Varicose veins of the small pelvis in women are the most pressing problem of our time. Several decades earlier, when humanity did not yet know many of the benefits of civilization, such pathologies were much less common. Passive rest, spending most of the day at the computer, using a car - all these factors have become a good help for the emergence of new health problems in people.
Enlargement of the veins in the pelvis is a pathology caused by a decrease in the elasticity of the vascular walls. This disease is called differently in medicine. The disease affects both males and females.
Medical definition of disease
There is hardly a person who has not heard about varicose veins of the small pelvis in men and women. You can diagnose this pathology in the lower extremities yourself - the affected veins of the extremities are clearly visible through the epithelial covers.
In contrast, deformed pelvic veins cannot be seen or felt - they are located deep under the skin, making themselves felt only through indirect symptoms.
Dilated veins in the pelvis differ from varicose veins of the lower extremities in that they are located in the pelvic cavity - the patient will not be able to see and evaluate their condition.
Consequently, it becomes more difficult to suspect that you have a disease. VRVT leads to the structure of the vascular walls being disrupted, the elasticity of the veins decreases, and the blood flow begins to work worse. This leads to stagnation of blood in the pelvis.
To put it simply, blockage of the vessels passing through the pelvic cavity begins, the veins swell, and blood clots form at the site of stagnation.
Varicose veins of the small pelvis have another name - pelvic venous congestion. Some sources interpret this term as “female varicocele.”
However, this approach is not entirely correct. The fact is that varicocele implies the participation in the process of testicular veins, which, by definition, cannot be present in a woman. However, the symptoms of both pathologies are still similar.
Some researchers are accustomed to calling this venous disease chronic pelvic pain, which is also correct. The syndrome in question can be a consequence of many inflammatory processes (gynecological and urological diseases). Expansion of the veins in the pelvis itself often leads to ARVMT.
Causes and risk factors
By varicose veins of the pelvic organs in women, doctors understand a change in the structure of the vascular walls characteristic of other types of disease - weakening, followed by stretching and the formation of “pockets”, inside which blood stagnates. Cases when only the vessels of the pelvic organs are affected are extremely rare. In approximately 80% of patients, along with this form, signs of varicose veins of the inguinal veins and vessels of the lower extremities are observed.
The incidence of varicose veins of the pelvic vessels is most pronounced in women. This is due to anatomical and physiological features that suggest a tendency to weaken the venous walls:
- hormonal fluctuations, including those associated with the menstrual cycle and pregnancy;
- increased pressure in the pelvis, which is typical for pregnancy;
- periods of more active filling of the veins with blood, including cyclic menstrual periods, during pregnancy, as well as during sex.
All of these phenomena fall into the category of factors provoking varicose veins. And they are found exclusively in women. The largest number of patients are faced with varicose veins of the small pelvis during pregnancy, as there is a simultaneous layering of provoking factors. According to statistics, varicose veins of the small pelvis are 7 times less common among men than among the fairer sex. Their set of provoking factors is more diverse:
- hypodynamia - maintaining low physical activity for many hours;
- increased physical activity, especially dragging heavy objects;
- obesity;
- lack of sufficient fiber in the diet;
- inflammatory processes in the organs of the genitourinary system;
- sexual dysfunction or conscious refusal of sexual activity.
A genetic predisposition can also lead to pathology of the plexuses located inside the pelvis. According to statistics, varicose veins of the perineum and pelvic organs are most often diagnosed in women whose relatives suffered from this disease. The first changes in them can be observed in adolescence during puberty.
The greatest risk of developing inguinal varicose veins in women involving the pelvic vessels is observed in patients with vein pathology in other parts of the body. In this case, we are talking about congenital weakness of the veins.
Symptoms of the disease
Like any other pathology, varicose veins of the pelvic organs have their own characteristic signs. If you discover any of the following about yourself, then you need to consult a doctor:
- Varicose veins of the pelvis and symptoms of pathology may include chronic pain. Most often, discomfort is localized in the lower abdomen, groin or lower back. In women, the pain syndrome manifests itself more intensely in the second phase of the cycle, after making love or overworking the legs.
- Varicose veins of the pelvic organs in women are almost always accompanied by sexual discharge. This symptom applies exclusively to female symptoms. The color and consistency of the discharge do not alarm the patient in any way. However, their excessive abundance may indicate a pathological process.
- Varicose veins of the internal organs of the pelvis also manifest themselves externally in 50% of cases. For example, patients notice a clear venous pattern in the hip area. If we are talking about men, then they may see an increase in the size of the veins passing through the genital organ.
- One of the manifestations of pelvic varicose veins in women may be disruptions in the menstrual cycle and frequent urination. The last sign indicates that the disease is in an extremely advanced state.
Varicose veins of the pelvis: symptoms
The symptoms of the disease are varied and complex. Its manifestation is often confused with signs of pathologies of adjacent systems and organs of the body. A characteristic feature of the signs of this pathology is the prevalence of manifestations of one of the forms.
Signs of vulvar varicose veins include:
- Significant expansion of veins in the vulva or perineum. There is a feeling of itching, discomfort, heaviness. The labia are swollen, and the veins on their surface are enlarged and dilated. The appearance of hemorrhoids is possible.
- Spontaneous or post-traumatic bleeding.
- Thrombophlebitis of the perineal veins, as a complication of this type of varicose veins. Severe pain, swelling and discoloration of the skin in the perineum are felt. Veins are hard and painful. Their inflammation is also possible.
Against the background of such symptoms, there is a high probability of developing fear of sexual contact, feelings of anxiety and irritability. A woman develops dysfunction of the reproductive system, which can lead to infertility.
Hyperemia syndrome manifests itself:
- Constant pain in the lower abdomen with possible irradiation to the lumbar spine, sacrum, perineum or groin. They can be of varying intensity and nature. Their intensification is provoked by immobility and excessive physical activity.
- Dyspareunia. The appearance of pain is possible directly both during sexual intercourse and after its completion. Hyperesthesia of the skin of the perineum and vaginal mucosa is observed.
- Premenstrual syndrome. Pronounced manifestations of pain are observed in the second phase of the cycle. Painful menstruation, dysmenorrhea, and increased vaginal discharge are also possible.
- Urination disorder. Evacuations are accompanied by severe pain and are frequent.
The symptoms of pelvic varicose veins are very extensive and can be of any intensity. It can be complex or manifest itself according to one sign. The manifestation of the slightest signs of pathology requires immediate consultation with a doctor. Neglecting the symptoms of varicose veins can lead to the development of serious complications.
Possible consequences of pathology
In addition to discomfort and pain with varicose veins of the small pelvis, the disease carries with it a lot of other dangerous consequences. This vascular pathology can be corrected quite easily if you seek help in time. Otherwise, the patient will face a number of changes, many of which are irreversible.
The main problem lies in the difficulty of diagnosing the disease. This is influenced by insufficient awareness of the problem among the population, poor knowledge of the disease, vague and significant symptoms.
All of the above leads to the fact that many patients do not even realize that they have a problem. Meanwhile, the pathology progresses and provokes the following consequences:
- Inflammation of the pelvic organs involves neighboring parts in the destructive process - vascular thrombosis in the genital organs begins to develop. For example, enlarged veins on the penis in men, varicose veins of the legs.
- Depending on the cause of pain in the pelvis, the woman’s reproductive organs begin to lose their functionality. A woman may experience infertility or miscarriage. Childbirth with varicose veins is difficult.
- The expansion of the veins in the pelvis in women also affects the psycho-emotional state of the patient. Neurological or nervous system disorders are possible.
- If there are varicose veins in the pelvis and treatment is delayed, the process becomes chronic. Due to frequent exacerbations, both partners may experience discomfort and pain during intimacy.
- The rarest phenomenon that makes ARVMT dangerous is thrombus formation in the respiratory organs - the lungs. This consequence is fatal in almost 100% of cases.
How is diagnosis carried out?
You cannot do without diagnostics and consultation with a specialist. Particular attention is paid to differentiation from such diagnoses as uterine fibroids, endometriosis, and organ prolapse. To confirm the verdict, the area of reflux is identified.
Taking this into account, consultations with a doctor include:
- vaginal examination,
- Ultrasound,
- Dopplerography of blood vessels,
- transuterine venography,
- hormone testing.
When diagnosing IVMT in women, the list also includes laparoscopy and CT (computed tomography). Ultrasound is informative using both abdominal and transvaginal sensors. Doppler examination of blood vessels allows us to establish the nuances of blood circulation in internal structures.
With the help of phlebography, the functional ability of the veins and the current features of local blood flow and pathology of the pelvic floor are identified. CT scans are prescribed only in situations that require a more precise diagnosis. For example, it is introduced to neutralize other pathologies localized in this area (postoperative neuropathy, inflammation of the bladder or large intestine).
How dangerous is IVMT during pregnancy?
For pregnant women, the pathology can be dangerous. This threatens a difficult birth with critical consequences. Thinning vein walls are prone to injury and even rupture, causing pain and bleeding.
One of the common pathologies of the pelvic veins is the likelihood of blood clots that block the vessels, aggravating or creating obstacles to the usual supply of blood to the placenta. This leads to aging of the placenta and oxygen starvation of the fetus. At stages 1 and 2 of pathology, childbirth usually occurs naturally.
Specialists will monitor blood pressure indicators, ensuring their reduction and the introduction of blood thinning drugs (venotonics). Severe (3rd) degree of IVMT requires a cesarean section, and infertility may develop in the future.
Medical diagnosis of pathology
According to studies by American scientists conducted at the beginning of the last century, only 1% of patients with varicose veins of the pelvic organs were diagnosed the first time.
Quite often, misdiagnosis led to the need to remove reproductive organs from women. This would not have happened if internal varicose veins had been diagnosed using the following methods:
- Ultrasound examination and Dopplerography of veins make it possible to suspect pelvic inflammation at its earliest stages; duplex scanning and venography - a surgical examination that allows you to accurately confirm or refute the presence of a problem;
- laparoscopic scanning of the veins is an indispensable study for the comprehensive diagnosis of ARVMT; it can be used to recognize the disease among other female diseases;
- Ovariography using the selection method allows you to assess the condition of the venous walls by injecting a special substance into the vessels, it allows you to determine URVMT up to degree 2;
- computer diagnostics has the most positive reviews in identifying pelvic varicose veins; This type of examination makes it possible to see in detail the process of the disease.
With this method, it is almost impossible to confuse pelvic varicose veins with other pathologies that have a similar clinical picture.
VVMT degrees
Three successive degrees (stages) of development of venous expansion in the pelvic area are identified.
- I degree - the veins increase to five mm in circumference, tend to expand in the upper part of the left ovary. All this is associated with acquired or genetic valvular insufficiency of the structure.
- II degree – the veins reach a girth of up to 10 mm, involving the left ovary. Additionally, varicose veins of the uterine veins and the right ovary are formed.
- III degree – the veins thicken by more than 10 mm. Varicose veins of the right and left ovaries are approximately proportionate. This is associated with gynecological pathologies – neoplasms.
Basic therapy
In such a matter as the treatment of pelvic varicose veins, the basis consists of correcting your diet. To begin with, women with ARVMT should understand that even Detralex will not be as effective as it should be if you do not refuse to work in hazardous work.
If there is such an opportunity, then it is better to switch to easier work - excluding excessive physical exertion and heavy lifting.
If you have to sit or stand for long periods of time during your workday, give yourself 5-minute breaks every half hour. At this time, you can simply walk or lie down, or you can do therapeutic exercises.
High-quality treatment of varicose veins is also not possible without changes in the diet. It is necessary to completely remove fatty and fried foods, smoked foods and preserves from the diet. Eat as little citrus fruits as possible, try to use seasonings less often when cooking.
Add more natural products - fruits and vegetables - to your daily menu. Instead of animal fats, eat vegetable ones - they contain a large amount of vitamins E.
If the pelvic veins are painfully dilated, it is necessary to wear special compression garments. We are talking about tights or stockings, which help normalize blood circulation in the vessels and also eliminate fluid stagnation in the veins.
In addition to all of the above, women with ARVMT should practice anti-varicose veins every day. It includes the following exercises:
- swimming in a pool or open water with clean water;
- morning jogging;
- cycling;
- roller skating or ice skating.
A daily shower will also help tone your veins. Water the area of the hips, abdomen and buttocks with jets of different temperatures.
Classification
Depending on the severity of the condition, three degrees of the disease can be distinguished:
- The affected vessels have a diameter of up to 0.5 cm. In this case, any of the vascular plexuses can be dilated.
- If the width of the veins is from 0.6 to 1 cm, then they speak of the second degree of varicose veins. In this case, pathology is noted in the ovarian plexuses, vessels of the parametrium or myometrium. A total change in the vascular walls cannot be ruled out.
- The diameter of the venous branches of more than 1 cm indicates the last, third degree. In this case, the disease is widespread.
Drug therapy
If pelvic vein disease is in the initial stages of development, you can try to cope with it with the help of medications. The extent of the lesion can be determined by ultrasound (ultrasound examination of the pelvic veins).
Pelvic varicose veins are quite common during pregnancy. If a woman is about to give birth, it is necessary to stabilize her condition as early as possible. The following groups of drugs will help with this:
- anti-inflammatory ointments that improve lymph flow;
- phlebotonics that improve the tone of the venous walls;
- ointments that prevent the formation of blood clots and relieve pain;
- sorbents that remove waste from the intestines;
- antioxidants are drugs that normalize cellular and energy metabolism. Contain a large amount of vitamins.
Popular drugs - venotonics for pelvic varicose veins:
- Detralex helps improve the tone of vascular walls and normalizes the lymphatic drainage of fluid. Detralex must be taken for six months.
- Phlebodia has the same principle of action as Detralex. In addition, it reduces the distensibility of blood vessels, removes blood stagnation in the veins, and has a positive effect on overall blood microcirculation. Phlebodia quickly copes with inflammation if you take the drug regularly for 2 months;
- Troxevasin (release form - ointment, suppositories, tablets) - is applied topically, the course of treatment is 3 months. Using the product, you can treat vulvar vessels and perineal veins.
How are varicose veins of the pelvis treated?
If symptoms of varicose veins of the small pelvis occur in women, treatment should begin as early as possible. The main direction of therapy is to restore vascular tone, strengthen their walls and improve blood flow in the pelvic area.
For pelvic varicose veins, treatment is prescribed and monitored by a phlebologist. If varicose veins of the small pelvis are detected in women during pregnancy, treatment is carried out by a phlebologist and gynecologist.
Treatment of the disease requires an integrated approach. It includes several treatment methods:
- Conservative influence. Consists of regular and long-term use of medications. Using this method, it is possible to cure pelvic varicose veins at an early stage, when the vessels have partially lost their tone.
- Non-drug therapy. Consists of following a daily routine and doing exercises. The method is considered auxiliary, although reducing the risk of further progression of varicose veins depends on it.
- Surgery. It is used when other methods are ineffective, as well as when the disease is detected in late stages.
Drug therapy involves taking several groups of medications that can not only eliminate unpleasant symptoms, but also improve the condition of the veins:
- Phlebodia, Troxevasin and Detralex are venotonics that are designed to improve venous outflow;
- Curantil is a drug that reduces blood density, which is prescribed to prevent thrombosis;
- Wobenzym is a complex remedy for reducing unpleasant symptoms and strengthening blood vessels;
- Aescusan is a herbal preparation intended to reduce swelling and eliminate the inflammatory process;
- Ascorutin is a complex with vitamins designed to strengthen venous walls.
Almost all venotonic drugs for pelvic varicose veins are not recommended to be taken during pregnancy. If symptoms progress, the doctor may prescribe them in minimal dosages from the 12th week of gestation.
Surgical intervention for varicose veins in the pelvic organs is considered a last resort. It is used in the absence of positive dynamics with long-term use of drugs. The surgical treatment methods used may differ depending on the location of the vessels damaged by the disease:
- if only the internal veins are affected, ligation of the ovarian vein is performed;
- when varicose veins of the pelvic organs are combined with varicose veins of the perineum, the surgeon performs ligation of the vena cava;
- when varicose veins are combined in the pelvis and lower extremities, a crossectomy is performed.
Before and after the intervention, women must undergo a course of medication, wear compression garments and adhere to a strict diet aimed at losing weight.
Prevention
Preventing exacerbations and reducing the risk of progression are as important as therapeutic measures. It involves performing exercises for varicose veins of the pelvis and following a special diet. With their help it is possible to:
- reduce weight, that is, reduce the load on blood vessels;
- improve blood flow;
- reduce the likelihood of blood clots;
- reduce the risk of other complications.
The set of exercises for varicose veins of the small pelvis can include the classic “Birch” and “Scissors with legs”, “Bicycle” and raising on toes from a standing position. Such loads stimulate the outflow of blood from the pelvis, strengthen the pelvic floor muscles, which helps reduce the swelling of the veins. It is necessary to perform gymnastics for varicose veins of the small pelvis regularly, preferably every day in the morning and evening.
Features of the diet for pelvic varicose veins include the inclusion in the diet of foods high in fiber and vitamins (mainly groups B, A, C, Omega-3 and Omega-6). Fiber is necessary to improve intestinal function and eliminate congestion in the abdominal and pelvic organs. Vitamins are necessary to strengthen the walls of veins and reduce blood viscosity. To meet their needs, the diet includes:
- whole grain cereals - buckwheat, brown rice, millet, oats;
- vegetables and fruits, berries and fruits, citrus fruits;
- skinless chicken or turkey fillet;
- seafood, white and red fish, seaweed;
- green tea, freshly squeezed juices, compotes.
You need to eat in portions, giving preference to boiled, stewed and baked dishes, salads from fresh vegetables.
Surgical intervention
If the patient was diagnosed with varicose veins at a fairly late stage, therapy with folk remedies, as well as various gymnastics for varicose veins, will no longer have an effect sufficient to completely get rid of the problem.
Prompt resolution of the issue is carried out only in extreme cases. As a rule, doctors insist on surgery if even such strong drugs as Detralex do not help. In addition, for surgical treatment there must be the following indications:
- low effectiveness of conservative treatment;
- the last stage of the inflammatory process;
- inability to relieve acute pain in any other way.
There are several effective methods of surgical treatment of the disease. The choice depends on the location of venous reflux:
- ligation of the affected ovarian vein (access to the peritoneum is opened or laparoscopy is performed);
- scleroobliteration - a substance is injected into the affected vein that glues the venous walls (the intervention is carried out under local anesthesia);
- resection of diseased veins (partial removal);
- complete removal of veins (used in case of perineal vascular inflammation);
- correction of thrombotic veins using a laser or radio wave technique;
Causes of the disease
Pathology occurs when the functioning of large main veins that collect blood from the genital organs is disrupted. Also, the disease often occurs from a uniform weakening of the entire venous network of the small pelvis. Most often, the causes of the disease are hereditary predisposition and the presence of connective tissue dysplasia. The latter causes underdevelopment of the vascular wall and a gradual decrease in its density.
The following reasons can also cause varicose veins:
- severe hormonal disruptions, hormone-dependent ovarian tumors and other dishormonal diseases;
- pregnancy and childbirth (due to increased pressure in the pelvis);
- gynecological diseases - endometriosis, chronic endometritis, previous surgeries;
- physical labor, high sports loads;
- obesity;
- sedentary work;
- lack of orgasms, especially for many years;
- abnormalities in the position of the uterus - backward bending, prolapse.
Symptoms of varicose veins
The likelihood of varicose veins can be determined only by two characteristic symptoms:
- development of chronic pain in the lower peritoneum, intensifying during sexual intercourse, physical activity, before menstruation and during pregnancy;
- increased vaginal discharge.
Vulvar varicose veins
With ordinary vulvar varicose veins, the expansion of the veins is noticeable visually. There are complaints of discomfort, powerful bursting pain felt in the genitals. Examination reveals swelling of the labia. Sometimes spontaneous bleeding is added; it is usually provoked by childbirth or sexual intercourse.
Venous congestion syndrome
With this type of varicose veins, the clinical picture is very polymorphic, so the problem is often accepted as an inflammatory pathology. A constant sign of the problem is pain in the lower peritoneum, changing intensity, places of irradiation, and character. Usually they are aching, radiating in the perineum or lower back.
Causes
The pathology is caused by the following reasons:
- heredity;
- hormonal imbalance;
- abortions;
- lack of treatment for inflammation;
- disruption of the menstrual cycle;
- pathology of vascular valves;
- pathologies of the hematopoietic system;
- bend of the uterus.
Provoking factors
In addition to the main reasons, there are factors that provoke the likelihood of such an illness:
- overweight;
- the need to stand or walk for a long time;
- poor physical activity;
- use of shapewear;
- sexual dysfunction;
- frequent births.
Folk remedies
To alleviate symptoms and speed up the recovery of affected veins, the use of traditional medicine is allowed. However, you should not use natural medicines without first consulting your doctor.
List of effective recipes:
- Chopped ginger (4 tbsp) and lemon zest are poured with boiling water (1 l). After cooling, honey (2-3 tbsp) is added to the infusion. The drink is used instead of tea.
- Horse chestnut (200 g) is crushed and filled with vodka (1 l). The product is infused for 7 days in a dark place. Recommended dosage: 10 drops 3-4 times a day for a month.
- Chopped branches of oak, willow and chestnut (1 tbsp each) are poured into a pan, poured with boiling water (1 l) and placed on low heat. Half an hour after boiling, the broth is removed from the stove and cooled. Next, chamomile, string, cudweed and St. John's wort are added to it (1 tbsp each). Infusion period is 12 hours. You need to add a little honey to the strained medicine.
Dosage regimen for the decoction: the first 2 days – 3 times 50 ml, the next 2 days – 100 ml, later the dosage increases to 150 ml. The duration of therapy is 20 days, after which a break is taken for 10 days.
To improve the condition of blood vessels, it is useful to consume blueberries daily, as well as pollen.
When using folk remedies, it is important to understand that they only complement the main course, so it is not advisable to refuse medications prescribed by a doctor.
Other means to combat the disease
In addition to drug treatment, you can combat the problem with the help of physical therapy, as well as wearing special compression garments. In this case, compression tights will be useful, as they will improve blood flow in the legs and, as a result, partially in the pelvic organs.
Considering beneficial physical activity, it is important for women with this problem to do at least the “scissors”, “bicycle”, “birch” exercises every day. Breathing exercises and a contrast shower on the upper legs and pelvic area are also useful. However, full-fledged gymnastics is a quick path to a normal and healthy life. Simple but effective exercises:
- Lying on your back, stretch your legs, then bend them and pull them towards your chest. Do this 5 times.
- Again, lying on your back, raise your legs up, then bend them, then lift them again. And so on several times.
- Lie on your stomach, lifting each leg up in turn. In the highest position, the leg should be fixed for a couple of seconds. You need to do at least 5 approaches for each leg.
- You will have to walk around the room for 15 minutes. First - on your toes, then - on your heels, and then - raising your knees high.
Symptoms and photos
Varicose veins in the pelvis have specific symptoms. Frequent signs of vasodilation in women are:
- Irregularities in the menstrual cycle also indicate varicose thickening of the veins of the female pelvic organs.
- Increased sensitivity of the skin in the perineum, sensitivity of the vaginal mucosa.
- Severe intermittent or constant pain. It often becomes more intense during menopause or after ovulation.
- Vaginal discharge: colorless or slightly white.
- Pain in the last stage of pregnancy, during sex or towards the end of the day.
- In the presence of varicose veins, there is a slight swelling of the vagina and vulva.
- Heaviness, pressure on the pelvic area is another possible symptom of varicose veins.
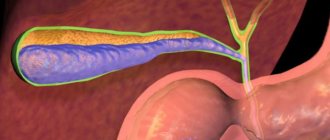
The photo below shows how the disease manifests itself in women.
Diagnostics
The symptoms characteristic of pelvic varicose veins are for the most part similar to the symptoms of various gynecological diseases. When making a diagnosis, you should not exclude them, since they can occur against the background of circulatory disorders.
The examination, which will be carried out in a medical institution, includes the main stages:
- Examination on a gynecological chair.
- Ultrasound of the pelvic organs. For a more thorough examination of the condition of the pelvic organs, ultrasound can be recommended using two sensors: abdominal and transvaginal. When examining the structure of blood vessels, dilated veins will be found in the form of numerous connections in which the blood flow process will be multidirectional and weak.
- Dopplerography to determine the condition of blood vessels. Examination of the condition of blood vessels using the Doppler ultrasound procedure helps to determine in detail the existing deviations in vascular formations in a specific area.
- Phlebography, which allows you to assess the condition and level of functioning of the veins, as well as determine the existing features of blood flow.
- Laparoscopy.
- CT scan. Prescribed as an additional study if it is necessary to clarify the diagnostic results.
A detailed examination using several approaches allows you to confirm the accuracy of the diagnosis and eliminate the possibility of an erroneous conclusion.
Conservative treatment
Due to the internal location of the veins affected by the disease, medications are prescribed orally; it is not possible to use venous gels and ointments. The following means are used:
- Diosmin (detralex, phlebodia) - to eliminate increased elasticity of blood vessels, reduce their permeability, and prevent fragility;
- Horse chestnut extract (escusan) – to relieve swelling and inflammation;
- Troxerutin (troxevasin) – to improve the outflow of blood from damaged vessels, increase the tone of the veins, reduce swelling and inflammation;
- Vitamin C (ascorutin) – to strengthen the walls of blood vessels.
Experts recommend combining drug therapy with physical therapy and wearing special compression garments. There is a special need for compression garments during pregnancy.
Prognosis and possible complications
The most favorable prognosis for treatment will be in the initial stages of ARVMT. If the disease develops for a long time, accompanied by characteristic symptoms, it can often be dealt with only through surgical intervention.
Thanks to medications, it is possible to reduce the discomfort caused by deformation of the veins, as well as reduce the risk of undesirable consequences.
Patients should know that even surgery does not guarantee the absence of relapses. If a man continues to lead his previous lifestyle, the disease is most likely to return.
In other words, you can count on good results from treatment if:
- timely completion of therapy;
- strict adherence to medical recommendations;
- correction of behavioral habits.
If the venous vessels of the small pelvis are affected by varicose veins, the patient runs the risk of getting:
- infertility;
- deterioration of spermatogenesis indicators;
- diffuse changes in the prostate parenchyma;
- erectile dysfunction.
Due to the deformation of blood vessels, the likelihood of blood clots forming and their migration, thromboembolism, up to rupture of the vein with massive hemorrhage increases. Such complications are fatal for the patient (occur in 5% of cases).
Diet
The basis of treatment and preventive measures should be built on the basis of the rules of a balanced diet and following recommendations for a healthy lifestyle.
In case of pathology in the pelvic area, special attention should be paid to the normal functioning of the intestine. To do this, it is recommended to ensure the presence of cereals and fiber in the daily diet. To start the regeneration process in the walls of blood vessels, you should eat protein foods.
General recommendations to follow:
- Reduce or completely eliminate the consumption of fried, fatty, smoked, and too salty foods. Such food provokes fluid retention and the appearance of edema, which can aggravate the condition and increase discomfort and pain.
- Reduce your consumption of sweets.
- Consume dairy or fermented milk products daily.
- Saturate your body with vitamins by eating vegetables and fruits.
Varicose veins of the pelvis very often occur in women who are overweight. This is another reason why it is recommended to adhere to the principles of proper nutrition. Particular attention should be paid to products that have a beneficial effect on blood circulation and tone the walls of blood vessels: pineapples, seaweed, pine and nutmeg, ginger, honey.
Therapeutic stage of treatment
The main goal of therapy for pelvic varicose veins is to restore blood flow and normalize the tone of elastic tissues. No less important are the stages of relieving unpleasant symptoms of the disease and increasing blood circulation in the veins.
Medicines for varicose veins should only be prescribed by a phlebologist. There are two groups of medications prescribed for this disease. The first (venotamics) improves the tone of venous tissue, and the second (angioplatelet agents) prevents the formation of new blood clots.
Only a doctor can prescribe medications for treatment
In general, drugs for varicose veins contribute to:
- Stopping the reverse flow of blood;
- Normalization of venous tone;
- Help supply tissues with blood;
- Reducing discomfort from disease symptoms.
It should be remembered that the use of medications must be combined with special exercises and a prescribed diet.
Treatment
The necessary treatment methods are prescribed individually based on examination data. For mild cases, lifestyle changes may be effective. For more severe cases, surgical intervention cannot be avoided. Conservative methods are effective for I-II degrees of pathology:
- pharmacological therapy (NSAIDs, antiplatelet and venoactive agents);
- physical therapy classes;
- contrast shower twice a day;
- wearing compression stockings;
- correction of physical activity;
- changes in working conditions;
- hemostatic therapy (for uterine bleeding).
The necessary treatment methods are prescribed individually based on examination data.
Patients often experience severe discomfort and have certain psychological problems, which negatively affects the success of therapy. In this case, sedatives and consultations with a psychotherapist are prescribed.
The presence of stage III disease and pain that is not relieved by conventional painkillers are indications for surgical intervention. Today surgery offers minimally invasive techniques:
- Scleroobliteration.
- Embolization of the uterine arteries.
Such operations are performed under angiographic control, that is, using a special contrast agent. The essence of the intervention is obliteration or occlusion of the vein, which is achieved through the introduction of a sclerosant drug or an embolization coil. An alternative to these techniques may be vein resection, plastic surgery of the uterine ligaments, or endoscopic clipping. The choice of method by which surgical intervention will be performed is determined by the localization of the pathology and its etiology.
Patients often experience severe discomfort and have certain psychological problems.
We will now live in a new way
And of course, lifestyle changes are necessary. Required:
- Increase physical activity. Good results are obtained from therapeutic exercises, in particular, performing exercises such as “Birch”, “Bicycle” and “Scissors”, walking in place on toes, on heels, with knees raised high. Swimming is ideal for preventing relapses.
- Get enough sleep and maintain a work-rest schedule. When working sedentarily, get up and move every half hour.
- Avoid stress that disrupts hormonal balance.
- Avoid visiting saunas, beaches, solariums. Instead of a bath, take a contrast shower every day, irrigating the inner surfaces of the thighs, perineum and lower abdomen.
- Give up bad habits (smoking and drinking alcohol).
- Drink at least 2 liters of clean water per day and change your diet. Avoid foods high in saturated fat, sweet, spicy and salty foods. Increase the proportion of fiber (vegetables, fruits, grains) and healthy fats (vegetable oils, nuts).
Possible complications
Without treatment, the inflammation will spread to other organs.
Varicose veins of the pelvic organs can cause serious complications for the female body, this is especially dangerous in the later stages of the disease. Sometimes the inflammation spreads to neighboring organs; uterine bleeding looks more frightening.
For better protection, you should understand the dangers of pelvic varicose veins. Frequent bleeding in the uterus can contribute to the formation of thrombosis, as well as develop into an extensive inflammatory process.
Treatment of varicose veins
To get rid of a pathology, it is not enough to eliminate its symptoms. It is important to influence the causes of the disease. Dilatation of parametric vessels involves an integrated approach to therapy, including the following methods:
- medications;
- treatment with folk remedies;
- a set of exercises for the legs and pelvis;
- surgical intervention;
- special procedures.
Return to contents
Medicines
Varicose veins of the pelvic vessels are dangerous because their cause is usually hidden. The doctor prescribes the medicine based on the individual needs of the patient. Selecting medications on your own is dangerous to your health. Advanced parameters involve the use of several groups of tools:
- phleboprotectors - drugs to relieve inflammation and improve lymphatic drainage;
- phlebotonics - improve blood flow;
- antiplatelet agents - minimize the risk of blood clots;
- non-steroidal anti-inflammatory drugs - relieve pain;
- enterosorbents - eliminate gastrointestinal toxins;
- membrane protectors - prevent oxidative processes.
Exercises for VRMVT
Treatment of varicose veins of any degree involves performing gymnastics. This technique does not mean that normal vessel sizes will immediately appear, but such measures will improve the condition. It is recommended to do the following exercises:
- "Birch". The hip joint lifts off the floor and the legs are raised in an extended position.
- "Bike". The patient lies on a flat surface and with raised lower limbs imitates a ride.
- "Scissors". The patient raises his legs and crosses them in the air.
- Leg pull-up. The patient lies on his back and presses his knees bent to his stomach.
- Move on your toes, heels and different sides of your feet.
It is also recommended to take a contrast shower for the ovarian zone, perineum, and thighs.
Traditional medicines
Ectasia of the pelvic vessels is eliminated using traditional methods only in the case of stages 1-2 of the development of the pathology, in which the veins are enlarged to non-critical sizes, which is determined by the diagnosis. The following means are considered effective:
- Kombucha infusion;
- tincture of horse chestnut fruit;
- hirudotherapy (leech therapy) in the areas of the sacrum and coccyx;
- infusion based on dandelion roots.
Return to contents
Vein surgery
Stage 3 varicose veins of the pelvic organs can only be eliminated through surgery. In addition, an indication that surgery is necessary is severe pain, which cannot be relieved with traditional medications. Type of intervention:
- ligation of the vein surrounding the ovaries;
- injection of a special painkiller into the venous cavity;
- removal of ovarian veins (partial);
- removal of blood vessels for vulvar varicose veins;
- vein clipping surgery;
- ligation of the saphenous vein.
Return to contents
Procedures for illness
To effectively influence varicose veins of the internal organs of the pelvis, additional influence is necessary through special procedures, including:
- wrap with oils, clays and algae;
- relaxing baths and baths;
- douches and contrast showers;
- electrophoresis;
- massage.
Return to contents
Degrees of pathology
There are three degrees of development of varicose veins:
- Mild degree - damage to one or more peripheral vessels of the genital organs. Most often asymptomatic, may be temporary, requiring repeated examination.
- Medium degree - dilation of large veins of the parametrium (outer lining of the uterus) or myometrium (muscular lining). Causes menstrual irregularities and poor health.
- Severe degree – varicose veins and swelling of most organs of the female reproductive system. Serious sexual dysfunction, high risk of disease and infertility.
To standardize diagnosis and attempt a differential approach to treatment, A.E. Volkov classified pelvic varicose veins depending on the diameter of the dilated vessels and the localization of venous ectasia.
There are 3 degrees of this disease:
- 1st degree - vein diameter up to 5 mm (any venous plexus of the small pelvis), “corkscrew-shaped” course of the vessel;
- 2nd degree - vein diameter 6-10 mm with total type of varicose veins, loose ectasia of the ovarian plexus (pl.pampiniformis ovarii), VR of the parametric veins (pl.uterovaginalis), VR of the veins of the arcuate plexus of the uterus;
- 3rd degree - vein diameter
Prevention
Varicose veins can be prevented by following simple measures. You must adhere to the following rules:
- eliminate hard work;
- move more;
- do not sit in one place for hours;
- lead a healthy lifestyle;
- eat more fruits and vegetables;
- take vitamins that affect the condition of blood vessels;
- promptly treat chronic diseases of the genital organs;
- give up weightlifting.
If signs of varicose veins appear, you should immediately visit a doctor. You need to wear compression stockings and take medications that strengthen blood vessels. These medications are taken for several months, otherwise there will be no effect. Thus, varicose veins of the pelvic organs are a common pathology among women.
Classification of pathologies
Congestive syndrome (dilated pelvic venous system) is divided according to several characteristics:
- According to the form of the course: Primary veins are dilated - an increase in pelvic blood vessels caused by genetic pathology or valvular insufficiency that has developed as a result of changes in the body.
- The secondary form is dysfunction of the gynecological system.
- dilation of the veins surrounding the vulva (in advanced cases, the flow affects the vessels on the thighs and perineum);
Return to contents
Surgery
Surgical treatment of varicose veins of the pelvis is carried out according to strict indications:
- ineffectiveness of conservative therapy;
- 3 degree of disease;
- inability to relieve pain.
Various surgical techniques are used depending on the location of reflux and venous conglomerates:
- ligation of the ovarian vein (through retroperitoneal access or laparoscopy);
- scleroobliteration of ovarian veins under the control of hagiography (a sclerosing substance is injected into the lumen of the vein, the operation is performed under local anesthesia);
- resection (partial removal) of ovarian veins through retroperitoneal or laparoscopic access;
- clipping of ovarian veins laparoscopically;
- phlebectomy (removal of veins) for vulvar and perineal varicose veins;
- laser and radiofrequency coagulation;
- crossectomy - ligation of the great saphenous vein and its tributaries - with a combination of varicose veins of the perineum and lower extremities.
Varicose veins of the pelvis in women
Statistics show that varicose veins of the small pelvis, or as it is also called chronic pelvic pain syndrome, usually affects young women - 20-45 years old. Moreover, with age, the number of women suffering from this disease increases many times. So, at the age of 17 years, 19% of women suffer from varicose veins of the small pelvis, and by the age of 45 their number increases to 80%, the statistics are disappointing.
What leads to such a huge increase in the number of patients with age? Let's omit cases where the cause of the disease is a hereditary predisposition (genetically determined special structure of blood vessels and valves, causing their tendency to overstretch). And let's talk about the reasons that we encounter throughout our lives.
First of all, this is a sedentary lifestyle. A long, static stay in one position, when you have to sit or stand for a long time, disrupts venous outflow and leads to stagnation of blood in the vessels of the lower part of the body, to CVI (chronic venous insufficiency). The valves in the varicose veins of the small pelvis can no longer close tightly and leave a gap between them. A clot begins to form in such a vessel, which can subsequently turn into a thrombus.
The second factor causing the risk of developing varicose veins of the pelvic vessels is pregnancy. During it, the amount of blood in the circulatory system increases significantly, the uterus begins to compress the retroperitoneal veins, and the hormonal background changes. All this leads to persistent vasodilation and further development of pathology.
What are the dangers of pelvic varicose veins during pregnancy? There is no direct danger; childbirth with pelvic varicose veins occurs without complications, so it is not treated. This is an expansion of the veins of the perineum and vulva and is observed in 30% of women. However, immediately after the birth of a child, these vessels often quickly return to normal without any intervention, and as a result, pelvic varicose veins persist after childbirth in only 2-8% of women.
The third reason for the development of varicose veins of the pelvis is the presence of gynecological diseases, the use of hormone replacement therapy and contraceptives. The fourth, important factor is smoking. We especially note that simultaneous use of hormonal contraceptives and smoking are unacceptable. These two factors mutually reinforce each other. And there are many tragic cases where young, smoking women who took hormonal birth control pills died from vascular thrombosis. Another risk factor is excess body weight. Obesity significantly increases the load on blood vessels. The last predisposing factor is considered to be ecology; air pollution in large cities increases the risk of developing vascular pathologies.
These were the causes of varicose veins of the pelvic organs. But how can you recognize the presence of this pathology? The main symptoms of varicose veins of the small pelvis:
- the appearance of aching pain in the lower abdomen, intensifying after the body is in one position for a long time, as well as when lifting heavy objects, hypothermia and general fatigue;
- painful sensations in the perineum during or after sexual intercourse;
- pain with varicose veins of the small pelvis often accompanies premenstrual syndrome;
- increased amount of vaginal discharge;
- menstrual irregularities;
- the venous pattern on the buttocks and back of the thighs becomes more pronounced,
- The external genitalia may also be affected - nodes, thickening, itching, soreness.
What to do if you discover symptoms of pelvic varicose veins?
If you notice such symptoms, you should immediately consult a doctor to avoid complications. The first doctor a woman with the symptoms described above should contact is a gynecologist. After the examination, he will prescribe all the necessary tests and studies. As a rule, patients with suspected varicose veins of the internal organs of the pelvis first need to undergo an ultrasound examination of the abdominal organs to exclude gynecological diseases (also, on ultrasound, the doctor will be able to see the presence of pathological, dilated and tortuous vessels).
After ruling out the presence of gynecological diseases, the patient is referred to a phlebologist. To clarify the diagnosis, they may be prescribed ultrasound duplex scanning of blood vessels (USDG), which allows them to obtain more detailed information about blood flow. In difficult cases, computed tomography (CT), magnetic resonance imaging (MRI) and laparoscopy may be prescribed. Usually, these studies are sufficient to make a final diagnosis and determine the extent of the disease.
Degrees of varicose veins of the small pelvis:
- The diameter of the veins does not exceed 5 mm, the affected vessels are located along the upper edge of the left ovary.
- Diameter is from 5 to 10 mm, the vessels of the right ovary and uterus are affected.
- The diameter of the veins is more than 10 mm, you can see pronounced varicose veins in both ovaries (vessels are equally dilated on both the left and right) and the uterus; dilated veins and nodules are observed in the thighs, buttocks, and groin.