What doctors don't see with microscopy?
1) Cancer of the uterus and cervix.
To diagnose malignant degeneration of the endometrium, histological material is needed, and in large quantities. 2) Pregnancy. To determine it, a smear is not needed and it does not matter what result it shows. It is necessary to take a blood test for hCG, undergo a gynecological examination by a doctor, or do an ultrasound of the uterus.
https://youtu.be/1KAY1iz3HhA
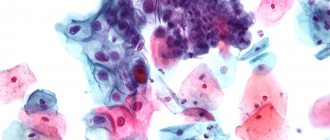
3) CC and other pathologies (erosion, leukoplakia, koilocytosis, HPV infection, atypical cells, etc.) are diagnosed based on the results of a cytological examination.
This analysis is taken directly from the cervix, from the transformation zone, using a certain method with Papanicolaou staining (hence the name of the analysis - PAP test). It is also called oncocytology.
The first four infections are diagnosed using the PCR method. And it is impossible to determine the presence of the immunodeficiency virus from a smear with high accuracy. You need to take a blood test.
Bacterial culture of urogenital smear
As you know, candidiasis (thrush) is caused by yeast fungi of the genus Candida. Thrush is indicated by the detection of fungal spores and mycelium during microscopic examination of a smear.
It is worth noting that a microscopic examination of a smear can only reveal the presence of yeast-like fungi, but does not determine the type of microorganism. This information can be obtained using a bacterial smear culture.
Bacterial culture of a smear is a study during which the collected material is placed on a special nutrient medium. Within several days, active reproduction of existing microorganisms, in particular fungi, occurs.
Bacterial culture allows you to determine the number of yeast fungi. The diagnosis of thrush is confirmed when the number of fungi exceeds 104 CFU/ml. In addition, culture of a urogenital smear makes it possible to determine which type of fungus caused candidiasis, as well as which antifungal drugs will be most effective.
This is especially important in case of chronic candidiasis, when a woman is treated with all kinds of drugs, but they turn out to be ineffective and the disease returns again and again.
To obtain reliable results, a woman must follow the rules of preparation for the procedure:
- A urogenital smear is taken before starting treatment with antifungal and antibacterial drugs;
- It is recommended to refrain from urinating for three hours before the procedure;
- Two days before the manipulation, refrain from sexual contact;
- For two days, completely avoid douching, the use of vaginal suppositories and ointments;
- The study cannot be taken during menstruation, only three days after the end.
After confirming the diagnosis of thrush, the doctor prescribes appropriate treatment for the woman. Fourteen days after completion of the course of treatment, a repeat bacterial culture of the urogenital smear may be required.
Grigorova Valeria, medical observer
Treatment
Therapy for pseudomycelium is absolutely identical to the destruction of Candida fungus. For these purposes, modern pharmacology offers a wide selection of drugs:
- Polyenes: “Nystatin”, “Levorin” destroy Candida fungus.
- Allylamines: “Terbinafine”, “Naftifin” - drugs for the treatment of skin fungus and onychomycosis.
- Azoles: “Ketonazole”, “Bifonazole”, “Miconazole”, “Oxinazole” - drugs with a wide antifungal spectrum.
At the beginning of infection with a fungus, local preparations are limited. If the number of pseudomycelium and blastospores is significant, treatment with systemic antifungal drugs is necessary . Most often, doctors prescribe:
- “Clotrimazole”;
- “Fluconazole”;
- “Pimafucin”;
- “Nystatin.”
The doctor prescribes a set of specific medications and their treatment regimen.
If the selection is incorrect, the fungus will develop resistance to fungicidal substances, then treatment will be ineffective and candidiasis will become chronic.
IMPORTANT! The detection of pseudomycelium is not only evidence of Candidiasis, but also a signal of decreased immunity. To maintain the body’s defenses, it is necessary to drink immunostimulating drugs (“Immudon”, “Immsunal”), prebiotics to normalize the intestinal microflora (“Lactofiltrum”, “Hilak Forte”, “Acipol”).
The meaning of the letters on the analysis form
Usually a vaginal smear is part of a woman's routine medical check-up. It is performed by a specialist during a gynecological examination. Biological material is also collected from the urethra and cervix.
This diagnosis allows you to detect possible problems with women's health, such as an inflammatory process or a disease caused by an infection.
A smear is taken when planning pregnancy and after antibiotic therapy. In addition, the smear allows you to monitor the effectiveness of therapy in the treatment of gynecological diseases.
Advantages of the method:
- Painless procedure.
- Simple rules for preparing for a smear test.
- Monitoring the effectiveness of treatment of female diseases.
- Possibility of identifying many diseases of the genitourinary system.
For preventive purposes, women periodically need to undergo this diagnosis. This will help prevent possible undesirable consequences.
The analysis is most often taken by a doctor when you come to him for a regular appointment at the clinic or when you simply go to a paid laboratory, where obstetricians and medical staff take biomaterial from you.
In men, a urologist or another doctor inserts a special disposable probe into the urethra, turns it around its axis several times and takes an analysis. It is believed that the examination does not cause pain, however, this does not exclude the carelessness of the doctor, as well as individual sensitivity or the presence of a particular disease, which can cause discomfort.
Doctors do not use full names, but abbreviations - the first letters of each of the analysis parameters. To understand the normal microflora of the vagina, knowledge of the letter designations will be very helpful.
MORE ABOUT: Dilution of ceftriaxone with lidocaine and water
So, what are these letters:
- abbreviations of the areas from which the material is taken are designated by the letters V (vagina), C (cervical area of the cervix) and U (urethra or urinary canal);
- L - leukocytes, the value of which may not be the same in normal conditions and in pathology;
- Ep - epithelium or Pl.Ep - squamous epithelium;
- GN - gonococcus (the “culprit” of gonorrhea);
- Trich - Trichomonas (the causative agent of trichomoniasis).
In the smear, mucus may be detected, indicating a normal internal environment (PH), beneficial Doderlein bacilli (or lactobacilli), the value of which is equal to 95% of all beneficial bacteria.
Some laboratories make it a rule to mark the content of a specific type of bacteria. For example, somewhere they use the “ ” sign for this.
If there is no flora in the smear, the abbreviation “abs” is indicated (Latin, this type of flora does not exist).
- When to get tested for candidiasis
- Diagnosis of candidiasis
- Types of analyzes
- Polymerase chain reaction
- Linked immunosorbent assay
- Sowing for Candida albicans
- Preparing for tests
A woman at any age can face the problem of candidiasis - known to most people as thrush. The disease provokes a several-fold increase in Candida fungi, which are normally found in the vaginal microflora of every woman.
This disease poses the greatest danger to pregnant women. Because during this period the body is weakened and any disease is much more difficult to treat. But there is also a risk of fetal infection.
Every woman is at risk of encountering the problem of thrush. But you should only visit a doctor to diagnose thrush if you have the following symptoms:
- itching;
- curdled discharge;
- pain when urinating;
- sour milk smell of discharge.
It is necessary to undergo examination for the presence of Candida fungi in the presence of the following diseases: vaginitis, urethritis, vulvitis, cystitis. Modern diagnostic techniques make it possible to determine which fungus provoked the development of thrush.
Many women put off visiting a gynecologist out of fear that diagnosing thrush is a difficult and painful process. And all because they don’t know how to identify thrush.
All their fears are unfounded, because in most cases a simple smear is enough to detect candidiasis. This procedure allows you to determine the presence of fungi in the vaginal microflora.
Candida fungi detected during a smear confirm the presence of thrush in a woman. Testing for thrush gives the doctor complete information about the disease.
Therefore, if symptoms of the disease appear, you should not self-medicate, but rather visit a gynecologist and undergo the necessary tests. An accurate diagnosis will allow you to get rid of candidiasis as quickly and painlessly as possible.
Types of analyzes
In addition to the simplest way to diagnose candidiasis using a vaginal smear, there are other methods for determining thrush. PCR, enzyme immunoassay, and culture for Candida albicans are used.
Because these two methods allow you to most accurately identify the type of fungus. Each of these types of research has its pros and cons. What they all have in common is that they are painless.
Only a doctor can decide which thrush test a patient should undergo. Most often, several types of tests are prescribed simultaneously; this is necessary to increase the accuracy of the diagnosis.
One of the effective laboratory tests is PCR. This type of analysis allows you to detect DNA or RNA of yeast fungi in the patient’s biomaterial. The material for the study is venous blood.
This type of study is carried out to determine the number of albicans fungi. It is worth noting that this fungus is most often the causative agent of candidiasis. With this analysis, material taken from a woman is compared with the genes of the fungus and the most accurate number of fungi in the microflora is obtained.
It is rightly considered an informative and accurate analysis. It is almost impossible not to detect candidiasis using this method, because not a single fungal cell will go unnoticed.
During this laboratory test, the concentration of immunoglobulins (proteins) in the blood plasma is determined using biochemical reactions. The main task of these proteins is to neutralize fungi.
To conduct this type of research, material is taken from a place where fungi accumulate and placed in a nutrient medium. If the material taken contains Candida fungi, then once in an environment favorable for them, they will begin to multiply.
MORE ABOUT: What does a smear at a gynecologist show?
Soon they will be visible even without special devices. To select treatment, several drugs are applied to fungal colonies and it is observed which of them will kill the fungi.
The accuracy of the analysis depends not only on the type of study, but also on how prepared the patient was for it. To get an accurate result, a woman will need to prepare in advance.
biomaterial (smears) from the vagina, venous blood, urine and feces. Most often, patients are prescribed a smear, urine and stool test. In this case, a week before the date of the study, the patient must stop taking any medications.
An accurate diagnosis cannot guarantee effective treatment and quick recovery if the patient does not adhere to the doctor's recommendations. Therefore, her recovery depends only on the patient herself.
What does pseudomycelium mean on a smear?
Pseudomycelium is formed by some species of yeast. The appearance of pseudomycelium in a smear in men and women indicates an increased proliferation of Candida albicans - single-celled microorganisms of round or oval shape.
Pseudomycelium is a thread of loosely interconnected elongated cells with blastospores - a kind of “buds” attached to the constrictions of the pseudomycelium.
In such cases, in addition to pseudomycelium, the smear may also contain some types of chlamydospores.
Candida differs from ordinary yeast:
- absence of spores in the cellular structure of microorganisms;
- characteristic cultural characteristics;
- presence of pseudomycelium.
The disease provokes an increase in the amount of the opportunistic microorganism Candida, which is part of the normal microflora of the intestines, vagina and mouth (a smear reveals pseudomycelium only in cases of thrush during an exacerbation).
Candidiasis can develop due to the active proliferation of the fungus or as a result of more pathogenic strains entering the body.
In most cases, the cause of thrush in women and men is a general or local decrease in immunity.
Video:
Thus, candidiasis often appears regardless of the sexual partner - under the influence of stress, as a result of decreased immunity or due to the use of antibiotics. Candida occurs even in young children.
Women exposed to the fungus may develop balanoposthitis, balanitis and vulvovaginal candidiasis.
Opportunistic microflora is also transmitted through sexual contact, so if one of the partners has pseudomycelium in a smear, then in order to avoid relapse, both should undergo treatment procedures, regardless of the severity of the symptoms.
Women should also undergo a smear test during and at the planning stage of pregnancy to reduce the likelihood of transmitting infection to the fetus.
In addition, while carrying a child, immunity is greatly reduced, and all the “hidden sores” can actively manifest themselves.
Testing for pseudomycelium is also recommended for those who have been treated with corticosteroids or antibiotics.
Flora smear during pregnancy
The microflora of each woman is strictly individual, and normally consists of 95% lactobacilli, which produce lactic acid and maintain a constant pH of the internal environment.
But opportunistic flora is also normally present in the vagina. It got its name because it becomes pathogenic only under certain conditions.
This means that as long as there is an acidic environment in the vagina, opportunistic flora does not cause any inconvenience and does not actively multiply. These include yeast-like fungi, which under certain conditions can cause vaginal candidiasis, as well as gardnerella, staphylococci, streptococci, which under other conditions can cause bacterial vaginosis (inflammatory process) in a woman.
A woman's flora can change for a variety of reasons - with decreased immunity, taking antibiotics, common infectious diseases and diabetes.
One of these factors that can change the microflora is a change in hormonal levels. Thus, a pregnant woman produces virtually no estrogen until the end of pregnancy, but produces the hormone progesterone in large quantities.
This hormonal background allows Doderlein's rods to increase 10 times, so the body tries to protect the fetus from possible infection during pregnancy.
Therefore, it is very important to undergo an examination before a planned pregnancy to determine the degree of cleanliness of the vagina. If this is not done, then during pregnancy the opportunistic flora can be activated and cause various diseases of the vagina.
Candidiasis, bacterial vaginosis, gardnerellosis, gonorrhea, trichomoniasis - this is not a complete list of diseases that weaken and loosen the walls of the vagina.
This is dangerous because ruptures may occur during childbirth, which might not have happened if the vagina was clean and healthy. Diseases such as mycoplasmosis, chlamydia and ureaplasmosis are not detected by smear analysis, and these pathogenic microorganisms can only be detected by blood analysis using the PCR (polymerase chain reaction) method, using special markers.
A smear test is taken from a pregnant woman during registration, and then for monitoring at 30 and 38 weeks. Usually, to assess the state of the vaginal microflora, doctors talk about the so-called degrees of vaginal cleanliness, which a woman should know and ensure that the required degree is maintained during pregnancy.
When is pseudomycelium detected in a smear?
The body is a complex system where each person normally has many other microorganisms – bacteria and fungi – that are necessary to ensure the proper functioning of the organs.
Together, all microorganisms - normal and opportunistic - create a special microflora. In order for human health to remain in order, it is necessary to maintain a balance between all components of the microflora.
A smear is one of the diagnostic procedures used in gynecology and urology to detect the presence of pathogenic fungi or bacteria.
A flora smear is one of the most popular and effective types of laboratory microscopic analysis. The smear allows you to evaluate the amount of opportunistic microflora based on characteristic features.
In the genital organs of women, the microflora is mainly represented by lactobacilli, which maintain an acidic environment in the vagina, preventing the development of infection.
One of the most common “female” diseases caused by an imbalance of microflora is thrush (candidiasis), in the presence of which pseudomycelium may be detected in tests.
Smears should be taken for preventive purposes once or twice a year. In addition, both men and women must undergo testing if discomfort or unusual discharge occurs.
In women, thrush is characterized by:
- unpleasant, pungent odor;
- painful sensations that appear during sexual intercourse or when urinating;
- the presence of white cheesy discharge;
- itching and burning on the surface of the genitals.
In men, candidiasis is usually asymptomatic.
But sometimes they appear:
- mucus excreted in urine.
- pain during urination and sexual intercourse;
- white plaque in the folds at the head of the penis;
- redness of the skin in the genital area;
- burning and itching sensation in the area of the foreskin and glans penis.
READ Abnormalities in the flora smear during pregnancy
Tests can reveal the presence of pseudomycelium in the smear or detect other pathological manifestations.
Evaluation of results
During a microscopic examination of the smear, the laboratory technician determines the number and ratio of microorganisms (bacteria, fungi), as well as cellular elements (leukocytes, epithelial cells).
What indicators are the norm?
- Leukocytes - the norm in the vagina is 0-10 cells in the field of view, in the cervix - 0-30, in the urethra - 0-5;
- Epithelium - moderate amount of squamous epithelium;
- Mucus - in moderation;
- Gram-positive rods (Gr.), Doderline rods, lactobacilli are normally found in large quantities in the vagina, but are absent in the cervix and urethra;
- Gram-negative rods (Gr.-), gonococci (gn.), Trichomonas (trich), chlamydia, yeast fungi, as well as key cells are normally absent.
MORE ABOUT: Culture of prostate secretion for flora and sensitivity to antibiotics
Epidemiology [edit | edit code]
Most people encounter Cand mushrooms >[5] .
The possibility of infection of the fetus is confirmed by the detection of fungi in the amniotic fluid, placenta, and umbilical cord membranes. In the future, contact of newborns with Candida
can occur during the passage of the birth canal, with the mucous membrane of the mouth, with the skin of the nipple during feeding, the skin of the hands during care, as well as with food or household items.
Significant contamination of raw meat, dairy products, as well as vegetables and fruits with these fungi has been revealed. The source, in addition to carriers, can be young domestic animals (calves, puppies, foals), as well as poultry. Read more Bloody pimples on the testicles
The manifestation of candidiasis is mentioned as a common side effect that occurs when using powerful broad-spectrum antibiotics that are active against many gram-positive and gram-negative microorganisms [6] [7].
Preparation for delivery
Some doctors say that this test does not require special preparation, however, this is not true. To ensure the reliability of the results, the patient is advised not to go to the toilet for 2-3 hours, since urine can wash away all pathogenic bacteria and infections, making it difficult for the attending physician to determine the causes of your pathological condition.
Douching, vaginal suppositories and antibacterial soap also contribute to unreliable indicators. Women must undergo this test after the end of menstruation, and in addition, all patients should refrain from any sexual intercourse 2 days before taking the biomaterial.
Microscopic examination of a urogenital smear includes the determination of cellular elements (leukocytes, epithelial cells) and bacteriological examination to identify bacteria and yeast fungi.
This diagnostic method is familiar to all women. However, not everyone knows how to properly prepare for research. A woman needs to remember that a smear can be taken only two days after sexual intercourse, as well as diagnostic procedures (colposcopy, transvaginal ultrasound).
During menstruation, a urogenital smear is not taken, which means you will have to wait until it ends. It is optimal to take a smear on the fifth to seventh day after the end of menstruation.
It is not recommended to urinate two to three hours before the procedure. On the eve of the procedure, you should not douche or use antiseptics. In the morning, just wash with water and dry with a clean towel.
Where can I get tested?
You can undergo the necessary examination at the clinic at your place of residence. To get results quickly and without queues, you can contact any medical clinic with its own laboratory, for example, Invitro. Tests for thrush in Invitro include the following types of studies:
- determination of antibodies to candidal fungus (serological blood test);
- DNA determination in scrapings of epithelial cells;
- culture to determine the fungal flora, identifying the type of pathogen and determining its sensitivity to antifungal drugs;
- INBIOFLOR (typing and screening).
It is necessary to contact a specialist immediately after the first signs and symptoms of pathology appear. It is recommended that women undergo screening for candidiasis once a year. If a couple is preparing to conceive, both partners should undergo examination - this will increase the chances of a successful pregnancy and the birth of a healthy child.
Smear procedure
During the manipulation, the gynecologist uses a special spatula to alternately take smears from the urethra, cervix and posterior vaginal fornix. Before the manipulation, two glass slides are prepared, each of which is divided into three parts and marked with the letters “U”, “C”, “V”. What do these letters stand for?
- “U” stands for urethral; the doctor applies a smear from the urethra to this part of the glass;
- “C” stands for cervical; the doctor applies a smear from the cervix to this part of the glass;
- “V” stands for vaginal, and the doctor applies a vaginal swab to this part of the glass.
Next, the selected material is transferred to the laboratory, where a laboratory assistant stains one piece of glass with methylene blue and the other with Gram stain. When the pieces of glass are dry, they begin to study them in detail under a microscope.