What is endometrial hypoplasia?
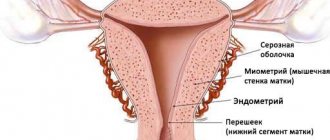
Hypoplasia of the uterine endometrium is a pathology in which there is underdevelopment of the inner mucous membrane of the uterus , which covers its surface and is called the endometrium. The main task of this layer is to create a favorable environment for the implantation of a fertilized egg into the uterine cavity. And in the case when a woman has thinning of the endometrium (hypoplasia), this pathology does not allow the egg to implant normally, therefore, pregnancy does not occur. In such a situation, the patient is diagnosed with infertility.
In order for the fetus to be securely implanted in the uterus, the thickness of the endometrium must be at least seven millimeters.
When a woman has hypoplasia, the attachment of the egg may occur, but it will be unreliable, therefore, such a pregnancy may end prematurely.
In addition, sometimes a woman may experience uterine hypoplasia, characterized by underdevelopment of the uterine cavity. This pathology is called the baby uterus. This deviation is fraught with complications during pregnancy.
https://youtu.be/Udk9Ncr7cK8
What does this mean?
This issue should be considered in more detail.
If a woman has thinning of the endometrium, that is, hypoplasia, implantation does not occur; the cell, in principle, is not able to gain a foothold in such a thin tissue. In this case, the woman is diagnosed with infertility. To successfully implant an embryo in the uterine cavity, the endometrium must have a thickness of at least seven millimeters. If the patient has hypoplasia, then there is a possibility of implantation, but the attachment may be characterized by a lack of strength, and such a pregnancy may cease to develop in the future.
How it manifests itself
In ordinary life, the hypoplastic endometrium does not manifest itself in any way; the first symptoms appear during the planning period for fertilization. An experienced doctor can determine diseases by how the girl develops, whether she has periods, etc.
The main symptoms of the pathology are:
- Long absence of pregnancy;
- Cases of miscarriage and miscarriages;
- The presence of adnexitis, endometritis and other diseases of the reproductive system;
- Abortion, curettage;
- The appearance of menstruation after 16 years;
- Irregular, scanty menstruation;
- Dissatisfaction with sex life;
- Insufficient hair growth.
The above signs of endometrial hypoplasia should be taken into account, but not guided by them for independent diagnosis. Only after a complete examination can the doctor confirm or deny the presence of pathology.
Causes of endometrial hypoplasia
The main factors provoking the appearance of endometrial hypoplasia are the following:
- the presence of chronic endometritis;
- inflammatory processes in the pelvic area;
- improper blood circulation in the pelvic area;
- the mucous membrane of the uterine cavity is damaged as a result of surgery;
- disruptions in the functioning of the endocrine system;
- the presence of infections that are transmitted during sexual intercourse;
Also, do not discount the factor of heredity. So far, this fact has not been fully proven, but health workers believe that if the mother had moderate endometrial hypoplasia, then her daughter may also develop the same disease.
Causes
The main causes of endometrial hypoplasia are:
- chronic endometritis - inflammation of the inner mucous layer of the uterus;
- infectious and inflammatory processes of the pelvic organs;
- circulatory disorders in the pelvis;
- damage to the uterine mucosa as a result of surgical interventions;
- endocrine disorders;
- congenital pathologies of the uterus.
Any of these factors can have a negative impact on the condition of the uterine mucosa and lead to thinning of the endometrium or disruption of its functions. It is important that the doctor performing the diagnosis has complete information not only about the patient’s current condition, but also about any gynecological procedures, operations or diseases she has undergone in the past.
Therapy
For a patient diagnosed with endometrial hypoplasia, it is necessary to select treatment depending on the cause of the pathology.
The set of measures includes the prescription of medications, physical therapy, and, if necessary, surgical intervention.
If the cause of the appearance is hormonal deficiency, then the following is selected:
- oral contraceptives that normalize hormonal levels;
- progesterone drugs to reduce the initial manifestations of hypoplasia;
- hormonal injections of estradiol to increase the normal volume of the endometrium.
Important! Duphaston causes fewer side effects and is better absorbed!
Chronic inflammation of the reproductive organs, as a factor in the appearance of impaired growth of the intrauterine membrane, requires a different approach.
This is the direct elimination of infections: antibacterial tablets, immunomodulators, suppositories that restore vaginal microflora.
Physiotherapeutic treatment of endometrial hypoplasia in the uterine cavity improves blood supply and is used as an additional method.
These are gynecological massage, laser therapy, ozokerite and diathermic methods.
After consulting a gynecologist with his permission, it is worth turning to the teachings of Ayurveda, practicing the use of folk remedies, paying attention to short therapeutic diets, and meditation.
Important! Followers of Ayurveda do not exclude the possibility of surgical operations!
Features and symptoms of the disease
When a diagnosis of mixed endometrium is made, its type is immediately specified - hypoplastic or hyperplastic. Most often, in women of reproductive age, the first type of pathology of the upper layer of the uterine mucosa occurs. It has characteristic features that make it possible to distinguish it from other diseases.
Main features of hypoplastic endometrium:
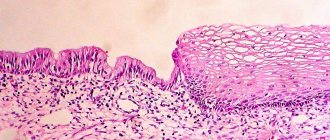
- pronounced underdevelopment of cells of the functional layer;
- the presence of areas that have undergone secretory changes;
- the presence of indifferent type glands in the functional layer of the uterus.
Note! Most often, endometrial hypoplasia affects women of childbearing age who exhibit disturbances in the functioning of the ovaries. Pathology can also occur during the period of decline of childbearing ability, which can be accompanied by heavy bleeding from the uterus, especially of a dysfunctional direction.
Endometrial hypoplasia has its own signs that help doctors identify the disease and prescribe the correct treatment. The overall picture of the development of pathology emerges when all the signs of the disease are combined together.
The main symptoms of endometrial hypoplasia:
- late first menstruation (after 16 years);
- painful menstrual flow, varying frequency with constant disturbances in the main cycle, abundance of flow or, conversely, a small amount of it;
- distinctive features in a woman’s physique (narrow pelvis and shoulders, small mammary glands);
- lack of orgasm during intimate relationships.
It is worth noting that the listed signs are not a sufficient basis for the diagnosis of endometrial hypoplasia. Their presence helps doctors navigate the research and prescribe the woman the necessary set of examinations, which will allow her to study the endometrium and identify abnormalities in it. This may be a histological analysis.
What is hypoplastic endometrium?
The diagnosis of endometrial hypoplasia is made as a result of histological analysis. It represents a histological characteristic of endometrial cells. Endometrial hypoplasia is a serious gynecological disease, because due to it a woman cannot become pregnant.
Disease Information
Hypoplasia is understood as underdevelopment of the tissue of any organ or even an organism. If a woman is diagnosed with endometrial hypoplasia, this means that the upper mucous layer of the uterus is underdeveloped.
The endometrium is the lining of the uterus, which consists of blood vessels and glandular cells. Normally, the endometrium has different thickness (depending on the day of the menstrual cycle). Thus, the highest indicator was recorded on the 24-27th day of the cycle and ranges from 1 to 1.3 cm. The endometrium becomes thinnest on the 3-4th day of the cycle, and its thickness ranges from 0.3 to 0.5 cm .
This disease is most common in women of reproductive age.
However, this problem is the cause of infertility. This is explained primarily by the role of the endometrium in the female reproductive system.
The endometrium is responsible for creating optimal conditions for a fertilized egg to implant into the uterine cavity. For this to happen, the thickness of the endometrium must be at least 7 mm.
With hypoplastic endometrium, the blastocyst simply cannot attach to the thinned tissue. In some cases, even its implantation occurs, but it is not firmly attached, as a result of which the development of pregnancy still becomes impossible and is interrupted.
If a woman cannot become pregnant for a long time, she is sent for histological examination. If the analysis shows that a woman has a mixed endometrium, this means that its tissue contains structures that reflect the influence of both estrogen and progestogen hormones. In this case, the mixed endometrium can be either hyperplastic or hypoplastic. Hypoplastic mixed endometrium has the following features:
- underdeveloped functional layer;
- the functional layer consists of glands of the indifferent type;
- the presence of areas with secretory changes.
Often this picture occurs in the following categories of women:
- during reproductive age in women suffering from ovarian hypofunction;
- during premenopause, which is accompanied by dysfunctional uterine bleeding;
- during menopause, which is accompanied by bleeding.
Endometrial hypoplasia has a number of characteristic symptoms.
Return to zmystSymptoms of endometrial hypoplasia
Based on some signs, one can suspect the presence of this disease in a woman. If hypoplasia is suspected, the gynecologist collects an anamnesis, that is, a medical history, since the prerequisites for its development must be looked for in the past.
The main signs of hypoplasia:
- Menarche. In women with this pathology, their first menstruation occurred at the age of 16 years and older.
- Features of the course of menstruation. Pathological pain, irregular menstruation, short duration, abundant or, on the contrary, scanty discharge - these are the most characteristic deviations from the norm.
- Anorgasmia. If a woman does not experience orgasm during sex, this may also be a symptom of hypoplasia.
- Body features. Typically, women with hypoplasia have a specific figure and unusual appearance: narrow shoulders and pelvis, small breasts, insufficient hair growth.
- Imbalance of the hormonal system. In particular, the release of insufficient amounts of estrogen leads to the fact that the uterine mucosa becomes pathologically thin.
- Infections. We are talking about any infections that are sexually transmitted.
- Inflammation. In particular, we are talking about chronic endometritis, that is, an inflammatory process that occurs in the uterus.
- Abortion. As a result of curettage, the endometrium may also become thinner than the stated norm. This is why doctors do not recommend abortion during the first pregnancy, because this can cause further infertility.
- Receptor dysfunction. If the functioning of receptors that are sensitive to estrogen is disrupted, this can also contribute to the thinning of the endometrium.
- Blood supply disorders. Stagnation of blood in the uterus is one of the causes of the disease.
- Surgical intervention. If a woman has undergone ovarian surgery, this can cause hypoplasia.
- Laboratory research. In this case, the woman takes a blood test for gonadotropic hormones. The analysis is taken on the 20-22nd day of the cycle.
- Ultrasonography. Using the ultrasound method, the actual thickness of the endometrium is determined.
- Biopsy of the uterus. This is a surgical research method. It is prescribed if additional and more accurate information about the condition of the endometrium is needed.
- estrogen (high dosage);
- Aspirin (low dosage).
Of course, these signs alone are not enough to make a final diagnosis, but thanks to them it is possible to make a preliminary diagnosis and refer the woman for further comprehensive examination.
Return to zmystCauses of endometrial hypoplasia
Doctors identify a number of reasons why hypoplasia can develop. The most common ones include:
The factor of heredity cannot be ruled out. Although this fact has not been fully proven scientifically, some doctors do not rule out that the presence of moderate hypoplasia in the mother can cause the development of the disease in the daughter.
Return to zmist Diagnosis and treatment of disease using traditional medicine methods
Prescribing a course of treatment is possible only after a thorough and comprehensive examination. To make a final diagnosis, the doctor refers the patient to the following diagnostic procedures:
Only based on the data received, the doctor prescribes treatment. It is always long-term and depends on how thin the mucous membrane is and the state of the endometrium.
The main method of treatment is hormonal therapy. It is important to take into account not only the degree of hypoplasia, but also the reason that provoked it. So, usually prescribed:
In addition to drug therapy, physiotherapy is prescribed. They are taught in courses, always taking breaks. The following physiotherapeutic procedures have a good therapeutic effect:
- laser therapy, that is, laser irradiation;
- ozokerite therapy, that is, exposure to heat;
- diathermy method, that is, the effect of alternating current on the skin.
The main goal of these procedures is to improve blood circulation in the pelvic organs, in particular in the uterus.
Return to zmistuLikuvannya folk remedies
Alternative medicine is no less effective. Like the traditional one, it also aims to improve blood circulation in the uterus. For this, methods such as:
All of these remedies are effective. They help not only stop further thinning of the endometrium, but also its gradual increase. However, treatment of hypoplasia without hormonal therapy is not carried out.
https://youtu.be/mapFkRh2KsI
If a woman wants to use any of the traditional methods and treat herself, she must inform her doctor about this.
The effect of endometrial hypoplasia on pregnancy
It is very important how thick the endometrium will be during pregnancy and in the early stages. Its minimum norm for a fertilized egg to be successfully implanted is 7 mm.
If at the time of ovulation the thickness of the endometrium is less than the established norm, this can lead to significant difficulties in achieving pregnancy. Conception may not occur at all, and if the embryo is fixed, then there is a risk of spontaneous abortion, an ectopic pregnancy, and other complications during pregnancy or directly during childbirth may occur.
Thin endometrium can cause severe bleeding after childbirth, increased toxicosis, and provoke weak labor. However, today there are enough methods that can successfully eliminate this pathology.
The concept of hypoplasia
Endometrial hypoplasia is a disease in which there is underdevelopment of the uterine mucosa lining its surface. This layer creates the right environment for the egg to move into the uterine cavity. If the endometrium is too thin or a hyperplastic process is observed, the egg cannot attach normally, and as a result there is no pregnancy.
For successful fertilization, the thickness of the functional layer should be 7-13 mm, it depends on the menstrual cycle. At the very beginning, the old endometrium is excreted along with the blood, and after 3 days a new one develops. On days 25-28 of the cycle, the normal thickness of the layer is at least 1 cm. Cases have been recorded when, with hypoplasia, the egg was still attached to the uterus, but weakly, which caused miscarriage in the early stages.
Most often, the pathology appears in women of reproductive age, sometimes diagnosed together with ovarian dysfunction. Often the disease develops as a result of a decrease in the level of female hormones estrogen. The cause of hormonal imbalance may be menopause or improper functioning of the ovaries. In some cases, the endometrium grows excessively, then hyperplasia is diagnosed. Both types of disorders lead to infertility or miscarriages.
Symptoms of the disease
A doctor may assume that a woman has endometrial hypoplasia based on the following signs:
- unsuccessful attempts to conceive a child, which have been going on for a long time;
- the patient’s history of miscarriage, resulting in early miscarriage;
- previous abortions, curettage according to indications, other gynecological and surgical interventions;
- the woman had endometritis, adnexitis or other diseases of the reproductive system;
- The patient’s menstruation is irregular and accompanied by small discharge;
- A woman’s first period appeared after 16 years;
- lack of orgasm during sexual intercourse;
- insufficient hair growth of the genital organs.
Undoubtedly, one cannot be guided only by these symptoms when determining the diagnosis, but their presence is sufficient grounds for prescribing additional examinations to the woman to confirm or refute endometrial hypoplasia.
How to treat hypoplasia
Endometrial hypoplasia and its treatment should be determined only by the attending physician. Therapy is selected depending on the stage of thinning of the mucosa. To eliminate the disease, 3 methods are used - surgical, drug and physical therapy. Often women try to get rid of pathology on their own using folk remedies. Acupuncture, hirudotherapy and other methods aimed at improving blood circulation are also used. Let's consider all the ways to enlarge the endometrium so that a woman can prepare in advance for what awaits her during the therapy period.
Medication
Medicines are used when an imbalance of hormones or sexually transmitted infections that cause inflammation have been detected. The following remedies are used to restore hormonal balance:
- Combined oral contraceptives - necessary to restore endometrial function and hormone levels;
- Homeopathic medicines, for example, Hormel;
- Preparations containing estradiol (Divigel) - promote faster growth of the required amount of tissue;
- Products with progesterone (Duphaston);
Utrozhestan and Duphaston help the mucous membrane to mature, creating good conditions for conception, fertilization and gestation. Hormonal medications reduce the risk of spontaneous miscarriage.
Immunomodulators, antibiotics and agents for restoring vaginal microflora help eliminate pathologies that could cause endometrial hypoplasia. In addition to drug treatment, physiotherapy is prescribed, and in advanced cases, surgery is used.
Physiotherapy is needed to improve blood circulation. For this purpose, gynecological massage, ozokerite therapy, laser exposure, and diathermy are used.
Surgical
The method is used to stimulate the growth of the functional layer. A slight mechanical effect on the uterus is performed using a hysteroscope. In addition, the inner layer can be removed, and then conservative hormonal therapy is prescribed, due to which the endometrium is renewed.
Surgical treatment is prescribed in the following cases:
- Ineffectiveness of drug therapy.
- There are contraindications to taking hormonal drugs.
- Repeated precancerous hypoplasia.
- Atypical hyperplasia during menopause.
Sometimes doctors prescribe cryodestruction, cauterization or laser ablation. During treatment, the pathological area is removed, and a new, healthy endometrium is formed in its place. The treated area is independently removed along with blood clots, the mucous membrane is restored as after menstruation.
Other methods - folk remedies
In the early stages, good results are achieved by non-traditional therapy that improves blood circulation in the pelvis. The most commonly used folk remedies and methods are:
- Mud therapy – clay or mud is applied to the lower abdomen in the form of a compress for 2 hours;
- Medicinal peony tincture - the extract is diluted with water in a ratio of 1:2 and taken 2 ml 3 times a day;
- Hirudotherapy – leeches relieve congestion and activate blood circulation;
- Acupuncture - special needles affect certain points, thereby improving overall health;
- Sage - a decoction is taken orally or used for douching in order to normalize estrogen levels;
- Flaxseed oil – the product is taken on an empty stomach, 1 tbsp;
- Endovasal galvanization - the method activates the pituitary gland area, due to which the cells actively synthesize hormones.
Treatment of endometrial hypoplasia
The treatment regimen for the disease is individual in each specific case and is based on the results of laboratory and instrumental studies. The duration of therapy depends on two factors:
- degree of thinning of the functional layer;
- current state of the endometrium.
Modern medicine offers three methods of treating endometrial hypoplasia:
- medicinal;
- physiotherapy;
- surgical
Medication
Medicines are prescribed if a woman is diagnosed with a hormonal imbalance or genital infections, accompanied by the development of an inflammatory process.
Hormonal drugs are selected individually. Most often used in the therapy process:
- COCs (combined oral contraceptives). They help regulate the level of sex hormones, which over time helps restore the thickness of the endometrium and its functional properties.
- Products containing estradiol. Drugs in this group promote faster growth of the endometrial layer to the thickness required for pregnancy.
- Medicines that contain progesterone. In the vast majority of cases, women are prescribed Duphaston or Utrozhestan. They accelerate the maturation of the mucosa and help in creating the most favorable conditions for the development of a fertilized egg. In addition, the products reduce the likelihood of miscarriage by strengthening the cervix.
When identifying diseases of the genital area that can provoke the development of endometrial hyperplasia, the following are used:
- immunomodulators;
- drugs from the group of antibiotics;
- products that restore vaginal microflora.
Physiotherapy
Physiotherapy is part of the general therapy for endometrial hypoplasia. The techniques used help improve blood circulation in the uterus. This:
- laser treatment;
- hirudotherapy;
- diathermy;
- acupuncture;
- ozokerite therapy.
Additionally, therapeutic exercises, adherence to the principles of dietary nutrition, and gynecological massage are prescribed.
Surgical
A surgical technique in the form of light exposure of the uterine mucosa with a hysteroscope is used if taking pills does not give the expected therapeutic result. The procedure helps stimulate the thickening of the functional layer, which guarantees the successful implantation and consolidation of the fertilized egg and the beginning of gestational development.
Indications for surgical treatment of endometrial hypoplasia, in addition to the ineffectiveness of drug therapy, are:
- presence of contraindications to taking hormonal drugs;
- precancerous form of hypoplasia;
- atypical course of the disease, especially during menopause.
In some cases, cryodestruction, laser ablation or cauterization techniques are used. The procedure removes the pathological area of the endometrium, which is then replaced with a new layer of healthy cells. After treatment, the removed tissue leaves the uterus on its own, and the mucous membrane is restored.
Treatment of endometrial hypoplasia of the uterus is successfully complemented by folk methods. Good results are given by:
- warm clay compresses - the product is diluted with warm water to a consistency convenient for application and applied to the lower abdomen (projection of the uterus) for 2 hours;
- tincture of medicinal peony - the product is diluted with clean water in a ratio of 1:2, the composition must be taken three times a day, 2 ml;
- sage decoction (take 1 tablespoon of dry product per 200 ml of boiling water) - used for oral administration, as well as for vaginal sanitation in order to restore estrogen levels;
- flax oil - the product must be taken in the morning (after waking up) before meals, 1 tbsp. l.
The endovasal galvanization technique shows excellent results. It is based on the activation of the pituitary gland, which ultimately leads to the active synthesis of sex hormones necessary for the body.
Endometrial hypoplasia, diagnosed at an early stage, is well treated. In the case of an advanced or congenital form of the pathology, the likelihood of complete recovery is extremely low. That is why, if suspicious symptoms develop (pain, heavy menstruation, irregular periods, absence of pregnancy), a woman is recommended to seek qualified medical advice and, if necessary, undergo therapy adequate to the condition.
The choice of therapeutic strategy depends on the cause of endometrial hypoplasia. If endocrinopathy is detected, hormone replacement therapy is prescribed - combined oral contraceptives, progesterone and estradiol preparations or their analogues; Vitamin D deficiency is eliminated through nutritional supplements and vitamin complexes.
Diagnosis of endometrial hypoplasia
To identify endometrial hypoplasia, a specialist must prescribe clarifying studies. Initially, you need to conduct a thorough examination of the woman, and for this the doctor may prescribe certain procedures, for example, a blood test that will help determine the level of gonadotropic hormones. This test must be taken 20-22 days after the start of menstruation. An ultrasound may also be prescribed, which can be used to determine the thickness of the endometrium. To obtain a more complete picture, surgical diagnostic methods are used. One such method is a uterine biopsy.
What are endometrial hyperplastic processes?
Hyperplasia is characterized by uncontrolled growth of connective and glandular tissue and enlargement of the uterus.
Drug treatment of uterine hyperplasia - identifying symptoms
The existence of a woman with hyperplastic endometrium becomes dangerous due to possible malignant degeneration and sudden uterine bleeding.
Important! Treatment of hyperplasia for more than four months consists of taking hormonal drugs that suppress the activity of the ovaries, which provokes the growth of the walls of the uterus.
Factors influencing the development of the disease
Any pathology in the endometrium, as well as the uterus, can arise for any reason: stress, ecology, overexertion, concomitant diseases, inflammatory processes in the genital organs, heredity and much more. It must be remembered that the female genitourinary system is very vulnerable, and any minor disturbances in the body can negatively affect it.
The main reasons for the development of hypoplasia of the upper layer of the uterus:
- Negative disturbances in a woman’s hormonal background. The most common cause of such changes may be the presence of insufficient amounts of the hormone estrogen. This condition causes the lining of the uterus to become thinner.
- Various infections in the genitals, which tend to be transmitted through intimate relationships. Pathogenic organisms not only negatively affect the condition of the endometrium, but can also significantly affect the development of epithelial cells, thereby causing hypoplasia.
- Chronic endometritis is a disease that affects the uterus, provoking inflammatory processes in it.
- Thinning of the endometrium as a result of impaired functioning of receptors dependent on the hormone estrogen.
- Processes of stagnation in the uterus, problems with blood circulation.
- Any kind of surgical intervention in the reproductive organs (curettage method, laparoscopy).
Important! Hypoplasia can be caused by surgery on the ovaries, as well as any other injury to the endometrium through surgical manipulation. A genetic predisposition to hypoplasia should not be ruled out.
Reasons for development
Endometrial hypoplasia can occur for various reasons, the most common are the following:
- Chronic inflammation of the genital organs;
- Complications after ovarian surgery;
- Insufficient development of the uterus and disruption of its blood supply;
- Damage to the endometrium during abortion and cleaning of the uterine cavity;
- Sexually transmitted infections;
- Hormonal imbalance;
- Use of contraceptives (after stopping the medication, over time the endometrium returns to normal);
- Dysfunction of the uterus as a result of damage to the hypothalamus or pituitary gland;
- Congenital developmental pathologies.
Doctors suggest that thinning of the endometrium may have a hereditary predisposition. There is also an opinion that unfavorable factors that affect the pregnant mother are the cause of hypoplasia in the daughter.
Treatment options
Before prescribing therapy, a number of studies are carried out.
- Blood test for hormones: progesterone, follicle-stimulating hormone, luteotropic hormone. The analysis is taken on days 20-22 of the cycle.
- Ultrasound examination of the uterus to measure the exact thickness of the endometrial layer. When hypoplasia is suspected, ultrasound is often performed dynamically, every 4-7 days throughout the cycle, to identify the time of failure and suggest the cause of its occurrence.
- Hysteroscopy of the uterus (examination of the uterus from the inside using a miniature camera).
- Histological examination of the uterine mucosa - endometrial biopsy.
Treatment of thin endometrium is prescribed depending on the cause of the disease. There are two possible directions that can be applied either separately, simultaneously or sequentially:
- drug treatment;
- surgery;
- physiotherapy.
Drug treatment is most often used in cases of disorder caused by a lack or imbalance of sex hormones. It consists of individual selection of hormonal agents. Depending on the results of the examinations, they are prescribed.
- Combined oral contraceptives - normalize hormone levels and gradually restore the proper functioning of the uterine mucosa.
- A course of estradiol injections (“Divigel”). This drug often allows you to quickly increase the required volume of tissue.
- Progesterone preparations (Utrozhestan or Duphaston) help the mucous membrane to “ripen,” which is a necessary condition for conception. This therapy helps and reduces the risk of miscarriage in the future, when hypoplasia is in the initial stages of development.
It is believed that the synthesized progesterone that Duphaston consists of has fewer side effects and is better absorbed, in contrast to the more natural Utrozhestan.
If hypoplasia is caused by chronic inflammatory processes in the pelvic area, the doctor will first treat infectious diseases. In this case, antibacterial drugs, immunomodulators, as well as suppositories that normalize the vaginal microflora can be prescribed in combination.
Surgical treatment consists of stimulating the growth of the mucosa through physical action:
- curettage of the uterine cavity (cleaning) followed by expansion of the endometrium using conservative hormonal therapy;
- stimulating endometrial growth using a hysteroscope is a fairly “young” method of treating hypoplasia, which, according to research, allows you to stimulate growth in the current cycle due to the gentle touch of the device to the walls of the uterus.
Physiotherapy for a diagnosis of hypoplasia is aimed mainly at improving blood supply in the pelvic area and uterus and is used as an auxiliary method:
- gynecological massage;
- laser therapy;
- diathermy;
- ozokerite therapy.
Additional treatments
Treatment of hypoplasia is also possible with the help of other non-traditional treatment methods:
- Electroreflexotherapy, which includes acupuncture and electropuncture. Acupuncture is a process that is based on the impact of special needles on the skin of a woman’s labia. Electropuncture is the effect of weak electric current on active points. Both procedures have an analgesic effect.
- Endonasal electrophoresis with thiamine. This is a constant effect on the body of a weak electric current, which is combined with the introduction of vitamin B1 (thiamine). The substance has a positive effect on the body, strengthening its immunity. Due to this, the healing process proceeds faster.
- Another method is the Shcherbak collar. It is performed lying on your stomach. Collar-shaped electrodes are placed on the lower back and shoulders. An electric current is then passed through them, which has a sedative effect. At first, the procedure lasts 6 minutes, and after every 2 sessions its duration is increased by 2 minutes. To achieve results, the course of treatment should include 25-30 procedures.
- Paraffin treatment is also widely used in gynecological practice. To do this, a warm substance in a liquid state is applied to the lower back or upper part of the pubis. Paraffin retains heat for a long time, so with this procedure the ovaries will warm up and gradually recover. The session lasts until the substance has completely cooled.
- If a diagnosis of stage 1 uterine hypoplasia is made, treatment is carried out using the ocokeritotherapy method. In this case, warm wax is applied to the lower back and upper groin area. The procedure is the same as with paraffin treatment.
- Electrical stimulation of endocervical receptors is also possible. In this case, a weak electric current acts on the receptors of the cervix. Due to this, the activity of the organ increases.
- During abdominal decompression, the lower body is exposed to reduced pressure air.
- UHF therapy is a method in which the body is exposed to a high-frequency electromagnetic field, which improves immunity. The body is also affected by an electromagnet during inductotherapy.
- With magnetic therapy, an alternating magnetic field with a low frequency is applied to the ovarian area, and with laser therapy, low-energy laser light is used.
- Gynecological massage is also used, in which the doctor acts on the labia with his fingers, performing massive movements.
- Balneotherapy is a treatment with mineral waters, which have a positive effect not only on the woman’s genitals, but also on the entire body as a whole.
- Sanatorium-resort treatment is a therapy that combines the effects of natural factors on the body (sun, air and water), as well as physiotherapeutic procedures.
Treatment with folk remedies
To eliminate endometrial hypoplasia, the following folk recipes are used.
- Clay compresses are a fairly common remedy. They are applied to the lower abdomen for about 2 hours.
- Peony extract (medicinal) can also help with hypoplasia. To do this, it must be diluted with water (proportion 1:2) and consumed 3 times a day, 2 ml. Its active components normalize hormonal levels and serve to prevent the progression of pathology.
- An infusion of plantain leaves to combat hypoplasia is taken 4 times a day. To prepare it, plantain leaves (50 g) are poured with boiling water (1 glass) and left in a container with a tight lid for at least 2 hours. Before taking, the solution must be filtered.
A comprehensive course of treatment , designed for 4 months, is also considered an effective remedy:
- During the first month, you need to drink fresh carrot and beet juice; the daily intake of each drink should be at least 100 ml per day. In addition, before each meal you should consume one tablespoon of flaxseed oil, washing it down with plenty of cold water. For greater effect, you can douche with celandine infusion. Infusion recipe: celandine herb (30 g) is poured with boiling water (3 liters) and infused for half an hour.
- In the second month of treatment, the main remedy is aloe tincture with the addition of honey and Cahors. Tincture recipe: aloe juice (400 ml), flower honey (400 g) and Cahors or other red wine (700 ml) must be thoroughly mixed and infused for 2 weeks. It is recommended to take this medicine daily. Treatment can be supplemented by taking an infusion of boron uterus herb and continuing douching.
- In the third month of treatment, it is necessary to continue taking infusions, but stop douching with celandine infusion.
- At the beginning of the fourth month of treatment, you should take a break for 1 week, eliminating all procedures. After this, you need to resume taking flaxseed oil and boron uterus infusion.
Endometrial hypoplasia is a dangerous disease that causes problems with conceiving and bearing a child. Therefore, its treatment must be approached with all seriousness and responsibility.
Possible complications of pregnancy with endometrial hypoplasia
When a woman’s endometrium is thinner than expected, this deviation has a significant impact on the possibility of conception, the process of pregnancy and birth. Malfunctions in the reproductive function of the female body can be expressed by the following manifestations:
- infertility;
- frequent miscarriages;
- ectopic pregnancy due to the fact that a woman’s fallopian tubes are elongated and tortuous;
- very strong toxicosis;
- during childbirth: sluggish labor, poor dilatation of the uterine cervix;
- heavy bleeding after childbirth.
Endometrial hypoplasia and pregnancy
Too thin endometrium negatively affects conception, the process of gestation and the birth of a child. A woman can become pregnant, but this is fraught with the following consequences:
- Early miscarriages.
- Severe toxicosis.
- Ectopic pregnancy.
- The most difficult birth.
During childbirth, labor becomes sluggish, the cervix dilates poorly, and heavy bleeding occurs after birth. Patients diagnosed with endometrial hypoplasia require special monitoring.
Before planning fertilization, it is advisable to cure endometrial pathology in order to avoid complications and negative consequences. With minor deviations, pregnancy and childbirth can proceed normally, but such cases are rare.
Diagnosis of hypoplasia of the uterine mucosa
The doctor can detect signs of endometrial hypoplasia already during a gynecological examination by a characteristic change in the shape of the external genitalia and cervix. Using ultrasound, the thickness of the endometrium is determined on different days of the menstrual cycle. A hysterosalpingography is performed - an x-ray of the body of the uterus and fallopian tubes. In this way, the condition of the endometrium, changes in its structure are determined, and the presence of adhesions and folds in the uterine cavity is determined.
A blood test is performed for sugar, pituitary and thyroid hormones, as well as for the content of estrogen and the hormone progesterone. A smear is taken from the vagina to determine the composition of the microflora. To establish the type of infectious agents, PCR and ELISA methods are used.
A uterine biopsy is performed.
If necessary, an MRI of the brain is done to detect signs of pituitary dysfunction and confirm the cause of hypoplasia.
Video: What is “thin endometrium”. How is diagnosis and treatment carried out?
Therapeutic methods
Treatment of endometrial hypoplasia directly depends on how thin this mucous membrane is. When carrying out drug therapy, a woman may be prescribed high dosages of drugs containing estrogen and low dosages of aspirin. In addition, physiotherapeutic procedures and folk remedies are often used. Methods that are aimed at increasing blood circulation in the pelvic organs, such as hirudotherapy and acupuncture, are also often used.
Most often, treatment for endometrial hypoplasia varies in duration, and therapy consists of selecting hormone-containing drugs. The selection of treatment agents is carried out by the doctor.
Physiotherapy also brings good results, especially if it is prescribed by an experienced doctor.
Treatment
Thin or functionally incompetent endometrium is always a consequence of some kind of disorder, so treatment of this pathology is primarily aimed at eliminating the factors that caused it. The intensity and duration of therapy directly depend on the degree of thinning of the uterine mucosa.
The main treatment usually consists of hormone replacement therapy, which is selected on a strictly individual basis. Therapeutic methods can also be used: physiotherapeutic procedures (ozokerite treatment, laser therapy, diathermy), unconventional methods (hirudotherapy, acupuncture, taking medicinal herbs).
How to diagnose
Hypoplasia can be suspected during a routine examination. The doctor notices insufficient pubic hair, changes in the shape of the cervix and external genitalia, and signs of immaturity. To confirm the diagnosis, additional examination is carried out, which includes:
- Ultrasound - allows you to determine the thickness of the functional layer and the degree of development of hypoplasia.
- X-ray examination.
- A blood test that determines hormone levels.
- Hysterosalpingoscopy.
- Biopsy of the uterus.
In some cases, the presence of pathology is determined by the presence of adhesions and folds in the uterus. To determine abnormalities in the functioning of the pituitary gland, an MRI of the brain is performed, a smear is taken for sexually transmitted infections, and a blood test is taken to determine glucose levels. After confirmation of hypoplasia, the doctor individually selects the treatment method.
Diagnostics
During a gynecological examination, patients with endometrial hypoplasia show signs of sexual immaturity: insufficient pubic hair, underdevelopment of the genital organs.
However, these symptoms are not enough to make an accurate diagnosis. Therefore, if a disease is suspected, additional examination is carried out:
- Ultrasound of the pelvic organs will determine the thickness of the endometrium and the degree of hypoplasia;
- Blood test to determine hormone levels (LH, testosterone, progesterone, prolactin, FSH, estradiol);
- Hysterosalpingoscopy, x-ray examination of the uterus;
- Biopsy, histological examination of the endometrium.
In some cases, uterine probing, determination of bone age, x-ray of the sella turcica, and MRI of the brain are used.