It is not without reason that gynecologists constantly say that every woman is simply obliged to undergo preventive examinations. The condition of the organs of her reproductive system not only affects general health, but also determines the ability to produce healthy offspring. And if expressed in simple human language, this means that a woman can conceive, bear and give birth to a healthy child only in the absence of gynecological diseases. And the condition of the uterine endometrium of the expectant mother is simply of great importance here.
Chances of pregnancy
There are statistics that in 14% of cases of various pathologies during pregnancy, the “culprit” is chronic endometritis. Experts say that a viable fertilized egg along with a healthy, functional endometrium are the deciding factors when trying to conceive. The fertilized egg is looking for a safe haven for further development, and only the uterus is suitable for this role. But if its tissues are damaged, then the blastocyst cannot take root. This is exactly what happens in chronic endometritis, when the affected uterine tissue cannot create conditions favorable for the development of the fertilized egg.
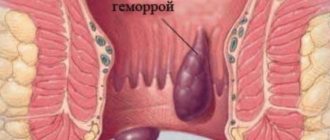
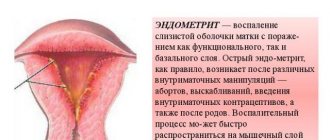
Endometritis is an inflammation of the uterine mucosa, as a result of which the (internal mucous membrane) becomes covered with adhesions and scars, thickens and hardens. It is almost impossible to get used to such armor, and the egg that makes an unsuccessful attempt is mercilessly rejected - a miscarriage occurs even in the early stages. Very often, a woman does not even suspect that conception has taken place, since menstrual-like bleeding occurs.
Endometritis develops as a result of a violation of the integrity of the uterine endometrium when mechanical damage occurs. Abortions are especially common causes of endometritis; the disease can also develop after childbirth or surgery. Sexual infections also contribute to the disruption of the integrity of the uterine mucosa.
Untreated or untreated endometritis becomes chronic. It not only causes discomfort with its systematic manifestation (signs of endometritis include acute pain in the lower abdomen, purulent discharge from the genital tract, chaotic uterine bleeding, menstrual irregularities), but in many cases, as we have already said, it becomes the cause of infertility and.
Forecasts during pregnancy
In rare cases, a woman manages to become pregnant against the background of chronic endometritis, but almost always such a pregnancy is doomed. If the egg manages to implant into the uterus affected by endometritis, it will persist throughout the entire gestation period. Other disorders and complications will also always accompany such a pregnancy. In addition, endometritis will spread, affecting the tissues of the fetus, which will ultimately lead to fetal death.
Complicated type of disease
The disease easily becomes chronic if it is not treated, and then conception and pregnancy are called into question. An even more dangerous condition is postpartum purulent catarrhal endometritis, in which already on the 2nd day after delivery the body temperature can reach 40ºC. In this condition, the following symptoms are observed:
- chills, fever
- nagging pain in the lower abdomen
- pain radiating to the lower back
- profuse bleeding from the uterus.
How to get pregnant and give birth?
Yet chronic endometritis and pregnancy are not mutually exclusive. We have painted a rather gloomy picture just so that you understand that we are talking about serious things. This is your health, your life and the fate of your future children. If you are unsuccessfully trying to get pregnant, be sure to undergo a full examination, including checking the condition of the uterus. If the diagnosis of chronic endometritis is confirmed, you will have to undergo the entire course of treatment, including antibacterial, physiotherapeutic, immunostimulating therapy, taking oral contraceptives, sedatives and vitamin preparations, and treatment of concomitant diseases. Recently, modern methods of treating chronic endometritis have been increasingly used - laser therapy, magnetic therapy, infusion therapy, ozone therapy and others. Let us immediately note that chronic endometritis is a serious pathology that takes quite a long time to be treated. But without this, it is vain to hope for a successful pregnancy and safe gestation. Completely cured endometritis does not pose any danger to future pregnancies.
In some cases, when pregnancy took place against the background of chronic endometritis and it was detected early, treatment can be carried out with minimal risk to the child.
Do not despair if you are diagnosed with chronic endometritis. In fact, today women are being diagnosed with this more and more often. And this does not prevent in the future, after completing the treatment course, from giving birth to healthy children, many healthy children. Often (but not necessarily!) doctors resort to and, but the main thing is that everything is possible! And everything will be fine with you too - you’ll see!
Especially for
— Elena Kichak
From Guest
I am 33 years old. Patients with endometritis are referred for IVF. My preparation for IVF included 6 injections of alloferon. The gynecologist convinced me to try adding this immunomodulator. Studies were conducted in Samara that showed very good results.
From Guest
I treated endometritis for a long time, after an unsuccessful pregnancy and miscarriage I managed to get pregnant on my own without the help of IVF, the pregnancy was quite difficult, but it was worth it, I gave birth to a son and am very happy! I am undergoing treatment again, preparing for the next pregnancy! Do not despair if you have been diagnosed with this, with proper treatment and under the supervision of a qualified gynecologist, everything is possible! 
From Guest
I am 35 years old, I have secondary infertility and chronic endometritis (two ectopic pregnancies), I have been living with this diagnosis since 2004. I treated endometritis many times, but it subsided for a while and then reappeared. Two IVF attempts in 2012 and 2013. The first attempt was unsuccessful, but the second attempt was successful. In July 2014, I gave birth to my son. I was monitored throughout the pregnancy, it was not easy, but it was worth it. Don't let go and believe your dreams come true!!!
Among the reasons causing difficulties with conception and pregnancy, endometritis is not the least important. Indeed, in 90% of cases, the disease is detected in women of reproductive age. But are endometritis and pregnancy really incompatible? By no means, doctors do not put an end to the reproductive capabilities of patients even with such a serious illness.
Read in this article
How to cure endometritis and get pregnant
If you have been diagnosed with endometritis and planning a pregnancy is now the only thing that occupies your thoughts completely, then you should know that pregnancy is undesirable until complete recovery.
Comprehensive treatment of endometritis should consist of the following:
- antimicrobial therapy with broad-spectrum antibiotics to normalize the uterine microflora;
- metabolic therapy, including drugs that improve the rheological properties of blood, have an antioxidant effect, and enzyme preparations;
- immunomodulators to correct immune imbalance;
- physiotherapeutic procedures;
- taking combined hormonal oral contraceptives to normalize a woman’s hormonal status and “prevent” premature pregnancy.
On average, it will take a woman at least six months to complete complete therapy for chronic endometritis. This group of patients does not require hospitalization and can undergo the prescribed course of treatment at home.
In addition to drug therapy, treatment should be supplemented by giving up bad habits, following healthy eating rules and taking vitamin complexes.
Endometritis and pregnancy are two conditions that do not exclude each other, but one significantly aggravates the other. According to statistics, about 45% of women with endometritis encountered difficulties in conceiving, more than 65% of patients lost their pregnancies at short notice.
Pregnancy in this group of patients is usually difficult and with complications. Pregnant women and chronic endometritis require closer attention from obstetricians and gynecologists. As a rule, these patients visit antenatal clinics twice as often, and they are also indicated for hospitalization in an obstetric hospital during critical periods of pregnancy. In order to prevent the threat of miscarriage, it is reasonable to prescribe progesterone drugs in a minimal dose.
A little about endometritis
Endometritis is the result of the destructive work of viruses and bacteria on the inner lining of the uterus. They cause an inflammatory process on the mucous membrane, interfering with its proper development.
The acute form is easy to detect due to severe symptoms. If the wrong treatment is chosen to eliminate the disease, or it is not completed, it turns into a more hidden form. This is also facilitated by the persistence of disease-provoking factors.
The chronic form may not make itself felt with tangible signs. But one of them is the inability to conceive and bear a child, since the inflamed mucous membrane is unable to hold the embryo. Chronic endometritis and pregnancy are practically incompatible things.
Causes of endometrial inflammation
The main culprits of endometritis are pathogens. The uterine mucosa is normally sterile. It is closely connected with other parts of the reproductive system, so there are several ways for pathogenic bacteria to penetrate it:
- through blood or lymph with long-term infection in other organs and systems;
- ascending, when the vagina and other external reproductive organs become inflamed first.
Damage to the uterine mucosa by bacteria or viruses can occur as a result of:
- incorrect invasion of the organ cavity during a hysteroscopic examination or a simple gynecological examination;
- medical abortion;
- diagnostic or therapeutic curettage;
- transmission of sexually transmitted infections;
- protection;
- sex during menstruation.
Is it possible to get pregnant with endometritis? Of course, but only after his treatment.
Who is at risk of developing the disease?
Under all of the above circumstances, women are at greater risk of developing endometritis:
- leading a too free lifestyle with frequent changes of sexual partners;
- having ;
- suffering from bacterial;
- having or ;
- ignoring hygiene rules, especially on critical days;
- those with weakened immunity (this includes not only women who are often ill, but also those who have recently given birth);
- having diseases of the fallopian tubes, vagina (inflammation of the cervix of the organ is especially dangerous);
- often resort to abortion;
- using douching without a doctor’s prescription;
- recently freed from a sexually transmitted infection.
Symptoms of the disease are determined by its form. In acute endometritis the following appear:
- Abdominal pain of varying intensity, similar to menstrual pain. They become more noticeable when pressing on the abdominal wall in the area of the uterus.
- Severe loss of strength, chills.
- Temperature up to 39 degrees.
- Copious discharge (transparent, yellow, brown, but always with an unpleasant odor).
In chronic endometritis, all signs may be present, but less pronounced:
- low-grade fever;
- weakness, desire to lie down;
- periodic abdominal pain, always occurring after sexual intercourse or physical activity;
- small discharge mixed with pus, blood, and an unpleasant odor.
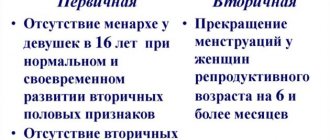
But its main symptoms are related to menstrual function:
- appear due to insufficient development of the uterine layer affected by the disease, in some menstruation stops altogether;
- menstruation becomes noticeable and lasts longer than usual;
- spotting is noticed outside of menstrual periods;
- Menstruation becomes much more painful.
What is endometritis?
Enometritis is a process when the lining of the uterus becomes inflamed. The pathology is dangerous due to the spread of infection; over time, it is localized on neighboring organs: ovaries, fallopian tubes, causing a number of associated complications. As a result of the inflammatory process, adnexitis, oophoritis occur, adhesions and polyps appear, which adversely affects reproductive function and leads to infertility.
Initially, an acute form of the disease occurs; over time, with inadequate treatment or its absence, it develops into a chronic form. Acute endometritis cannot be ignored; it passes with pronounced symptoms. A chronic disease can develop over several months or years; a woman, as a rule, does not pay attention to minor signs.
The cause of the disease is:
- the postpartum period, when the body of the uterus is in a vulnerable state, the risk of infection increases;
- intrauterine contraceptives;
- frequent douching;
- STIs (sexually transmitted infections), such as trichomoniasis, chlamydia and others;
- violation of the vaginal microflora (bacterial vaginosis);
- gynecological procedures (curettage, hysteroscopy, installation of an intrauterine device).
When endometritis occurs, the reproductive organs suffer, without which full fertilization is impossible. Due to extensive inflammation and disruption of the functioning of the uterine body, women often experience infertility.
Diagnosis of endometritis
Even the acute form of the disease cannot be diagnosed by a specialist only based on the signs listed by the patient. They are too similar to the manifestations of other pathologies. Hardware methods and laboratory tests will help make a diagnosis, including:
- general blood test, which also reveals ESR;
- Ultrasound of the uterus and appendages;
- flora smear to determine the composition of bacteria in the vagina;
- hysteroscopy to obtain organ tissue for examination;
- sowing material to determine the type of pathogens;
- blood test for antibodies to rule out or confirm the presence of viral infections;
- PCR diagnostics, which makes it possible to identify all microorganisms involved in the occurrence of the disease.
Some women also need a blood test for hormones to understand how much endometritis has disrupted the functioning of the reproductive system as a whole. Disorders in this area become a serious obstacle to conception. And to the question of whether it is possible to get pregnant with uterine endometritis, the doctor will answer only after a complete diagnosis of the expectant mother’s body.
An acute form of endometritis forces a woman to see a doctor. But in chronic conditions, her state of health is such that she may not associate the malaise with the disease, but blame fatigue and nerves. This allows endometritis to destroy the lining of the uterus for a long time. The inflammation can progress further, affecting the fallopian tubes and ovaries.
Naturally, you can get pregnant with endometritis, but only in the initial stages of the disease. The progression of the disease results in:
- lack of ovulation;
- impossibility of implantation of the fertilized egg;
- pregnancy fading;
- miscarriages.
That is, the general result of chronic endometritis is infertility.
Treatment of endometritis
Considering the culprits in the development of the infection, therapy should be directed primarily against them, that is, contain antibacterial drugs:
- “Amoxicillin”;
- “Ciprofloxacin”;
- “Cephalexin”;
- “Gentamicin.”
In addition to injections and tablets, vaginal suppositories will help, including Ternidazole, Nystatin, Niomycin, Prednisolone, Betadine.
The doctor may add to these:
- antimicrobial drugs “Tinidazole”, “Ofloxin 400”;
- antiviral “Atskilovir”, “Zovirax”, “Virolex”.
In addition to the direct effect on pathogens, you will need the following:
- diclofenac, ibuprofen, analgin to relieve pain and inflammation;
- suprastin, tavegil, claritin to eliminate edema;
- kipferon, vitamins to stimulate the immune system;
- hemostatic agents “Vikasola”, “Tranexama”;
- hormonal drugs “Duphaston”, “Utrozhestan” to normalize the cycle and development of the endometrium.
In case of severe bleeding, curettage is performed, but conservative treatment is not canceled. The choice of drugs is up to the doctor; a combination of several antibiotics in different forms is possible. It is important to complete the entire course without giving up medications when you feel better.
Planning pregnancy after getting rid of endometritis
In order for endometrial function to be fully restored, treatment must be brought to its logical conclusion. The test results become the point:
- Ultrasound of the pelvis;
- endometrial tissue biopsy;
- smear on vaginal microflora;
- blood tests for hormones.
If the doctor is convinced that they are satisfactory, nothing prevents the woman from starting to plan a pregnancy.
Many people are sure in advance that there is no possibility of getting pregnant naturally with chronic endometritis. But if the disease, even becoming chronic, has not existed without treatment for years, the chance of conceiving without the use of medical technologies remains.
Some people succeed in this in the first cycle after stopping hormonal medications. Others are prescribed a course of progesterone drugs that promote the development of the endometrium for 3-6 months, after which the mucous membrane acquires a thickness normal for each stage of the cycle. It is good to supplement it with physiotherapy using UHF, magnetic waves, and calcium chloride. This will help restore the endometrium and prevent the formation of adhesions in the uterus, which will subsequently interfere with pregnancy.
Pregnancy after endometritis is quite possible, but treatment should be a mandatory part of planning. To restore the proper functioning of a woman’s reproductive organs, the use of drugs will also help:
IVF increases the chances of pregnancy after treatment of endometritis. The method allows you to “unload” the female body, helping the process of bringing the egg and then the embryo to the desired state.
But pregnancy through IVF does not eliminate possible difficulties with pregnancy. A woman should especially carefully monitor her well-being, not lift heavy objects, eat right, and take vitamins. It will be necessary to take progesterone medications to maintain the thickness and friability of the endometrium necessary to retain the fertilized egg.
And some women have to spend a significant part of the time of gestation in a horizontal position.
If endometritis develops during pregnancy, you will have to be under constant medical supervision without IVF.
The disease, despite the absence of obvious signs in its chronic course, can leave consequences for life. Therefore, it is better to start treatment as early as possible, then the chances of getting pregnant after endometritis are higher.
The appearance of inflammatory processes in the pelvic organs is quite common, statistics remind us of this. According to her data, such a problem occurs in every tenth woman. And if some, fearing for their health, immediately go to the doctor, undergo the prescribed course of therapy and do not remember the disease for a long time, then others prefer restraint, self-medication, which is inappropriate in this case, and risk the appearance of serious complications.
A visit to a qualified specialist when symptoms of female diseases appear is a must. Moreover, sooner or later this will still have to be done, since there will be a need to plan a pregnancy.
Chronic endometritis is one of the most common diseases of the female genital area. This disease is an inflammation of the mucous membrane lining the inner cavity of the uterus. It can be very difficult to detect and often happens that this occurs only after a miscarriage or long-term infertility.
What is the main danger of uterine endometritis during pregnancy? And which activities will be most important in planning? This is what we will talk about.
Endometritis as a cause of infertility
home
Infertility treatment
Treatment of female infertility
Diseases causing infertility
Endometritis
Endometritis is an inflammatory disease of the inner layer of the uterus. It can be acute or chronic. Acute inflammation most often occurs after mechanical damage to the endometrium (childbirth, abortion, intrauterine contraception).
Chronic endometritis usually develops after acute inflammation of the endometrium, or with dysbiosis (disturbance of the mycofolor) of the vagina. The leading role in pathogenesis belongs to the activity of opportunistic flora.
Endometritis is quite often the cause of infertility in women.
- Reproductology
- Treatment of female infertility
- Can't get pregnant for a year
- When to see a doctor?
Endometritis and infertility
There are many complications that can accompany chronic endometritis, and infertility is one of them. Reproductive function is impaired due to damage to the endometrium - the inner layer of the uterus, which must receive a fertilized egg for pregnancy to occur.
However, if a woman has endometritis, infertility does not always develop. Pregnancy is possible if there are no deep morphological changes in the endometrium and no pronounced inflammatory process. But without treatment for this condition, the risk of miscarriage or miscarriage increases significantly.
If a woman is diagnosed with endometritis, treatment of infertility comes down mainly to restoring the endometrium affected by the pathological process.
Possible formation of intrauterine synechiae. This occurs with a long course of the disease or in the case when a woman has suffered acute endometritis. Infertility in this case is treated using surgical methods.
Endometritis and pregnancy
Infertility does not always develop if a woman has been diagnosed with chronic endometritis, and pregnancy may well occur even without treatment. This is possible if there are no pronounced changes in the endometrium and it fully performs its function. But this increases the risk of miscarriage or miscarriage.
Endometritis and frozen pregnancy are not uncommon. Much more often this disease leads to recurrent miscarriage than infertility. Therefore, when planning a child, a woman requires treatment for endometritis, and pregnancy after completing a course of therapy is much more likely to end in childbirth.
Endometritis and IVF
One of the contraindications to in vitro fertilization is endometritis. Before IVF, a woman necessarily requires treatment. After the destruction of pathogenic flora and restoration of endometrial function, pregnancy can occur.
With inflammation of the endometrium, the ovaries are usually not affected by the pathological process, so the woman’s hormone levels are normal, and the cycle is not always disrupted. This allows you to get a sufficient number of good eggs, even if a woman has chronic endometritis.
Before IVF treatment, treatment is required primarily because without it, the embryo will not be able to implant into the wall of the uterus. If this happens, the pregnancy will most likely end in miscarriage in the early stages.
Treatment of chronic endometritis before IVF can be prescribed differently, and it depends on the etiology and course of the disease.
A woman can be diagnosed with specific or nonspecific endometritis. Treatment before IVF usually involves the use of broad-spectrum antibiotics. Specific (gonorrhea, tuberculosis, actinomycosis) inflammation of the endometrium is rare.
In the chronic form of the disease, the pathological process is more often associated with the activity of opportunistic flora.
Deterioration of the endometrium is the main problem caused by chronic endometritis, and IVF cannot be performed until the inner layer of the uterus has been restored. This usually takes several months.
The disease can occur in different ways:
- atrophic – the endometrium becomes thinner, the glands atrophy, stromal fibrosis occurs;
- hypertrophic – hyperplasia of the mucous membrane is observed;
- cystic - the glands are compressed by fibrous tissue, their contents thicken, and cysts form.
Diagnosis of endometritis at VitroClinic
Diagnosis of endometritis is carried out in several areas:
- medical history and examination by a gynecologist;
- laboratory tests (blood and smear tests);
- Ultrasound;
- endometrial biopsy.
At VitroClinic you can undergo a full examination to detect endometritis.
Only after diagnosis and based on the data obtained, the doctor selects an individual treatment regimen. In some cases, hospitalization in a hospital may be necessary.
In the process of restoring the endometrium, different methods are used - this includes taking drugs orally and using them locally.
After a few months, if the doctor believes that the endometrium is ready to accept the embryo, you can become pregnant naturally or through in vitro fertilization. After IVF, if pregnancy occurs, it is usually supported with hormonal drugs for up to several months (individually). A successful pregnancy after endometritis is more than likely with the right approach under the supervision of a competent doctor.
Author of the text: Gynecologist-reproductologist, Ph.D. Pavlukhina S.S.
Cost of services
All services
| Complete blood count with leukocyte count + ESR (blood with EDTA, period: 1 day) | 440 rub. |
| Initial consultation with an obstetrician-gynecologist (without ultrasound) | 3 000 rub. |
| Initial consultation with a gynecologist-reproductologist (including ultrasound) | 4 000 rub. |
| Gynecological smear (smear from the urethra, cervical canal, vagina, period: 1 day) | 370 rub. |
| Endometrial biopsy (Pipel biopsy) (including histological examination of surgical material) | 8 000 rub. |
| Ultrasound of the pelvic organs | 3 000 rub. |
Our specialists
doctor
Bazanov Pavel Aleksandrovich Head of the VitroClinic network of clinics, Ph.D.
Sign up Schedule
Gorskaya Olga Sergeevna Gynecologist-reproductologist, Ph.D.
Sign up Schedule
Kuznetsova Irina Andreevna Gynecologist-reproductologist, Ph.D.
Sign up Schedule
Pavlukhina (Selezneva) Svetlana Sergeevna Gynecologist-reproductologist, Ph.D.
Sign up Schedule
Tupikina Natalya Vladimirovna Gynecologist-reproductologist, Ph.D.
Sign up Schedule
Maeva Nora Khachaturovna Gynecologist-reproductologist
Sign up Schedule
Mityushina Natalya Gennadievna Head of the Department of Embryology, embryologist, Ph.D.
Sign up Schedule
Gavrilova Olga Evgenievna Embryologist, geneticist
Sign up Schedule
Iskakova Aliya Temirkhanovna Obstetrician-gynecologist, reproductive specialist
Sign up Schedule
Soldatova Marina Fedorovna Ultrasound diagnostics doctor
Sign up Schedule
Rusanova Galina Pavlovna Ultrasound diagnostics doctor
Sign up Schedule
Patient reviews
Read more reviews on the forum Oksana Zh.
I want to tell my story. My husband and I tried for a long time to get pregnant and carry a child to term. We went to different doctors, who at some certain point threw up their hands and said that they could not help us. This continued until chance brought me together with the wonderful doctor Natalya Vladimirovna Tupikina. From our first meeting, Natalya Vladimirovna showed concern, attention, care, showed her competence, and used treatment methods that other doctors did not use on me. After a short time, my husband and I managed to get pregnant, carry and give birth to two beautiful babies - a boy and a girl. For this we are very grateful to Natalya Vladimirovna, who was by our side throughout our difficult pregnancy, supported us, showed medical interest, human care, and quickly responded to various situations related to bearing children.
More details
Nata
I really liked the consultation with Svetlana Mikhailovna. I called and wanted to make an appointment with another doctor, but over the phone they told me that a new ultrasound doctor had appeared and was highly recommended. I went because... The time and day of the cycle coincided with the appointment of this doctor. And I didn’t regret it at all! I looked at everything very carefully. She explained everything in detail and showed it on the big screen. True, my doubts about the endometrium and a very small fibroid were confirmed. For some reason, the other doctors didn’t see anything. But there were problems and no one could say anything intelligible. Now I will stay with her, as if I were seeing a gynecologist. I hope that during gynecological appointments she will also be attentive and help me.
More details
What causes the appearance of chronic endometritis?
Since adolescence, every woman knows that every month, under the influence of hormones, a number of changes occur in her body that are necessary for successful conception and bearing a healthy baby.
It is also no secret that implantation and subsequent growth of the embryo occurs in the uterus, and its inner lining is ideal for this: it is sterile, rich in all necessary nutrients and is capable of sensitively responding to all sorts of changes in the hormonal background, creating all the conditions for normal fetal development.
But if infectious inflammation occurs in the vagina or on the cervix, viruses and microorganisms can ascend into the uterine cavity.
Poor immunity, lack of treatment or incorrectly selected therapy allows the infection to penetrate the endometrial cells and become its “resident”. And under the influence of bad habits, stress, hypothermia or other negative factors, the disease begins to constantly “disturb” the woman’s immunity and sooner or later becomes chronic.
As a result of ongoing inflammation, the mucous membrane in the endometrium, as a rule, begins to be replaced by connective tissue, resulting in poor circulation and decreased sensitivity to hormones. And this can lead to improper attachment of the embryo to the wall of the uterus.
All these reasons invariably indicate that treatment of chronic endometritis should be carried out before pregnancy. Otherwise, there may be difficulties with conception, insufficiency of the 2nd phase of the cycle, miscarriage or its “fading” in the initial stages.
The main factors provoking the appearance of endometritis are:
- any surgical interventions in the uterine cavity (abortion, hysteroscopy, curettage, endometrial biopsy, etc.);
- infectious diseases of the external genitalia, vagina or cervix;
- bacterial vaginosis;
- radiation therapy;
- intrauterine devices;
- various complications after pregnancy or childbirth.
Symptoms and diagnosis of chronic endometritis
The main symptoms that can be used to suspect CE are:
- uterine bleeding (before, after, or between menstrual periods)
- nagging pain in the lower abdomen
- painful menstruation
- pain during intercourse
- serous leucorrhoea with an unpleasant odor
- non-developing pregnancies and IVF failures
- infertility
Often there are no signs of the disease at all. Therefore, to clarify the diagnosis, ultrasound, hysteroscopy, histological examination, and immunohistochemical examination of the endometrium are used.
Ultrasound examination of the uterus
Signs of HE:
- expansion of the uterine cavity
- change in the structure of the endometrium (thinning or discrepancy between the thickness and the phase of the cycle).
- presence of gas bubbles
- foci of sclerosis, calcification and fibrosis in the basal layer
- asymmetry of the uterine walls
Often several signs are identified. Ultrasound is performed twice: on days 5-7 and 17-21 of the cycle. However, based on ultrasound, the diagnosis of CE can only be suspected!
Hysteroscopy
Signs of HE:
- heterogeneous endometrial thickness
- polyps
- uneven redness
- increased endometrial bleeding
The procedure is carried out on days 7-10 of the cycle. A diagnosis can be made only in 16-35% of cases. In approximately 30% of cases of cholecystectomy, the hysteroscopic picture is ideal, so the method also only allows one to suspect the disease.
Histological examination
Only with the help of this method can the diagnosis of CE be confirmed or refuted. It is carried out by pipel biopsy or diagnostic curettage on the 7-10th day of the menstrual cycle (but in no case in the second phase!). The presence of CE is indicated by plasma cells and lymphocytes, foci of fibrosis or sclerosis of the stroma during a long course of the disease, sclerosis of the walls of the spiral arteries that feed endometrial cells.
Immunohistochemical diagnostics
Its essence is to determine the sensitivity of endometrial receptors to estrogen and progesterone in order to select a further treatment regimen.
Planning pregnancy: how to get rid of the disease in time
It is necessary to treat chronic endometritis when planning pregnancy in a comprehensive and step-by-step manner. The main goal of therapy should be both restoration of the endometrium and normalization of reproductive function in general.
The first stage includes
antibiotic therapy.
Only the attending physician should prescribe this or that antibacterial drug and only after conducting laboratory tests to determine the causative agent. It is also possible to prescribe intrauterine infusions of drugs.
From the very first day of the cycle, the use of immunostimulants should be indicated to strengthen the body's immune forces. But before this, the doctor must check the woman’s interferon status (i.e., the state of her body’s innate nonspecific defense) and determine sensitivity to interferon inducers.
The second stage is divided into:
- Metabolic therapy. It is aimed at improving the supply of oxygen and glucose to the endometrium and increasing local immunity.
- Physiotherapy. It is usually prescribed taking into account all gynecological pathologies of a woman. It has a resolving effect, increases blood circulation and also increases local immunity.
If necessary, hormone replacement therapy may be prescribed.
In general, treatment for endometritis takes three to four months. The effectiveness of the treatment measures taken is determined 2 months after the end of therapy. After such treatment of chronic endometritis, women can plan both natural pregnancy and with the help of assisted reproductive technology (ART) programs.
Features of pregnancy with chronic endometritis
Cases when a woman manages to become pregnant against the background of a progressive disease are quite rare and such a pregnancy is usually considered doomed. If the egg was able to implant in the affected uterus, then the threat of miscarriage will persist throughout the entire period of gestation. However, other complications may accompany such a pregnancy.
Endometritis is a chronic disease of the female reproductive system that is asymptomatic. The pathology occurs in women of childbearing age; the disease is especially dangerous at the age of 25-35, when a girl faces the question of pregnancy.
Modern scientific research in the field of medicine shows that women with chronic endometritis as a concomitant disease suffer from infertility, undeveloped pregnancy and recurrent miscarriage in almost 100% of cases. Traditional treatment methods are not always able to cope with this pathology, which attracts the close attention of gynecologists. This article will discuss the possibilities of pregnancy and gestation for women with chronic endometrial pathology.
Treatment of chronic endometritis
A woman who has heard this diagnosis and is aware of its consequences immediately wonders whether it is possible to get pregnant with chronic endometritis. After all, in order for the egg to be fertilized and attached to the uterus, and then develop normally, a healthy endometrium is needed. If this disease is not treated, then it will be difficult to get pregnant and, even if you manage to do this, there is a very high risk of miscarriage and fetal death. After all, pregnancy, even after treatment of chronic endometritis, does not always proceed normally and often does not end with childbirth on time. Therefore, following the doctor’s instructions must be approached with all seriousness.
The chronic form of endometritis is more dangerous for a woman’s reproductive health than the acute form. After all, the initial stage of inflammation is characterized by distinctive signs that are easy to notice and promptly seek medical help. With timely treatment of acute endometritis, not a trace remains of it, a woman can easily become pregnant and give birth to a baby. Chronic endometritis is difficult to get rid of, so complete rehabilitation requires the patient to follow the doctor’s recommendations a lot of time and patience. The treatment regimen for chronic endometritis is quite complex and depends on the stage of the disease. Antibiotics are primarily used as drug therapy for chronic endometritis. The gynecologist determines the doses of antibacterial drugs and their dosage regimens depending on the severity of endometritis and the form of its course.
Treatment of chronic endometritis also involves the treatment of infectious diseases that accompany it and may have led to its appearance. If there are several pathogenic microorganisms in the body, more than one type of antibiotic may be used. Also, doctors usually prescribe intravenous administration of protein and saline solutions, which help cleanse the body, lower body temperature, relieve intoxication and improve the patient’s condition as a whole. Supplement treatment with vitamins and proper nutrition. Doctors use drugs that enhance immunity and antifungals.
In some cases, to achieve a better therapeutic effect, local therapy is used, when medications are injected into the inflammation in the uterus. Treatment of chronic endometritis takes about 3-4 months.
Treatment of chronic endometritis
The effectiveness of treatment for chronic endometritis is checked no earlier than two months after its completion. The doctor assesses the symptoms that bother the patient, performs an ultrasound diagnosis of the pelvic organs, as well as an endometrial biopsy. Remission of chronic endometritis requires new treatment.
For the treatment of chronic endometritis in remission, the doctor often reconsiders the correctness of the treatment at the initial stage and mainly uses physical therapy, which helps improve blood circulation in the uterus, promote regeneration and stimulate its receptive function. It is also possible to prescribe hormonal drugs.
Causes of infertility and miscarriage
The uterus is the main organ of the reproductive sphere, where all stages of conception and implantation of the embryo, and then the development of the fetus, take place. The inside of the uterus is lined with a layer of epithelium - the endometrium. In accordance with the phase of the menstrual cycle, the thickness of the endometrium changes due to active regeneration. The greatest thickness of the endometrium corresponds to the middle of the menstrual cycle, when the egg is released and the woman’s body prepares for conception. A regenerated thick layer of the endometrium is the main condition for successful implantation of the embryo into the mucous wall of the uterus and further development of the fetus.
In chronic endometritis, endometrial regeneration does not occur due to the inflammatory process. With endometritis, the processes of fibrosis (proliferation of connective tissue at the site of inflammation), disruption of hormonal regulation at the local and systemic level, as well as disruption of the normal flora and cellular composition of the uterine mucosa predominate.
Thus, infertility and miscarriages with endometritis occur for several reasons:
- Violation of the morphology of the endometrium with replacement by connective tissue. As a result, the fertilized egg cannot implant in the uterus and is released along with vaginal discharge. In this case, the woman does not even suspect that she was pregnant.
- Progesterone synthesis disorders. Progesterone is the only hormone of the reproductive system that maintains pregnancy, maintaining it for a long time, by reducing the tone of the inflamed uterus. In chronic endometritis, progesterone is not produced, since the synthesis of inflammatory mediators predominates, which is manifested by termination of pregnancy in the early stages.
- Pregnancy with endometritis does not occur due to the inactivation of male sperm already at the stage of conception. In the process of inflammation, phagocytic cells take an active part: macrophages, neutrophils, dendritic cells. They destroy foreign antigens, including sperm. When male germ cells enter the uterine cavity, they are phagocytosed and destroyed by inflammatory macrophages and neutrophils.
It is important to know! Chronic endometritis is often asymptomatic. For its timely detection, women need to undergo annual preventive medical examinations with a gynecologist. This way you can significantly reduce the risk of infertility in the future.
Chronic endometritis and pregnancy
Women diagnosed with endometritis in the chronic stage who want to give birth to a child will likely face a number of problems.
Are there any chances for a healthy pregnancy with endometritis?
Can a woman suffering from a chronic form of the disease hope for successful conception and birth of a child? Doctors are unanimous on this score - chronic endometritis and planning a pregnancy cannot be combined in any way; there is very little chance of carrying and giving birth to a healthy child.
Firstly, the degenerated uterine mucosa will not be able to become a reliable basis for the embryo to attach to it, even if fertilization occurs. It happens that the egg manages to remain in the affected area of the endometrium, but the risk of miscarriage is extremely high and will persist throughout the entire pregnancy.
Most often this happens at the initial stage, while some women do not even know that they could already become a mother. Therefore, if someone is guilty of their “infertility,” this is another reason to undergo a thorough examination by a specialist.
The second serious threat is that with the onset of pregnancy, the inflammatory process does not die down, but continues to actively develop, affecting not only the walls of the uterus, but also spreading to the growing fetus. Most often, this also ends in miscarriage at various stages; cases of intrauterine intoxication and death of the embryo cannot be excluded.
Are you sure that you have this particular disease? Look again at the symptoms of endometritis to be sure. A disease such as colpitis has many variations, you can read about one of them in our article.
Can a woman have children after an ectopic pregnancy? Follow the link to find the answer.
Don't lose heart - everything can be fixed!
After such difficult conclusions, women should be reassured - the overwhelming majority of cases of chronic endometritis can be completely cured, after which you can plan to increase your family.
Treatment of the disease is carried out, as a rule, without hospitalization, on an outpatient basis, and includes a course of therapeutic procedures using antibiotics, carefully selected by the doctor taking into account the pathogenic microflora of the genital organs.
Taking anti-inflammatory drugs is combined with drugs that boost immunity. In some cases, intrauterine administration of drugs is practiced. Surgical interventions are extremely rare, in cases of extremely advanced forms of the disease and the absence of a therapeutic effect from medications.
If the dynamics of treatment are positive, the inflammatory process is relieved, restorative procedures (physio- and phytotherapeutic) are carried out, promoting the regeneration of endometrial cells and restoring its original properties.
The general course of treatment can last up to four months; the first significant conclusions are drawn after the first two. Perhaps this may seem like too long a period, but the results are worth it: pregnancy after endometritis, detected and treated in time, is not only possible, but also completely safe for the expectant mother and baby.
Disease prevention, regular examinations by specialists, a healthy lifestyle, optimism and faith in your inexhaustible feminine capabilities are the key to a future happy motherhood.
What you need to know about treatment when planning pregnancy
- Follow your doctor's recommendations. Find an experienced gynecologist who has repeatedly treated endometritis.
- If possible, see a fertility specialist to check your chances of pregnancy.
- During the therapeutic course, use contraceptives so as not to deplete your body with abortions.
- Antibacterial and anti-inflammatory drugs are used for treatment. Physiotherapeutic procedures have a great effect in the treatment of endometritis: UHF exposure, massage.
- To restore hormonal levels, psychotraumatic influences are excluded and sedatives are prescribed.
- Heavy physical and mental labor is not recommended during this period of time. It is important to create a favorable atmosphere around yourself.
Important information! Before a course of treatment, a woman needs to be patient. Treatment lasts from 4 to 6 months, and pregnancy itself occurs 2-4 months after it.
Also, do not forget that after the last miscarriage, at least six months must pass before the onset of a new pregnancy. This is why it is so important to use contraceptives during treatment, especially if the woman has previously had spontaneous abortions due to endometritis.
Course of pregnancy
Numerous reviews from women and doctors indicate that after treatment of endometritis, pregnancy occurs with a probability of up to 90-100% and ends in childbirth in 60-70% of cases. A pregnant woman should be regularly observed at the antenatal clinic, at least 2 times a month.
If there are signs of a threat of miscarriage, progesterone drugs (preserving pregnancy) are prescribed. When pregnant, it is advisable to take vitamin complexes, after consulting with your doctor.
A pregnant woman is at high risk of miscarriage, so it is necessary to limit physical activity and stress. Heavy lifting is strictly prohibited.
In general, 60-70% of pregnancies end in childbirth; most women carry and give birth to a second child without problems.
IVF after endometritis
Modern reproductive technologies have brought into our lives the possibility of in vitro fertilization. In cases of recurrent miscarriage and infertility, this procedure is often the only chance to have children. However, there are nuances here.
Difficulties with IVF are associated with endometrial restructuring. If the patient cannot become pregnant and carry a fetus to term, this means that the endometrium is not ready to accept the embryo and preserve it. With IVF, the egg is fertilized outside the uterine cavity, after which the embryo is artificially implanted into the mother, but there is a high risk that the endometrium will not accept this embryo either.
Research shows that only a small percentage of women with chronic endometritis carry and give birth to children after in vitro fertilization. To increase efficiency, it is better to use several attempts at embryo transfer with a short time interval.
Is it realistic to get pregnant?
The chances of a positive outcome from IVF depend on the characteristics of the woman’s body and her general health. Properly treated endometritis and normalization of the menstrual cycle are the key to successful conception. It is important to understand that in vitro fertilization is a “lottery” - doctors cannot guarantee that at least one of several fertilized eggs will implant.
Fulfilling the above conditions increases the chance of conception. The future dad should also prepare for the IVF procedure. The man undergoes a full examination of his health, then is cured of diseases that interfere with fertilization.
For several months before IVF, a man should refuse to visit the bathhouse, sauna, and not drink alcohol. These measures will help reduce the negative impact of external factors on sperm.
Pathology is a significant obstacle to conception. This is due to the fact that pathological disorders of the endometrium cause the production of lymphocytes in the basal layer, so the substances do not have the power to implant an already fertilized egg inside the uterine mucosa and cause embryo rejection.
All this becomes a provocateur of infertility, miscarriage or frozen pregnancy. To avoid such negativity, treatment is required.
After the embryo is fixed in the uterine cavity, the pregnant woman must take a number of medications:
- folic acid with iodine;
- improving blood circulation;
- medications that block the contraction of the muscles of the uterus to avoid spontaneous abortion.
Symptoms and treatment
Endometritis in acute form is usually manifested by fever, vaginal discharge, pain with localization of pain in the lumbar region or lower abdomen. Sometimes cycle disorders are observed. During an objective examination, the doctor discovers an enlarged uterus, painful upon manual examination.
At the same time, in the chronic form of the pathology, pronounced symptoms may be absent. Body temperature is usually within normal limits. There is no discharge at all, or it is small in quantity and mucopurulent in nature. Diagnosis is difficult because the patient usually does not see a doctor.
There may be no symptoms at all. In this case, chronic inflammation in the uterus is detected during diagnosis for other diseases.
Treatment of endometritis has several goals. But the main one is the destruction of pathogenic microbes. For this, a course of antibiotic therapy is prescribed. Preference is given to broad-spectrum antibiotics.
In parallel, anti-inflammatory and symptomatic therapy is used.