What is toxocariasis?
Toxocariasis is a rare human infection caused by the larvae of animal parasites known as Toxocara canis (in dogs) and Toxocara cati (in cats). They are better known as roundworms.
Toxocara parasites live in the digestive systems of dogs, foxes and cats. The parasite's eggs can be released into the feces of infected animals and contaminate the soil. If someone accidentally ingests small particles of contaminated soil, they may develop toxocariasis. To prevent the spread of infection, dog owners should always dispose of dog and cat waste responsibly.
Toxocariasis usually affects children aged 1 to 4 years. However, cases of toxocariasis have been reported in people of all ages.
Young children are especially at risk because their play habits make them more likely to come into contact with contaminated soil.
Prevention
To prevent re-infection with parasites, it is important not only to follow the prescribed treatment for toxocariasis in adults, but also to adhere to certain preventive measures:
- Adults should avoid direct contact with stray animals, and do not allow small children near stray cats or dogs.
- Since toxocariasis often occurs in people due to the specifics of their work, it is necessary to undergo regular preventive examinations in the clinic. The professions at risk include veterinarians, hunters, dog breeders, kindergarten teachers, and gardeners.
- After a walk, be sure to thoroughly clean the paws and fur of pets, wash your hands several times with soap, and for adults, observe the rules of personal hygiene.
Types of toxocariasis
Symptoms of toxocariasis can vary depending on where in the body the infection occurs. There are three main types of toxocariasis:
- latent toxocariasis;
- visceral migratory larva;
- eye larva migrans.
Hidden toxocariasis
The latent form of the disease is the most common and mild form of toxocariasis. Symptoms of latent toxocariasis include abdominal pain, cough and headache.
Visceral migratory larva
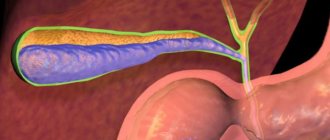
Visceral larva migrans develop when large numbers of parasites spread through various organs of the body such as the lungs, liver and heart.
The main symptoms of the visceral form of the disease are fever, abdominal pain and shortness of breath.
Eye larva migrans
This form of the disease is the least common, but potentially the most serious type of toxocariasis. This form can develop if Toxocara canis parasites get into the eyes.
The main symptoms of eye larva migrans are blurred vision and eye irritation. If left untreated, this type of disease can cause permanent loss of vision in a person, although usually only one eye is affected.
Diagnostics
Diagnosis of toxocariasis involves several points:
History taking
The doctor interviews the patient about his living conditions and past illnesses. Information is being sought about how the person could have become infected, what symptoms were observed and whether treatment measures were taken.
…
Inspection
The doctor examines the patient’s skin for allergic reactions, listens to the lungs and heart, palpates the spleen, liver, and lymph nodes.
Laboratory tests for toxocariasis
These include a general and biochemical blood test, a serological blood test for toxocariasis to determine antibodies and antigens in the blood serum. The most accurate results are those obtained by ELISA with a sensitivity of about 95%.
Instrumental diagnostics
They prescribe a chest x-ray, ultrasound of the abdomen, checking vision clarity and fundus examination, CT, MRI.
The diagnosis of toxocariasis is made if the blood biochemistry shows an increase in protein, bilirubin, liver enzymes, and immunoglobulins. In a general blood test, the level of red blood cells and hemoglobin decreases, the level of leukocytes and eosinophils increases, and the ESR accelerates. Ultrasound of the abdomen shows an enlarged liver, spleen, and inflammation of the pancreas . A chest x-ray reveals areas of hardened tissue that move over time. CT and MRI show altered tissues with areas of inflammation where larvae are contained. titer of 1:400 for toxocariasis indicates that there is an infection with larvae. If titers exceed 1:800, the diagnosis of toxocariasis is confirmed.
Symptoms and signs
Hidden toxocariasis
Symptoms of latent toxocariasis include:
- cough;
- difficulty sleeping;
- abdominal pain;
- headache;
- swollen lymph nodes (glands).
Children with latent toxocariasis may also exhibit changes in their usual behavior, for example they may be unusually irritable.
Visceral migratory larva
Depending on which parts (or organs) of the body are infested with parasites, migrating visceral larvae can cause a wide range of possible symptoms. These may include:
- fatigue;
- lack of appetite;
- weight loss;
- high temperature (fever) 38C (100.4F) or higher;
- cough;
- labored breathing;
- abdominal pain;
- headache;
- rash (see photo);
- swollen lymph nodes;
- convulsions (fits), which are rare.
Eye larva migrans
Symptoms of eye larva migrans include:
- impaired (or decreased) vision, such as blurred or clouded vision that usually affects only one eye;
- the eye is very red and sore;
- Photosensitivity (photophobia) occurs.
Types and manifestations of the disease
There are several forms of toxocariasis:
- Manifest - has clearly defined symptoms;
- Erased - symptoms practically do not appear;
- Latent - hidden form, asymptomatic.
Age also influences the severity of the disease:
- The severe manifest form most often affects children under 12 years of age;
- Adults are characterized by either erased or latent forms.
If the period of the disease is less than 3 months, then it is considered acute; if longer, it is considered chronic. The latter form is characterized by alternating periods of remission and exacerbation. With an exacerbation, the activity of the larvae increases - infection of new organs begins.
Forms of toxocariasis are determined by their symptoms:
- Visceral - infection of internal organs;
- Ophthalmic;
- Skin;
- Neurological.
When you get toxocariasis, the immune system is activated. This is expressed in allergic reactions:
- Skin rash is similar to mosquito bites, but does not have a specific localization. The rash is characterized by itching of varying strength - from unobtrusive to severe;
- Quincke's edema - located in the cervical region, compresses the larynx, which makes breathing difficult. A person suddenly begins to choke - he cannot take a full breath and exhale, his skin turns blue. The victim needs quick medical care, because... failure to act may result in suffocation and death;
- Bronchial asthma - characterized by a prolonged dry cough, which produces a small amount of light mucus, attacks of shortness of breath and asphyxia. Breathing becomes hoarse, noticeable from a distance.
For reference. The acute phase and the period of exacerbation during the chronic phase are often accompanied by fever, an increase in body temperature to 37-38 degrees Celsius. In this case, signs of poisoning are observed - headache, loss of appetite, muscle pain either manifests slightly or is absent altogether. Lymph nodes indicate infection with a worm - more than 5 groups increase in size, however, they remain without symptoms of inflammation (they remain mobile, painless).
Visceral form
In the visceral form of toxocariasis, internal organs are affected in 90% of cases. At the same time, the symptoms correspond to damage to the organ in which the parasite larvae have settled. Characterized by allergies and poisoning. As already mentioned, the worm is carried throughout the body through the blood, so organs with a large circulatory system and slow blood circulation are more susceptible to infection. Infection of the digestive system begins with infection of the liver tissue. Then, the parasites penetrate the bile channels, pancreatic channels, and intestines. As a result, the outflow of gastric juice is disrupted and the intestinal wall suffers. I point out the following symptoms:
- pressure in the right hypochondrium;
- pain in the right hypochondrium of a stabbing nature;
- painful bloating;
- bitter taste in the mouth;
- unstable stool;
- abdominal pain;
- weight loss.
Attention! The parasite is able to damage the intestinal wall, leading to constant slight bleeding. This is manifested by anemia, weakness, pallor of the skin and mucous membranes and tinnitus.
Symptoms of respiratory infection:
- persistent dry cough, with or without white sputum;
- asthma;
- difficulty breathing;
- attacks of asphyxia.
Tocrocarosis subsequently develops into bronchial asthma, less often into pneumonia and pulmonary edema. Sometimes, the parasite is localized in the heart valves, which causes endocarditis. A dysfunction of the valve disrupts the movement of blood through the vessels, which is expressed in the form of heart failure, the signs of which are:
- lethargy;
- blueness of fingers, nasolabial triangle;
- asthma and coughing when lying down (damage to the left side of the heart);
- symmetrical swelling of the legs and abdomen (impaired functioning of the right side).
Ophthalmic toxocariasis
A form of toxocariasis that affects the eyes is quite rare. Occurs when the eye orbit, its muscles or internal components of the eye are damaged. In this case, the symptoms are as follows:
- rapid loss of vision (complete or partial), usually only in 1 eye;
- conjunctivitis;
- bulging of the eyeball;
- swelling and congestion of the eyelids and orbital tissues;
- pain in the eye socket;
- strabismus
For reference. Ophthalmic toxocariasis primarily affects children, and the disease is asymptomatic.
Cutaneous form
The movement of the larvae occurs directly in the dermis of the skin, and manifests itself in the form of:
- skin itching, burning, pain;
- sensations of movement under the skin;
- manifestations of inflamed traces of the worm (red);
- inflammation of the skin at the site of invasion.
Neurological form
When the Toxocara parasite enters the brain area, it causes inflammation. This form of the disease has a severe course and is expressed in the form of neurological disorders:
- severe headache of a bursting nature;
- severe nausea and vomiting;
- muscle tension in the neck and back;
- hypersensitivity of the sensory organs;
- muscle weakness or complete epiplexia;
- miotic spasms;
- dysfunction of the vestibular apparatus;
- mental disorders - aggression, decreased intelligence, delayed development (in children).
Causes of toxocariasis
To better understand the causes of toxocariasis, it is helpful to learn a little more about the life cycle of the Toxocara parasite.
The adult parasites live in the small intestines of dogs and puppies (and a number of other mammals, such as foxes and cats). They range from 4-12 cm in length (1.5-5 inches).
Adult parasites are capable of producing large numbers of eggs. The eggs are passed into the stool (feces) of an infected animal.
The eggs have a strong outer shell and can survive for up to 5 years once they are released into the external environment.
Most cases of toxocariasis develop when someone touches contaminated soil and then transfers the eggs to their mouth.
Once the eggs enter the human body, they enter the intestines before hatching and releasing parasite larvae (insects in the earliest stages of development). The larvae are able to travel to all parts of the body.
Most symptoms of toxocariasis occur in people who have an allergic reaction to the larvae. In many cases, people become infected with parasites but do not experience any symptoms.
Pathogens
The causative agents of toxocariasis are two species of parasitic roundworms of the genus Toxocara, which belongs to the class Ascarididae. Representatives of the cat family are the only hosts of the cat toxocara (T. cati), and dogs, foxes and other canines are the only hosts of the canine toxocara (T. canis). The main causative agent of the disease in humans is still considered to be canine toxocara, which is why it is more common.
It is also assumed that toxocariasis can be caused by Toxocara vitulorum, although there is no reliable evidence of this. Methods for diagnosing toxocariasis, which are usually used, do not allow us to specifically determine the type of parasite whose larvae caused the disease.
Broadcast
Most transmission of Toxocara to humans occurs through ingestion of invasive eggs. The dog Toxocara is capable of producing about 200 thousand eggs per day, while a puppy may have about 100 thousand eggs per gram in his feces.
Eggs of pathogens come out of cats and dogs, but the peculiarities of canine feces make the Toxocara species parasitizing them more common, and therefore more dangerous to humans.
Both feline and canine toxocara require several weeks to mature in damp, humid conditions away from the host before the eggs become infective. Therefore, eggs recently released from an animal do not pose any danger.
Puppies and kittens pose the greatest risk of infection with toxocariasis. They become infected with Toxocara from their mother and contain eggs in their stool. In adult animals, the larvae in the body are usually encapsulated without maturing into adult worms
The main route of infection . Many objects and surfaces may be contaminated with infectious Toxocara eggs. Also, flies that feed on feces can spread them to other surfaces or food products, but most infections occur without their participation. Young children often put contaminated objects in their mouths or eat dirt, putting them at risk of developing toxocariasis. People also touch contaminated food and do not wash it or wash their hands before eating.
Additional route of infection . Since people are not the only casual hosts of Toxocara, there is another way to become infected. Undercooked rabbit, chicken or sheep meat can lead to infection. At the same time, encysted larvae in meat, when they enter a person, have the ability to reactivate and migrate again in a new host, causing toxocariasis. Particular attention should be paid to preparing giblets and liver thoroughly to avoid transmission of infection.
Reservoirs for the parasite
Dogs, foxes and other canids are natural reservoirs for Toxocara Canis, but puppies pose the greatest risk of spreading the infection to humans. The disease in most adult dogs is characterized by encystment of second-stage larvae. However, they can be reactivated in pregnant females and infect puppies through the placental barrier. Transmission also occurs through breast milk during feeding. Infected mothers and puppies under five weeks of age shed many eggs in their stool. About 50% of puppies and 20% of adult dogs are infected with Toxocara.
Cats are a reservoir for feline toxocara. As with canines, second-stage encysted larvae are reactivated in pregnant or lactating cats. However, transmission to kittens can only occur through breastfeeding.
Life cycle
Diagram of the life cycle of Toxocara using Toxocara canis as an example.
Cats and dogs can become infected with Toxocara through eating eggs or by passing the larvae from a mother to her offspring. Transmission can also occur when larvae enter from infected accidental hosts - earthworms, cockroaches, rodents, rabbits, chickens, sheep.
Further development is similar to the human roundworm. Inside the intestine, the eggs hatch into larvae in the second stage of development. Although there is controversy over the appearance of a second or third larval form. They enter the bloodstream and migrate to the lungs, where they are coughed out and re-swallowed. They then mature into adults within the small intestine of a cat or dog. Mating and laying also take place there. The eggs are passed in the feces and become infective only after several weeks outside the host. During this period, the development of the first to second (and possibly third) stage of the larva inside the egg occurs, i.e. maturation.
In most adult dogs and cats, the full life cycle does not occur, but the second stage larvae are encapsulated after a period of migration by the body. Only pregnant or lactating cats and dogs have active larvae. The complete life cycle usually occurs only within such females and their offspring.
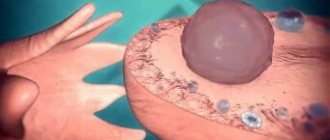
A second form of larvae also hatches in the small intestine of an accidental host, such as a human, after ingesting infective eggs. They then migrate through organs and tissues - most often to the lungs, liver, eyes and brain. Since the larvae cannot mature in the bodies of accidental hosts, after their migration they get stuck in the blood vessels and penetrate into neighboring tissues, where they become encapsulated.
Morphology
Both species produce brown eggs with an uneven surface. The eggs of T. canis are 75-90 µm in diameter and spherical in shape, while the eggs of T. mystax are 65-70 µm in diameter and oblong. In the second stage, the larvae hatch from these eggs and measure about 0.5 mm in length and 0.02 mm in width. Adults of both species have a fully formed digestive system and three lips around the mouth opening.
The larvae enclosed in tissues are microscopic in size, so it is impossible to feel them under the skin. Unlike infection with cysticercosis, when sometimes people find nodules (balls) in themselves.
The adult worm T. canis is found only in the bodies of dogs and other canids (wolves, foxes, etc.). Males are 4-6 cm long with a curved rear end. Each has two spicules (protruding parts of the reproductive apparatus) and one tubular testis. Females can reach 15 cm and contain a vulva extending over one third of their body. They do not have a curved rear end.
Adult females of T. cati are about 10 cm long, while males are 6 cm or less. Adult worms live only in the bodies of cats. The male of this species also, unlike the female, has a curved rear end.
Treatment of toxocariasis
All three types of toxocariasis can be treated with a drug called mebendazole . Mebendazole prevents parasites from feeding on glucose. Without a food source, the parasites will die.
Most people need to take a four-week course of mebendazole. Mebendazole usually does not cause side effects, although some people may experience headaches at the beginning of their treatment.
Visceral migratory larva
For visceral larva migrans, which cause particularly severe breathing difficulties, hospitalization may be required so that the patient's breathing can be maintained while the infection is treated.
Eye larva migrans
In the case of the ocular form of the disease, additional treatment may be required to prevent damage to the eye. For example, steroid medications may be used to help reduce eye inflammation and irritation.
In some cases, laser treatment is required to kill any parasites that are present in the eye.
A type of treatment known as laser photocoagulation . Treatment is usually done on an outpatient basis, which means the patient does not have to stay in the hospital overnight.
To numb the surface during laser photocoagulation, drops are injected into the eyes. Next, a special contact lens is placed over the eyes to hold the eyelids open and focus the laser beam on the retina. The specialist then uses a laser to burn off the parasites in the eyes.
Laser photocoagulation is usually not painful, although a sharp tingling sensation may sometimes be felt during treatment of certain areas of the retina.
After treatment, vision may be blurry. However, it should return to normal after a few hours.
Some people who have had laser photocoagulation have experienced some loss of peripheral vision (side vision) and night vision. One study found that more than 50% of people treated noticed some difficulty with their night vision, and 25% noted some loss of peripheral vision.
Drug treatment of toxocara in adults and children
It is carried out only under the strict supervision of a specialist. All medications are properly tested for possible reactions of the body, and an individual treatment plan is drawn up.
- "Zentel" . It not only suppresses the vital activity of roundworms by disrupting glucose synthesis, but also removes them. It begins to affect helminths within 2 hours after administration. For toxocariasis, the daily dose is 2 tablets in the morning and before bedtime. Duration of treatment is from 5 to 10 days. It is possible to repeat the course.
- "Vermox" . It copes well with adults, but has no effect on larvae. Accepted up to 14 days. The daily dose is 5-10 mg per 1 kg of weight. Take in the morning, at lunch and before bed.
- "Albendazole" . There is a need for a repeat course. Duration of treatment is from 10 to 15 days. Take 5-10 mg/kg body weight 2 times a day. Drink plenty of water, do not chew. If the retina is damaged, it is prohibited to treat roundworms with this drug.
- Chewable tablets "Nemozol" . 400 mg twice a day. Duration of treatment is 1-2 weeks.
Be especially careful when choosing antihelminthic drugs. Consultation with an experienced physician is required.
All medicinal methods of treatment by a specialist provide for the exact concentration of components and take into account all allergic reactions. Therefore, do not self-medicate.
Detection methods
Enzyme immunoassay is the most effective way to determine toxocarriers. The accuracy of the ELISA result reaches 95%. Its essence is to detect antibodies produced by the immune system to roundworm antigens. Before donating venous blood, the patient does not consume fatty and fried foods, medications and alcohol.
If a person gets a result of 1:100, then he does not have toxocariasis. Weakly positive indicators of 1:200-1:400 may indicate infection. At a value of 1:800, one can confidently say about infection.
Diagnosis of helminthic infestation causes some difficulties due to the fact that conventional stool analysis does not show the presence of parasites in the body.
Other methods for diagnosing toxocariasis may be CBC, ultrasound, ART, liver tests, tomography, ophthalmological examinations, and radiography.
What determines the success of treatment
Only by using all therapeutic principles in combination can we ensure that toxocara begins to leave the body. The main components of successful treatment are medication, diet and folk remedies.
| Drugs | Anthelmintics (Albendazole, Vormil), immunomodulators (Likopid, Dekaris), glucocorticosteroids (Betamethasone, Prednisolone), anti-inflammatory drugs (Erius, Diclomek), antihistamines (Zirtec, Cetrin), drugs that restore the functioning of the gastrointestinal tract (Enterol, Ersefuril) and liver ( Darsil, Hepatrin), vitamin and mineral complexes. |
| Diet | Meals should be fractional (5-6 times a day), you should consume up to 1.5 liters of water per day. The diet should be enriched with herbs, vegetables and fruits of yellow or green color, herbs and spices, and animal fats should be replaced with vegetable ones. You will have to give up chocolate, sweets, baked goods, white bread, fatty, fried, smoked foods, alcohol, and sweet carbonated drinks. |
| Folk remedies | Decoctions and infusions based on wormwood seeds, elecampane root, wood sorrel, tansy, and ash twigs. Using an enema based on a decoction of garlic and milk. |
Even knowing how to get rid of toxocara, patients should not self-medicate. Most anthelmintic drugs have a considerable list of contraindications and adverse reactions. Therefore, the treatment regimen and dosage of medications is prescribed exclusively by the attending doctor.
Human infection with toxocara can occur in the following cases:
- touching the fur of an infected animal;
- poor washing of vegetable and fruit products;
- drinking raw and contaminated water;
- lack of adherence to personal hygiene rules.
Infection is possible in any season of the year, since the parasitic larvae are quite resistant to various weather conditions. At the same time, a special risk group for infection includes:
- people whose professional activities are closely related to animals: veterinarians, nursery or animal shelter workers;
- children in the age group of 3-5 years, often playing in the sand and not maintaining personal hygiene;
- hunters who constantly maintain contact with a hunting dog that may be a carrier of the infection;
- vendors selling unwashed vegetables that were in soil possibly contaminated with Toxocara;
- owners of their own vegetable plots and garden plots, constantly working in the ground.
When soil is infected with parasitic larvae, the likelihood of human infection is high.
Getting rid of toxocara with folk remedies
Gifts of nature often come as an addition to pharmaceutical drugs. They have a significant effect on the body only with prolonged use.
- Onion medicine . Finely chop a medium-sized onion, cover with 250 ml of boiling water, leave overnight. Every 6 hours drink 1 tbsp. spoon. Rest for a week and repeat the treatment.
- Elecampane root . Measure 10 g of crushed roots, pour 250 ml of boiling water, leave for 30 minutes. Filter. Consume according to the full st. spoon three times a day.
Expulsion of helminths can be carried out not only by taking medications orally, but also by using enemas. Particularly effective are compositions made from pharmaceutical herbs that have antiparasitic and laxative properties.
Use an effective recipe for enemas:
Grind sage, centaury, and sea buckthorn in equal proportions. Measure out 4 full tablespoons of each piece. Pour a liter of boiling water, cover tightly with a lid and let sit overnight. After waking up, use for a cleansing enema.
Damage to the eye area
In addition to internal organs, the larvae can penetrate the eye area. This occurs less frequently than internal lesions and is observed mainly in pre-adolescent children. They accumulate in the upper eyelid, in the tissues of the eyeball, in the muscles responsible for the normal functioning of the eye.
Symptoms caused by worms are as follows:
- blurred vision;
- tic contractions of the eyelids;
- increased tearfulness;
- swelling of the tissues of the eye area;
- eye pain.
The activity of helminths in the eye tissues can lead to complete or partial loss of vision, loss of visual areas from the picture, and strabismus.
Drug therapy
Infected people are not contagious to others and therefore do not need isolation. If one child is infected, it is advisable to examine all other family members, since there remains a possibility that children and parents could have come into contact with the same source of infection.
Patients with mild toxocariasis can receive treatment on an outpatient basis; those with severe infection are subject to mandatory hospitalization. In each specific case, the question of how and where to treat toxocariasis is decided individually, this is due to the following factors:
- 1How acute is the onset of the disease and what is the dynamics of symptoms?
- 2Is there damage to the nervous system or eyes?
- 3What is the child’s age? Young children (under 3 years of age) suffer from invasion more severely, and its consequences at this age are less predictable.
- 4Does the infected person have chronic diseases that can worsen the prognosis (diabetes mellitus, bronchial asthma, cerebral palsy, heart defects, etc.)?
- 5Compliance of the patient and his family members, the ability to care for the patient.
Treatment of toxocariasis, as a rule, is complex and includes the prescription of drugs of 3 groups:
- 1Etiotropic therapy – specific anthelmintic drugs of the benzimidazoles group (drugs of choice, level of evidence 2+). The CDC has approved two drugs in this group for the treatment of toxocariasis - albendazole and mebendazole.
- 2 Pathogenetic therapy - hepatoprotectors (Gepamerz, Essentiale Forte), expectorants (Ambrohexal, Acetylcysteine, Carbocysteine), bronchodilators (Berotek, Salbutamol, Berodual), antacids, enterosorbents (Smecta, Enterosgel), antispasmodics (No-shpa, Buscopan), etc.
- 3Symptomatic drugs - antipyretics (Paracetamol, Ibuprofen), antihistamines (Suprastin, Tavegil, Cetrin), glucocorticosteroids (Prednisolone, Dexamethasone), etc.
Table 3 below presents dosage regimens, duration of treatment and precautions when prescribing anthelmintics.
| Name of the drug | Average therapeutic doses | Precautions and side effects | Efficiency |
| Albendazole (Nemozol, Zentel, Sanoxal) | 400 mg 2 times a day orally for 5 days (source CDC); Russian infectious disease specialists recommend taking albendazole for 14-20 days. For children 2-6 years old, the dose is calculated as 10-15 mg/kg per day in 2-3 doses (source 2) | During treatment, monitoring the level of liver transaminases and UAC is necessary. Headache, dizziness, nausea, vomiting, rash and itching of the skin, urticaria and other manifestations of allergies are possible. Not recommended for use during pregnancy (group C), however, if necessary, can be prescribed in the 2nd and 3rd trimester | +++ |
| Mebendazole (Vermox, Wormin) | 100 – 200 mg 2 times a day orally for 5 days, for both adults and children (source CDC); Russian infectious disease specialists recommend taking mebendazole for 28 days. For young children 25 mg/kg per day in 2-3 divided doses (source 2) | While taking the drug, it is necessary to monitor the level of transaminases and OAC. Possible abdominal pain, dizziness, nausea, allergic reactions. The drug is undesirable for use during pregnancy (group C), however, if necessary, WHO allows its use in the 2nd and 3rd trimester | ++ |
Table 3 - Drugs and treatment regimens for toxocariasis in adults and children (CDC source and clinical recommendations of the Federal State Budgetary Institution Research Institute for Medical and Biology of the Federal Medical and Biological Agency of Russia)
Anthelmintic drugs are usually well tolerated. Despite the possibility of developing side effects when taking medications, there are simply no more effective treatments.
Treatment effectiveness indicators:
- 1Reduction or complete disappearance of clinical symptoms.
- 2Improved health and general condition, absence of signs of intoxication and allergization of the body.
- 3 Decrease in the level of eosinophils and normalization of the peripheral blood picture.
- 4 Decrease in titers of specific antibodies within 3-4 months after the course of treatment.
Recovery of the body after an invasion can take several more months. During this period, the patient must follow a gentle diet and daily routine. The prescription of probiotics, hepatoprotectors, multivitamins, dietary supplements is carried out by the attending physician.
After a course of therapy, patients require clinical observation for a year, with regular examination by an infectious disease specialist (once every 2 months) and performing a general blood test, blood biochemistry, coprogram (twice), and assessment of the titer of specific antibodies (every 6 months).
There are also so-called “folk” methods of treatment, which use tinctures and decoctions from the bark of ash, tansy, elecampane, garlic, and wormwood. Unfortunately, there is no reliable data confirming the effectiveness of such treatments. The use of various enemas is unjustified due to the fact that Toxocara larvae are localized outside the intestine, in tissues and organs.
Under no circumstances should you hesitate to contact a specialist and wait for the body to spontaneously heal itself, because worsening the infectious process can lead to permanent disability and death.
Consequences of Toxocara parasitism
During the migration process, the larvae that provoke toxocariasis damage tissue, resulting in inflammation, necrosis and hemorrhage. In this case, the helminth dies, causing irreparable harm to the host’s body.
If the symptoms of ocular toxocariasis are not treated, one-sided blindness may subsequently develop. And with the visceral type, the complication is severe pneumonia, which often leads to death.
In some cases, Toxocara canis larvae migrate to the myocardium and other important areas of the central nervous system. Also, as a result of their vital activity, multiple granulomas are formed in tissues and organs (brain, lungs, lymph nodes, myocardium, pancreas). An area of necrosis appears in their center, which leads to destruction.