Varicose veins are a disorder in which prominent blue veins appear just under the skin. Of course, we are accustomed to the fact that varicose veins most often appear on the legs, but this disease can also affect other parts of the body.
Our body has a very interesting cardiovascular system. In order to transport oxygen to all tissues and organs from the heart to every part of the body, strong arteries are distributed, which are equipped with good muscles. But with veins everything is different. They use nearby muscles to direct blood back to the heart , and one-way valves work inside the veins to keep blood from flowing back. When the valves open, blood moves towards the heart, when they close, a barrier is created to prevent the blood from flowing back.
Prominent blue varicose blood vessels, often resembling a curved river, surrounded by a network of characteristic arachnoid-like capillaries, indicate superficial varicose veins.
Although they can be painful and unsightly, in general, superficial varicose blood vessels are considered harmless .
When these veins become inflamed, they become sensitive to touch and can impede circulation, causing symptoms such as:
- swelling;
- itchy skin;
- pain.
In our lower extremities, in addition to the superficial veins, there is also a developed internal venous system . In rare cases, varicose veins appear on the internal veins, causing pain throughout the entire affected limb. Due to their anatomical position, these blood vessels are more difficult to diagnose.
Unfortunately, varicose veins can cause blood clots . Inflammation of the internal blood vessels (thrombophlebitis) of the thighs increases the risk of pulmonary embolism, which is often fatal.
Varicose veins are a very common disorder. Some people have a genetic predisposition to developing this disease.
Women suffer from varicose veins twice as often as men. In Western countries, 20% of women and 10% of men suffer from varicose veins.
Medical history
The history of varicose veins began in the times of Byzantium, Ancient Egypt, and Old Testament Israel, as evidenced by archaeological excavations. In different eras, people tried to treat this disease, in particular, Avicenna and Hippocrates did this. In the second half of the 19th century, Russian and German doctors started talking about the effectiveness of ligation of the great saphenous vein.
This is what varicose veins of the lower extremities look like
At the beginning of the 20th century, very traumatic operations were carried out in Russia, during which the tissues of the thigh and lower leg were deeply dissected, veins were damaged, which were then ligated, nerve endings, arteries, and lymphatic ducts. Healing took a very long time, leaving large and noticeable scars.
In 1908, foreign doctors proposed removing the great saphenous vein and introduced a metal probe, which reduced injury to the patient. This was the first step towards minimally invasive surgery.
The breakthrough came when it became possible to take X-rays. It was first performed for varicose veins in 1924. At the same time, contrast based on strontium bromide solution was injected into the vein. Then ultrasound appeared, and the technique was further improved.
In the late 90s of the 20th century, laser therapy appeared, which became a modern breakthrough in the treatment of varicose veins.
Watch our video in which a doctor from Dr. Gruzdev’s clinic talks in detail about what varicose veins are:
Preventive measures for the development of varicose veins
Prevention of this pathological condition is important not only for people with a family history, but also for people with difficult working conditions and with a high body mass index.
As a preventive measure, patients should be provided with an intensive rest regime, but at the same time it is necessary to carry out specialized therapeutic exercises.
The opinion that patients with varicose veins should remain in a horizontal or sitting position for as long as possible is deceptive; to improve venous outflow, it is necessary to allow the muscles to periodically contract.
It is recommended to engage in sports such as running, rollerblading or cycling. During such exercises, the muscles of the limbs will regularly contract and ensure contractility of the muscular wall of the veins. If the necessary measures are taken to correct the underlying disease in a timely manner, the prognosis for recovery will be favorable. Prevention and treatment of the disease must be carried out in a timely manner.
Causes of the disease (etiology)
The main cause of varicose veins is genetic predisposition.
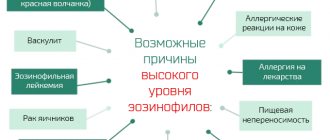
There are a number of other provoking factors:
- sedentary lifestyle;
- pregnancy;
- obesity;
- hormonal disbalance;
- endocrine diseases;
- taking oral contraceptives and other hormonal drugs;
- work in hot shops;
- strong physical activity;
- work that involves standing on your feet for a long time or, conversely, sitting;
- chronic diseases of the bronchi and lungs, accompanied by a prolonged cough.
Why are varicose veins dangerous?
There is an aphorism about varicose veins created by doctors - “A disease that manifests itself on the legs and shoots into the heart.” Indeed, this disease is not just an aesthetic problem that causes trouble and reduces the quality of life. In the absence of qualified medical care, varicose veins are fraught with serious complications, including death.
So, the consequences of varicose veins on the legs can be:
- thrombophlebitis - the disease is accompanied by inflammatory processes in the affected veins;
- bleeding;
- disruption of tissue nutrition;
- increased pigmentation;
- Increased thrombus formation is a dangerous complication not only for health, but also for life.
It is worth mentioning separately about such a common “companion” of varicose veins on the legs as a trophic ulcer. The reason for its appearance is constant venous insufficiency and increased pressure in the veins. Such ulcers, as a rule, do not heal for a long time, they are very difficult to treat and at the same time can limit the patient’s ability to work and even lead to his disability. Swelling, excruciating pain and even an unpleasant odor - all this makes the patient’s life very difficult. Even minor injuries and bruises, which simply cannot be avoided, contribute to the occurrence of trophic ulcers in a person suffering from varicose veins. By the way, sometimes (in rare cases) these lesions degenerate into a malignant tumor.
Symptoms of varicose veins
The first symptoms that appear in the initial stages:
- legs get tired quickly;
- short-term swelling appears;
- there is pain in the veins;
- At night there are cramps in the calves;
- There is a feeling of burning, fullness, heaviness in the legs.
There are no dilated veins in the initial stages, but the disease is already developing. Sometimes this takes decades.
Gradually the symptoms intensify, signs of venous insufficiency appear:
- evening swelling of the legs and ankles, which disappears after a night's rest;
- skin itching;
- nodes visible to the naked eye, varicose veins, pathological tortuosity;
- darkening, thickening of the skin, acquiring a brownish or bluish tint.
As the disease progresses, the symptoms intensify, signs of nutritional deficiency in the legs appear - deterioration in the condition and appearance of the skin, eczema, trophic ulcers.
You can find out the causes of varicose veins in consultation with our specialist.
Addresses of our clinics: St. Petersburg, Manezhny lane, 13 Chernyshevskaya metro station
St. Petersburg, st. Bolshaya Raznochinnaya, 27 metro station Chkalovskaya
Symptoms and first signs
Varicose veins of the legs are accompanied by the following symptoms:
- the appearance of pain in the legs: with varicose veins, the pain is pulsating and hot while walking, and in a calm state it is aching;
- cramps at night;
- visible skin changes on the legs - dark spots, nodules, swelling, dry skin;
- a feeling of heaviness in the legs - as if they were bursting from the inside; Basically, this happens in the evenings, after a working day;
- thickening of the veins on the legs, they clearly appear on the surface of the skin.
The number and intensity of symptoms depends on the stage of the disease - the longer it is left untreated, the more severe the symptoms will be.
Symptoms of the onset and progression of varicose veins in the legs are presented in the photo below; depending on their stage and the patient’s condition, treatment is prescribed.
The photo is not recommended for the faint of heart and minors.
Delayed treatment is very dangerous in case of VVNK. If left untreated, this disease can lead to deformation of the muscle structure in the legs, destruction of bone mass and irreversible changes in the skin.
As varicose veins progress, they will be accompanied by such phenomena as the formation of extensive eczema and the appearance of trophic non-healing ulcers , which can turn into gangrene. The consequences can be very sad - amputation of legs, blood poisoning and even death. But the greatest danger is the possibility of a blood clot, which can break off and lead to death.
Why varicose veins are dangerous: possible complications of the disease
Thrombophlebitis
- life-threatening condition. When it occurs, blood clots form in the veins, which can break off and clog the pulmonary vessels, leading to myocardial infarction. If a large vessel is affected, death is possible.
Venous thrombosis
- blockage of a vessel with a blood clot. It manifests itself as pain in the limb, which intensifies with physical activity, and swelling.
Pulmonary embolism
– blocking of the lumen of the pulmonary artery by a detached thrombus. Death can occur in the first 30 minutes. If the thrombus is small, then a pulmonary infarction occurs and the patient requires resuscitation measures. The condition is accompanied by pneumonia and chronic heart failure.
Trophic ulcers
– compaction of the subcutaneous tissue, darkening and thinning of the skin with the subsequent appearance of ulcers. Such ulcers exist for a long time, do not respond to treatment, and close very slowly.
What can varicose veins lead to?
Main symptoms and signs of varicose vascular pathology
The main symptomatic signs of structural venous disease include:
- pain during prolonged stays in an upright position and when walking;
- regular nocturnal attacks of local convulsive syndrome;
- feeling of heat and burning of the skin in the calf muscles;
- a pronounced feeling of fatigue and swelling of the lower extremities, with a disorder of superficial and deep sensitivity;
- bursting pain both during the day and at night;
- pathological changes in the color and trophism of the integumentary epithelium are manifested by severe dryness of the skin, the appearance of trophic ulcers on the leg and areas of hemorrhage in the area of rupture of damaged venous vessels. Formed ulcers on the skin are difficult to regenerate and are easily susceptible to bacterial infection;
- pronounced deformation and expansion of the walls of venous vessels under the influence of increased pressure. Deformed vessels are visible through the skin with the naked eye.
Risk factors for developing varicose veins
- Heredity.
Weakness of the vein walls is passed on to children. If both parents have varicose veins, then the child has a 90% chance of getting the disease. If only one has 60%. - Pregnancy.
During pregnancy, varicose veins are provoked by three factors:- Changes in hormonal levels - the production of large amounts of progesterone. This hormone relaxes the muscles, so the veins become more vulnerable.
- Pressure of the uterus, which increases in size. In this regard, the outflow of blood from the legs worsens.
- An increase in the amount of blood by an average of 20-30%. Venous valves cannot withstand such stress, especially if they were naturally weak.
- Obesity and simply being overweight
, which is accompanied by lipid metabolism disorders. This process causes vascular pathologies. - Poor nutrition
– predominance of fried foods, fatty foods, fast food, animal fats, milk fats. Uncontrolled consumption of salt and sugar, semi-finished products. - Hormonal background
- a surge in hormone production can weaken the muscle layer of the vein walls, which expands the lumen of the vessel and prevents the normal closure of the valves. - Incorrect clothing
, which negatively affects blood circulation. Pants that put pressure on the waist, tight belts, and too-tight jeans, the fabric of which lacks elasticity, have a negative impact on the condition of the veins. - High-heeled shoes
, which cause the veins to work to the limit. This is due to the fact that the load is unevenly distributed - the main part of it falls on the forefoot, the vessels of which are under too much pressure. Women who wear high-heeled shoes usually note that in the evening their feet hurt, ache, and swell. These are the first signs of beginning varicose veins.
Traditional medicine recipes
- Horse chestnut is a great healer. Firstly, it reduces blood clotting; secondly, it strengthens the walls of capillaries and veins, thereby preventing the formation of blood clots in blood vessels; in addition, it helps to resolve existing blood clots. It is worth remembering that it is horse chestnut extract that has a miraculous effect. An infusion of horse chestnut flowers and fruits also helps well with varicose veins. To prepare it, you need to mix half a liter of vodka and fifty grams of raw materials. Let this solution infuse for two weeks in a dark and warm place, shaking occasionally. After time, this infusion should be taken thirty drops, three times a day. The course of treatment is one month.
- To get rid of this disease, you can drink fresh juice, which is made from chestnut flowers. You need to drink this juice three times a day, twenty-five drops at a time.
- Fresh leaves and flower heads of silver wormwood need to be diligently ground. Add a tablespoon of raw material to the same amount of sour milk, stir properly, then apply an even layer to the cheesecloth. Then apply a bandage to the damaged area of the legs. Treatment should be carried out daily for 5 days, after which it is necessary to take a short break.
- For thrombophlebitis, use the following mixture: fifty grams of yarrow herb, one hundred grams of buckthorn bark, one hundred grams of lingonberry leaves, two hundred grams of immortelle flowers, 100g birch leaves. Brew a full tablespoon of this collection with 300 ml of boiling water and boil for 3 minutes. Then leave to brew in a warm place for 4 hours. Then take the decoction warm, half a glass three times a day, half an hour before meals.
- To prevent the formation of trophic ulcers and in order to reduce the permeability of the vascular wall, it is necessary to prepare an infusion of the following herbs: three parts of chamomile flowers, tricolor violet herb 1 part, horsetail herb 1 part, St. John's wort herb 2 parts, one part yarrow herb, two parts of calendula flowers and one part of oak bark. One tablespoon of this collection should be poured with a glass of boiling water, let it brew for half an hour and strain. This infusion is well suited for lotions, compresses and for washing trophic ulcers.
- Another infusion is famous for its equally effective treatment of trophic ulcers: one part of chamomile flowers, one part of coriander fruits, two parts of St. John's wort, a succession of 2 parts, 1 part of dried grass, 1 part of toadflax herb, one part of medicinal sweet clover herb, one part of licorice root . One tablespoon of this collection should be poured into a thermos, then pour one glass of boiling water and let it brew for 45 minutes, then strain and take half a glass two to three times a day, after eating, for 1-2 two months. .
- Where swollen veins are visible, you need to moisten them with fresh potato juice five times a day; you can also apply bandages to these places, soaked in the same juice. It is advisable to supplement this procedure with drinking infusions of fresh potato juice.
- An excellent remedy for varicose veins is Kalanchoe. For this method, it is necessary to thoroughly wash the leaves of this plant, dry them and finely chop them. Place them in a half-liter bottle until they are half full. Afterwards, they should be filled with hot water and placed in a dark, warm place for the infusion to infuse. Shake the bottle periodically. After a week, strain the infusion. Rub this mixture on your legs from the knees to the feet. In order to get rid of the blue network of small veins, this procedure must be repeated every day for four months. In parallel with this, you can take one teaspoon of pollen orally, three times a day.
- It will be very useful to make whey compresses at night. To prepare it, just moisten a regular cloth in the serum, then wrap it around the sore spot and cover it with compress paper on top. This compress must be kept throughout the night. After it has expired, you must thoroughly wash the damaged area with cool water.
- If you do not have serum, you can make compresses from horse chestnut leaves and chestnut flowers, which must be thoroughly ground. It is worth remembering that such treatment is quite lengthy.
- And with the help of an alcohol tincture of white acacia flowers, you can quickly get rid of swollen venous nodes by moistening the damaged areas with it.
- You can fill a half-liter bottle with birch buds and fill it completely with water. Infuse for ten days in a dark place, shaking the bottle occasionally. It is necessary to lubricate sore spots with this tincture.
- You can also use comfrey root by applying it to swollen veins and trophic ulcers. But it is several times more practical and convenient to use ointment. Comfrey root ointment is prepared as follows: one part of finely chopped comfrey roots and two parts of horse chestnut flowers, mix all this and pour a little vodka. Place in a warm place for half an hour.
- After the time has passed, add three parts of rendered lard to the infusion. Place this entire mixture in the oven for three hours, but under no circumstances allow it to boil. Afterwards, cool, strain and pour into vessels. This infusion must be stored in the refrigerator. This ointment must be applied to damaged areas every day before going to bed. Place a soft linen cloth, compress paper and bandage on top of the ointment. In parallel with the compress, you need to take the following tincture orally: ten drops of this decoction, mixing it with water. Take three times a day, 30 minutes before meals
Where varicose veins can occur: areas of localization of the disease
Lower limbs
The most common localization. It usually appears at a young age, and in women - during pregnancy or after childbirth. In the initial stages, symptoms are few and nonspecific - leg fatigue, heaviness in the legs, burning, bloating, night cramps. Already at the very beginning of varicose veins, pain and swelling appear along the vein. Usually the ankles, legs, and feet are affected.
Upper limbs
The most common symptom in this case is numbness in the hands. It can be partial or complete, most often manifesting itself during sleep. The patient becomes weather dependent, his hands hurt and ache with any weather changes. It becomes difficult to hold even light objects in your hands. Then more characteristic symptoms develop - the vessels swell, nodes form, pain begins, intensifying over time, the veins become tortuous and prominent.
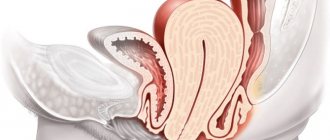
Groin and pelvis
Manifestations of the disease differ in men and women.
Among women
There is itching, swelling of the labia, heaviness in the pelvic organs, and bursting pain. If natural childbirth occurs against the background of varicose veins, bleeding may develop.
The disease can occur in the form of venous congestion syndrome. In this case, there will be pain in the lower abdomen, radiating to the sacrum, groin, lower back, and perineum. Their intensity will vary depending on the phases of the cycle. Pain will occur during intimacy, standing or sitting for a long time.
In men
In mild stages there are almost no symptoms. As the disease progresses, aching pain appears in the lower abdomen and perineum. The pain may radiate to the lower back and intensify during intimacy and after ejaculation. The scrotum and perineum also swell. In the later stages, urination becomes more frequent.
Diagnostics
The ease of diagnosing varicose veins in the legs is exaggerated, since the vessels do not always come to the surface. To confirm the diagnosis, the doctor will have to conduct an external examination and conduct a series of instrumental studies:
- duplex scanning or ultrasound on the lower limb - in case of varicose veins, it is used first to determine the degree of stretching of the vascular walls, the nature of the blood flow in them and the detection of blood clots;
- radiography of the extremities with contrast is the standard of functional examination for varicose veins of the lower extremities, which allows you to determine the patency of blood vessels;
- MRI is the gold standard for modern diagnosis of varicose veins in the lower extremities, which allows you to assess the functionality of venous valves, identify foci of ischemia in soft tissues, detect blood clots and other pathological changes that have arisen against the background of varicose veins.
To clarify the full picture of the disease, laboratory tests are prescribed: a coagulogram to assess the risk of thrombosis, a general and biochemical blood test.
Methods for treating varicose veins
Surgical techniques
A complete cure for varicose veins is possible only after surgical treatment. It can be carried out in three ways:
- Phlebectomy – removal of varicose veins.
- Sclerotherapy is the introduction of a sclerosant into a varicose vein - a special substance that “glues” its walls, stopping blood flow through it. As a result, the vein collapses, even the cosmetic defect disappears.
- Laser coagulation - the walls of the vein are destroyed due to thermal effects, as a result of which the venous lumen is “sealed”. Such an operation can be performed only if the vein is dilated by no more than 10 mm.
Also, one of the most modern methods of treating chronic varicose veins is adhesive obliteration of veins VenaSeal. Follow the link and read more about this procedure.
Drug treatment
Venotonics play a leading role in drug treatment
, which are taken in tablet form and act systemically. They correct disturbances in circulatory function. As a result, the blood vessels of the whole body are healed. Venotonics are also available in the form of gels and ointments, but they are less effective and act only at the site of application for a short time.
Phlebotonics are also used
– venotonic drugs. They are indicated for thinning of the walls of blood vessels, reduced elasticity, increased permeability, and blood stagnation. The drugs strengthen the venous walls, increase their elasticity, eliminate congestion, reduce swelling and other negative symptoms. An additional property of phlebotonics is the normalization of microcirculation in the affected area.
Antiplatelet agents are used to thin the blood
. The drugs are used when it is necessary to reduce the intensity of blood clot formation. Indicated for patients with increased blood viscosity. Antiplatelet agents can be used only if there is no tendency to bleeding.
Anticoagulants are also prescribed to stop the thrombus formation process.
. They destroy blood clots and reduce blood viscosity.
Compression therapy
A good helper in the fight against varicose veins is compression knitwear. The operating principle of such products:
- Throughout the length of the compression stocking, pressure is applied to the superficial and deep veins.
- The greatest pressure is at the bottom, where the veins are most narrowed and the outflow of blood is fastest.
- Thanks to the narrowing of the veins, the efficiency of the valves increases.
- Swelling, pain, and fatigue in the legs go away.
Features of treatment
A phlebologist treats varicose veins in the legs. After determining the degree of pathological changes, the doctor selects the most effective, in his opinion, methods of therapy. Unfortunately, it is not possible to get rid of varicose veins on the legs forever, since the disease is systemic, and even modern treatment methods give a long-term, but not 100% sustainable result.
According to statistics, even after using radical methods of treating varicose veins of the lower extremities, 80% of patients experience a relapse within 5 years.
In the initial stages of varicose veins in the legs, treatment is preferably conservative. It is based on the use of local and systemic drugs:
- anticoagulants that reduce blood viscosity and improve tissue nutrition (Aspirin, Heparin and their analogues);
- antiplatelet agents that reduce the risk of thrombosis and improve tissue trophism (Curantil and its analogues);
- venotonics to prevent further stretching of the veins, reduce inflammation and swelling (Phlebodia, Detralex, Lyoton).
For severe discomfort with varicose veins in the legs, NSAIDs are prescribed: paracetamol, ibuprofen, diclofenac. Drugs in this group help reduce pain and prevent the development of complications.
What to do if itching with varicose veins of the legs prevents you from sleeping, doing your usual activities and makes you nervous? It is worth trying ointments or gels with a cooling effect. They will not affect the veins and will not help cope with the disease, but they will relieve the symptom quite quickly.
In addition to conservative therapy, doctors often use methods of complex treatment of varicose veins of the lower extremities, when minimally invasive and surgical operations are used simultaneously with medication. This scheme is used for intense symptoms and extensive distribution of the venous network. The phlebologist decides what measures to take and what to do if varicose veins in the legs suddenly begin to progress. At the same time, he takes into account all aspects of the development of the disease, the individual characteristics of the body and health problems that may become contraindications to certain procedures.
What methods are used to eliminate pathological vessels:
- Laser coagulation. It is used if varicose veins have not progressed to stages 2 and 3, that is, if there are small “stars” on the surface of the skin. The method is painless and effective, but expensive. There is no 100% guarantee of cure, since visible blood vessels are eliminated, while the causes of the disease remain. Used in the early stages to eliminate cosmetic defects.
- Sclerotherapy. A sclerosant is injected into thin and medium-thick vessels, which seals the lumen of the vein, excluding it from the blood flow system. The procedure is practically painless and relatively inexpensive, but has a lot of contraindications. Used at stages 1, 2 and sometimes 3.
- Phlebectomy is the classic excision of pathological veins through punctures or incisions in the skin. This method eliminates superficial varicose veins on the thighs and legs. After the operation, visible scars remain, but the operation is the only effective one for advanced forms of varicose veins.
Carrying out surgical or minimally invasive intervention does not mean complete elimination of varicose veins. The patient will have to regularly visit a phlebologist, take medications to maintain vein tone, and wear compression garments.
Ways to prevent varicose veins
- People at risk, especially those with a hereditary predisposition, need to regularly visit a phlebologist and have an ultrasound scan to diagnose the disease at an early stage.
- It is necessary to do leg exercises regularly if you sit for a long time.
- The diet should include foods that improve liver function - tomatoes, carrots, olives, apples, blueberries. Thanks to the good functioning of the liver, the blood does not stagnate and thins out.
- Prevention of constipation is necessary, because regular constipation is a direct cause of stagnation of blood in the legs.
- You need to get proper rest, especially for women, who need 2-3 times more time to recuperate than men. You need to lie with your legs slightly elevated, and in case of swelling and fatigue, do foot baths with sage, chamomile or calendula.
- In the hot season, you need to drink as much as possible - at least 2 liters per day and not stay in the sun for a long time. Otherwise, the thickness and viscosity of the blood will increase.
- Swimming is very beneficial. During this, the legs cool down and work well while in a horizontal position.
Addresses of our clinics:
St. Petersburg, Manezhny lane, 13 m. Chernyshevskaya
St. Petersburg, st. Bolshaya Raznochinnaya, 27 metro station Chkalovskaya
Classification
Most often (in 75-80% of cases) the disease affects the trunk and branches of the great saphenous vein, in 5-10% - the small saphenous vein, and in 7-10% of patients both veins are involved in the process.
In the clinical course of varicose veins of the lower extremities, experts distinguish two forms and four groups.
Shapes:
- descending - the process spreads from top to bottom along the large femoral vein, starting from its mouth;
- ascending – the disease begins in the foot and is caused by a malfunction of the valve apparatus of the deep veins.
Groups:
- subcutaneous or intradermal pathology not burdened by venous discharge;
- segmental with reflux through perforating and superficial veins;
- widespread with venous reflux (through superficial and perforating veins);
- dilation with reflux through the deep veins.
According to the degree of venous insufficiency, there are four main stages of varicose veins:
- 0 – symptoms of the disease may be present, but it is not determined by diagnostic methods;
- I – this stage is characterized by transient swelling, “heavy legs” syndrome, and the appearance of “spider veins”;
- II – the appearance of persistent swelling that appears in the evening, discoloration of the skin, eczema;
- III – the presence of trophic ulcers, including non-healing ones.
FAQ
Who to contact for varicose veins?
Varicose veins are treated by a phlebologist. You can learn more about phlebologists from our article or make an appointment online with one of our doctors in St. Petersburg.
How to cope with leg fatigue with varicose veins?
You need to lie with your legs slightly elevated (put a sofa cushion under them) and do foot baths with chamomile, sage or calendula.
What is the nature of pain with varicose veins?
Pain varies from patient to patient. It can be stabbing, dull, aching, sharp in areas of varicose veins, bursting, hot pulsating, aching, burning.
Consequences of varicose veins on the legs
The danger lies not in varicose veins itself, but in the subsequent complications and consequences that become a real threat to human life. Let's take a closer look.
Venous insufficiency
This state requires several steps of development. At the very beginning of venous insufficiency, changes are insignificant and horizontal venous reflux appears.
There are 4 stages:
- Zero . There are no characteristic symptoms, only temporary swelling of the legs occurs, veins are slightly noticeable.
- First . Accompanied by severe varicose veins in the legs, but there are no trophic disruptions.
- Second . The obvious appearance of veins on the legs with a large number of nodes, the legs are affected by eczema and ulcers.
- Third . A persistent trophic disorder that cannot be controlled with medications.
With chronic venous insufficiency, patients experience the following symptoms:
- Itching.
- Pain.
- Cramps.
- Edema.
- Stagnation of blood and the appearance of formations (varicose nodes).
- Ulcers.
Thrombophlebitis
This complication is characterized by the appearance of blood clots that clog blood vessels. The blood becomes viscous, which leads to complicated outflow. The upper leg and lower thigh are affected. A phlebologist can easily identify a complication based on pronounced changes:
- Redness.
- Pain.
- Weakness.
- Tissue compaction.
With the development of thrombophlebitis, many veins are affected, including the pulmonary artery. Treatment of thrombophlebitis should be carried out without delay at the first symptoms; surgical intervention is used as therapy.
At the initial stages, outpatient therapy is carried out if varicose veins have not reached the lower leg.
For treatment use:
- Non-steroidal medications to relieve inflammation.
- Anticoagulants.
- Angioprotectors.
- Disaggregants.
Trophic ulcer
A trophic ulcer always occurs in advanced cases when the outflow of blood is severely impaired. Characteristic signs of complications:
- Slow formation.
- Darkening of the skin on the legs, strong pigmentation.
Any injury to the legs can cause damage and rupture of the ulcers. If you provide quick help, there will be no consequences and the injury will heal quickly, otherwise tissue inflammation begins, and a bacterial infection of varying severity may develop.
To treat complicated trophic ulcers, surgery is performed. During treatment, specialists prescribe bed rest for 2 or more weeks. Broad-spectrum antibiotics, regenerating drugs (Actovegin, Solcoseryl) and local antiseptics are prescribed as conservative treatment.
Pulmonary embolism
Thromboembolism is the most dangerous and often fatal consequence. This condition involves occlusion of the pulmonary artery or its branches by detached thrombotic masses.
Main development risks:
- Oncology.
- Carrying out surgical intervention.
- Heart failure.
- Thrombophilia.
- Prolonged lying down.
Women are more often susceptible to complications; development is possible even in children. Pulmonary embolism can be determined by the following symptoms:
- Chest pain.
- Rising temperature.
- Tachycardia.
- Coughing up blood.
- Cough.
- Wheezing.
- Dyspnea.
It is impossible to diagnose the disease yourself; if thromboembolism is suspected, urgent hospitalization is required.
Difficulties in treating advanced varicose veins on the legs in women.
Treatment of advanced disease is difficult. Even archaeologists and researchers of Egyptian mummies find signs of varicose veins. The history of the problem is ancient and has not been completely resolved. Therefore, close attention should be paid to the health of the vascular system: the poor mummy, in suffering, reached a trophic ulcer of the leg, dying, probably due to its infection.
Every day I receive questions from readers about varicose veins in women. I understand why you are so concerned about problems of the lower extremities in women. The dream is slender, smooth, strong legs. Reality - young beauties often have dark spots on their legs.
Dear lovers of my blog, it is difficult to wish you such an unenviable fate. In order to help avoid a neglected picture, I tried to understand it in detail.
Causes
Often the main cause of varicose veins of the lower extremities is called a hereditary factor, therefore, when diagnosing the disease, cases of varicose veins in close relatives are also considered.
However, not all scientists believe that heredity affects the condition of the veins, so while the scientific community is not clear on this matter, it is customary to identify other reasons. If we exclude the possibility of hereditary transmission of varicose veins of the legs, then the only “congenital” factor in the development of the disease can be considered only weak vessel walls. The lack of connective tissue, due to which varicose veins will subsequently develop, can be called the only genetic factor on which scientists agree.
The remaining causes are acquired, and therefore are often associated with a person’s lifestyle, which means that in most cases they can be avoided:
- Excess weight
Obesity is becoming the most common cause of varicose veins of the lower extremities, since in a person with a high body mass index, the pressure on the legs when walking increases.
- Long static load
Excessive workload can be achieved without having extra pounds, so the second risk category on the list is people who have to sit or stand a lot for work. This includes all office workers, sales consultants and some other professions. For them, varicose veins of the leg are practically an occupational disease associated with lack of mobility.
- Tight-fitting clothes
It is worth adding that uncomfortable tight clothing plays into the hands of varicose veins, increasing the chances of its development, so those who want to maintain healthy legs should refrain from corsets, belts, and trousers that pinch in the groin area.
- Poor nutrition
An incorrect lifestyle, which causes varicose veins, mainly concerns nutrition. There is a specific program of healthy and varied nutrition, thanks to which all the necessary elements are included in the diet. One of the important points is the availability of raw vegetables and fruits. These foods are sources of fiber, which not only helps the intestines do their job, but also affects the integrity and elasticity of the vein walls.
- Changes in hormonal levels
Problems with hormones also have a bad effect on a person’s overall health and the condition of the vein walls. This is usually associated with taking special medications, for example, contraceptives, fertility treatments or during menopause.
- Pregnancy
There are other reasons for changes in hormone levels, which lead to varicose veins. For women, pregnancy is one of these factors. In fact, pregnancy is almost always accompanied by varicose veins. This is due to changes in hormonal levels in the first trimester, as well as weight gain and increased pressure in the abdominal area in subsequent months. If most causes can be influenced from the outside by changing your diet or lifestyle, then pregnancy becomes an insurmountable obstacle for many. However, pregnancy does not mean that varicose veins in the legs will necessarily develop. It only increases the risk of leg damage.
Preventive measures to get rid of varicose veins
If you follow preventive measures, you can get rid of varicose veins forever without resorting to serious treatment with medications or surgery. Please note the following recommendations:
- Eliminate tight, loose clothing and tight shoes from your wardrobe;
- eliminate the habit of crossing your legs while sitting;
- do gymnastic exercises in the morning and evening;
- pay special attention to your weight;
- douse your shin with cool water;
- try to keep your legs higher than your body while lying down;
- do not drink alcohol;
- eat right, spend more than 15 minutes eating food;
- quit smoking;
- Monitor your body’s water balance (drink at least 2 liters of fluid per day);
- do not expose your body to sunlight for a long time;
- go swimming;
- pay attention to the beneficial benefits of cycling;
- lead an active lifestyle;
- eliminate unhealthy foods from your diet, increase the amount of fruits and vegetables you consume;
- Eliminate constipation in a timely manner, as it provokes an increase in pressure in the pelvis.
Please note that by following these tips you will prevent the development of varicose veins. If you notice a worsening of your condition, immediately seek help from a phlebologist.
Description of varicose veins of the lower extremities
Varicose veins begin with the appearance of the so -called venous network on the legs or “spider” veins . These vessels have a lumen of several millimeters in diameter. Due to the fact that they are located inside the skin, when they expand and enlarge they immediately become noticeable. They can be located singly, but most often as venous threads that intertwine with each other.
Enlargement of reticular veins is often the next stage of varicose veins after vein veins, although they often develop independently. They appear on the skin as green and purple veins. Most often they occur on the thighs and legs. Varicose reticular veins are thicker than spider veins, but they are smaller and practically do not protrude above the skin compared to varicose veins.
Causes of varicose veins of the lower extremities
Veins are blood vessels that typically return blood from the legs upwards towards the heart. The flow of blood in the venous system must also always move from the superficial veins to the deeper veins in the legs. Blood does not usually move downward in a reverse direction or outward from the deep to the superficial veins because there are one-way valves located inside the veins. With their help, reverse blood flow is prevented.
In some people, the venous valves can be affected, and then the blood flow is not only altered towards the heart, but can also move back down the leg, especially when standing, and this is called reflux.
Veins in which reflux occurs are called incompetent veins or have incompetent valves.
Because the valves in some veins do not work normally, the blood pressure in the veins increases, and then the vessels gradually become swollen, enlarged and called varicose veins. Such a pathological process can last for many years. Clinical manifestations of varicose veins are most often associated with constant high pressure in the veins.
Varicose veins tend to appear:
- with age;
- those who have a hereditary predisposition to varicose veins;
- when standing for a long time or in a sitting position;
- during pregnancy or after childbirth;
- in some cases after prolonged stress on the deep veins.
Removing varicose veins in such circumstances is considered a potentially dangerous action as it would eliminate an important pathway for blood to flow from the lower extremities back to the heart.
Symptoms and diagnosis of varicose veins of the lower extremities
Common symptoms of varicose veins include:
- cosmetically unpleasant appearance, expressed by venous dilatation;
- swelling of the affected lower limb;
- skin pigmentation;
- painful sensations;
- eczema.
Less common symptoms are ulceration, superficial thrombophlebitis and bleeding.
- Venous dilatation
Telangiectasia or reticular varicose veins are the most common initial manifestation of venous disease ( CEAP class 1 ).
The development of varicose veins of the calf muscles is usually observed with prolonged standing or during menstruation. As venous disease progresses, the veins become more tortuous and distended, and patients may notice them appearing in the proximal portion of the limb. Many women report that their varicose veins develop rapidly in size and number during their first pregnancy ( CEAP grade 2 ).
Edema is an early symptom of venous disease ( CEAP class 3 ). It usually occupies the metatarsal region. It is often the result of subcutaneous fibrosis and repeated infections, although its development can be caused by both varicose veins of the lower extremities and lymphangitis.
A feeling of pressure or pain in the limbs that occurs after prolonged standing, as well as when walking or lifting heavy objects, is characteristic of venous disease, while pain from arterial pathology increases with physical exertion. With severe chronic venous insufficiency with outflow obstruction, a symptom such as “venous claudication” can be determined - the patient feels pain when walking, so he needs to stop and wait until it passes and he can move on (CEAP class 4 ).
Patients usually also experience pain and tenderness as the varicose veins expand. In the presence of severe reflux, severe skin pigmentation may be noted ( CEAP grade 5 ).
Lipodermatosclerosis can dramatically compromise the integrity of the affected skin, and minor trauma can lead to the formation of ulcers - the final stage of chronic venous disease ( CEAP class 6 ).
- Physical examination
The physical examination evaluates the lower extremity in a standing position. As a rule, the doctor notes:
- Spider veins or spider veins.
- Telangiectasia (dilated intercutaneous venules up to 1 mm).
- Reticular veins (non-palpable saphenous veins 1-3 mm).
- Varicose veins (vessels with a diameter of more than 3 mm).
- Tissue swelling.
- Skin pigmentation.
- Venous ulcers.
More information can be obtained using duplex scanning of the blood vessels of the legs. The study allows us to determine the patency and competence of the superficial and deep venous system of the lower extremities. Such points as the location and relationship of the sapheno-popliteal joint and the diameter of the affected vein are also clarified.
Basic principles of prescribing therapy for varicose veins of the legs
The need for treatment of varicose veins arises when the blood vessels in the lower extremities dilate; increased pain and general discomfort in the affected areas. Sometimes this condition can indicate serious circulatory problems, which often require advanced therapeutic procedures such as sclerotherapy, laser surgery or endovascular surgery.
Before any treatment tactics are used, the symptoms of the disease are determined. In some cases they are completely absent or weakly expressed. Others define:
- dark purple veins:
- itching and burning at the site of the lesion;
- bleeding from veins;
- severe pain after sitting or standing for a long time.
The deadline for seeking treatment is when problems arise with the self-care process. At the same time, independent attempts to control or eliminate varicose veins are often unsuccessful.
As the experience of many victims of varicose veins shows, treatment of varicose veins of the lower extremities is most effective - in the early stages of the development of the disease.
Diagnosis and treatment of the disease
Since varicose veins of the feet and legs are far from just a cosmetic defect, its treatment must be approached with all seriousness; at the first manifestations, immediately seek advice from a phlebologist. If necessary, the doctor will prescribe you Doppler ultrasound, which is necessary to determine the quality of blood circulation and look for any obstacles.
Transillumination may also be prescribed, in which the surfaces of the veins are identified with a special light. All this will help the doctor determine the condition of your veins at the moment. These manipulations will be the first steps to solve the problem and prevent the spread of the disease. Below are the main ways to solve the problem of varicose veins.
The initial and most cost-effective way to solve the problem is to purchase ointments and gels that have the properties of relieving swelling, fatigue and dulling pain. Purchasing them is quite simple: it can be done at any pharmacy; there is no need for a doctor's prescription. The disadvantage of this method is that the exposure to beneficial substances is minimal, but it is still a good option in the initial stages.
Ultrasound examination is considered the most common and effective method for diagnosing dilated veins in the legs. It will help determine the exact location of the varicose vein, its type and degree of disease.
In addition, the doctor will prescribe a general blood test, which will show the number of red blood cells, hemoglobin, white blood cells and platelets. This will help determine a predisposition to thrombophlebitis or indicate the presence of an inflammatory process in the vein.
The stage of the disease can be determined using a method such as rheovasography - determining the lack of blood supply to tissues. In complex and difficult to diagnose cases, surgical examination is resorted to (for example, venography).
The diagnosis of “varicose veins of the lower extremities” is made after a comprehensive examination, which includes:
- general blood test - by the number of red blood cells, platelets, leukocytes and hemoglobin level, one can judge about blood clotting disorders and the presence of inflammation;
- Ultrasound is the most effective method for identifying affected vessels and veins;
- rheovasography is carried out in order to determine the lack of tissue nutrition with blood (the so-called rheographic index), on the basis of which the stage of the disease can be determined;
- venography, during which a contrast agent is injected into the veins, after which the condition of the venous system is assessed using an X-ray machine;
- physiological tests (Troyanov-Trendelenburg test, Hackenbruch test) make it possible to judge the functioning of the valve apparatus of the superficial veins.
Varicose veins - how to relieve pain with folk remedies, using lemon
Having asked this question, how to relieve pain with folk remedies, I would like to pay special attention to such citrus as lemon. Note that lemon can be used for therapeutic purposes for both internal and external treatment of varicose veins. At the same time, external use involves the use of fairly effective compresses that can be made quickly.
To prepare a pain-relieving lemon compress, you need to take one lemon and cut it into circles, which should be applied to the sore spots and secured with a bandage or gauze bandage. This pain-relieving compress must be worn throughout the day, while not forgetting to replace the used citrus slices with fresh ones.
You should also not neglect lemon for internal use . Eating this citrus fruit helps cleanse blood vessels, strengthen the elasticity of their walls, and also prevent the onset of the inflammatory process.
We invite you to familiarize yourself with the popular folk remedy made from lemon for varicose veins . You will need the juice of six lemons, chopped garlic (5 cloves), a leaf of golden mustache (3 leaves) and 2 cups of liquid honey. All ingredients are thoroughly mixed and placed in a dark place for one week. The product is taken daily for a month, 4 tsp. at once.
The mechanism of varicose veins
Varicose veins appear on the legs primarily due to the structural features and functions of the venous network. With the onset of upright walking, the veins experience increased stress. They carry blood from the peripheral parts of the body to the heart, overcoming gravity. And if the arteries have a muscular layer, thanks to which the blood “pushes” through the vessels, then the veins do not have one.
Their contraction occurs under the influence of residual contraction of nearby arteries and due to the functioning of muscle-venous pumps. The muscles located around the veins contract and push blood toward the heart.
When the muscles relax, blood from the periphery rises upward due to the suction function of the diaphragm, which, by contracting, compresses the veins passing through the diaphragmatic opening.
When muscles contract, blood rises further to the heart. When muscle function is impaired, intra-abdominal pressure increases, the structure of the veins themselves, blood stagnates, stretching the walls of blood vessels.
With prolonged stagnation, the thin walls are stretched and deformed, forming varicose veins on the legs. As the disease progresses, it affects the valve system that regulates the flow of blood from the subcutaneous to the deep veins.
Experiencing constant irritation, the walls of the veins become inflamed. The smoothness of the endothelium is disrupted.
Prevention
In order to prevent varicose veins of the lower extremities, it is necessary to avoid prolonged static loads. If work requires long periods of standing or sitting, you should periodically take breaks for short exercises or at least walking. After a working day, it is recommended to lie down with your legs in a horizontal or elevated position.
In the prevention of varicose veins, a significant role is given to active activities: sports (swimming, cycling, fitness), dancing, walking, etc.
Video from YouTube on the topic of the article:
Stages of the disease
In 2000, Russian phlebologists adopted a classification of varicose veins of the lower extremities, taking into account the form of the disease, the degree of venous insufficiency, and the presence or absence of complications. In accordance with it, three stages of varicose veins of the lower extremities are distinguished:
- Compensation stage. Patients do not show any complaints. During the examination, superficially located dilated veins are detected on one or both legs.
- Subcompensation stage. Patients complain of night cramps, impaired skin sensitivity (paresthesia) in the legs, and a feeling of fullness. In the evening, swelling of the legs, ankles and feet is often observed, disappearing after a night's sleep. When examining the legs, dilated varicose veins are clearly visible.
- Stage of decompensation. The symptoms described above are accompanied by eczema and dermatitis. The skin is hyperpigmented, dry, shiny, tightly adherent to the subcutaneous tissue.
Stages of varicose veins of the lower extremities
Symptoms of the second stage
Varicose veins of the 1st degree are characterized by the absence of external manifestations. The onset of the disease can be suspected by the following signs:
- Increased leg fatigue;
- Nagging pain at the end of the working day;
- Convulsions;
- Swelling of the feet and legs in the evening.
Some patients experience restless legs syndrome - lying in bed, a person cannot find a comfortable position, and there is a feeling of discomfort in the legs. This leads to sleep disturbance. Symptoms worsen in hot weather.
With grade 2 varicose veins, the symptoms are much more pronounced. They appear already at the height of the working day, and reach their maximum in the evening. The pain is so severe that painkillers are required.
This stage is characterized by the appearance of clinical signs:
- Severe swelling of the extremities;
- Specific spider veins are dilated small veins located just under the skin.
In these areas there is increased pain and itching. By the end of the second stage of varicose veins of the lower extremities, the veins become visible under the skin in the form of blue spots and stripes.
Attention! At this stage, the disease is still curable. A person can get rid of the disease if he seeks medical help in a timely manner.
Grade 3 varicose veins are characterized by pronounced deformation of the vascular wall - it thickens, and the vessels become tortuous. Veins protrude noticeably under the skin, resembling bunches of grapes.
A person is worried about severe pain in the legs, cramps, and fatigue. Swelling appears both in the evening and in the morning. This stage of varicose veins is characterized by a change in the condition of the skin. It becomes excessively dry and flaky. These manifestations are especially pronounced in the area of deformed veins.
At the third stage, complications of the disease develop - thrombophlebitis and thromboembolism. Their appearance is associated with severe stagnation of blood in the vessels, resulting in the formation of blood clots. With thrombophlebitis, inflammation of the venous wall occurs, which is manifested by increased temperature and severe pain in the legs.
Thromboembolism is a dangerous complication of varicose veins associated with the detachment of a blood clot from the venous wall and its entry into large vessels. Most often, blood clots from the leg veins enter the pulmonary artery. This causes pulmonary edema and death occurs within minutes.
This is already advanced varicose veins of the legs. The veins are even more deformed, resembling tourniquets or ropes under the skin. Touching them is painful, they are almost always in the stage of inflammation. Lymphostasis develops - stagnation of lymph in the vessels. The legs swell greatly, and the swelling does not subside even with rest.