Granuloma annulare is one of the complex diseases, the cause of which has not been fully elucidated. This is a chronic skin disease characterized by the appearance of small, dense, raised nodules that form a ring with normal or slightly sunken skin in the center.
Characteristics of the disease
Granuloma annulare is a complex type of skin pathology that is still under study. It is characterized by rashes in the form of nodules or compactions of different sizes. The disease may manifest itself without pain, but as it develops, the pain progresses or disappears completely. The nature of the pathology is benign with a chronic course.
The shape of skin rashes can be round or oval, resembling nodules. When formed, compactions appear in a chaotic manner. After some time, the rashes may disappear on their own.
A papule occurs on any part of the body. In medical practice, granulomas are more often diagnosed on the face, in the area of the hand, finger, elbow and on the leg (foot and knees). A person may not notice a suspicious spot for a long period of time.
During the process of growth and maturation, the compaction accumulates collagen, which leads to inflammation inside the diseased tissues and forms a kind of ring of nodules. Pathomorphology calls this manifestation “granuloma,” which gives the name of the pathology – granuloma annulare. An unknown nodule on the skin often does not cause discomfort - there is no itching or burning, and no painful sensations are observed either.
Granuloma annulare
The ICD-10 pathology code is L92.0 “Annular granuloma.” The disease can occur in adults and children. Women and small children suffer from skin rashes more often.
Concept and characteristics
Granuloma annulare in children - photo:
Granuloma annulare is one of the rare skin diseases. The pathology is characterized by a benign course . Dense nodules on the skin form a characteristic ring.
Such formations can be localized on any part of the child’s body, but most often symptoms appear on the scalp, feet, chest area or back.
Children with a tendency to dermatitis and a low level of immunity are at risk for the disease.
Features of the disease:
- symptoms of granuloma annulare may appear and disappear on their own;
- in most cases, the symptoms of the disease are not accompanied by pain, itching or burning of the skin.
Types of pathology
Many doctors believe that granuloma annulare is a dermatosis with an unclear manifestation pattern. The appearance of a foreign spot on the skin should not be left without treatment - this can have unpleasant consequences for health.
The disease is classified according to the degree of proliferation of skin rashes and the distinctive characteristics of pathological nodules. The course of therapy depends on the type of pathology. Some forms can disappear on their own without requiring medical intervention.
The following types of disease are distinguished:
- The localized form occurs mainly in children. It occurs without pain, there is no itching or burning. Capable of self-healing.
- Subcutaneous granuloma affects children under 6 years of age. The papule is connected to nearby tissues, which can be characterized by deep germination into the deep layer of the skin.
- The perforating form differs from the localized form by the presence of a capsule that periodically secretes a yellowish liquid.
- The perforating appearance often occurs in the fingers and hand. The skin at the site of papule formation becomes lighter in color. Occurs mainly in childhood.
- The disseminated form is typical for adults. Children rarely get sick. The nodules spread throughout the body, affecting large areas. The ring form of the formation is often absent - nodules appear singly in a chaotic manner.
- The middle type is characterized by aggressive growth and proliferation throughout the body. Characterized by severe symptoms, urgent treatment is required.
- The cholesterol type is rare. It is characterized by inflammation of the bone of the temporal lobe of the skull caused by trauma or otitis media of the middle ear.
- The vascular form is papules containing a large number of blood vessels.
- Epithelioid granuloma is formed from epithelioid fiber cells.
- The purulent form is characterized by the development of nodules with purulent inflammation.
- The ligature form is a manifestation of pathology at the site of the postoperative suture. The reason for this is a foreign particle in the tissue.
- The sarcoid type is formed in the tissues of the lymph nodes and in the area of internal organs.
- The syphilitic form is a complication of severe syphilis.
- Tuberculosis granuloma occurs in the tissues of the respiratory tract when a pathogenic particle enters the lungs and bronchi.
- The giant cell species affects bone tissue. The nodules do not grow, remaining in the formation zone.
- The calcific form is characterized by the accumulation of calcareous deposits in the area where the nodule appears. The calcified form is treated with drug therapy.
The disease is divided into two types - typical and atypical granuloma. The typical form is localized pathology. All other types are classified as atypical forms.
Classification and forms
Classification of granuloma annulare is carried out depending on the degree of spread of the disease and the characteristics of the process of formation of nodules .
The form of the disease plays an important role in determining the course of therapy. Some types of granuloma annulare are initially distinguished by their ability to quickly heal themselves. In this case, there is no need to take special measures.
Forms of granuloma annulare:
- Localized type (this form of the disease is characterized by the ability to heal itself, in most cases it manifests itself in childhood and does not cause discomfort to the small patient).
- Subcutaneous type (papules can connect with neighboring tissues, the pathology is typical for preschool children, foci of the inflammatory process differ in the depth of formation of papules);
- Perforating type (visually this form of the disease does not differ from the localized type, but a nuance of this pathology is the presence of a specific plug from which a yellowish liquid is regularly released).
- Perforating type (nodules appear mainly on the fingers and hands; in most cases, lightened areas of skin form at the site of the formations; this form of the disease is most often found in preschool children).
- Disseminated type (in childhood, this disease practically does not occur, lesions can be numerous and spread throughout the body, the connection of papules into a ring may not be observed).
Granuloma annulare is classified into typical and atypical forms. The first category includes the localized type, the second - the disseminated, perforating and subcutaneous type of the disease.
Perforating granuloma annulare is a separate type of disease. The nodules may secrete yellowish contents or not contain much fluid.
Reasons for the development of the disease
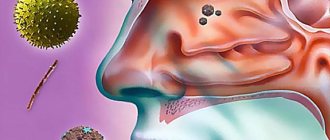
The etiology of the disease has not yet been fully studied, so research is still being carried out today. The disease is classified as idiopathic. An anular node can be caused by an external factor or internal disorders of the body.
Anular granuloma on the hand
The causes of granuloma may include the following:
- Mutations in the genetic structure of a cell are disrupted chromosomal sequences of DNA.
- Exposure to direct sunlight for 5-7 hours a day.
- Complication after vaccination or Mantoux test.
- An insect bite that provoked the formation of nodes.
- Presence of warts.
- Cutaneous dermatosis or other skin diseases.
- Respiratory tract infection – tuberculosis.
- Disease of the endocrine system - diabetes mellitus or pancreatitis.
- Metabolic disorders in the body.
- Hereditary predisposition.
- Mechanical injury to the skin.
- Decreased protective functions of the body.
Causes and development factors
Granuloma annulare is an idiopathic type .
The reasons for the development of pathology remain poorly understood.
Based on research, a list of factors that can provoke such skin damage has been compiled. According to most experts, the main cause of granuloma annulare is a violation of cellular immunity .
factors can provoke the development of pathology :
- consequences of a child's prolonged exposure to the sun (sunburn);
- a specific reaction of the body to manta or other vaccinations;
- negative consequences of insect bites;
- formation of warts on the skin;
- consequences of skin diseases;
- tuberculosis;
- diabetes;
- endocrine diseases;
- disruption of metabolic processes in the body;
- genetic predisposition;
- consequences of skin injuries;
- autoimmune processes in the body.
Recommendations from pediatricians for the treatment of vitiligo in children can be found on our website.
Signs of the disease
At the initial stage, the disease is asymptomatic. A person may not suspect a granuloma for a long time. Papules develop over several years. The first symptoms appear when the node grows to a large size. Extraneous rashes form on the skin, representing a chain of nodules of different shades.
The following are considered characteristic signs of the disease:
- the papule differs from skin pigmentation in structure and color;
- suspicious seals form a specific ring in the affected area;
- papules have a smooth surface;
- in childhood there is no pain;
- In a child, papules form on the legs, under the knee, in the elbow area and on the hands.
If a suspicious lump appears, you should consult a doctor and undergo an examination to rule out possible malignant pathologies. Clinically, the disease may not manifest itself for several years.
Symptoms of granuloma annulare
The first manifestations of the disease can be noticed on the skin long before large spots appear. First, dense shiny nodules, mostly smooth, are observed. They come in purple, red-pink or flesh tones (see photo below). There are no painful sensations during this period.
Pain may appear in later stages of granuloma development.
As soon as the first nodules appear on the skin, they begin to develop and grow. After a few months, these nodules form a ring-shaped plaque.
Over time, the size of the granuloma will increase. The size can increase from 0.5 to 10 centimeters. In the center of the node, the color of the formation changes and becomes flesh-colored or slightly bluish.
Another symptom of the disease is the appearance of evolutionary polymorphism. The elements of polymorphism include:
- scales;
- crusts;
- ulcers;
- scarring;
- cracks;
- erosions on the skin.
Plaques can be located on the hands, elbows, feet, and knees. In rare cases, they may appear on the neck, forearms or buttocks.
Diagnosis of granuloma
Diagnostic procedures will help distinguish granuloma from other skin diseases:
- The doctor conducts a visual examination of the diseased area, collecting a verbal medical history.
- A sample of diseased skin is taken to the laboratory for examination.
- Blood and urine are submitted for general clinical and biochemical analysis to identify structural changes.
- Histology of biological material is carried out.
After receiving the test results, the doctor can determine the extent of damage to the dermis and select a course of therapy.
Treatment options
Treatment of granuloma annulare depends on the etiology of its occurrence. If concomitant chronic pathologies are detected, then their persistent therapy is required. To improve blood circulation in the body, Retinol is prescribed. It is definitely recommended to use vitamin preparations, in particular, B vitamins and ascorbic acid are prescribed.
There is no universal way to get rid of a pathological neoplasm. The algorithm of the therapeutic course is determined by clinical manifestations, location, size of the element, general well-being of the patient, medical history and other factors.
Note: cold treatment has proven itself well. The doctor irrigates the affected area with Chlorethyl until a layer of “frost” appears on the skin - this manipulation is carried out once every 7 days. The duration of the full course is 5 procedures for each focus of inflammation.
Pyogenic granuloma in most cases is treated through surgery. This method allows you to guarantee a solution to the problem. The essence of the procedure is the complete removal of the affected area. The operation is performed under local anesthesia. Bleeding often occurs because the tumor is vascular in nature.
Sometimes the doctor recommends laser removal or cauterization with nitrogen. In some cases, conservative therapy is used. The doctor prescribes the use of the drug Imiquimod. Its mechanism of action is due to modification of the immune system, which provokes rapid regression of the tumor.
Treatment of the disease
The choice of treatment depends on the child’s physical characteristics and medical indications. In the presence of chronic pathologies, therapy is adjusted taking into account the use of other medications. The doctor sometimes chooses a wait-and-see approach; the node may disappear on its own.
You can get rid of granuloma annulare using the following treatment methods:
- taking medications to stop the growth of papules;
- excision using cryodestruction;
- procedure using carbonic acid;
- Irrigation of the sore spot with chlorethyl.
For granuloma annulare, doctors prefer to use drug therapy. The following drugs are used for treatment:
- Prescribe vitamins and other means that improve blood circulation - Tocopherol, Ascorbic acid, vitamin B and iron tablets.
- Non-steroidal drugs – Phenylbutazone, Indomethacin.
- Ointment with corticosteroid – Psoriderm.
- Creams, ointments and gels containing hormones - Triderm or Dermovate.
- Preparations with glucocorticoids - Hydrocortisone, Betamethasone valerate.
- Injections for subcutaneous administration around the papule - Acetonide.
In adults, the disease is preferably treated according to the same scheme as in childhood. To speed up recovery, you need to follow the doctor’s recommendations - this will prevent further growth of the lesions.
Causes
Why granuloma annulare forms is not clear. Medical experts believe that the formation of a ring-shaped form is a skin reaction that occurs due to exposure to provoking factors.
Important: there is reason to believe that there is a connection between chronic pathologies - rheumatism, tuberculosis and sarcoidosis and granuloma neoplasm. Moreover, it is not the infection itself that causes the pathological process, but a peculiar reaction of the human skin.
The infectious theory of the occurrence of a pathological element also includes other diseases - fungal infections, sexually transmitted diseases, chlamydia, syphilis. The non-infectious assumption identifies rheumatoid arthritis, surgical interventions, and trauma.
Granuloma can form at the site of tattoos, after removal of papillomas and warts, or at the site of shingles rashes. In medicine, cases of growths appearing on scar tissue have been described.
Pyogenic granuloma occurs due to the following reasons:
- Appears at the site of severe burns;
- Taking certain birth control pills;
- Acne therapy with Tretinoin (cream);
- Severe skin trauma;
- Skin diseases of various etiologies;
- Insufficient or excessive hygiene.
Granuloma annulare in children occurs for the same reasons as in an adult; no fundamental differences are noted. Treatment of ring-shaped lesions is determined by the clinical picture of the disease, the primary source of the problem.
Many granulomas that appear in women during pregnancy quickly regress after childbirth. This is due to the fact that during pregnancy the growth rate of the epithelial tissue lining the blood vessels increases. After the birth of the child, everything returns to normal.
Traditional medicine
Doctors allow the use of alternative medicine recipes. Before using a mixture based on medicinal herbs, it is recommended to exclude an allergic reaction of the body. Therefore, such treatment is carried out under the supervision of a doctor. To do this, an allergy test for incoming components is carried out. You should be careful with honey and some types of berries - there is a risk of urticaria and other reactions.
The following recipes are most often used:
- Take glycerin (capsules or ointment) and celandine tincture 30%. Mix the ingredients in a 1:1 ratio until smooth. Moisten a bandage or napkin in the resulting mixture and place it on the sore spot. Secure with adhesive tape or a tight bandage. Leave the compress until the morning. Use the mixture until complete recovery once a day.
- You will need rosehip leaves (5 tbsp) and finely chopped elecampane root (1 tbsp). Mix the ingredients in a separate bowl, pour boiling water (1 cup). Place on low heat and simmer for 15 minutes. Drink the infusion once a day in the form of tea.
- You need to squeeze juice out of radishes and carrots - 200 ml each. You will need 1 tbsp lemon juice. Pour everything into the prepared container and mix thoroughly. Drink 3 times a day, 1 tbsp.
When a granuloma appears, it is recommended to exclude mechanical impact on the node. Injury to the papule can provoke severe complications and re-infection of the body. Following good hygiene will help speed up your recovery.
Recommendations of Dr. Komarovsky
Dr. Komarovsky recommends, in addition to the basic treatment measures for granuloma annulare in children, to take measures to protect the affected area of the skin .
The units should not be subject to clothing friction, injury or other mechanical stress. Such factors can aggravate the situation and cause negative consequences.
Doctor advises:
- observe the rules of personal hygiene and prevent contamination of the affected areas of the skin;
- treat affected areas with prescribed ointments;
- if the disease does not go away for a long time or is prone to frequent relapses, then radical measures must be taken (injections, liquid nitrogen treatment procedures, etc.);
- When treating a disease, one must use the tactic of waiting for its self-healing.
How to remove lice and nits from a child? Find out the answer right now.
Preventive measures against pathology
The exact causes of the disease are still unknown to doctors. Therefore, it is difficult to decide on the prevention of pathology. The difficulty lies in the spontaneous disappearance of the seals.
It is recommended to perform the following procedures to help prevent the development of dangerous papules:
- It is worth taking medications that enhance immunity.
- Promptly treat skin and other diseases that can provoke granuloma.
- It is recommended to treat allergies at an early stage of formation.
- Prevention of infectious and viral pathologies will prevent illness.
- Balance your diet – increase foods with plant fiber.
- Take vitamins regularly.
If you follow the rules of prevention, this will avoid the formation of papules on the skin. The disease does not cause serious consequences, but it does cause psychological and cosmetic discomfort. Therefore, when the first suspicious symptom appears, you need to consult a doctor and undergo an examination. Early treatment helps avoid other complications.
Treatment of granuloma annulare
Due to the unknown cause of the disease, it is difficult to cure it effectively. Moreover, sometimes it is not necessary. Indeed, in some cases, granuloma goes away on its own without any consequences. If there is no pain, doctors recommend waiting until the granuloma goes away on its own.
If there is pain, then local treatment with vitamins B, E, C, D2 is prescribed. Fortified preparations are injected around the infected area.
The most popular treatment method is hydrocortisone emulsion. It helps to slow down the hypersensitivity reaction, proliferative and exudative processes at the site of inflammation. The drug itself acts through special intracellular receptors
In addition, doctors practice “scarification”. That is, they make a notch on the skin.
To make treatment of the disease faster and more effective, doctors recommend correcting carbohydrate metabolism, as well as treating diseases that may be the cause of granuloma (tuberculosis, chronic infections, diabetes, allergic reactions).
It is recommended to take medications that will help improve microcirculation. For example:
- retinol;
- B vitamins;
- ascorbic acid;
- preparations containing iron.
Perforating form
In rare cases, a perforating form may develop - a traumatic type of granulomatosis annulare. The hands and fingers are affected; the formation looks like a papule, which eventually turns into a plaque. Granuloma usually goes away on its own, but if it causes discomfort to a person, comprehensive treatment with corticosteroids may be required. Ultraviolet light therapy, biopsy, and surgical excision are also performed.
How to recognize granuloma
In most cases, this disease is asymptomatic and is discovered by a doctor by chance when taking an x-ray. In this case, most often the granuloma has an advanced form. However, some signs may indirectly indicate a neoplasm at the apex of the tooth root.
- acute toothache (especially during the development of any viral or respiratory disease),
- swelling, redness, tenderness of the gums,
- purulent discharge from the gum pocket,
- darkening of tooth color,
- headache, malaise,
- occasionally – enlargement of the cervical or submandibular lymph nodes.
Important! Only a doctor can diagnose the presence of a granuloma and only based on the results of an x-ray. It will show not only the purulent capsule on the root, but also the general condition of the tooth, which will help you choose treatment tactics.
Causes
There are a number of known causes that can cause granulomas on the body. These include:
- Chronic or acute infectious diseases
- Presence of a foreign body
- Scleroderma
- Wegener's granulomatosis
- Dental diseases
- Rheumatism
- Crohn's and Horton's diseases
- Taking certain medications
- Venereal diseases
- Silicosis
- Talkoz
- Byssinosis
- Asbestosis
- Surgical interventions
- Sarcoidosis
Treatment and prognosis
In some cases, eosinophilic granuloma does not require treatment, does not manifest itself in any way and goes away on its own within a few years. In case of severe symptoms and/or pronounced bone defects, different approaches and their combinations are used: surgical removal of the lesion (curettage, excision) or its radiofrequency ablation; prescription of cytostatics or a combination of cytostatics and glucocorticosteroids (including those administered into the pathological focus); radiation therapy in the presence of large lesions or lesions that compress neighboring tissues and organs. Correction of concomitant pathologies is also carried out.
Anti-cytokine drugs, anti-CD1a monoclonal antibodies, and trans-retinoic acid drugs are considered promising treatment regimens for histiocytosis X.
EG generally has a favorable prognosis, up to the possibility of spontaneous recovery, however, when transitioning to other forms, the course of histiocytosis from Langerhans cells can be more malignant - this happens, for example, when the bone marrow is involved (a rather rare phenomenon). In some cases, Taratynov's disease requires surgical intervention. After the course of treatment, patients must be under clinical supervision of an oncologist for 3 years with monthly examinations and x-ray examinations every six months.
Treatment
The treatment of granuloma annulare, as well as its etiology and pathogenesis, remains a mystery. This is due to the fact that, despite the huge number of drugs and methods of physiotherapeutic treatment, none of them led the patient to a 100% recovery or stable remission. Therefore, the main principle of therapy was the correction of existing disorders in the body: diabetes mellitus - control of blood sugar levels, infectious process - antibacterial therapy, etc.
There are local and systemic methods of treating the disease.
Local therapeutic methods are the safest approved for use in children. These include the use of corticosteroid ointments of moderate and high potency. The course of treatment is two weeks of daily lubrication, and then every other day. To improve the absorption of the active substances of the drug, phonophoresis is used.
Systemic treatment of granuloma annulare in children is prohibited. In adults, it includes oral administration of corticosteroids (in the disseminated form), antimalarial drugs. Physiotherapeutic treatment includes PUVA therapy (long-wave ultraviolet irradiation). This method has proven effective in the treatment of psoriasis, neurodermatitis, eczema and other dermatological diseases.
The essence of the method is to irradiate the skin with ultraviolet light after its preliminary sensitization (increased sensitivity) with special preparations: psoralens
Both adults and children are prescribed immunostimulating therapy and vitamin supplements (ascorbic acid, tocopherol, iron supplements, B vitamins, etc.).
In addition to traditional therapy, there are also traditional methods of treatment. Their advantages:
- availability;
- ease of use;
- low cost;
- safety.
Recipe 1
You will need:
- Celandine tincture 30%
- Pharmacy glycerin.
Mix the components 1:1. Apply compresses to the affected area once a night.
Recipe 2
Aimed at strengthening the immune system. You will need:
- 5 tablespoons dried rose hips
- 1 tablespoon dried elecampane roots
- 1 liter of boiling water.
Elecampane is tall. Perennial herbaceous plant. It grows in the territory of Belarus, the Caucasus, Crimea, Central Asia, in the steppe and forest-steppe zones of the European part of Russia, in the Urals and Western Siberia.
After mixing the dry ingredients, pour boiling water over them. Heat over low heat for 10-15 minutes. Leave for 60 minutes. Take as tea, after diluting with water.
External manifestations of the disease
The disease is chronic and asymptomatic. The patient is not bothered by itching or pain. They are extremely rare, most often with a perforating form of granuloma. The disease is prone to self-healing and gradually (within 2 years) disappears in 3/4 of patients. It is also prone to relapses (exacerbations), in almost half of patients. It goes away without a trace, sometimes pigmentation remains, but after some time it also disappears. Scars rarely remain, usually in the perforated form.
Clinically it looks like chains of papules or ring-shaped plaques (round, oval, less often polygonal). The middle is free from rashes, sometimes looks slightly depressed. The skin color does not change or acquires a purple, pink, or grayish tint. Sizes range from 2 to 5 cm, rarely more. Papules can spread peripherally (outward).
Publications
Granuloma annulare (granuloma anulare, anular granuloma) is a chronic, slowly progressive, relapsing benign granulomatous dermatosis of unknown etiology.
Historical information. The skin disease known as granuloma annulare was first described in 1895 by Englishman Thomas Fox under the name “Ringed eruption of the fingers” [2]. In 1908, G. Little analyzed all descriptions of granuloma annulare known at that time and identified it as a separate disease [12]. He was the first to suggest a relationship between granuloma annulare and tuberculosis infection. Later, atypical forms of granuloma annulare were described. For example, in 1938, dermatologist S. Monash first mentioned a case of a common form of granuloma annulare [14]. The first description of the pathomorphological picture of granuloma annulare is found in an article by V. Dubreuil, published in 1895. The author described the dermal histiocytic infiltrate, the absence of changes in the epidermis, areas of destruction of collagen fibers - signs known today as the classic signs of granuloma annulare [5].
Epidemiology of granuloma annulare. The incidence of granuloma annulare is not known. Granulomas occur at any age. There are two age periods for the onset of the disease. Approximately 70% of patients are young people under 30 years of age, in whom the disease is predominantly mild and often goes away on its own. The second group of patients are people over 50 years old. In this age period, the disease is usually combined with a number of pathologies of internal organs and is difficult to treat.
Etiology. The causes of granuloma annulare are not known. One of the largest groups of patients with granuloma annulare (100 people) was described in 1989 by K. Dabsky and R.K. Winkelman, who noted that in 21% of patients the disease was associated with diabetes mellitus [3]. Proving the relationship between the two diseases is difficult because the incidence of diabetes in the United States is quite high. The authors also suggested that the disease may occur as a result of excessive solar radiation and as a result of an adverse reaction due to medication. These assumptions, however, were not supported by convincing evidence.
There are several reports of the occurrence of granuloma annulare in children after vaccination [8, 16, 26]. A certain role in the occurrence of granuloma annulare is played by chronic infections, sarcoidosis, rheumatism, tuberculosis, hepatitis B. The granulomatous process is considered in this case not as a result of altered tissue reactivity. Great importance is attached to allergic reactions. A combination of granuloma annulare and autoimmune thyroiditis has been described [21].
The occurrence of granuloma annulare is the result of a delayed-type hypersensitivity reaction that occurs in response to an unknown antigen. The infiltrate is dominated by Th1 lymphocytes that produce IFN-γ and cause collagen degeneration [4, 9, 25].
Clinical picture and classification. The most common form of granuloma annulare found in the literature is limited . This form is characterized by the appearance of small (3-4 mm in diameter), dermal nodules of dense elastic consistency, flesh-colored or pinkish-brown, which are grouped into rings, semi-rings, and arcs. The size of the lesions varies from 1 to 5 cm or more. The center of the lesion sinks somewhat, giving the impression of skin atrophy. The rashes do not peel off. Typical localization is the skin of the back of the hands (feet), phalanges of the fingers, the extensor surface of the back of the elbow and knee joints, the anterior surface of the legs, i.e. in places where the skin is most susceptible to mechanical trauma and least protected by a layer of subcutaneous tissue (Fig. 1).
Rice. 1. Localized granuloma annulare on the forefoot
Disseminated granuloma annulare is characterized by the presence of multiple disseminated foci of granuloma annulare. The vast majority of patients are over 50 years of age. In these cases, the rashes are multiple, scattered or merging, which can give the lesions a reticular character, but without a significant tendency to a ring-shaped arrangement. In this form, the papular rash is skin-colored or purple in color. This form occurs in persons with carbohydrate metabolism disorders and diabetes mellitus.
In the papular form of granuloma annulare, the papules are located isolated from each other. The rash in this form is monomorphic, consists of sharply limited, rather deep-lying nodular elements of dense consistency with a diameter of 4-6 mm in the dermis. Their shape is hemispherical, their outlines are round or polygonal. The elements are slightly shiny, pearlescent, pinkish or the color of normal skin, sometimes reminiscent of keloids. The preferred location is the back of the hands and feet; less commonly, rashes are located on the skin in the area of the knee and elbow joints, neck, forearms, and buttocks. Papules accompany the typical annular rash of granuloma annulare. Eruptions similar to the papular form of granuloma annulare have been described in children exposed to Culicoides furans mosquito bites. Bite-associated rashes are accompanied by eosinophilia, and the typical ring-shaped elements are absent [15].
The deep form of granuloma annulare was described for the first time by A. Barzilai et al. in 2005. The condition should be differentiated from rheumatoid nodules [19]. This type of granuloma annulare is usually located on the scalp, elbows, forearms, dorsum of the hands, fingers, legs, and rarely in the periorbital region. The clinical picture is of skin or subcutaneous mobile nodes tightly connected to the periosteum.
The term “ perforating granuloma annulare ” was first used by D. Owens in 1971 [18]. With this form, a papular rash with a horny plug in the center is observed on the hands and fingers, from which a gelatin-like liquid is secreted, then crusts and lesions with an umbilical depression in the center are formed, then atrophic scars can form. The histological features of perforating granuloma annulare are the superficial location of the granulomas, in which they are injured and “removed” through the epidermis. A similar picture occurs with perforating collagenosis and metabolic diseases (diabetes mellitus, renal failure, etc.).
Cases of erythematous annular granuloma , when the rashes were located on open areas of the body and were infiltrated erythematous spots and papules. The histological picture of the cases described in the literature was consistent with interstitial histiocytic dermatitis. The condition should be differentiated from interstitial toxicoderma, which can be the result of ingestion of antihypertensive, lipid-lowering, antihistamines, and antidepressants [11].
In 1975, J. Obrian describes a special type of granuloma annulare - actinic granuloma , the rashes of which were located on the back of the neck - on skin exposed to solar insolation [17]. According to J. Obrian, a feature of this form of granuloma annulare was the presence of giant multinucleated histiocytes, sometimes including degenerated elastic fibers. However, this symptom also occurs in classical forms of granuloma annulare when the elements are located on open areas of the skin, which does not allow actinic granuloma to be identified as a separate form of the disease.
Often, a combination of several clinical forms can be identified in the same patient (Fig. 2).
Rice. 2. Patient A., 46 years old. Diagnosis: granuloma annulare. A – disseminated rashes on the skin of the abdomen, B – deep granuloma annulare on the back of the neck
Pathomorphological picture of granuloma annulare. In pathological examination, two types of granuloma annulare are distinguished: front garden type and interstitial type [10]. In the front garden type, a granulomatous infiltrate is noted in the papillary dermis in the center of which there are mucin deposits, surrounded by histiocytes and lymphocytes in the form of a palisade (Fig. 3).
Rice. 3. Front garden type of granuloma annulare. A – no changes in the epidermis, B – granulomatous infiltrate with mucin in the center and radially located histiocytes and lymphocytes along the periphery
In the interstitial type of granuloma annulare, accumulations of mucin and histiocytes are located between the fibers of the dermis (Fig. 4). Degeneration of collagen fibers can be observed in any histological type of granuloma annulare, but is limited in nature, unlike necrobiosis lipoidica.
Rice. 4. Interstitial type of granuloma annulare. A - no changes in the epidermis, B - mucin and histiocytes between the fibers of the dermis
Differential diagnosis of granuloma annulare. The disease must be distinguished from tuberculoid leprosy, cutaneous tuberculosis, tubercular syphilis, persistent elevated erythema, small nodular sarcoidosis, necrobiosis lipoidica, and rheumatic nodules.
Tuberculosis and leprosy are excluded based on the results of a pathomorphological examination using Ziehl-Nelssen staining, as well as on the basis of PCR examination of tissue. Skin tuberculosis (with the exception of atypical mycobacteria), as a rule, is accompanied by damage to the lungs or other organs.
The differential diagnosis of tubercular syphilide and granuloma annulare does not present any significant difficulties. The presence of ulceration of the tubercles with the subsequent development of focal mosaic scars, often positive specific serological reactions help in making the correct diagnosis.
With persistent raised erythema, the rash is more often localized around large joints than with granuloma annulare; they are larger in size and have a more acute inflammatory nature. Typically, the consistency of the nodules changes from soft (at the beginning of the disease) to hard (fibrotic). The nodules usually have a less pronounced tendency to group into ring-shaped lesions and form a recess in the center. Significant histomorphological differences are also noted. Persistent raised erythema is characterized by changes characteristic of leukocytoclastic vasculitis (fibrin deposits in the walls of blood vessels, the presence of neutrophils and “nuclear dust” of neutrophils). In the later stages of persistent raised erythema, sclerosis is noted [10].
Granuloma annulare differs from the small nodular form of sarcoidosis in its preferred localization (the area of small joints of the hands and feet, while in sarcoidosis the rashes are scattered, the skin of the face is often affected, the mucous membranes of the mouth and nose may be involved in the process), the color of the rashes (pale pink in annular granuloma; bluish or brownish in sarcoidosis). The diagnosis of sarcoidosis is established when clinical and radiological signs are confirmed histologically by the presence of noncaseating epithelioid cell granulomas. In the early stages (I and II), radiological data may be sufficient for diagnostic purposes. Diagnosis can be confirmed by transbronchial biopsy. In patients with active pulmonary sarcoidosis, serum angiotensin-converting enzyme (ACE) levels are usually elevated and the test becomes negative with treatment [4].
The differential diagnosis of granuloma annulare and the annular form of necrobiosis lipoidica can be much more difficult. In these cases, such signs as the predominant development of necrobiosis lipoidica in middle age, often in persons with impaired carbohydrate metabolism, and its preferential localization on the legs are taken into account. Pathomorphological differences are the deeper location of the infiltrate in necrobiosis lupoidum, the presence of plasma cells in the infiltrate, pronounced necrosis of collagen fibers, and the absence of mucin.
Rheumatic nodules, unlike nodules with granuloma annulare, are more often localized in the area of large joints; they are larger and lie deeper, located isolated or in groups consisting of several nodules. Unlike nodules in granuloma annulare, which are not accompanied by subjective sensations, rheumatic nodules are painful when pressed. On pathological examination, rheumatic nodules are characterized by large foci of collagen degeneration located deep in the dermis or subcutaneous fat, predominantly histiocytic and fibroblastic cellular infiltration with an admixture of plasma cells and lymphocytes.
Treatment of granuloma annulare. Treatment for granuloma annulare is often carried out on an outpatient basis. In our opinion, the use of systemic therapy, especially for limited forms, is unjustified. In children, the disease rarely requires treatment and goes away on its own within a year. If the disease persists, strong external corticosteroid medications may be recommended (for example, clobetasol propionate cream or ointment - “ Psoriderm ”, Pharmacare Inc.) [1]. Local corticosteroids of weak and moderate activity in the treatment of granuloma annulare are ineffective, since the inflammatory infiltrate is located in the dermis. Corticosteroids (triamcinolone) can be injected into the lesions.
Single lesions can be removed surgically or by laser or cryodestruction. There are known cases of reverse involution of granuloma annulare foci when taking a biopsy from the lesion [22].
The most difficult treatment is for disseminated granuloma annulare, associated with metabolic disorders. In such cases, niacin (vitamin B3) 500 mg 3 times a day, antimalarial drugs (hydroxychloroquine 6 mg/kg/day), dapsone (100 mg per day) are used [3, 23, 24]. There are known cases of effective therapy for disseminated granuloma with isotretinoin and cyclosporine [6, 7, 20]. Physiotherapeutic methods that can be used are PUVA therapy and ultraviolet B spectrum radiation.
Literature:
- Kozlovskaya, V.V. The use of Psoriderm cream in the treatment of chronic dermatoses / V.V. Kozlovskaya // Medical news. – 2010. – No. 5-6. – pp. 83-86.
- Colcott-Fox, T. Ringed eruption of the fingers / T. Colcott-Fox // Br. J. Dermatol. – 1895. – P. 91-92.
- Dabski, K. Generalized granuloma annulare: clinical and laboratory findings in 100 patients / K. Dabski, RK Winkelmann // Journal of the American Academy of Dermatology. – 1989. – Vol. 20. – P. 39-47.
- Dermatology / J. Bolognia et al. – Mosby, 2003. – P. 2500.
- Dubreuilh, W. Eruption circinée chronique de la main / W. Dubreuilh // Ann. Dermatol. Syphiligr. – 1895. – P. 335-338.
- Fiallo, P. Cyclosporin for the treatment of granuloma annulare / P. Fiallo // Br. J. Dermatol. – 1998. – Vol. 138. – P. 369-370.
- Generalized granuloma annulare in a patient with type II diabetis mellitus: successful treatment with Isotretinoin / M. Sahin at al. // Journal of the European Academy of Dermatology and Venereology. – 2006. – Vol. 20. – P. 111-113.
- Granuloma annulare following BCG vaccination / C. Houcke-Bruge et al. //Ann. Dermatol. Venerol. – 2001. – Vol. 128. – P. 541–544.
- Hanna, W.M. Granuloma annulare: an elastic tissue disease? Case report and literature review / WM Hanna, F. Moreno-Merlo, L. Andrighetti // Ultrastruct. Pathol. – 1999. – Vol. 23. – P. 33-38.
- Histologic Diagnosis of Inflammatory Skin Diseases, third ed. / AB Ackerman et al. - New York: “Ardor Scribendi”, 2005. – 522 rub.
- Interstitial granulomatous drug reaction with a histological pattern of interstitial granulomatous dermatitis / C. Perrin et al. //Am. J. Dermatopathol. – 2001. – Vol. 23. – P. 295-298.
- Little, E. Granuloma annulare / E. Little // Br. J. Dermatol. – 1908. – P. 213.
- Ma, A. Response of generalized granuloma annulare to high-dose niacinamide / A. Ma, M. Medenica // Arch. Dermatol. – 1983. – Vol. 119. – P. 836-839.
- Monash, S. Granuloma annulare disseminatum / S. Monash // Arch. Dermatol. Res. – 1932. – P. 122-131.
- Moyer, DG Papular Granuloma Annulare / DG Moyer // Arch. Dermatol. – 1964. – Vol. 89. – P. 41-45.
- Multiple lesions of granuloma annulare following BCG vaccination: case report and review of the literature / M. Kakurai et al. // Int. J. Dermatol. – 2001. – Vol. 9. – P. 579.
- O`Brien, JP Actinic granuloma. An annular connective tissue disorder affecting sun- and heat-damaged (elastic) skin / JP O`Brien // Arch. Dermatol. – 1975. – Vol. 111. – P. 460-466.
- Owens, DW Perforating granuloma annulare / DW Owens, RG Freeman // Arch. Dermatol. – 1971. – Vol. 103. – P. 64-67.
- Pseudorheumatoid nodules in adults: a juxta-articular form of nodular granuloma annulare / A. Barzilai et al. //Am. J. Dermatopathol. – 2005. – Vol. 27. – P. 1-5.
- Ratnavel, RC Perforating granuloma annulare: response to treatment with Isotretinoin / RC Ratnavel, PG Norris // Journal of the American Academy of Dermatology. – 1995. – Vol. 32. – P. 126-127.
- Report, C. Localized granuloma annulare and autoimmune thyroiditis: a new case report / C. Report // Journal of the American Academy of Dermatology. – 2000. – P. 943-945.
- Resolution of patch-type granuloma annulare lesions after biopsy / N. Levin et al. // Journal of the American Academy of Dermatology. – 2002. – Vol. 46. – P. 426-429.
- Simon, Jr.M. Antimalarials for control of disseminated granuloma annulare in children / Jr.M. Simon, P. Von den Driesch // Journal of the American Academy of Dermatology. – 1994. – Vol. 31. – P. 1064-1065.
- Steiner, A. Sulfone treatment of granuloma annulare / A. Steiner, H. Pehamberger, K. Wolff // Journal of the American Academy of Dermatology. – 1985. – Vol. 13. – P. 1004-1008.
- Umbert, P. Histologic, ultrastructural, and histochemical studies of granuloma annulare / P. Umbert, RK Winkelmann // Arch. Dermatol. – 1977. – Vol. 113. – P. 1681-1686.
- Wolf, F. Generalized granuloma annulare and hepatitis B vaccination / F. Wolf, P. Grezard, F. Berard // Journal of the European Academy of Dermatology and Venereology. – 1998. – Vol. 8. – P. 435–436.
Kozlovskaya V.V., Abdel M.V.
Gomel State Medical University, Gomel, Belarus
Diagnostic methods
Since the clinical manifestations of granuloma annulare are quite specific, diagnosis, in most cases, does not cause difficulties. If the case is doubtful, then it is necessary to perform a skin biopsy and subsequent histological examination of the obtained material.
When examining a biopsy specimen under a microscope, foci of necrobiosis located in the connective tissue are revealed. Mucin deposits are observed in them; histiocytes, lymphocytes and multinucleated cells are present in the tissues. Signs of granulomatous inflammation are clearly visible in the dermis.
Molluscum contagiosum ICD-10 B08.1
Discussion: 16 comments
- Lana:
04/28/2018 at 15:55Thanks to the author for this article, I have never heard of such a disease from anyone, I read and even studied a lot for myself, I learned a lot from what I read, now I will know that there are such types of diseases, thank you again for the high-quality information provided!!!
Answer
- Stepan:
04/28/2018 at 16:20
The disease is quite rare. And the most important thing is that, as I understand it, the reasons for it are not known. Everything is described in quite detail and this is good, because timely detection of such a disease will help to cure it and stop it in time. There are so many diseases, but when something like this appears on the skin, it is noticeable and natural discomfort. We will now know what it is and what to do.
Answer
- Andrey:
04/28/2018 at 16:51
I had a similar granuloma, only in the chest, almost in the middle. It went away on its own after about 1.5-2 years. I didn’t go to the doctors because... There were no scary tumors, just a 3-4 mm abscess.
Answer
- JefferyMaine:
05/05/2018 at 18:12
I will sell databases of websites, forums, blogs with TICs from 10 for promotion on the Internet. Collection of thematic databases for promotion. Topic: Loans, borrowed money - 11000942 sites. Topic: online stores, shopping - 5217310 sites. Topic: crypto, bitcoin - 700,000 sites. Collection of bases for promotion to order
ICQ 726166382
Answer
- Markuzi:
05/06/2018 at 03:52
Internet promotion.
Skype: Seo promotion+ ICQ 726166382 *strong*
Answer
- Dennis Enent:
05/06/2018 at 13:40
We know how to value your time and share common tasks with you. Promoting your website is our top priority. Our services: Collection of thematic databases with TICs FOR promotion Attracting visitors to the site Order promotion of your product. Write on Skype: Seo Promotion+
*&*
Answer
- BobbyKap:
05/06/2018 at 18:36
We are offering to you . What does such a run give: Your site will rise higher in search engines.
His attractiveness will increase. The number of visitors will increase. Advertising income will increase (if any) Depending on the volume, the work stretches over time! (200k - 200,000 resources on which profiles will be registered with a link to your resource.)
ps we do not engage in spam, mailing or direct posting to forum topics, we register profiles on resources that allow this. Contact ICQ 726166382
Answer
- Kirill Zotov:
05/30/2018 at 16:04
Is that really possible? We are living in 2018...
Answer
- BruceMP:
06/01/2018 at 01:44
We are dedicated to one goal: helping you overcome addiction for good. Every detail is taken into account to give you stability and comfort, and help you break free from addiction and rebuild your life without drugs. Phone: +79506268241
Answer
- Robertunall:
06/10/2018 at 00:31
high site Jarle Thorsen Unaico Reviews
Answer
- Andrey Golubpn:
06/12/2018 at 09:19
___123___Granuloma annulare: symptoms, diagnosis, treatment, photo___123___
Answer
- RobertZero:
06/22/2018 at 04:09
Have a good day.
Answer
- MashaNom:
06/22/2018 at 05:52
Holidays in Russia, where to choose a hotel?
Answer
- 3d models:
07/01/2018 at 10:09
Thanks for every other great article. The place else may anyone get that kind of info in such an ideal method of writing? I have a presentation next week, and I am on the search for such information.
Answer
- KeysParry:
07/02/2018 at 07:05
Greetings to all! Good site you have!
Not long ago I found an ei p7002 300h on the Internet from an industrial electrician company. I recommend!
Thank you!
Answer
- video sesso donne italiane:
07/03/2018 at 17:23
donna nuda che fa sesso video sesso donne italiane sesso pipi porno gratis por el culo ninfomane sesso porno tube italiano sesso al mare chat di sesso annunci sesso gratis roma guida al sesso anale sesso in romania video sesso forte gratis paese del sesso cos e il sesso incontri sesso liguria video porno gratis mogli troie video porno gratis con neri tumblr a tutto sesso thailandia porno gratis incontri per sesso padova malattie genetiche legate al sesso samba porno italiano film porno donne grasse gratis porno star sesso sesso italiano tube sesso zia porno tube gratis video sesso in piscina my porno gratis porno video italiano fetish porno gratis seks porno italia incontri per sesso aosta video sesso donne porno donne anziane gratis anime che fanno sesso sesso erotico film sex sesso sesso italiano hd porno gratis live annunci di sesso bergamo sesso orale per lui mara carfagna sesso sesso dildo porno gratis tette enormi nonne che fanno sesso con i nipoti incontri sesso martina franca porno gratis strapon videos porno gratis hd film porno anale gratis sesso a castelvetrano
Answer
Prevention
There is no specific prevention for granuloma annulare. Patients are advised to maintain a good immune system, carefully monitor various metabolic processes and promptly correct chronic diseases, preventing their decompensation. Additionally, it is recommended to avoid permanent trauma to the skin or exposure to cold.
Although granuloma annulare is a benign disease that resolves without treatment in 90% of cases, it is still necessary to see a doctor. The development of pathology indicates that some negative processes are occurring in the body.
There are no similar articles.
Classification
There are many types of granulomatous neoplasms and they all differ in causes, clinical manifestations and localization.
Eosinophilic granuloma is a rare disease that often affects the skeletal system, lungs, muscles, skin, and gastrointestinal tract. The reasons for the formation of this pathology are unknown. But there are several hypotheses - bone injuries, infection, allergies, helminthic infestation. Symptoms of the disease are often completely absent, and nodes are detected accidentally during examination for other reasons. If a patient, despite the absence of signs of the disease, does not reveal an increased level of eosinophils in blood tests, then diagnosis may be difficult.
Treatment tactics
As mentioned, granuloma annulare has a tendency to heal itself, so many specialists adhere to a wait-and-see approach. However, recurrent forms of the disease are detected quite often. In such cases, doctors begin treatment, the goal of which is to reduce the pathological formation and prevent further relapses.
As with other diseases, treatment must begin with proper nutrition, which consists of limiting the amount of carbohydrates. Of drug therapy, the main preference is given to the local use of ointments and creams containing glucocorticoids or non-steroidal anti-inflammatory drugs.
- Among hormonal ointments, the most popular are Elokom, Momat, Psoriderm, Hydrocortisone. Use them daily for 2 weeks, and then once every 3 days for 2 weeks. Injectable hormonal drugs are also used - Kenalog, which is used to inject the site of the pathological focus. Local glucocorticoids significantly reduce pain and itching of the skin in areas of existing lesions.
- Anti-inflammatory drugs - Protopic, Tacropic, which prevent the occurrence of atrophic changes in the skin. They are also prescribed in a long course, over 6 weeks.
- It is justified to use products that improve blood microcirculation - vitamin preparations of group B, as well as A and E.
- To normalize the regenerative function of the skin, use Retasol or Roaccutane.
Liquid nitrogen cryotherapy is considered to be an effective treatment method that can achieve remission in 80% of cases. It is actively used in the long-term absence of any improvement with drug therapy. It is necessary to take into account that scars may form at the site of intervention. Often they use the method of scarification - surface notches. Physiotherapeutic procedures - ultraviolet irradiation, phonophoresis - bring significant benefits.
All of these therapeutic methods should be carried out only in accordance with the recommendations and under the supervision of the attending physician.
What diseases can it be associated with?
Subcutaneous granuloma of the face is primarily associated with an infectious focus such as periodontitis. In the majority of cases, it is from this that it develops. Other diseases of the oral cavity, as well as inappropriately performed dental work, can also ultimately provoke the formation of granulomas in the subcutaneous tissue.
Indirect factors of facial granuloma include an allergic reaction and increased photosensitivity.
Subcutaneous granuloma can be complicated by an abscess in the facial area, which, however, is considered as an independent stage of the above-mentioned disease.
Types of granuloma
Based on the reasons for the development of granulomas, a distinction is made between the infectious and non-infectious nature of the onset of the disease. Separately, nodules of unknown etiology . Based on appearance, location and characteristic manifestations, the following types of granulomas are called:
- Pyogenic
- Eosinophilic
- Ring-shaped
- Tuberculosis
- Purulent
- Leprosy
- Scleroma
- Vocal cord granulomas
- Migrating subcutaneous
- Tooth granulomas
- Venereal
- Nonspecific
- Ligature
Treatment with folk remedies
Treatment with folk remedies is assessed not only by doctors, but also by patients as ineffective. This is explained by the fact that granuloma annulare is closely associated with various immune problems that are difficult to correct using traditional methods.
Baths, lotions and rubdowns are not recommended. It is better to focus your energy on strengthening the immune system of a person suffering from granuloma. To do this you can:
- drink echinacea in the form of tablets or tinctures;
- drink more restorative teas and fresh juices if there are no allergies;
- lead a generally healthy and active lifestyle.