The environmental situation in the world, unfortunately, is worsening every year, and therefore the number of people susceptible to allergies is growing. According to statistics, about a quarter of the world's population suffers from allergic rhinitis, which often provokes the development of bronchial asthma.
Allergic rhinitis (hay fever) is an inflammation of the nasal mucosa caused by allergens. In childhood, it causes the development of adenoids, otitis, sinusitis, and throat diseases. Patients do not always take the disease seriously, despite severe symptoms that impair performance and quality of life in general. Many people treat themselves, which often only aggravates the inflammatory process. Let's figure out how serious this disease is and what to do if symptoms of hay fever appear.
Causes
This disease was first discussed in 1819 in England, but at that time doctors assumed that hay fever in patients was associated with hay, and not with seasonal flowering of plants. Nowadays, this disease is one of the leading in allergology, as it is recorded in 24% of the world's population.
Hay fever is an allergic disease that is predominantly genetic in nature, that is, in most cases it is passed on from generation to generation. This pathology rarely develops in a child at an early age, but as they grow older, the first symptoms of the disease appear, and by the age of 14 an allergist can diagnose true hay fever.
The disease is caused by the smallest pollen of pollinated plants. These can be various trees, shrubs, weeds, flowers - there are at least 50 species in total. Pollen is usually carried by the wind over long distances, and less often by insects.
During flowering, not only in the spring months, but also in summer, and even in autumn until October, there is a lot of pollen in the environment.
Most of it is in the air on dry and windy days. During rainy and cold weather, the concentration of plant pollen in the environment sharply decreases, and it itself descends closer to the soil.
Let's look at the table at what time and on what plants hay fever of the allergic seasonal type can develop.
| Flowering period | Plant name |
| End of April – May | Oak, ash, birch |
| Mid-May – mid-June | Pine, spruce |
| Late May – mid July | Rye, wheatgrass and many others |
| End of June – beginning of July | Linden |
| June – mid-July | Plantain, buckwheat |
| July – mid-August | Nettle |
| End of July – October | Wormwood, quinoa |
Less commonly, allergic hay fever is caused by fungal mold spores; in this case, the disease will have a year-round nature.
Hay fever is a seasonal disease
Hay fever (from Latin pollinis - dust, pollen) pollen allergy, hay runny nose, chronic allergic disease caused by plant pollen and manifested by allergic inflammation of the mucous membranes of the respiratory tract, mainly the nose (seasonal runny nose) and eyes (conjunctivitis). Hay fever is one of the most common allergic diseases in children. They affect from 4.8 to 11.8% of children. And although a child may develop a pollen allergy as early as the second year of life, the disease often remains undiagnosed.
Back to contents
Causes
The development of hay fever is determined by sensitization - an increase in the body's sensitivity to the effects of any environmental factor, in this case to plant pollen, and depends on what plants grow in a given climatic zone. In central Russia there are three main flowering periods:
- spring - April-May: pollen from trees (birch, alder, oak, hazel, etc.) is present in the air;
- summer - June-July; in the air - pollen of cereal grasses (bluegrass, wheatgrass, fescue, hedgehog, foxtail, timothy, etc.);
- late summer, or summer-autumn, associated with the flowering of asteraceae and goosefoot plants (wormwood, quinoa, ragweed).
The pollen of these plants is widespread in our region. Its dimensions are extremely small - from 10 to 50 microns. It is released in huge quantities and is easily carried by the wind.
In the occurrence and development of allergic reactions, heredity plays an important role - the transmission from parents to the child of genes responsible for a predisposition to allergies. If only the mother suffers from hay fever, the gene is transmitted in 25% of cases, if the father and mother - in 50%.
Back to contents
Development
The mechanism for the development of allergic reactions in a child predisposed to them can be started at any age. Pollen enters the body through the respiratory tract or eyes and settles on the mucous membrane of these organs. In order for an allergy to develop, negligible doses of pollen are enough.
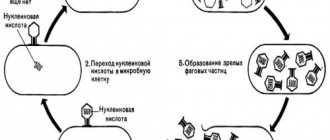
First, the body undergoes a process of recognition of the allergen by cells of the immune system and the production of protective substances (antibodies) against this foreign agent - the so-called sensitization phase. Outwardly, it does not manifest itself in any way, and a lot of time can pass from the moment of first contact with pollen until signs of the disease develop. For example, last year the child did not react to flowering plants, but pollen entered the body. And this spring, with the first buds opening, the baby had a second encounter with the allergen, which is why the cells of his immune system released specific substances (histamine, cytokines, etc.) that cause allergies and inflammation of the mucous membranes of the respiratory tract.
Hay fever developed. This is called the resolution or manifestation phase of the disease.
Back to contents
Symptoms
This disease has a clear seasonality, repeating from year to year and coinciding with the flowering period of certain plants. Symptoms of hay fever are most intense in the morning hours during the period of maximum pollen concentration in the air.
Allergic conjunctivitis1 appears (lacrimation, photophobia, severe redness of the mucous membrane, severe itching and swelling of the eyelids, a feeling of sand in the eyes), combined with an allergic runny nose (itching in the nose, impaired nasal breathing, copious liquid transparent nasal discharge, bouts of sneezing - from 10 up to 30 sneezes in a row).
The child breathes through his mouth, wrinkles his nose, rubs it with his palm, causing a transverse wrinkle to appear on it.
Damage to the nasal mucosa is usually bilateral. Swelling of the mucous membrane leads to decreased hearing, sense of smell, and headaches. Unlike acute respiratory viral infection (ARVI), with hay fever, fever and weakness are rarely observed, there is no sharp sore throat, redness, and enlarged lymph nodes (ear, submandibular, etc.) are rarely noted.
However, if at this moment the baby gets sick with ARVI, the signs of allergic rhinitis will only intensify, the recovery period will be delayed and the effect of antiallergic drugs will decrease.
A severe manifestation of hay fever is bronchial asthma2, usually combined with allergic runny nose (rhinitis) and allergic conjunctivitis.
Signs of pollen asthma are typical for asthma in general: attacks of suffocation, wheezing, wheezing, audible even at a distance, dry cough. 1Conjunctivitis is an inflammation of the mucous membrane covering the back surface of the eyelids and the front surface of the eyeball. 2Bronchial asthma is a chronic infectious-allergic inflammatory disease of the respiratory tract that occurs with attacks of suffocation.
The above-mentioned manifestations of hay fever may include headache, weakness, sweating, drowsiness, irritability and tearfulness, chills, fever, and increased fatigue.
Back to contents
Diagnostics
If you suspect an allergic disease in a child, first of all you should contact a pediatrician to rule out diseases that are similar in manifestations, but not allergic (ARVI, inflammation of the bronchi - bronchitis).
In case of an allergic disease, it is better to be examined and treated by an allergist-immunologist in a regional or large multidisciplinary children's medical institution.
Diagnosis of the disease consists of two stages. The first stage includes a thorough survey of parents about the child’s development, illnesses he has suffered, etc., then an examination of the child himself, laboratory methods for examining his blood, nasal mucus, etc. The second stage is identifying the allergen, in this case a plant. It is best to carry it out in winter, after treatment and reduction (or absence of signs) of the disease. At this time, tests are carried out with allergenic substances, the content of specific protective proteins of the immune system (class E immunoglobulins) in the blood is determined.
All allergy testing methods can be performed on an outpatient basis. Admission to hospital is only required in case of an emergency, such as a severe attack of bronchial asthma.
Back to contents
Allergen tests
The simplest and most accessible method of identifying an allergen are prick tests1 and their variant in the form of a prick test.
They are carried out only in winter, no earlier than ten days after the end of taking antiallergic drugs. 1Scarification - from. lat. scarification - scratching, cutting.
The technique is as follows: drops of various industrially prepared allergens are applied to the hands (forearms), and scratches or injections are made. The foreign substance enters the body through damaged skin, and after 20 minutes doctors assess the size of the blisters that have formed at the site of the scratches. The “culprit” allergen will cause the largest blister to form.
Such tests are only possible for children over 5 years of age, since young patients cannot sit still for 20 minutes while the tests last.
An alternative method for identifying the causative allergen is a blood test to determine the content of specific protective proteins of the immune system (class E immunoglobulins) produced in response to a particular pollen.
This method can be carried out year-round, regardless of the child’s condition and the treatment used for another disease, and is the only method that identifies the source of allergies in young children.
In general, it is recommended to carry out an allergy examination of a child with hay fever every 2-3 years, since the spectrum of allergens may change over time.
Back to contents
Treatment
To treat and prevent exacerbations of hay fever, the simplest, safest and most effective method is to eliminate the effect of identified allergens on the body and drug therapy. If the effectiveness of these actions is insufficient, then the issue of allergen-specific immunotherapy (ASIT) is considered.
Back to contents
Elimination (elimination) of the effect on the body of causally significant allergens (pollen)
During the flowering season, it is recommended to avoid walking outside the city, not to go outside in hot, windy weather, to take walks after rain, on cloudy days - when pollen is nailed to the ground - to clean and humidify the air in the apartment. To protect against pollen, it is recommended to put mesh over the window openings. They must be regularly moistened and periodically changed or washed.
When going outside, you should wear sunglasses.
After a walk, you need to rinse your eyes and nose with water and change your outerwear.
If possible, during the flowering period you should change the climate zone to one where flowering has already ended or has not yet begun.
During the flowering of a causally significant plant, you should adhere to a strict specific hypoallergenic diet1.
This is due to the fact that the fruits of related plant species can aggravate allergy symptoms associated with pollen. For example, during the flowering of trees (April-May), children who are allergic to their pollen are strictly prohibited from eating fruits (apples, pears, cherries), berries and their processed products (juices, preserves, jams) (see table. 1). It is also undesirable for children with hay fever to consume honey and medications containing herbal components. 1Hypoallergenic diet is a diet from which foods containing allergens, as well as pungent and irritating substances, are excluded.
Back to contents
Drug treatments
In the treatment of hay fever, medications are used that suppress allergic inflammation or reduce the severity of the external manifestations of the disease. They should be used daily throughout the flowering period, otherwise the disease will recur the next season and continue to progress.
Treatment usually begins with taking antiallergic (antihistamine) drugs. They act only against one of the substances responsible for the allergic reaction - histamine, which causes symptoms of the disease such as sneezing, itchy nose, and watery discharge from the nose. If swelling of the nasal mucosa and congestion occurs, vasoconstrictor medications are required. They constrict the vessels of the mucous membrane, reduce tissue swelling, and restore nasal breathing. They are used in the form of drops or as an aerosol, but no more than seven days in a row.
In cases where the above therapy is ineffective, hormonal drugs (glucocorticoids) are prescribed for local action in the form of aerosols (in the nose, eyes, bronchi), which have the ability to effectively suppress the process of inflammation and the production of substances responsible for the development of hay fever. In addition, topical hormonal drugs do not enter the bloodstream, and a short course of treatment is sufficient to improve the condition. Therefore, the risk of side effects in this case is minimal.
Possible options for intolerance to related plant allergens, foods and herbal preparations for hay fever.
| Plant foods | Herbal preparations | ||
| Birch | Hazel, alder, apple tree | Apples, cherries, peaches, plums, hazelnuts, carrots, celery, potatoes | Birch leaf, buds, sap, alder cones |
| Cereals | No | Food grains (oats, wheat, barley, etc.) sorrel | No |
| Sagebrush | Dahlia, chamomile, dandelion, sunflower | Citrus fruits, sunflower seeds, (oil, halva), chicory, honey | Wormwood, chamomile, string, calendula, coltsfoot |
| Quinoa | No | Beetroot, spinach | No |
| Ambrosia | Sunflower, dandelion | Melon, bananas, sunflower seeds (butter, halva) | No |
When taking hormones, antiallergic (antihistamine) drugs may be additionally prescribed, especially in cases where nasal congestion predominates.
To prevent exacerbation in advance (2-3 weeks before the expected flowering period), cromoglycates or antihistamines are prescribed, cromoglycates in the form of dry and wet aerosols into the eyes, nose, bronchi, which prevent the development of an allergic reaction by blocking body cells from which they could substances leading to allergies would be released. Therefore, they should be prescribed 10-15 days before the expected onset of an exacerbation, and used throughout the entire season (several months every day, several times a day). Once an exacerbation begins, they are ineffective.
The best preventative treatment for hay fever is ASIT.
Allergen-specific immunotherapy (ASIT). This is the only way to achieve a change in the body's response to an allergen. Therapy helps prevent the transition of mild forms of the disease to severe ones, reduces (or even completely eliminates) the need for medications. After its completion, it is possible to achieve long-term remission, which cannot be achieved by taking medications. But children can only do it from the age of seven.
This treatment method consists of introducing increasing doses of the “culprit” allergen into the child’s body. ASIT is carried out during the period of absence of manifestations of the disease (remission).
For pollen allergic rhinitis, ASIT begins in October-November and treatment ends two weeks before the start of flowering of the causal plants. The course is partly carried out in a hospital (2-3 allergen injections daily for 2-3 weeks), partly in a clinic (1-2 injections per week for 1-2 months).
Thus, we see that the treatment of hay fever is divided into treatment of exacerbation of the disease and prevention.
In case of exacerbation, antihistamines and local hormonal agents (in the nose, eyes) are first prescribed. Manifestations of bronchial asthma are treated by prescribing bronchodilators and local hormonal agents.
Back to contents
Complications
Sinusitis is inflammation of the mucous membrane of the maxillary sinuses. It can develop due to swelling of the nasal mucosa, which disrupts the flow of mucus from the sinuses and causes inflammation.
Internal otitis is an inflammation of the inner ear. It occurs due to swelling of the auditory tube connecting the nasal cavity with the tympanic cavity of the ear.
Purulent conjunctivitis can be a consequence of allergic conjunctivitis, in which the child rubs his eyes due to severe itching, which facilitates the penetration of infection.
Timely treatment and seasonal prevention of the underlying disease is the best way to prevent complications.
Today, medicine can at least effectively control and combat the manifestations of hay fever. And with proper treatment, your child will be able to forget about the disease for many years.
Nadezhda Snegova, immunologist-allergist, doctor of the highest category, senior researcher at the State Scientific Center of the Institute of Immunology of the Ministry of Health of Russia, Ph.D. Article from the June issue of the magazine
Symptoms of hay fever
The resulting disease in both children and adults is accompanied by inflammatory changes in the mucous membrane of the respiratory tract and eyes. Hay fever in children and adults has two groups of symptoms - specific and general.
Let's look at them in more detail in the table.
| Specific symptoms | General symptoms |
|
|
Before the onset of the disease, a person begins to complain of repeated sneezing associated with severe irritation of the nasal mucosa by pollen particles. Pollen irritates the mucous membrane, causing the development of a runny nose and swelling of the tissues of the respiratory tract. A runny nose is characterized by the appearance of copious mucous discharge. The duration of the disease is individual for each patient, as is the severity of the clinical symptoms of the pathological process.
For example, if some people complain only of a runny nose and itching of the nasal cavity, others experience every attack of hay fever as a serious allergy, suffering not only from respiratory signs of the disease, but also from a general feeling of poor health.
Sometimes the clinical picture of hay fever is complicated by a dry cough and attacks of suffocation. In this case, doctors talk about bronchial asthma. Also, the symptoms can be supplemented by skin manifestations in the form of allergic dermatosis, urticaria and Quincke's edema.
Having appeared once, the disease may go away within a few years, but most often a person will be forced to suffer from it all his life.
Reasons for the development of hay fever
Plant pollen acts as a strong allergen, and this is the main factor in the development of hay fever. Plants, during flowering of which hypersensitivity is noticed and the disease worsens, are divided into cereals, weeds and trees.
Pollen, which is visible only under a microscope, settles on the skin and gets into the mucous membranes of a person, causing allergic reactions in the body.
Time intervals for flowering plants:
- Mid to late spring: Trees are actively blooming in the midst of spring. Often, pollen from poplar, oak, hazel, birch, and alder is a strong allergen;
- June-July: During this period of time, plants of the grass family bloom. The most well-known allergens are bluegrass, grain crops - rye and wheat, as well as fescue, foxtail, wheatgrass, bluegrass, raygrass, and cocksfoot. Most often, hay fever affects people living on the outskirts of the city or rural residents;
- August-September: active antigens are weeds - quinoa, timothy, ragweed, wormwood.
Hay fever is felt depending on the weather. If it is windy and dry outside, the accumulation of pollen in the air increases, therefore, allergic symptoms intensify.
If the weather is rainy and damp, there is less pollen in the air, then hay fever does not manifest itself as a very pronounced clinical picture.
Article on the topic: Methods of treating allergies to cats, relevant in [y] year
Flowering calendar for patients with hay fever
Sensitization to a certain type of pollen varies from person to person: some people are allergic to ragweed, the most harmful herb for allergy sufferers, while others feel discomfort regarding increased sensitivity to sunflower and corn.
In addition, hay fever manifests itself under the following factors:
- hereditary feature, often on the mother’s side;
- serious damage to organs and tissues during childbirth, frequent bacterial, viral, parasitic infections;
- poor nutritional intake, smoking, alcohol abuse;
- climatic conditions;
- harmful working conditions.
Particular attention should be paid to herbal medicines. Young parents often treat their children with medications. For example, exudative diathesis is considered a type of allergic skin pathology.
To prevent the disease, the baby is bathed in a string or chamomile. Both Asteraceae plants contain large amounts of pollen. If a child is predisposed to allergies, his condition worsens.
Using a chamomile enema, washing the eyes with chamomile infusion, and drinking wormwood tea also lead to allergy symptoms. Honey, which contains accumulations of pollen grains, is a strong allergen, posing a danger to human health.
Sometimes, during the flowering of plants of the Aster family, cross-allergies develop. Allergy sufferers are contraindicated to eat nuts, mustard, drink champagne, and vermouth. These products pose a threat ranging from urticaria to anaphylactic shock and Quincke's edema.
Symptoms of hay fever
Diagnostics
If there is a suspicion that we are talking about a diagnosis such as hay fever, it is necessary, first of all, to seek advice from a therapist or allergist. This is necessary to exclude possible pathologies similar in symptoms to this disease, namely ARVI, bronchitis and pneumonia.
It is not difficult to distinguish a true allergic disease from a respiratory infection of viral or bacterial origin. The only difference between them is the presence of elevated body temperature. Hyperthermia is not typical for hay fever. The same cannot be said about infectious and inflammatory diseases of the respiratory tract. An experienced therapist or allergist will always be able to make the correct diagnosis and prescribe the necessary course of treatment depending on the patient’s well-being.
If a disease is diagnosed in a child, then during the initial examination, the doctor should ask the appropriate questions to his parents, clarifying the characteristics of the baby’s development and the history of his past diseases. Then, in children, as in adult patients, the specialist takes a swab from the nasal mucosa and sends it for laboratory blood testing.
After the disease is confirmed, it is necessary to determine which allergen is causing it. It is advisable to carry out allergy tests not during the period of exacerbation of the pathological process, but a little later - in the autumn or winter, when the irritating factor in the environment is completely absent. Against this background, determining the cause of the disease will be as accurate as possible.
Diagnosis of hay fever
Due to the fact that the symptoms of this disease appear seasonally, its diagnosis does not present any particular difficulties for specialists. Taking into account the exact period in which the attacks appeared, the doctor helps the patient to determine which flowering plant affects a person in this way. However, it should be noted that people who are susceptible to allergic reactions to plant pollen very rarely suffer from only one specific type of pollen.
When making a diagnosis, it is sometimes necessary to study the contents of nasal discharge. With hay fever, they contain eosinophils , as well as mast cells , that is, white blood cells that take part in allergic reactions. Also, to make a diagnosis and establish the type of pollen that provokes such a reaction, skin tests are taken.
Treatment of hay fever
Treatment of a disease such as hay fever is almost impossible, since the hypersensitivity of the immune system to plant allergens, once acquired, remains with the person for the rest of his life.
Thus, the only way to prevent the risk of developing acute symptoms of the disease is to completely avoid contact with plant pollen. Otherwise, treatment of hay fever in children and adults will be only symptomatic.
Children under 18 years of age with this disease should be closely monitored by a pediatrician and allergist. For adults, it is enough to see the latest specialist. If exacerbations develop in the form of crises and a serious deterioration in the general condition of the patient, intensive treatment of the pathological process is urgently carried out, the task of which is to eliminate swelling of the respiratory tract, relieve symptoms of inflammation from the visual organs, and improve the functionality of the respiratory organs.
The list of drug therapy includes the following medications:
ANTIHISTAMINES. These remedies for hay fever are prescribed with the aim of breaking the pathological chain that leads to the appearance of clinical signs of the disease. In the acute form of the pathology, antihistamines are introduced into the body by injection intramuscularly or intravenously. After the patient’s well-being returns to normal, the drugs are taken enterally in the form of tablets. The drugs in this group are Loratadine, Suprastin, Zyrtec, etc.
How to treat hay fever with antihistamines is determined by the attending physician - he prescribes the exact dosage and duration of taking the drug.
VASCONSTRUCTORS. Also necessary in the treatment of this disease. they belong to the group of alpha-adrenergic agonists, which have a direct effect on adrenergic receptors, concentrated in large quantities in the nasal cavity. The stimulating effect on adrenergic receptors leads to a narrowing of blood vessels and the elimination of swelling of the nasal mucosa. The therapeutic effect from the use of vasoconstrictors is observed within a few minutes. As a result, nasal congestion goes away, rhinorrhea is eliminated, and breathing becomes easier. The drugs in this group are Naphthyzin, Xylene, etc.
Clinical manifestations of conjunctivitis are relieved with the drug Albucid, which prevents the penetration of a secondary infection into the mucous membrane of the organs of vision and the occurrence of purulent complications. Less often, the prescription of hormonal agents is required - drops and ointments that relieve severe symptoms of the inflammatory process and itching, for example, Prednisolone ointment. If secondary infection cannot be avoided, antibacterial ointments are prescribed for local treatment, for example, Erythromycin.
During the period of remission, when the main signs of the pathological process subside, the specialist prescribes specific hyposensitization. This method allows not only to reduce further manifestations of an allergic disease, but also to answer the question - how to cure hay fever in full?
The basis of specific hyposensitization or the ASIT method is the introduction of minimal doses of an allergen into the human body in order to develop the adaptation of the immune system to them. Treatment is lengthy and expensive, usually lasting for several years, with breaks for the period of possible relapse of the disease.
The patient is given a minimum dose of the irritating factor by injection every day for several months; for hay fever, these are purified pollen allergens, which in small quantities are not capable of provoking the development of a violent allergic reaction in the body. During the course of therapy, resistance to introduced irritants is formed, as a result of which a person eventually stops responding to the allergen in the environment. With a positive effect from specific hyposensitization of the body, long-term remission or complete recovery occurs.
Treatment: how to cure with sprays and drops
The ICD-10 code for allergic rhinitis helps doctors find their way around the world. If the patient is abroad and feels unwell, but has medical documents, then the emergency doctor will be able to recognize the cause of this condition using the codes. Such codes are relevant for diabetes mellitus, bronchial asthma, heart pathologies and other dangerous diseases.
Allergic rhinitis is not easy to treat. The main task in this case is to exclude all contact with the allergen. But often the problem is that it is not possible to recognize the exact reason causing the reaction. If the allergen is found, there is a great chance to get rid of the problem forever. In other cases, symptomatic and anti-inflammatory therapy is selected.
Treatment of sinusitis at home
Scheme of step-by-step treatment of allergic rhinitis
Vasoconstrictors (naphazoline, oxymetazoline, otrivin), antihistamines (fenkarol, tavegil, telfast) and hormonal drugs are used. Cromones (cromosol, cromhexal), intranasal H1-blockers (allergodil, histimet spray), and antileukotriene drugs are also prescribed. Sometimes combined drugs are selected: clarinase, vibrocil, allergophthal, rhinopront, etc.
It is no coincidence that ICD-10 identifies allergic rhinitis as a separate disease. Having familiarized yourself with the drugs prescribed for the treatment of hay fever, you can safely talk about serious and long-term therapy, especially when the allergen has not been identified.
Self-treatment of allergic rhinitis most often only aggravates the situation and can lead to complications. There is only one algorithm: differential diagnosis plus competent treatment under the supervision of a specialist.
Diet
A diet for hay fever is a mandatory item, which includes comprehensive treatment. Allergists advise excluding or minimizing the following foods from your diet:
- cow's milk and products based on it, for example, sour cream, ice cream, etc. They should be temporarily replaced with products enriched with calcium and proteins, such as legumes and green vegetables;
- dishes made from premium flour - pasta, bread, pastries. They are temporarily replaced with rice, oatmeal, buckwheat and millet.
Changing the diet during an exacerbation of the disease in the spring can significantly improve a person’s well-being. In addition to the products listed above, you must avoid fast food and any bee products.
It is also important to pay attention to the definition of cross allergens. These are potential irritants to which no allergic reaction has previously occurred, but should not be eaten. If this is not possible, then you need to eat dishes from them after careful heat treatment, namely long-term stewing and boiling.
For example, if you are allergic to birch (the pollen of which is the most common cause of hay fever in the spring), it is undesirable to eat the fruits of fruit trees (plums, apricots, etc.) during its flowering season, or to indulge in herbs and seasonings.
In addition, it is necessary to take note that during the period of exacerbation of spring hay fever, you should avoid eating exotic and any unfamiliar foods.
When a difficult clinical situation develops, the patient is prescribed a hypoallergenic diet that excludes all types of allergens.
Classification of hay fever and their characteristics
At the moment, the classification according to EAACI//WAO, ARIA 2008 is considered the most correct and reliable, which distinguishes two forms of the disease - persistent and intermittent hay fever.
The first type is characterized by the presence of symptoms more than 4 days a week or more than 4 weeks a year, the second - less than 4 and 40, respectively.
There is a clinical classification:
- hay fever, leading rhinoconjunctival syndrome;
- hay fever with broncho-obstructive syndrome (or hay fever with an asthmatic component);
- hay fever with skin rashes and other dermal manifestations.
In addition, it is customary to distinguish the disease according to its severity:
- Easy. Manifestations of the disease do not interfere with physical activity and sleep, the need for antihistamines is minimal;
- Moderate weight. Manifestations of the disease force the allergy sufferer to change their lifestyle, may interfere with sleep, and the need for antihistamines is significant;
- Heavy. The usual routine of life and sleep is so disrupted that without antihistamines it is almost impossible.
Another classification feature is the stage. There are stages of exacerbation and remission of the disease.
Seasonality
Another name for hay fever is seasonal allergies. And it was not given in vain, since the disease is absolutely dependent on the season of the year.
Each plant has its own period of “activity”; at the same time, allergies worsen. Therefore, the term “year-round hay fever” is incorrect. But the name “spring hay fever” is quite appropriate, just like summer hay fever. Can hay fever occur in winter? As such, no, unless you visit a greenhouse.
Much more important is the phenomenon of cross-allergy. In this case, the reaction can be caused by some fruits and vegetables, the protein of which is similar in structure to pollen. However, the symptoms of this pathology are different.
In total, there are three periods when the disease can worsen:
- Spring . Starts in April and ends by the end of May. A reaction to pollen from wind-pollinated trees develops;
- Summer . It begins in June and ends at the end of July. The body reacts to grass pollen;
- Summer-autumn . Lasts from the end of July until October. This is the so-called “weedy” period.
It is important to understand that in different climatic conditions, the time intervals for flowering of certain plants vary greatly. Therefore, the timing of exacerbations may vary (range - up to two to three weeks).
To track when active dusting begins in a particular area, there is a special allergy calendar.
Seasonal triggers of hay fever by month
"Pollinosogenic" plants
There are countless plant species in the world—tens of thousands. However, only about 50 of them produce allergenic pollen. The most common disease is birch hay fever. In addition to this tree, the reaction can be caused by:
Photo: Blooming birch is one of the strongest triggers of hay fever
- alder;
- hazel (hazel);
- willow;
- oak;
- maple;
- chestnut;
- elm;
- poplar;
- Linden;
- quinoa;
- sagebrush;
- ragweed (in the middle of the 20th century there was even an outbreak of reaction to this plant in the Krasnodar region);
- Timothy grass;
- quinoa
– and this is not a complete list of allergens.
Dust forecast for Moscow from Pollen.club
Hay fever in children
Hay fever in children should be treated without fail; this disease cannot be left unattended. Otherwise, there is a high probability of deterioration of the clinical picture of the disease, serious weakening of the immune system, aggravation of the pathological process, up to the development of complications such as bronchial asthma. Cross-hypersensitivity of the body to other allergens may also occur.
For therapeutic purposes, children, as well as adults, are prescribed antiallergic medications, which not only relieve the symptomatic picture of the disease, but also prevent its further development.
In addition, it is recommended to pay attention to the child’s diet, minimizing as much as possible the amount of allergens from food products that can complicate an already difficult situation.
In order for the child to recover faster, it is advisable to create a favorable psychological microclimate at home, carry out wet cleaning daily, and prevent the development of the disease (we will talk about this below). After each stay outside, the child should take a shower with hypoallergenic detergents and thoroughly rinse the nasal cavity from possible allergens.
Symptoms and manifestations of hay fever
The most common manifestations are symptoms of allergic rhinitis, which is characterized by:
- prolonged sneezing - copious mucous discharge from the nose
- itching in the nose area
- soreness in the oropharynx
- mucus draining down the back of the throat (“postnasal drip”)
- nasal congestion
In most patients, rhinitis is combined with allergic conjunctivitis :
- redness and swelling of the mucous membranes of the eyes,
- itching of eyelids,
- photophobia,
- lacrimation,
- “sand in the eyes.”
Another manifestation of hay fever may be pollen bronchial asthma , when it appears:
- cough,
- labored breathing,
- “wheezing” and/or “wheezing” in the chest,
- suffocation.
Somewhat less frequently, with hay fever, itchy skin rashes (urticaria) or local swelling (Quincke's edema or angioedema) , individual manifestations of atopic dermatitis, are observed.
Treatment in pregnant women
With the onset of pregnancy, serious physiological changes occur in a woman’s body, leading to a decrease in immune defense. This is necessary so that the female body does not reject the developing fetus. Any disease, for example, hay fever during pregnancy, can interfere with physiological processes and cause various complications.
For example, an allergy to pollen can cause an expectant mother to experience infectious and inflammatory processes in the respiratory tract and associated organs (inflammation of the middle ear, tracheitis, contact dermatitis, headaches, convulsions).
It should be noted that hay fever, which worsened during pregnancy, can negatively affect the development of the baby and the pregnancy itself. Very often, a newborn child is diagnosed with various pathologies of an allergic nature.
To prevent and eliminate the clinical signs of hay fever, the expectant mother is prescribed the latest generation of antihistamines, for example, Telfast, Zyrtec, which not only successfully cope with their task, but also have minimal negative effects on the body of the pregnant woman and the developing fetus. Additionally, your doctor may prescribe nasal sprays, such as Cromohexal.
Differential diagnosis
Differential diagnosis of hay fever should be carried out with several diseases:
- all types of rhinitis (for example, vasomotor rhinitis or hay fever?);
- infectious diseases of the eye and respiratory tract.
The process of differential diagnosis is clearly described by the Federal Clinical Guidelines for Allergology (Russian Association of Allergologists and Clinical Immunologists, Moscow-2014). National guidelines recommend differentiating allergic rhinitis from vasomotor, infectious and eosinophilic rhinitis.
Unlike hay fever, all of the three types listed above appear more often in adulthood, in people without a history of allergies.
| Comparison points | Allergic rhinitis | Non-allergic rhinitis | ||
| Vasomotor | Infectious | Eosinophilic | ||
| Clinical picture | Seasonal | The clinical picture does not change after elimination of the allergen, there is no seasonality. | ||
| Nasal discharge | purulent, has a greenish-yellow color | |||
| Presence of eosinophils in the smear | No | No | ||
| Presence of eosinophils | increase 10% | No | No | increase of 30% or more |
| Presence of immunoglobulins in the blood | present | No | No | No |
In addition, in non-allergic diseases there are no immunoglobulins in the blood, skin tests and stress tests are negative, and they are not combined with conjunctivitis and do not respond to antihstamin therapy. Seasonal allergic rhinitis (hay fever) and allergic rhinitis are different in the absence of seasonality in the second case.
Prevention
Prevention of hay fever is a set of measures that will prevent the development of the disease and its complications. The main task of preventing this pathology, as well as other allergic diseases, is to exclude direct contact of a sick person with irritating factors, that is, plant pollen in this case.
Prevention of the disease can be primary and secondary.
Primary prevention is aimed at preventing the disease as a whole, that is, it is necessary for people who have never previously encountered symptoms of hay fever, but have a predisposition to it. Secondary prevention applies to persons already suffering from other allergic pathologies, as well as to people engaged in agriculture, beekeeping, gardening, and professional activities related to plant growing.
Primary prevention. Preventive measures are as follows:
- During pregnancy, a woman should minimize contact with pollen, refuse hazardous work in production, follow recommendations for a daily routine, and eat only high-quality foods.
- In childhood, it is important to protect a child from frequent colds and chronic infectious and inflammatory processes in the respiratory tract; this can be done by strengthening the body’s defenses.
Frequently ill children are at risk for hypersensitivity of the immune system to various irritants, including plant pollen.
- Reduce the negative impact of environmental factors that often provoke allergic diseases. These could be exhaust fumes, contact with chemicals, or household allergens such as pet hair.
Secondary prevention. Necessary for people who have previously encountered clinical manifestations of hay fever. The goal of secondary prevention is to prevent possible contact with plant allergens. As a rule, people who suffer from hay fever know exactly what irritant causes their body to become hypersensitive.
The rules of secondary prevention should be followed not only on the street, outside the home, but also at home and in the workplace. So they will be as follows:
- Daily ventilation of the home or work area and regular wet cleaning. During ventilation, it is recommended to cover window openings with damp gauze folded in several layers to prevent possible irritants from entering the room. Unfortunately, this practice is not always feasible in the workplace.
- In a house where an allergy sufferer lives, there should be a minimum of upholstered furniture and soft toys, and a complete absence of carpets. The room should be moderately spacious so that nothing interferes with high-quality cleaning and regular ventilation.
- Books and bedding, particularly feather-filled pillows and duvets, should be stored in an appropriate environment that minimizes the risk of spreading pollen and general dust. For example, books should be stored in tightly closed cabinets, and bedding in special sealed covers.
- It is prohibited to use industrial air fresheners, various aerosol deodorants, perfumes and other strong-smelling household chemicals in the environment of an allergy sufferer.
- You cannot have pets in a house where an allergy sufferer lives, since wool particles are a strong allergen that provokes increased sensitivity of the body to various kinds of irritants.
- During the off-season, the risk of developing the body's susceptibility to mold fungi, which also have pronounced allergic properties, increases. They prefer places of high humidity, so in the fight against the development of symptoms of an allergic disease, including hay fever, it is necessary to prevent the appearance of mold spores in the home.
- While on the street, a person must protect himself from the negative influence of the environment. For example, avoid second-hand smoke and exhaust fumes, tightly close the windows in your personal car while traveling.
- Wherever a person suffering from hay fever goes, it is important to protect the eyes from the risk of potential irritants coming into contact with the mucous membrane of the organs of vision. To do this you need to wear sunglasses.
- It is undesirable for people with hay fever to go to places with the highest concentration of plant pollen, namely, where there are the most plants - forests, fields, gardens.
- It is important before each season of flowering of plants (or a specific plant, if a person knows about his allergen), to carry out preventive preparation of the body with medications that reduce the susceptibility of the immune system to plant pollen. Most often these drugs are cromoglycates, for example Intal.
Prevention of hay fever
To prevent the development of hay fever during the flowering period, a number of simple rules should be followed. Thus, the patient should, if possible, stay at home until eleven o'clock in the morning. It is not recommended to go outdoors outside the city during this period. It is advisable to curtain the windows in the house with a very fine mesh and throw away all the dry bouquets. Before going outside, be sure to take sunglasses, and at home, after returning from the street, immediately wash the mucous membranes of your nose and eyes with clean water. People prone to allergies should not use cosmetics, shampoos, and soaps made from allergenic plants. Similarly, you should not eat food from these plants. Long before the start of the flowering season, you need to take a course of medications prescribed by your doctor.
Hay fever and military service
Will they be accepted into the army with hay fever? This question worries many young people of military age and their parents. The presence of allergies, in our case it is hay fever, is regulated by Article 85 “Schedule of Diseases”. We invite you to find out what this article says about this pathology.
Persons who suffer from food allergies to basic foods, confirmed by clinical examination, are examined under point “B”. For other types of allergies (hay fever, atopic dermatitis and others), the examination is carried out in accordance with the appropriate articles of the disease schedule, depending on the functional changes in the affected organs and systems.
Based on this, a conscript may be unfit for military service if he has two important conditions: 1. Food allergies.
2. Allergens are basic foods.
Hay fever cannot relate to these aspects.
An exception may be a pronounced form of the disease, which is a predisposing factor to the development of bronchial asthma. To confirm asthma, you must be examined by a pulmonologist. If asthma is documented, you can receive an exemption from conscription.
Thus, if status asthmaticus and respiratory failure are absent, a person suffering from seasonal hay fever is subject to conscription on a general basis. These rules apply to both countries, Russia and Ukraine.
Hay fever - what is it?
Hay fever disease: ICD 10 code – J30.1. Also called:
- allergic rhinitis;
- allergies caused by plant pollen;
- hay fever;
- seasonal allergies.
Hay fever (hay fever) is the name given to an immediate allergic reaction that manifests itself within a few minutes after pollen contacts the mucous membranes of the nose, eyes or respiratory tract. At the same time, many people with pollen allergies run the risk of being hypersensitive to the flowering of several plants at the same time.
The fundamental factor due to which allergic hay fever develops is considered to be disturbances in the functioning of the immune system.
Seasonal hay fever is divided into 3 types, depending on the period of pollination of all kinds of plants. There are spring, summer and autumn hay fever.
Allergy hay fever can occur at different times of the year, and in some cases, occur almost all year round, depending on the flowering time of individual plants.
As a rule, in the spring, from March to May, the first wave of allergies is caused by pollen from trees: birch, ash, elm, hazel, maple, spruce, alder, willow, oak, lilac, pine. And also flowers: coltsfoot, dandelion, etc.
In the summer, from June to August, allergens from nettle, hazel, poplar, sunflower, apple tree, etc. cause illness.
In the summer-autumn period from July to October, pollen allergens of weeds and cereal grasses are activated: wormwood, ragweed, wheatgrass, etc.
Please note that the flowering calendar for plants may vary depending on the area in which you live. In the southern regions, flowering begins much earlier than in the rest.
Who is at risk?
Some people are at risk, that is, they are more likely to develop hay fever from March to October, depending on the pollen that is not tolerated by the immune system of a particular organism:
- children of parents suffering from hay fever (this is a hereditary disease);
- living in cities with large populations (polluted air reduces immunity and increases the sensitivity of the respiratory organs);
- presence of bad habits;
- living in areas where many plants that cause hay fever grow;
- birth of allergenic plants during the flowering period.
Anatomy and physiology of the nose and paranasal sinuses
The nose is the first section of the upper respiratory tract.
There are three main parts of the nose:
- external (external) nose;
- nasal cavity;
- paranasal sinuses, which are connected to the nasal cavity by very small openings.
The external nose can be divided into:
- root;
- back;
- top;
- wings of the nose.
General structure:
- the back of the external nose smoothly passes into the upper part of the nose;
- the root of the nose is located in the upper part of the face and is separated from the forehead by the bridge of the nose;
- The lateral sections of the external nose are united by a median line and form the dorsum of the nose. While the lower parts of the lateral sections directly form the wings of the nose;
- The nostrils perform the function of passing and removing air. In the middle, the nostrils are separated from each other by a movable partition;
- First, the air passes through the nasal cavity. This is the distance between the cranial fossa (anterior) and the oral cavity;
- the nasal cavity consists of the left and right halves, which are separated by the nasal septum and connected to the external environment through the nostrils;
- the left and right parts of the nasal cavity are divided by the nasal concha (lower, middle and upper) into curved nasal passages - also, respectively, lower, middle and upper;
- small openings are inherent in the upper and middle nasal passages. With their help, the nasal cavity connects with the paranasal sinuses. In the lower nasal passage there is the mouth of the lacrimal canal. Tears enter the nasal cavity through this channel.
There are three components of the nasal cavity:
- vestibule;
- respiratory part;
- olfactory part.
In humans, there are four groups of paranasal sinuses.
The names of the sinuses correspond to their location in the body:
- maxillary sinus;
- frontal sinus;
- paired lattice labyrinth;
- sphenoid sinus.
To date, there is no common point of view regarding the functions performed by the paranasal sinuses.
The most reliable possible functions can be considered:
- reduction in the mass of the skull (anterior), especially the facial bones;
- increased vocal resonance;
- softening shocks in case of injuries;
- ensuring insulation of the eyes and roots of teeth from rapid temperature changes in the nasal cavity during breathing;
- humidification heating the air that is inhaled due to slow air flow.
Complications and prevention
Without treatment or insufficient treatment, complications may develop. The most common of them are bacterial conjunctivitis and keratoconjunctivitis. The first means inflammation of the mucous membrane of the eyes, and the second means inflammation of the cornea joins this process. The most severe complication of hay fever is anaphylactic shock, which can be fatal.
To prevent exacerbation of hay fever, it is recommended to observe the following measures:
- avoiding contact with the allergen;
- timely use of medications during the season of hay fever development;
- preparing the body by reducing sensitization.
Those suffering from hay fever must follow a special diet, which involves excluding from the diet various foods, fruits and vegetables, to the pollen of which they become allergic. Such patients are advised to switch to foods containing low levels of allergens. These are, for example, fermented milk products, stewed or boiled meat, dried fruits.
Treatment
Treatment of hay fever involves two forms: alleviating the condition during exacerbation and preventing relapses during remission. In the first case, medication is required.
Here are the antihistamines prescribed for hay fever:
- Antihistamine tablets. There are first and second generations. The former cause drowsiness, apathy, and require taking several times a day. The latter, as a rule, have a prolonged action (one tablet per day is enough) and do not have side symptoms. However, in any case, they should not be abused.
- Local medications. This group includes drops - eye and nasal, as well as gels. These drugs may be antihistamines. More often they are made on the basis of cromoglycic acid, a powerful antiallergic agent. Additionally, vasoconstrictors and other drugs may be prescribed.
- Local glucocorticoids. These are hormonal drugs - nasal sprays. They relieve inflammation well, while being poorly absorbed into the blood. However, hormonal drugs are addictive, so they are used last.
Allergen-specific immunotherapy (ASIT) allows you to get rid of allergy symptoms for many years. After the doctor uses tests to determine the main allergen, he begins to regularly introduce it in safe doses into the patient’s body.
This is done so that the immune system gets used to the presence of this substance and stops reacting to it. Treatment is long, from several months or more. However, after it is carried out, you can forget about the manifestations of allergies for years. Important: such treatment is carried out only outside the period of exacerbation.
Symptoms of hay fever
In general, hay fever can manifest itself with a whole range of symptoms. Therefore, it is not always possible to immediately determine that this is the effect of an irritant on the body. It should be understood that an allergy to pollen can manifest itself:
- Hyperthermia;
- Rhinitis;
- Urticaria;
- Atopic or contact dermatitis;
- Difficulty breathing;
- Quincke's edema;
- Conjunctivitis;
- Cystitis;
- Inflammation of the external genital organs.
At the same time, pollen intoxication manifests itself in the form of fatigue, decreased appetite, increased irritability, migraine attacks, and depression.
If the patient swallows pollen, gastrointestinal symptoms may also appear in the form of vomiting, nausea and severe pain in the abdominal area.
Symptoms and manifestations of hay fever
Exercises for hay fever
To achieve a faster effect in the treatment of allergies, as well as to prevent relapses, you can perform gymnastics and breathing exercises.
- Close one nostril with your finger and exhale through the other. Legs bent at right angles, feet firmly on the floor, back straight, abdominal breathing. Do the exercise, alternating nostrils, for 7-10 minutes.
- While standing, take a deep, calm breath for a count of 4. Hold your breath and, after counting to 16, exhale calmly. You need to start the exercise with 10 repetitions, gradually increasing to 20.
Breathing exercises require an individual approach to the patient, taking into account the general condition of his body and the characteristics of the course of the disease. Our doctors create an individual program for each patient.
How to identify hay fever? Diagnostics
Diagnosis of hay fever occurs in several stages:
1
The history of a small patient is studied. To do this, the child himself and his parents are interviewed. They focus on the connection of the disease with the time of year and the flowering season of dust plants. The child is examined by various specialists: ENT, ophthalmologist and others.
The probability of hay fever is high with the following anamnestic data:
- allergies in parents and close relatives;
- the disease and its symptoms occur once a year during the flowering period of plants;
- at other times there are no signs of the disease.
Based on the data obtained, a diagnosis of hay fever is suggested .
2
Establishing a connection between the disease and the causative allergen. For this purpose, various methods are used:
- skin tests. Do not carry out during the period of exacerbation of the disease and in children under 3 years of age. Before the study, the patient should not take hormonal or antihistamine medications.
- determination of specific immunoglobulin E in blood serum;
- immunoblotting. The air panel includes the most common pollen allergens, such as birch, alder, poplar, ragweed, wormwood, etc.
- provocative tests. They are used only in hospital settings for patients with complex diagnoses. Practically not used in childhood.
3
At the last stage, the doctor assesses the severity of the disease (mild, moderate or severe) and develops an individual treatment regimen for the patient separately for the period of exacerbation and remission.
to the content?
How does hay fever develop?
Plant pollen settles on the mucous membranes of the eyes, nose, and mouth, comes into contact with the skin, and penetrates the bronchi along with the inhaled air.
Plant pollen is able to penetrate the body through mucous membranes, which is due to the presence of the so-called “permeability factor” in the pollen composition.
In addition, the penetration of pollen is facilitated by disruption of the protective functions of the upper respiratory tract, which normally should act as a barrier. Such security violations are:
- Violation of the protective functions of the body's immune cells, granulocytes and macrophages;
- Lack of secretory immunoglobulin A;
- Insufficient production of a substance that reduces the activity of the “permeability factor” of plant pollen;
- Damage to the functions of the ciliated epithelium of the respiratory system, which can occur due to exposure to the “permeability factor” of plant pollen, chemical air pollutants (for example, in people living in unfavorable environmental conditions), and previous viral respiratory diseases
Most of these protection defects can be inherited.
At the point of contact of the mucous membranes with pollen, a local allergic reaction develops. Particles of allergens that can dissolve in water penetrate the epithelium of the mucous membranes, entering the blood and lymph, as a result of which sensitization (the body's susceptibility to allergens) increases and the allergy begins to affect tissues and organs that are not directly in contact with pollen, for example, the lower parts of the organs respiration, digestive organs, kidneys, etc. Pollen allergens that penetrate the blood trigger the immunological phase of the mechanism for the development of hay fever, during which an abnormal response of the human immune system to the penetration of pollen allergens is formed, which within 10-20 minutes after contact with pollen can manifest itself as swelling of the mucous membranes, increased mucus production, spasm smooth muscles (for example, spasm of bronchial smooth muscles).
How to prevent hay fever?
Preventive measures provide good results for allergic hay fever. They are very simple, so everyone can follow them:
- minimize contact with allergens, which are pollen;
- try to give up perfumes and cosmetics during the hay fever season;
- go on a diet excluding honey, chocolate, citrus fruits and seasonal fruits and vegetables;
- Before the onset of hay fever, perform immunotherapy with multivitamin complexes to strengthen the immune system.
Regular rinsing of the nasal sinuses with a pharmaceutical saline solution or ordinary boiled water also helps a lot.
Efficacy of various groups of drugs on AR symptoms
| Drug groups | AR symptoms | ||||
| H1 blockers | |||||
| inside | ++ | ++ | + | +++ | ++ |
| intranasally | ++ | ++ | + | ++ | 0 |
| GCS intranasally | +++ | +++ | ++ | ++ | ++ |
| Cromony | |||||
| intranasally | + | + | + | + | 0 |
| inside | 0 | 0 | 0 | 0 | ++ |
| Decongestants | |||||
| intranasally | 0 | 0 | +++ | 0 | 0 |
| inside | 0 | 0 | + | 0 | 0 |
| Anticholinergics intranasally | 0 | ++ | 0 | 0 | 0 |
| Leukotriene receptor antagonists orally | 0 | + | ++ | 0 | ++ |
Modern approaches to the treatment of allergic rhinitis are reflected in the international consensus (ARIA 2001; ARIA 2008 Update; ARIA 2010 Revision) - a consensus document created in collaboration with WHO (Fig. 3).
Rice. 3. Algorithm for the treatment of allergic rhinitis
Topical corticosteroid drugs are usually used in the treatment of patients with moderate and severe forms of AR. They, having a pronounced anti-inflammatory effect, penetrate the cell membrane, suppress the synthesis of histamine by mast cells and reduce the permeability of vascular walls. Modern intranasal glucocorticosteroid drugs (GCS) have virtually no systemic effect, which is explained by their rapid metabolic inactivation in the liver [5]. These medications are available in the form of nasal sprays. Intranasal corticosteroids are characterized by a relatively slow onset of action - the maximum effect develops after several days or weeks, so long-term use is necessary - for 4-6 months. Modern intranasal corticosteroids, as a rule, do not cause atrophy of the nasal mucosa. Regular prophylactic use of topical corticosteroids reduces nasal congestion, rhinorrhea, sneezing and itching, which has been confirmed by a number of placebo-controlled clinical trials [4].
In patients with mild to moderate AR, it is advisable to use topical antihistamines that have the necessary therapeutic effect and are free of systemic side effects [4]. Local antihistamines - azelastine, dimethindene/phenylephrine, levocabastine are available as a nasal spray and eye drops. Their advantages: rapid onset of effect (10-15 minutes) and good tolerability. Azelastine and levocabastine are used 2 times a day after toileting the nasal cavity. Dimetindene/phenylephrine - 3-4 times a day.
Regardless of the severity of allergic rhinitis, all patients are prescribed systemic antihistamines (H1-histamine receptor blockers). For mild AR, they can be used as monotherapy; for moderate and severe AR, they can be used in combination with cromoglycates or topical glucocorticosteroids. The widespread use of antihistamines as antiallergic drugs is explained by the critical role of histamine in the pathogenesis of most symptoms of allergic diseases [3]. Although the clinical manifestations of AR are caused by one or another set of allergy mediators, only histamine, through stimulation of H1 receptors, is involved in almost all symptoms. The only exception is the late phase of the allergic response - the maintenance of allergic inflammation and the associated hyperreactivity of the mucous membrane.
Regardless of the severity of allergic rhinitis, all patients are prescribed systemic antihistamines (H1-histamine receptor blockers)
According to the classification adopted by the European Academy of Allergy and Clinical Immunology (EAACI, 2003), antihistamines are usually divided into two large groups: classical H1 antagonists of the first generation and highly selective inverse agonists of H1 receptors of the second generation [8].
Most first generation antihistamines were synthesized in the middle of the last century, but are still used to this day.
The features of this group of drugs include a short duration of therapeutic action (1.5-6.0 hours) and incomplete binding to H1 receptors (30%), which necessitates the use of high therapeutic doses and a high frequency of administration of these drugs, as well as rapid development of tachyphylaxis to them. First generation drugs are highly lipophilic and therefore easily penetrate the blood-brain barrier, causing drowsiness, fatigue, dizziness, headache, impaired coordination of movements, decreased attention and memory. All these effects are enhanced by combined use of antihypertensive drugs with alcohol or sedatives.
Another disadvantage of first generation AGPs is their low selectivity of action: in addition to H1-histamine receptors, they block M-cholinergic receptors, α-adrenergic receptors, serotonin and bradykinin receptors. Due to the blockade of M-cholinergic receptors, they increase the viscosity of mucus, which adversely affects sputum separation, and increase bronchospasm, therefore they are contraindicated in patients with bronchial asthma. In addition, first-generation antihypertensive drugs can increase intraocular pressure, interfere with urination, increase heart rate, cause stomach pain, constipation, nausea, vomiting, and increase body weight. In this regard, these drugs have a number of serious restrictions for use in patients with glaucoma, benign prostatic hyperplasia, cardiovascular pathology, etc. [12].
Due to the unfavorable safety profile of first generation antihistamines, ARIA does not recommend their use for the treatment of patients with allergic rhinitis, giving preference to second generation drugs. This group of drugs includes highly selective inverse agonists of H1 receptors (cetirizine, loratadine, desloratadine, levocetirizine, fexofenadine, arivastine, azelastine, ebastine, rupatadine), effective in relieving symptoms such as itching, sneezing, rhinorrhea, and, to a lesser extent, nasal congestion , as well as accompanying symptoms of conjunctivitis and skin manifestations of allergies. Second generation drugs have the following advantages over classical antihistamines: very high affinity for H1 receptors; high safety profile due to high specificity and lack of penetration through the BBB; long-term action and absence of tachyphylaxis [3].
A special place among them belongs to cetirizine. The drug currently remains a kind of standard of antihistamine and antiallergic action, used for comparison in the development of new antihistamines and antiallergic drugs [13]. There is a reasonable opinion that cetirizine is one of the most effective H1-antihistamines. It is supported by a large number of clinical trials, exceeding the number of studies with other antihistamines. This drug is preferred for patients who respond poorly to the therapeutic effects of other antihistamines [13].
In comparative studies of the efficacy and safety of cetirizine and loratadine in the treatment of seasonal allergic rhinitis, the mean reduction in overall symptom severity was significantly greater for cetirizine compared with loratadine and placebo. In the group receiving cetirizine, the antihistamine effect appeared earlier and its duration was significantly longer [14].
In comparative placebo-controlled, randomized, double-blind trials with the replication of exacerbation of seasonal allergic rhinoconjunctivitis with ragweed pollen in an exposure chamber, it was shown that cetirizine at a standard therapeutic dose (10 mg) provides a more pronounced suppression of rhinitis symptoms than fexofenadine (180 mg) at 12 hours and throughout the entire period between the 5th and 12th hour after taking the therapeutic dose of the drug [15].
Cetirizine is preferred for patients who do not respond well to other antihistamines.
Currently, one of the most effective, safe and cost-effective systemic antihistamines is Cetrin (cetirizine). Cetrin is a competitive histamine antagonist, a metabolite of hydroxyzine, and selectively blocks H1 receptors. In addition to the antihistamine effect, cetirizine has an additional anti-inflammatory effect:
- inhibits the chemotaxis of eosinophils and neutrophil granulocytes;
- reduces the “squeezing out” of adhesive molecules onto the eosinophil membrane;
- inhibits cell migration to the allergic reaction zone by inhibiting the expression of ICAM1 on endothelial cells;
- inhibits IgE-dependent platelet activation and the release of cytotoxic mediators.
Cetrin begins to act within 20 minutes. The duration of the effect is more than 24 hours. After a course of treatment, the effect lasts for 3 days. Cetrin is well tolerated: it practically does not cause a sedative effect, which allows it to be used by patients whose professions involve increased concentration. Cetrin does not block M-cholinergic receptors, so it can be used to treat patients with concomitant bronchial asthma, prostate adenoma, and glaucoma.
In addition, Cetrin does not disrupt the rheological properties of mucus, which is important for patients with productive cough and acute rhinosinusitis. The drug does not have a cardiotoxic effect, does not interact with other drugs, and is not metabolized in the liver. Therefore, if necessary, it can be prescribed simultaneously with systemic antibiotics, systemic corticosteroids and other drugs that undergo metabolism with the participation of cytochrome P450.
Cetrin has a low probability of developing tolerance to the drug, which allows it to be used for a long time. It is used once a day, which increases compliance with therapy.
Cetrin has proven full bioequivalence with the original cetirizine, while it compares favorably with its greater economic accessibility.
Thus, the main principles of treatment for hay fever are allergen elimination, ASIT, and pharmacotherapy. ASIT is prescribed and carried out only by an allergist, and therefore all patients with pollen allergies must be registered at the allergology office. Of the drug treatments for hay fever, in particular allergic rhinitis, the use of Cetrin (cetirizine) is one of the most effective and safe among other inverse agonists of H1-histamine receptors.
Bibliography:
- Goryachkina L. A., Peredkova E. V., Bzhedugova E. R. Treatment of hay fever. Attending Physician 2004, 3: 1-6.
- Guseva E.D., Fayzullina R.M. Features of mucosal immunity in children with allergic rhinitis. Bulletin of Otorhinolaryngology, 2012, 6: 33-35.
- Gushchin I.S. Allergic inflammation and its pharmacological control. M.: Farmarus Print, 1998.
- Zaitseva O.V. Approaches to the diagnosis and treatment of allergic rhinitis. Bulletin of Otorhinolaryngology, 2011, 5: 62.
- Ilyina N.I., Fedenko E.S., Kurbacheva O.M. Allergic rhinitis. A manual for general practitioners and pharmacists. Russian Allergological Journal, 2004, 3: 12-13.
- Kolenchukova O.A., Ignatova I.A., Smirnova S.V., Kapustina T.A., Kin T.I. Features of the microflora of the nasal mucosa in patients with allergic rhinosinusitis. Bulletin of Otorhinolaryngology, 2008, 5: 33-35.
- Kudaibergenova S.F. Informativeness of the cytological method of research in allergic rhinitis with concomitant pathology from the ENT organs. Bulletin of Otorhinolaryngology, 2010, 3: 37.
- Lopatin A.S., Latysheva E.N. Levocetirizine in the treatment of allergic rhinitis. Bulletin of Otorhinolaryngology, 2010, 4: 98.
- Lopatin A.S. Rhinitis. M.: Litterra, 2010.
- Lopatin A.S., Gushchin I.S., Emelyanov A.V. and others. Clinical recommendations for the diagnosis and treatment of allergic rhinitis. Consilium medicum, 2001, 3(9): 33-34.
- Crobach M, Hermans J et al. Health Care, 1996, 14(2): 47.
- N.S. Tataurshchikova. Modern aspects of the use of antihistamines in the practice of a general practitioner. Pharmateka, 2011, 11.
- Gushchin I.S. “Cetirizine is a standard H1 antihistamine.” Guidelines. M., 2008.
- Day JH, Briscoe MP, Rafeiro E et al. Comparative efficacy of cetirizine and fexofenadine for seasonal allergic rhinitis, 5-12 hours postdose, in the environmental exposure unit. Allergy Asthma Proc, 2005,
- Russian Association of Allergists and Clinical Immunologists. Federal clinical guidelines for the diagnosis and treatment of allergic rhinitis. M., 2013.
Risk factors
As you know, hay fever most often occurs in women. But among residents of rural areas it is quite rare. The number of cases may be influenced by geographic, environmental and climatic factors.
An important role in the formation of hay fever is played by hereditary predisposition. If the parents suffer from allergies, the percentage of probability that the child will also have an allergy is about 50%, if one parent has an allergy, then 25%, and if the allergy does not affect the parents, the child still has a risk of illness, this is - 10%.
The risk of disease increases if the child constantly stays in dusty and polluted rooms, has poor nutrition, or very often suffers from viral diseases.