Hematoma (from Latin haemat - blood, oma - tumor) is a term denoting a local accumulation of blood in the human body. It is formed due to the direct impact of trauma. Concomitant factors are vascular pathologies and blood diseases: platelet purpura, hemophilia type (A) and type (B), von Willebrand disease. Subcutaneous hematoma – The most common manifestation of this condition, less often there are hematomas of internal organs and their walls.
Description of subcutaneous hematoma
A subcutaneous hematoma is characterized by a small, limited protrusion above the skin, dark blue or purple in color. The boundaries are not smooth and clear. Sharply painful on palpation, it can also hurt at rest.
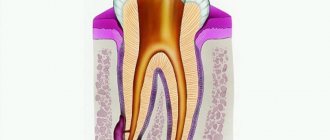
Due to the action of the etiological factor, blood flows out of the damaged vessel, which enters the skin, subcutaneous tissue and muscles. Each of the above structures contains septa and trabeculae. They form so-called anatomical reservoirs into which blood flows. As they fill, the pressure in the reservoir increases and thereby compresses the bleeding vessel. Blood flow in a pinched vessel slows down, and this leads to the formation of a blood clot and blockage of the damaged artery or vein. A reservoir filled with blood can compress nerve endings, which leads to pain.
An internal hematoma is much more dangerous than a subcutaneous one. The pathogenesis and etiology are the same for all types of such manifestations. Most often it appears in organs such as the brain, liver, and kidneys. The clinical picture depends on the organ in which the hematoma appeared and its size. The essence of the problem is compression of the organ by accumulated blood.
The hematoma takes a very long time to resolve. Throughout the entire time it changes its color from darker to lighter. This phenomenon is called “blooming”; it occurs due to the breakdown of hemoglobin in the blood, which forms a hematoma.
Bruise, bruise, hematoma, lump. How to say it correctly? Let's learn proper terminology.
In practice, we often encounter cases where a wide variety of terms are used to describe the same injury, which often leads to significant confusion. And the greatest confusion arises when, as a result of some impact (usually traumatic) on the body a person develops intradermal and subcutaneous hemorrhage - bruise.
They just don’t call this kind of damage – a bruise, a hematoma, or just a “bump.” Are these all synonyms?
Let's figure it out.
What is the difference, if any, between the terms hematoma and bruise? Both hematoma and bruise can form either as a result of external mechanical impact or as a result of disease.
A hematoma is a hemorrhage with a violation of tissue integrity and the formation of a cavity filled with blood. Literally translated, hematoma is a blood tumor (from ancient Greek αἷμα - blood + ōma - tumor).
A hematoma is formed due to the rupture of a vessel, followed by hemorrhage, which leads to tissue separation with the formation of a cavity in them.
A hematoma can be located superficially (under the skin or external mucous membranes), or it can also form deep in soft tissues, such as muscles. Rice. Hematoma of the leg
Rice. Subcutaneous hematoma
Rice. Neck hematoma
Formation of hematomas in the walls of organs is possible.
Rice. Nasal septum hematoma
If a hematoma has formed in the cranial cavity, then in relation to where it is located, the following are distinguished: - epidural (extradural) hematoma (located between the bones of the skull and the dura mater) - subdural hematoma (under the dura mater) - subarachnoid hematoma (under the soft mater) membrane) - intracerebral (parenchymal) hematoma (in the substance of the brain).
Rice. Variants of intracranial hematomas.
In newborns, there may often be a birth tumor on the head - a subcutaneous hematoma, which forms during childbirth in the presenting part of the head. This is fine. In adults, such a hemorrhage under the scalp is formed as a result of a blow, and is popularly called . ”
Newborns may also have a cephalohematoma (cephalohematoma) on their head. This is a hematoma, formed during childbirth and located between the periosteum and the outer surface of the cranial bones. The tumor is limited to the edges of one or another bone of the skull.
Rice. Variants of birth trauma to the head of a newborn. A. Cephalohematoma (subperiosteal hematoma). B. Birth tumor (subcutaneous hematoma)
So, an important, significant sign of a hematoma is the formation of a cavity filled with blood. If there is no cavity filled with blood, it is not a hematoma. Bruising is bleeding into soft tissue (for example, skin) while maintaining the tissue structure. A cavity in the tissue does not form during a bruise; this is not a cavity formation.
Rice. Bruise
In unprofessional, everyday speech, a bruise is called a bruise. Bruise is not a medical term, but a colloquial one. Not a single doctor, including a forensic expert, uses the word “bruise.” It is not recommended for lawyers to use this word in their professional activities.
Sometimes, wanting to show knowledge of medical terminology, a bruise is called a hematoma. This is fundamentally wrong. If someone wants to call a bruise in Latin, call it hemorrhagic permeation of the skin.
As a synonym for the word bruise, doctors often use the terms “ecchymoses” and “petechiae.” Ecchymosis is hemorrhage in the skin or mucous membrane, the diameter of which exceeds 3 mm. Petechiae are pinpoint hemorrhages in the skin, mucous membranes, serous membranes and internal organs, up to 3 mm in diameter.
Rice. Multiple petechial hemorrhages (point hemorrhages) in the skin of the arm.
Bruises in the skin change color over time and “bloom,” which allows forensic medicine to determine how long ago they formed.
Bruises in an array of soft tissues are called hemorrhages, for example, hemorrhages in the muscles of the thigh, forearm, etc.
Rice. Hemorrhage into the muscles of the forearm.
So, in this brief review, we tried to find out what the difference is between a bruise and a hematoma.
And knowing this difference is very important, since a bruise and a hematoma are different formations, they have different consequences for the body, the tactics of their treatment are different, and the severity of bodily injuries is different.
Symptoms
One of the earliest and longest lasting symptoms is pain. Pain occurs after swelling and may be pulsating or pulling. The intensity of the pain depends on which nerve endings have been compressed.
During injury, many cells are destroyed, in other words, alteration occurs. When a cell dies, many biologically active substances (BAS) are released, which irritate the receptors and cause a burning sensation and itching. Patients complain of decreased function of nearby muscles and the appearance of limited edema. Due to the release of biologically active substances into the blood, body temperature rises to subfebrile levels. An old hematoma, when disintegrating, can also raise body temperature.
If the swelling does not disappear for a long time, and the bruise does not change color, you need to consult a doctor. This can occur when bacteria multiply in the cavity formed by the hematoma. If a hematoma appears after a blow to the head, in addition to pain, as a rule, symptoms of damage to the central nervous system are observed: nausea, vomiting, loss of performance. It is necessary to examine the patient for the presence of a concussion or other injuries to the brain or skull.
Also, with internal bruises, dizziness, loss of consciousness, decreased blood pressure, and twitching of small and large muscle groups may occur.
If a child develops a bruise two to three hours after being hit, hemophilia should be suspected and tested for clotting factors.
What does a hematoma look like?
If deeper tissues are damaged, the bruise may become noticeable on the second or third day. Sometimes it appears far from the point of impact.
Depending on the severity of the injury, a tense hematoma may form. This is a blood clot that compresses surrounding tissue. With this type of hematoma, bursting pain, thickening and tension of the muscles, and numbness of the skin are noted.
A hematoma or bruise looks like a spot that changes color over the course of several days. At the beginning of formation, the hematoma has a bright red color, then the spot becomes successively violet, blue, green, yellow and finally disappears completely.
A bruise is dried blood in soft tissue. The color change of the hematoma occurs due to the breakdown of the coloring substance in the blood - hemoglobin.
Classification by severity
Depending on the size of the damage and the patient’s condition, subcutaneous hematoma has four degrees of severity.
- First degree. Hematoma after a bruise or minor injury. Weak hemorrhage of small sizes. The pain is minor, the temperature rises only locally. Color light blue or red. Goes away without treatment after a few days.
- Second degree. The bleeding is more severe, the area of damage increases. Local temperature rises. It hurts and burns slightly at rest. Color blue or dark purple. Without treatment it goes away in ten to fifteen days.
- Third degree. Large size and very intense pain, loss of function of nearby muscles. Raising body temperature to subfebrile levels. As a rule, it occurs when vessels of medium diameter are damaged.
- Fourth degree. Serious condition, severe damage to the skin and underlying structures, very severe pain, high fever. Such damage is most often accompanied by a secondary infection.
There is also a classification based on the lumen of the vessel. The hematoma can be pulsating or non-pulsating. There may be blood clots, blood, pus, or infected blood inside. It is important to prevent the contents from becoming infected.
Why is a hematoma dangerous?
Photo: Pixabay
A strong blow can cause serious damage and lead to serious consequences - traumatic necrosis. Traumatic necrosis is the death of muscles and soft tissues.
The breakdown products of dead tissue enter the bloodstream and cause traumatic toxicosis - poisoning of the entire body. Skin necrosis can develop with extensive skin detachment, which is caused by a blow directed at a tangential surface.
A severe bruise left untreated can lead to the formation of an encysted hematoma. This is a clot of dried blood that is surrounded by connective tissue. The formation of areas of bone tissue in the thickness of the muscles is possible.
Therapy methods
Removing a hematoma using conservative methods takes a lot of time. The body needs a significant amount of energy and resources to break down its own blood at the site of hemorrhage. Also read how to treat a hematoma on the leg after a bruise.
Subcutaneous hematomas without complications should be treated immediately. The first thing to do is apply cold immediately after the injury. Thanks to the cold, the vessel narrows, bleeding stops, and the area of the bruise does not increase. The cold should be kept for about 20 minutes, after which ten-minute breaks should be taken. You can apply a pressure bandage in the area of manifestation.
Non-steroidal anti-inflammatory drugs are used to relieve pain. You should not take Aspirin because it thins the blood.
After a hematoma has formed from the blow, special heparin ointments or bodyagu ointment can be applied for treatment. Such products will speed up the resorption process. Indications for surgical removal of hematoma:
- big sizes,
- severe compression of tissues, muscles,
- suppuration,
- hematomas of internal organs that do not respond to conservative treatment.
The operation is performed immediately if the hematoma threatens the patient’s life, for example, there is compression of the brain or its parts, or compression of large arteries.
You cannot open bruises yourself, as this can lead to infection and continued bleeding.
Traditional methods
Each of us knows several folk ways to get rid of a hematoma. If the hematoma does not resolve for a long time, you can speed up this process with the help of traditional medicine.
Treatment at home can be carried out using a leaf of white cabbage. You need to take a sheet, make cuts and apply it to the bruise overnight. The notches are needed so that the juice comes out better.
To remove an unsightly blue stain, you can use salt lotions. To do this, you need to melt 150 grams of salt in hot water and soak a bandage in it, then apply a bandage for 12 hours.
Onion mixture works great. Chop the onion and add 3 tablespoons of salt to it, stir. Apply 2 times a day to the bruise. Treatment period is up to 5 days.
A mixture of honey and aloe in a 1:1 ratio is very popular. Apply 2 times a day.
Grated plantain leaf has a good effect. Apply the resulting pulp to the site of the hematoma. Also use castor oil lotions.
All folk remedies are aimed at improving blood flow and accelerating metabolic processes, which stimulates faster resorption of blood clots.
How does a hematoma form?
At the moment of impact, a person feels pain, but after a few minutes it noticeably weakens. Then, a swelling begins to develop at the site of the bruise—edema of the soft tissues. Sometimes, swelling forms only 2-3 days after injury.
With serious impacts, small blood vessels rupture and a hematoma is formed at the site of the impact - hemorrhage into the subcutaneous tissue. In common parlance, a hematoma is called a bruise.
Bruises and injuries can be of two types: external and internal. External ones include hematomas, bruises, tumors, and lacerations. Internal – these are closed fractures, dislocations, sprains, displacement of internal organs, damage to internal organs. A hematoma can involve any internal organs and tissues, not just the skin. Its distribution depends on the severity of the injury.
Characteristics and types of hematomas
There are several types - subcutaneous, internal and cerebral hematoma after surgery. The last two species are the most dangerous to human health and life. The symptoms of these types are similar, but treatment for each is selected individually and only by an experienced doctor.
Hematomas after plastic surgery
The symptoms of this disease are easy to notice:
- there is pain and swelling in the area of injury;
- the color of the skin can vary from red to yellow;
- in the case of a hematoma of internal organs, signs of compression appear in this area.
Diagnostics
A hematoma is diagnosed by visual examination. If the hemorrhage is located deep under the skin, in internal organs, or in a joint, it is often very difficult to assess its size and possible consequences.
Patients are prescribed an examination, which may include:
- Ultrasound of internal organs, joints;
- computed tomography and magnetic resonance imaging;
- puncture (puncture with a needle): for example, a puncture of the knee joint is often done if there is a suspicion that blood has accumulated in it after an injury.
Causes
Hemorrhage usually occurs after injury. This could be a bruise of the skin, internal organs, a concussion or bruise of the brain, an injection with thin (sharp) objects. Sometimes blood leaves the vessels and pours into the skin and internal organs as a result of infections, autoimmune diseases, and poisoning. The occurrence of hemorrhages and bruises is promoted by increased fragility of blood vessels, fasting, lack of vitamins in food, high blood pressure, and congenital bleeding disorders.
- Initial consultation – 2,700
- Repeated consultation – 1,800
Make an appointment
Treatment with folk remedies
For small superficial hematomas, you can use traditional medicine recipes that help resolve the hematomas
For small superficial hematomas, you can use traditional medicine recipes that help resolve the hematomas.
- Vodka compress is a remedy for hematomas No. 1. A gauze swab soaked in vodka is applied to the hematoma, then the gauze is wrapped in polyethylene and the compress is left overnight;
- Saline dressings also help with hematomas. To do this, dissolve 2 tablespoons of salt in 100 milliliters of water and soak a gauze cloth in the solution. A bandage is secured to the damaged area with an elastic bandage and left overnight;
- A mixture of mustard powder and radish juice helps resolve the hematoma. The ingredients must be mixed to form a paste. The paste is applied to the hematoma and held until a burning sensation is felt, then the mixture is washed off with water at room temperature. It is recommended to apply such a compress daily until the hematoma completely disappears;
- A compress of vodka and vinegar is also an effective treatment for hematomas. Mix 100 milliliters of table vinegar, 100 milliliters of vodka and 500 milliliters of cold boiled water. A gauze cloth is soaked in this solution and a compress is made from it on the damaged area.
https://youtu.be/NrWp560jrKk
Predisposing factors
The formation of hematomas occurs after injuries, including pinching, blows, squeezing, and bruises. Subarachnoid hemorrhage does not fall into this category, since it does not appear due to trauma, but due to damage to an unchanged vessel. Often small hematomas appear due to eating large quantities of food or drinking alcoholic beverages. This is due to stretching of the gastrointestinal tract and the appearance of cracks.
The development of pathology is influenced by vascular weakness and problems with blood clotting. Often due to a weakened immune system due to infections or age-related changes, the likelihood of pus accumulating in the affected area increases.
Treatment of hematoma
Photo: Pixabay
In case of severe bruise with severe pain and large hemorrhage, hospitalization in the surgical department of the hospital is necessary.
Minor bruises do not require medical attention. The appearance of a hematoma in minor bruises and injuries can be prevented; it is enough to provide first aid correctly.
First aid
Treatment of bruises without serious injuries is reduced to the use of cold in the first hours after the injury. Cold helps to resolve hemorrhage and reduce pain. An ice pack or a towel soaked in cold water should be applied to the injury site.
- To reduce pain and to make the bruise disappear faster, you need to apply a pressure bandage to the injured area. It will reduce subcutaneous bleeding from damaged capillaries.
- To reduce bleeding from bruises and other injuries, you need to apply a cold lotion or some cold object to the bruised area as soon as possible.
Previously, to resolve the hematoma, starting from the second day, it was recommended to start thermal procedures. Currently, doctors insist on longer use of cold - up to 3 days.
Thermal treatments (heating pads, warm baths) and then massage, physiotherapy should be used later.
After removing the tight bandage, you should take anti-inflammatory drugs (aspirin) and painkillers for some time.
Under no circumstances should you hover your leg or arm - this will only aggravate the injury. Bruises and bruises should not be smeared with iodine. Iodine causes even greater blood flow and swelling.
First aid
Before treating a soft tissue hematoma after a bruise, first aid should be provided:
- It is necessary to check that there is no damage to the musculoskeletal system. This is not difficult to do: you need to move your fingers, joints, bend over/unbend. If acute pain occurs or there is no movement, the help of a doctor is required.
- Cold is applied to the bruised area - ice, meat from the freezer, a cold compress. This reduces the intensity of pain and prevents the formation of a hematoma. One subtlety should be taken into account: cold is applied to the injury site for no more than 15 minutes. Then you need to remove it for 20 minutes and perform the procedure again.
- On the 2nd day after the injury, an iodine mesh is applied to the hematoma area. If movement is limited and there is no pain, massage is performed.
Only after providing first aid should treatment of a hematoma from a blow to the arm, leg or other parts of the body be performed. This can be done using pharmacy and home remedies.
How to distinguish a hematoma from an ordinary bruise?
How to distinguish a hematoma from an ordinary bruise?
There are certain signs of a hematoma that make it possible to distinguish it from an ordinary superficial bruise:
- sharp pain occurs in the area of the hematoma;
- a tumor appears at the site of injury;
- the muscles stop functioning normally and mobility is limited;
- the local temperature rises, that is, the skin becomes hot to the touch.
Hematomas during pregnancy
A hematoma during pregnancy is called retrochorial and poses a threat of miscarriage or the development of pathologies in the baby. A woman experiences accumulation of blood behind the chorion due to rejection of the fertilized egg from it. Symptoms of this phenomenon are expressed by unpleasant sensations and nagging pain in the lower abdomen and brownish discharge.
The causes of retrochorial hematoma are as follows:
- Excessive physical activity during pregnancy;
- Hormonal changes;
- Adverse environmental influences;
- Severe stressful situations;
- Presence of uterine malformations;
- Chronic endometritis;
- Infectious inflammatory processes;
- Genital infantilism and others.
Retrochorial hematoma usually appears early in pregnancy, approximately during the first 8 weeks. Discharge indicates not only the presence of a deviation, but also that the hematoma is resolving. In any case, only a doctor can accurately determine the source of the problem using ultrasound. At this stage, the main task is to stop its growth.
Hematoma during pregnancy can only be treated in a hospital. The patient is prescribed drugs that improve blood clotting. Modern means do not have a negative effect on the baby. In order to relax the muscles, No-shpa is indicated, and to activate the hormones necessary for the normal course of pregnancy, vitamin E is required. It is very important to normalize the activity of the nervous system, so valerian is useful for pregnant women.
To treat this type of hematoma, the patient must periodically donate blood for clotting. Diet therapy is also indicated to avoid stagnation in the intestines. If you consult a doctor in a timely manner and provide assistance, there is a high probability of maintaining the pregnancy and normalizing the condition of the expectant mother.
Degrees of bruises
Bruises can be single or multiple. Depending on the severity, the following degrees of damage are distinguished:
1st degree - mild bruises, accompanied by the appearance of small abrasions and wounds. Recovery occurs on its own within 3-4 days.
2nd degree - moderate bruises, characterized by the appearance of edema and hematomas. The person may feel sharp pain. In this case, special treatment for bruises is not provided. As a rule, applying a pressure bandage is sufficient. In case of blood formations under the skin, you should consult a doctor.
Grade 3 - damage to muscles and tendons, likelihood of dislocation. Such injuries can be dangerous if there is injury to the knees, head, or tailbone. An examination by a specialist is required to determine further treatment.
Grade 4 bruises can lead to disruption of the functioning of all human systems and organs. The doctor determines the type of treatment and the need for surgical intervention.
Intra-articular hemorrhage
The flow of blood into the joint cavity is typical, most often, for the knee joints, less often for the ankle joints. Hemarthrosis with bruises of the lower extremities is not as characteristic a hemorrhage as with sprains/ruptures of ligaments or meniscus injuries. In most cases, an immediate direct blow leads to an increase in the production of intra-articular fluid - synovitis. Most often, hemarthrosis in the lower extremities occurs when jumping from a height onto straight legs.
Clinically, the accumulation of blood in the joint cavity is difficult to determine. Even the presence of cutaneous and subcutaneous hematomas on the projection of the joints does not provide exceptional reliability. Hemarthrosis can only be diagnosed by puncture - by drawing synovial fluid mixed with blood into a syringe.
Treatment of intra-articular hemorrhages is carried out conservatively (joint puncture does not apply to surgical procedures). Based on the overall severity of the injury, inpatient or outpatient care of the victim is determined.
Intracranial hematomas
Intracranial hematomas are divided into the following types:
- Epidural.
- Subdural.
- Intracerebral.
- Intraventricular.
Epidurals appear in 1-3% of cases and are due to injury to the middle meningeal artery. Pathology is often observed with skull fractures or depressed fractures. A hematoma develops in 2-3 hours or within 24 hours. Lack of treatment leads to coma. The first symptoms are confusion and weakness. Children rarely lose consciousness after a severe blow. Significant swelling of the brain does not lead to the detection of a light gap (which is rare in adults).
Subdurals appear in 1-7% of cases and pose a threat to human life, since death occurs in 60% of cases. There is an acute, subacute and chronic form of the pathology. Bleeding occurs due to a rupture of a vein or artery in the damaged area. People report nausea and severe headaches. Symptoms characteristic of compression of the brain stem are often observed. Lack of treatment and worsening symptoms lead to coma.
Intracerebral are observed extremely rarely with severe traumatic brain injuries. The light gap is not visible, the development of pathology occurs quickly. Hemiplegia or hemiparesis often occurs, as well as extrapyramidal symptoms.
Intraventricular diseases are rarely diagnosed due to the serious condition of patients. There are acute disturbances of consciousness, an increase in body temperature, a decrease in heart rate, and an increase in blood pressure. To establish a diagnosis, a survey of close people is carried out, since the patient is unconscious. To establish the location of the hematoma, CT or MRI is used. In the most severe cases, lombal puncture is used.
Causes of hemorrhages (hematomas)
Most cases are associated with internal bleeding from trauma. This can be an injury from a blow, fall, pinching, pressure or other impact. Only in the subarachnoid subtype the cause is not only trauma, but also damage to the vein and aorta of a non-traumatic nature.
In some cases, small hematomas are formed against the background of diseases of the internal organs. With Mallory-Weiss disease, cracks occur in the gastrointestinal tract due to vomiting from overeating or alcohol intoxication.
Factors contributing to the occurrence of hematomas: poor permeability of the walls of blood vessels, their excessive fragility and poor blood clotting. When the body's immune systems are reduced due to old age, physical exhaustion, and chronic illnesses, the risk of hematoma infection increases.
WHEN YOU SHOULD SOUND THE ALARM, THE FIRST SYMPTOMS OF HEMATOMA
A hematoma gives its symptoms and signs almost immediately after injury.
- Firstly, the skin at the site of the hematoma is sharply painful.
- After a short period of time, the site of injury begins to swell, the tumor can spread significantly and interfere with movement (for example, with a hematoma on the ankle, the swelling may be such that it is impossible to move independently or step on the affected leg).
- After swelling, the site of hemorrhage quickly turns red. Patients feel internal tension in the area of the hematoma; it is hard to the touch.
The color of the hematoma can be different - from bright red to purple, most often it is heterogeneous - its edges are darker, bluish in color, and the inside of the hematoma is red.
Soft tissue hematomas
Soft tissue hematomas are divided into 3 types:
- Lungs - appear 24 hours after injury and are accompanied by mild pain. No special treatment is required.
- Medium - appear within 5-6 hours and are accompanied by pain and swelling. The motor function of the limb deteriorates. Consultation with a traumatologist is required.
- Heavy - formed within 2 hours after tissue damage. The function of the limb is impaired, acute pain and diffuse swelling are observed. You should immediately consult a doctor to determine a treatment strategy.
Immediately after the injury, swelling appears, and the skin acquires a purplish-bluish tint. After 5 days, the skin takes on a green tint as hemoglobin breaks down. Gradually, the hematoma resolves and “flows” down.
If there are no complications, the hematoma will resolve on its own. In the worst case, a hard area appears that causes discomfort and impairs motor function. When an intramuscular lump forms, external symptoms are rarely observed, but the limb swells significantly and an area forms inside, the touch of which causes severe pain.
When large lumps form, surgical intervention is required. Treatment is carried out by a traumatologist. The opening of infected seals is performed by a surgeon after a comprehensive diagnosis. The operation is performed on an outpatient basis, but for large hematomas hospitalization is required. An autopsy is performed, during which blood clots are removed and washing is carried out. Drainage and suturing are required. Sutures are not applied only for infected hematomas. Antibiotics are often prescribed in combination to eliminate the infection.