Modern methods and methods of treating pancreatitis and pancreas
Probably everyone fully understands the fact that if any effective method of treating a particular disease was found, guaranteeing recovery in 100% of cases, then doctors would not need to look for new and more effective methods in this direction.
However, unfortunately, the growth of the disease with pancreatitis is gaining such rapid momentum, and death is so common that doctors and scientists are forced to look for and try new ways to treat pancreatitis and prevent it. However, as practice shows, these researches are not in vain - for many patients who could not be helped by existing methods of combating inflammation of the pancreas, discoveries in the field of medicine have made their lives significantly easier. Modern methods of treating the pancreas combine not only the knowledge and experience of doctors, not only developments in the field of pharmacology, but also take into account the achievements of exact sciences, technology and electronics. For example, laser therapy. Its main area of application is the treatment of patients who have undergone surgery for acute pancreatitis. It is used immediately after surgery on the pancreas and is carried out in stages:
- Transcutaneous electrical neurostimulation of the necessary areas of the pancreas.
- Laser therapy itself: laser beam scanning of postoperative brine from a distance of about 1 cm.
The general course of laser therapy treatment is 15 days of daily exposure. The effectiveness of this method is that laser therapy has an anti-inflammatory, analgesic effect and accelerates scar healing after pancreatic surgery.
Remembering modern methods of treating pancreatitis, one cannot fail to mention the use of an alternating low-frequency magnetic field. Unlike the high-frequency method used previously, this one does not produce a thermal effect. As numerous studies have proven, magnetic techniques have an excellent anti-inflammatory effect, and in addition, relieve pain caused by pancreatitis, soothe the pancreas, and have a stimulating effect on the human immune system. Also, thanks to this method of combating pancreatitis, blood counts improve and microcirculation in tissues increases.
Another new method of treating the pancreas has been proposed by modern scientists. Strictly speaking, what is new is not the method itself, but its use in cases of pancreatitis. It consists of peloid therapy - exposure to therapeutic mud. As the practical application of this method has proven, it helps stimulate restoration processes and eliminates various disorders of the microcirculation of the pancreas. This method not only makes the fight against pancreatitis more effective, but also activates the body's defenses, and also helps in the treatment of concomitant diseases of the gastrointestinal tract.
Another modern way to combat the disease is musical electrotherapy. It affects not only the inflammatory process in the pancreatic gland, but also a wider range of problems associated with the stomach, liver, intestines, and biliary tract. Musical electrotherapy is based on the synchronous influence of an electrical impulse and listening to a piece of music. In this case, the patient chooses music according to his taste. The simplicity of this therapy makes it accessible to everyone.
How to take Phosphalugel for gastritis
Phosphalugel is an antacid often used in practice to treat gastritis with high acidity. Its effectiveness is explained by the fact that it reacts with hydrochloric acid in the stomach, neutralizing it, and therefore reducing the acidity of gastric juice. This promotes accelerated healing of the mucous membrane. To make recovery even faster, the drug envelops the affected area, preventing pathogenic microorganisms and poisons from entering it. It is important to know how to take Phosphalugel correctly for gastritis so that there are no side effects.
A doctor should prescribe the drug, since in some pathologies the drug can be harmful.
Typically, a course of treatment is used for chronic gastritis - how much you need to drink the drug depends on the severity of the pathology, so it is necessary to monitor the person’s condition. The average duration of taking Phosphalugel is up to 14 days.
Contraindications
There are not many contraindications to treatment with Phosphalugel. Among them:
- Alzheimer's disease;
- hypersensitivity to the active components of the formula;
- age up to six months;
- renal, liver failure.
If the dosage is chosen incorrectly, long-term use of Phosphalugel can cause kidney failure, disorders in the musculoskeletal system, distortion of the motor function of muscles and intestinal muscles. Sometimes constipation also develops, an allergic rash appears, nausea occurs, dry mouth occurs, and taste sensations are distorted. If such conditions occur, the drug is discontinued, replaced with another, and symptomatic treatment is carried out.
Similar drugs
Phosphalugel has many analogues. In terms of structure, the drug has no synonyms, but in terms of pharmacological action, many similar drugs can be selected. The most popular of them:
- Gastal;
- Aluminum and magnesium hydroxide;
- Almagel;
- Alumag;
- Maalukol;
- Inalan;
- Gaviscon;
- Almagel;
- Maalox;
- Enterosgel;
- Algeldrate and magnesium hydroxide;
- Rivolox;
- Prolanta;
- Gastracid;
- Altacid;
- Rennie;
- Anacid;
- Gaviscon forte;
- Palmagel;
- Almol;
- Mailax;
- Gestid;
- Ajiflux;
- Coalgel;
- Cherry namagel.
The main difference is in the forms of release and pricing policy. For example, Almagel and Almagel differ only in that one of them uses aluminophosphate as an active component, and the other uses aluminum hydroxide. The properties of the drugs are identical and, like Phosphalugel, they reduce the acidity of gastric juice and protect the mucous membrane. It is better not to take Almagel for a long time. The drugs taste sweet, so they are easy to give to children. Moreover, the products are suitable for diabetics, since they do not contain sugar. The choice of product depends on the preferences of the buyer.
Sometimes Maalox is used instead of Phosphalugel. It does not cause gas formation and fermentation in the intestines, as it absorbs carbon dioxide. Maalox gives a prolonged effect - it protects the mucous membrane longer and normalizes acidity for a longer period of time. The drug acts faster than Phosphalugel, but you can only drink it for a short period of time, as it washes out beneficial substances from the body. You should not drink it if you have hypovitaminosis or diseases of the central nervous system.
Phosphalugel is one of the most affordable, effective and efficient drugs for the treatment of gastritis with high acidity of gastric juice. The drug has few contraindications; even small children (5 years old) can take it. It is important to remember that an accurate calculation of the dosage is necessary - otherwise various side effects are possible.
New in the treatment of pancreatitis
New methods have emerged in the drug treatment of pancreatitis. Thus, relatively recently, experts have identified the beneficial effects of Mexidol on the outcome of the acute form of the disease. Tests were conducted on two groups of volunteers suffering from this disease. As a result, in the first group of patients who were administered Mexidol, only a few people required surgery, in contrast to the second group of volunteers, where the number of patients operated on was an order of magnitude larger.
In addition, intensive vitamin therapy, as well as special medications with a high concentration of enzymes, began to be used to treat the disease in its chronic course.
A modern method of invasive treatment is the elimination of non-functioning pancreatic tissue. In addition, nowadays specialists also perform resection of the gallbladder.
New in the invasive treatment of pancreatitis is gland transplantation, as well as β-cell transplantation. These cells produce insulin, which contributes to a favorable outcome of the disease. Currently, scientific research is being conducted in the field of using stem cells to get rid of severe forms of the disease.
Use of the drug in complex therapeutic measures
Pancreatitis requires an integrated and global approach, as a result of which all negative effects of the disease are eliminated. Phosphalugel is one of the components of this basic therapy. In addition to a strict diet, which must be present in the treatment of pancreatitis, the main methods of combating the disease include:
- use of antispasmodic medications;
- use of strong painkillers;
- prescribing protease inhibitors;
- carrying out a course of treatment with somatostatin;
- removing toxins from the body;
- use of antibiotics;
- therapy that temporarily blocks the action of enzymes produced by the pancreas;
- reducing the acidity of the environment to avoid damage to cells and tissues. It is the latter that the drug Phosphalugel does.
Important! You should not self-medicate, and if symptoms appear, take various medications. The complex that is suitable for a particular patient can only be selected by a specialist.
Modern methods of treating chronic pancreatitis
Chronic pancreatitis cannot be completely cured. The goals of therapy for this disease are to relieve symptoms, prevent complications and exacerbations, and improve the patient’s quality of life. Often the patient needs constant treatment, not only during an exacerbation, but also during remission. Sometimes chronic pancreatitis requires surgical treatment.
Treatment methods for chronic pancreatitis
All methods of treating chronic pancreatitis can be divided into conservative and surgical. Conservative ones, in turn, are divided into medicinal and non-medicinal. Surgical treatment involves open or minimally invasive endoscopic operations. During the period between exacerbations, the patient requires constant maintenance therapy.
Non-drug methods of treating chronic pancreatitis:
- diet
- lifestyle change
- compliance with the correct work and rest schedule
- Spa treatment
- physiotherapy
- non-traditional methods of treatment (acupuncture, herbs and other methods with unproven effectiveness)
The patient needs conservative treatment constantly, and not just during exacerbations. Typically the patient takes:
- enzyme preparations in case of pancreatic insufficiency
- antispasmodics or non-steroidal anti-inflammatory drugs if pain occurs
- if necessary, antisecretory drugs to reduce the functional activity of the pancreas
During an exacerbation, conservative treatment of chronic pancreatitis may include:
- painkillers
- synthetic somatostatin analogues to reduce pancreatic activity
- infusion solutions (for detoxification of the body)
- pancreatic enzyme blockers (aprotinin)
- antibiotics (to prevent infectious complications)
Endoscopic treatment of chronic pancreatitis
In recent years, endoscopic treatment methods, which are minimally invasive surgical interventions, have become increasingly effective. Penetration into the abdominal cavity is made in several places through small incisions. Such operations, compared to open surgical interventions, have many advantages:
- fewer complications
- short rehabilitation period and rapid restoration of working capacity
- less scarring
- reduced hospital stay time
Endoscopic methods for the treatment of chronic pancreatitis allow:
- remove stones from bile ducts
- remove strictures blocking the lumen of the pancreatic or bile ducts
- perform duct prosthetics
- perform puncture of a false cyst
- perform nerve excision to reduce pain
Endoscopic treatment is more effective for chronic pancreatitis caused by pathology of the biliary tract, compared with inflammation of the pancreas caused by alcohol abuse
Surgical treatment of chronic pancreatitis
Some patients with chronic pancreatitis require planned and sometimes forced surgical intervention. Indications for surgery for this disease:
- severe pain syndrome that is not relieved by medication
- formation of strictures in the bile or pancreatic ducts
- pancreatic abscess
- pancreatic cyst
- duodenal obstruction
- occlusion of the splenic vein
- bleeding
- pancreatic fistulas
- severe ascites (accumulation of fluid in the abdominal cavity)
Open surgery is always associated with a decrease in the amount of functioning pancreatic parenchyma. Therefore, the patient’s organ dysfunction progresses faster. After surgical treatment, the patient has a higher chance of developing diabetes mellitus due to chronic pancreatitis.
Replacement treatment of chronic pancreatitis
Patients with chronic pancreatitis sooner or later develop excretory pancreatic insufficiency. This means that the organ can no longer produce the amount of enzymes needed to break down food. Today, there are drugs that allow you to compensate for the function of the pancreas. Treatment of pancreatitis, which involves ingesting digestive enzymes, is called replacement.
Indications for the use of pancreatin (complex of pancreatic enzymes):
- 15 g of fat per day or more is excreted in feces
- progressive weight loss
- patient complaints of diarrhea, flatulence, nausea
In pharmacies you can find many medicines containing pancreatin. But they differ significantly from each other, so the drug must be selected by a doctor. The main differences are as follows:
- presence or absence of acid-resistant coating
- release form - tablets or capsules with microgranules
- presence of additional active ingredients (bile components, stomach enzymes)
- amount of lipase, amylase, proteolytic enzymes
- origin of pancreatin (most often it is made from organs of pigs or bovines)
Main properties of the drug
The drug belongs to a group of drugs called antacids. These substances are designed to lower the level of acidity within the human stomach. Phosphalugel itself is a gel-like substance with the active ingredient aluminum phosphate. The ingredients of the medication also include:
- water;
- orange flavor;
- sorbitol;
- agar-agar;
- potassium sulfate;
- potassium sorbate;
- pectin.
The unique composition of the drug combats the pH of the environment, and also helps to build a protective shell around the organ, or rather on its mucosa. In addition, the medicine has ingredients that easily come into contact with toxic formations. After this, they are quickly eliminated from the body.
Important! The medicine has no effect on metabolic processes with calcium and phosphorus.
Pancreatitis: modern methods of treatment
Treatment of patients with pancreatitis is carried out in accordance with the form of the disease and the severity of the patient's condition.
As a rule, treatment of acute pancreatitis is based on general principles, including suppression of secretion of the pancreas, stomach and duodenum, compensation of fluid lost by the body, elimination of water-electrolyte and metabolic disorders, reduction of enzyme activity, elimination of high pressure in the biliary and pancreatic tracts, improvement of rheological blood properties, prevention and treatment of functional insufficiency of the gastrointestinal tract, prevention and treatment of septic complications, maintaining the optimal amount of oxygen in the body, pain relief.
Treatment usually begins with transfusion of isotonic solutions and potassium chloride preparations with a reduced amount of potassium in the blood. If there is a shortage of circulating blood volume, colloidal solutions are used for infusion. To restore microcirculation and rheological properties of blood, dextran with pentoxifylline is prescribed.
Together with infusion therapy, measures are taken to suppress the functional activity of the pancreas. To do this, the patient is limited in food intake for the first five days. In addition, gastric contents can be aspirated through a nasogastric tube, followed by rinsing with cold water. In order to suppress the secretory activity of the pancreas and reduce acid production in the stomach, synthetic analogues of somatostatin are prescribed.
For the purpose of detoxification, extracorporeal cleansing methods are sometimes used: plasmapheresis, hemosorption, etc.
With the development of pancreatic necrosis, the prescription of antibacterial agents is required, which are selected by the doctor individually.
If the patient has severe pain, he is prescribed various painkillers.
In addition to conservative treatment, surgical treatment of pancreatitis is sometimes used. Currently, the main method of surgical treatment for sterile pancreatic necrosis is laparoscopy. Its main advantages are small incisions and quick recovery after surgery. If it is impossible to perform surgical intervention using a gentle laparoscopic method, a laparotomy (dissection of the abdominal wall) is performed.
Currently, as a rule, two main directions are used. One direction is the installation of drainages and peritoneal lavage dialysis. This allows toxic substances to be removed. Another direction is to remove the affected part of the pancreas (resection). In addition, for pancreatitis, Lawson's operation is sometimes performed, which consists of applying a gastrostomy and cholecystoma, draining the omental foramen and the pancreas area.
In general, the volume and form of surgical intervention are determined by the attending physician depending on the type of pancreatitis, the presence of complications and the patient’s condition.
Treatment of chronic pancreatitis during periods of severe exacerbation is carried out in the same way as for acute pancreatitis.
In case of chronic pancreatitis, meals should be fractional, in small portions. Alcohol, marinades, fried, fatty and spicy foods, and strong broths are excluded from the diet. The diet should contain an increased amount of protein, a reduced amount of fat and carbohydrates. With the development of diabetes mellitus, sugar is completely eliminated.
Pharmacological action of Phosphalugel
The drug has certain therapeutic properties.
Antacid property. This antacid is capable of binding hydrochloric acid contained in gastric juice and neutralizing it. This phenomenon is decisive in reducing the acidity in the stomach to normal.
After binding and neutralization, the action of the drug is aimed at maintaining normal acidity.
Enveloping property. Due to the aluminum content, which is capable of creating a special protective layer, a film effect occurs on the organ mucosa. It protects the mucous membrane from the unwanted effects of gastric juice, as well as from the influence of toxins that come with food. Creating a protective layer allows you to normalize intestinal motility.
Sorbing property. This effect of Phosphalugel is aimed at neutralizing pathogenic bacteria and toxins that enter the intestinal lumen. After neutralization, the drug removes them.
The medicinal substance allows for the eradication of all pathogenic microorganisms, from viruses to extremely dangerous bacteria, such as the causative agents of typhoid fever or salmonellosis.
What is pancreatitis
Inflammation of the pancreas is called pancreatitis. In this disease, the enzymes produced by the pancreas, instead of entering the duodenum, remain in the pancreas, gradually destroying it. Thus, toxins begin to enter the blood, negatively affecting the entire body.
There are two types of pancreatitis: acute and chronic. In the acute form, the disease occurs suddenly and is characterized by severe acute pain in the upper abdomen. Acute pancreatitis requires immediate hospitalization and adequate treatment in a hospital setting. Chronic pancreatitis usually develops as a result of untreated acute pancreatitis; pain in the upper abdomen is less pronounced than in the acute form of the disease and can radiate to the chest or lower back.
Reasons for the development of pancreatitis
The vast majority of cases of acute pancreatitis occur due to alcohol abuse or gallstone disease. In addition, the following factors may contribute to the development of pancreatitis:
- genetic predisposition;
- hormonal disorders;
- diseases of the duodenum, stomach, biliary tract, gall bladder;
- food and chemical poisoning;
- pancreas injuries;
- overeating, unhealthy diet with a predominance of fatty and fried foods;
- circulatory disorders in the pancreas, which occurs during pregnancy, vascular atherosclerosis, arterial hypertension, diabetes mellitus;
- use of certain medications, for example, glucocorticosteroids, metronidazole, estrogens, non-steroidal anti-inflammatory drugs, sulfonamides, tetracycline, etc.;
- infectious diseases such as mumps, chicken pox, hepatitis, etc.
Gordox: indications and recommended dosages
Antienzyme drugs for pancreatitis: a wide choice
The drug is a complete analogue of Kontrikal. The main active ingredient is aprotinin.
Indicated in the treatment of various forms of pancreatitis, including those caused by trauma and surgery.
To relieve a primary attack in adult patients, 0.5 million units of the drug are used. The antienzyme is administered by infusion.
When the patient's condition normalizes, the maintenance dose is 200 thousand units every 6 hours, but not less than 1 million per day. If general indicators improve, the dosage regimen is 0.5 million units per day.
Side effects during treatment with Gordox develop extremely rarely. Most often, hypersensitivity reactions occur, a decrease in blood pressure, and the appearance of dyspepsia are possible.
The drug is prohibited for use in the first 12 weeks of pregnancy. Further treatment is carried out according to vital indications and under the supervision of a doctor.
Important! The drug should not be taken during treatment with drugs containing dextran. This increases the risk of developing an allergic reaction.
The drug is not compatible with nutritional mixtures for parenteral nutrition or steroid hormones.
Symptoms of pancreatitis
Clinical manifestations of acute pancreatitis include the following:
- abdominal pain can be localized in different areas: in the epigastric region, in the right or left hypochondrium, it can also be of a girdling nature, radiating to the back, behind the sternum;
- nausea and vomiting;
- dry mouth;
- hiccups;
- pallor;
- increased sweating;
- elevated temperature;
- coating on the tongue;
- jaundice.
The following symptoms are characteristic of chronic pancreatitis:
- poor appetite;
- belching;
- nausea and vomiting;
- increased salivation;
- gas formation;
- diarrhea;
- weight loss;
- pain in the upper abdomen.
Diagnosis of pancreatitis
If pancreatitis is suspected, the doctor prescribes the following examinations:
- urine test - to detect amylase;
- general blood test - allows you to identify signs of the inflammatory process;
- biochemical blood test - carried out to determine the level of enzymes such as amylase, lipase and trypsin;
- gastroscopy allows you to determine the extent of the inflammatory process in the stomach and duodenum;
- Ultrasound examination makes it possible to detect changes in the pancreas;
- X-ray of the abdominal cavity allows you to determine pancreatic calcification, as well as the presence of intraductal stones;
- CT scan;
- cholecystocholangiography;
- coprogram.
Analogues of Enterosgel
It should be noted that today Enterosgel is number one among sorbents. It acts quickly, effectively, has few contraindications, and can be drunk by pregnant and nursing mothers, and even infants. The medicine itself has practically no contraindications (and those that are possible are not dangerous to human health).
However, for various reasons, this medicine may not be available at the right time. What can you take instead? Such drugs include:
- Activated charcoal (however, it can irritate the stomach lining) and white charcoal.
- Polyphepan (this product, along with toxins, also removes molecules of vitamins and nutrients).
- Smecta.
- Polysorb.
Smecta and Polysorb are considered the best analogues of the gel in terms of action and safety of use, but these drugs are not cheap.
Treatment of pancreatitis
Treatment should be selected individually, taking into account the form and causes of the disease, its stage, concomitant pathologies and other factors. In order to find out how to undergo treatment abroad at the Assuta clinic or other medical centers, contact Unimed for a consultation, where they will select specialists with a proven reputation for you.
Treatment of any type of pancreatitis involves following a diet, eliminating pain, correcting pancreatic insufficiency and preventing complications of the disease.
In acute pancreatitis, treatment involves a starvation diet, prescription of medications (painkillers, proteolytic enzyme inhibitors, albumin, etc.). In severe cases, surgery is indicated.
In the case of chronic pancreatitis, painkillers, vitamins, and enzyme replacement therapy are prescribed. Be sure to follow a diet. If indicated, treatment of diabetes mellitus, cholelithiasis, and endocrine disorders is necessary.
A diet for pancreatitis involves frequent meals in small portions, exclusion of alcohol, limitation of fats, carbohydrates, salt, coffee, and increased consumption of protein foods.
Side effects of taking the drug and contraindications
Despite the abundance of beneficial properties, Phosphalugel remains a medicine, which means it has side effects and can interact with other medications, so you should not use this drug for self-medication for more than 3-4 days.
The appearance of unusual or painful symptoms while taking the drug is a reason to consult a doctor
Important! If symptoms do not go away or your health worsens while taking an antacid, or if you have severe abdominal pain, you should immediately consult a doctor!
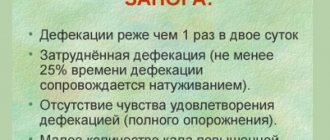
The most significant side effects of Phosphalugel include defecation disorders. Most often, patients note the development of constipation, this is especially true for the elderly and bedridden patients. To reduce the likelihood of stool retention, it is recommended to drink plenty of fluids (water, tea, compotes). In addition, due to the presence of sorbitol in Phosphalugel, it can also have a laxative effect, up to the development of diarrhea. In such cases, it is preferable to stop taking this medication.
People who have previously noted any allergic reactions to Phosphalugel or its individual components are strictly prohibited from taking this drug. If manifestations of intolerance to the drug (rash, itching, redness of the skin, anaphylactic shock, swelling of body parts) appear during treatment, then you should stop further use and see a doctor as soon as possible.
It is not recommended to take Phosphalugel if you have fructose intolerance, kidney failure, as well as patients with Alzheimer's disease and people suffering from chronic (habitual) constipation or chronic diarrhea.
Phosphalugel has no effect on the fetus, but it is not recommended to take it until late pregnancy
Important! Phosphalugel is allowed to be taken by pregnant women in later stages for a short time, but consultation with a doctor before using the drug is required.