the disease usually occur in autumn and winter.
Effective treatment
Treatment of this form of pathology is usually carried out in a hospital setting under the supervision of the attending physician. This helps to evaluate the effectiveness of the prescribed therapy, as well as avoid dangerous complications. Depending on the cause of the development of marginal keratitis, treatment is:
- If the disease is caused by a fungal or viral infection of the eyes, then antibacterial and antiviral effects are prescribed. For this purpose, drugs are used in the form of tablets and drops.
- If a foreign object gets into the eye, it should be removed using special tools using antiseptic drugs.
The marginal form of the disease, caused by dysfunction of the lacrimal glands, is eliminated with the help of moisturizing eye drops.
- In some situations, wearing medicinal contact lenses impregnated with drugs is prescribed.
- In advanced forms of the disease, steroid drops are required. This applies to severe inflammatory processes and the initial stage of scarring. When using these products, you should strictly adhere to the dosage prescribed by a specialist.
Note! Maintenance therapy is also required, which is aimed at taking vitamins and other beneficial substances. Because their deficiency provokes the active development of the disease. Serious complications can result from this.
The marginal form is one of the most serious diseases, which is difficult to treat. But if you follow all the doctor’s prescriptions, you can achieve positive dynamics of recovery.
Treatment
Having confirmed the diagnosis of viral keratitis, it is treated in a complex manner.
Medicines
Therapeutic methods are aimed at fighting infection, providing immunostimulation, and activating the cornea’s ability to regenerate.
- To combat the virus, eye drops or injections are prescribed: Interferon, Deoxyribonuclease, Poludan.
- Special ointments are placed behind the eyelid: Acyclovir, Tebrofenovaya, Bonoforovaya, Oxalinovaya.
- For immunostimulation, the drug Levamisole and immunoglobulin injections are used.
- For pain relief the following are used: Novocain, Analgin.
- During more severe forms of illness, large doses of antiviral tablets are prescribed.
- To prevent the resumption of an infectious disease with viral keratitis, antiseptic drops (Sulfacil) and ointments (Tetracycline, Erythromycin) are prescribed.
Other procedures
- Therapeutic methods also include the use of physiotherapy (electrophoresis, magnetophoresis).
- For herpetic keratitis, in case of ulcers, the use of cryoapplication and laser coagulation is indicated.
Surgery
If therapeutic treatment does not produce results and the disease continues to progress, the prognosis is not favorable, the following surgical methods are recommended:
- scraping operation;
- keratoplasty.
Scraping operation
Indicated in cases of superficial keratitis. It consists of removing the diseased epithelial layer of the cornea with surgical instruments.
The occurrence of keratitis and its prevention
With keratitis, its further course is determined by the localization of the pathology and how deep in the cornea its focus is located. If therapy is started on time, the maximum that remains from superficial infiltrates is a slight clouding, which has almost no effect on vision. But deep keratitis or an ulcer, and most of all this concerns pathology located in the central and paracentral part of the cornea, can greatly damage vision. This happens because this disease causes severe clouding and scarring.
Deep diffuse keratitis
In order to prevent this pathology, eye injuries and microtraumas should be avoided. And this means:
- carefully follow safety precautions during construction and production;
- scrupulously follow all rules for using contact lenses;
- avoid intoxication and eye burns from chemicals, including household ones;
- promptly identify and treat all eye pathologies;
- in case of problems with immunity, solve them as quickly as possible;
- As soon as there is even the slightest suspicion of keratitis, consult a doctor.
To avoid the occurrence of keratitis, it is important to follow safety precautions while working and avoid getting foreign objects into your eyes.
For keratitis, therapy must be started quickly. Otherwise, the cornea may perforate and infection may enter the eye. As a result, very severe infectious inflammation begins to develop. The worst thing is if keratitis is caused by herpes viruses: this type is prone to relapses, affects deeper, and also leaves large scars. The latter can even cause blindness.
Primary herpetic keratitis