Squamous metaplasia of the cervix is an adaptive reaction of the body, characterized by the replacement of a more vulnerable single-layer columnar epithelium with a more resistant multilayered squamous epithelium.
Single-layer cylindrical (also known as glandular) epithelium lines the cervical canal of the cervix, trachea, bronchi and stomach. The glandular epithelium also includes the inner lining of the uterus - the endometrium. This type of epithelium is quite delicate, located in one layer and is necessary for the secretion of mucus and other biologically active substances. Naturally, when the glandular epithelium is exposed to various irritating factors or when hormonal levels change, the body is able to rebuild and adapt to new conditions by replacing the type of epithelium.
Multilayered squamous epithelium is several times thicker than glandular epithelium and, accordingly, is more resistant to irritating factors. It covers the mucous membranes of the mouth, esophagus, vagina and outer part of the cervix, as well as the skin. Squamous metaplasia is a process when squamous epithelium appears in unusual places or when the epithelium is functionally displaced.
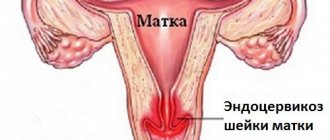
Squamous metaplasia of the cervix
The junction of columnar and stratified squamous epithelium
As mentioned above, the cervical canal is lined with glandular epithelium, and the outer part of the cervix is flat. The epithelial junction (pictured above) can migrate to varying distances within the cervix. This process is mainly controlled by hormones. Thus, in children, the epithelial junction is located near the external os, while in older women it is displaced deep into the cervical canal. In women of reproductive age with various hormonal disorders, pregnancy, inflammatory diseases of the pelvic organs, the glandular epithelium can move beyond the external pharynx and even reach the vaginal vault. Gynecologists call this cervical erosion or cervical ectopia. When hormonal levels are normalized, the glandular epithelium is again replaced by stratified squamous epithelium through squamous metaplasia (or epidermization).
Immature squamous metaplasia is the initial stage of metaplasia, characterized by the proliferation of germ (reserve) cells and their differentiation into squamous epithelium. Immature squamous epithelium contains little glycogen and is easily identified by cytological and histological examination. One of the key points in diagnosis is the determination of cellular atypia, which is a sign of tumor transformation. Excluding atypia is the main task of cytological examination. Reactive changes in metaplastic epithelium are often associated with pronounced inflammatory changes in the smear.
Mature squamous metaplasia is the final stage of metaplasia with the formation of a well-organized epithelial layer. Mature squamous epithelium contains a large amount of glycogen and a lot of cytoplasm. This option is the most favorable.
Both the integumentary glandular epithelium and the glandular epithelium undergo metaplasia. In this case, the excretory ducts of the glands can be blocked, which leads to the formation of retention cysts.
Squamous metaplasia does not require special treatment; it is enough to simply exclude provoking factors and undergo regular preventive examinations.
Squamous metaplasia in other organs
Squamous metaplasia is also observed in the lungs , namely in the bronchi of smokers, chronic bronchitis or bronchiectasis. With prolonged exposure to carcinogenic factors, metaplastic squamous epithelium can undergo malignant transformation with the development of squamous cell lung cancer. Squamous cell metaplasia of the bronchi is an unfavorable process, so eliminating provoking factors is the initial task in treatment.
Squamous metaplasia of the bladder is a common finding in chronic inflammation and appears as a white spot on the pink background of normal mucosa. In this case, a person may experience various disturbances in the functioning of the bladder, but the symptoms are nonspecific. Diagnosis is based on cytoscopy - examination of the bladder cavity using a special probe with a camera.
Squamous epithelial metaplasia can also be observed in cervical polyps and adenocarcinoma. These are accompanying changes and without treating the underlying pathology, the effect cannot be achieved.
Squamous cell metaplasia of the cervix can be diagnosed in women of different ages, but most often occurs in those who are on the threshold of menopause or already in the menopause phase. The disease under discussion is a condition that precedes cancer and, if not properly treated, can develop into a cancerous tumor. Essentially, during the metaplastic process, the glandular cells covering the cervix are transformed into others - a flat type.
What it is?
According to the International Classification of Diseases, this pathology is assigned code N87 . As already mentioned, the disease is usually diagnosed in women of premenopausal age. However, in 30% of cases, young women encounter this pathology. To better understand what processes occur in this case, it is necessary to delve into the anatomy.
The cervical epithelium has a heterogeneous structure. Near the vaginal canal, the cervix is covered with several layers of flat epithelium, closer to the uterus itself there is a gap - in the organ itself and the cervical canal the epithelium has a cylindrical structure and normally these layers do not overlap each other - a clear boundary can be traced.
When viruses or bacteria penetrate the cervix, the membranes of the nuclei are destroyed, the cells begin to divide rapidly, resulting in the appearance of cellular structures with an altered nucleus. In this case, protein synthesis is disrupted, and the processes of dysplasia begin. The boundaries between the epithelial layers disappear and tissue replacement occurs.
Reference! This environment is favorable for the emergence of oncogenic cells, which often appear in weakened tissues with reduced differentiation.
Unfortunately, metaplasia occurs in almost complete absence of symptoms; people often learn about the pathology when the malignant process starts. That is why gynecologists strongly advise women to regularly visit a gynecologist and, if necessary, undergo examinations. This is the only way to determine a precancerous condition at the beginning of development, avoiding complications.
https://youtu.be/Na9v2u8E_Vk
The main causes of squamous cell lung cancer
Reasons for development.
A malignant formation appears as a result of squamous metaplasia in the epithelial layer lining the bronchi. The main initiating factor leading to the pathogenic transformation of cellular structures is the action of harmful, especially toxic carcinogens.
The diagnosis of lung cancer of squamous cell etiology is mainly made to patients with long-term nicotine addiction. Also, one cannot ignore such a factor as passive smoking.
The composition of the inhaled air influences the appearance of dysplastic cells in the bronchi. That is, if the composition of the air passing through the bronchi contains harmful impurities (acids, nitrogen oxide, sulfur and others), changes may begin in the bronchi that predetermine the appearance of cancer in the future. The causes of squamous metaplasia include various pulmonary diseases: tuberculosis, bronchitis, various types of pneumonia, diseases of viral etiology.
To understand how harmful factors influence, it is necessary to consider the work of the bronchi. In addition to the passage of air, cleansing occurs in the bronchi by removing accumulated mucus.
Types of cervical metaplasia
To clarify the form of the pathology and prescribe the correct treatment regimen, it is necessary to take a smear and conduct a study of the exudate.
The following types are distinguished:
- Immature - cells with irregular boundaries and randomly located are detected. It is difficult to find out what type of epithelium they belong to, since there are no distinctive features yet. The cell cytoplasm has a disturbance in the structure of the structural cellular elements.
- Squamous - replacement of cells is observed, but they do not visually differ from those that should be in this area. However, they are located unusually. This type of metaplasia is characterized by the extension of the squamous epithelium beyond the border of the zone.
- Squamous with dyskaryosis - this species is quite easy to identify. This is already a mature form, and in this case, incorrect division of the nucleus is observed, as well as the formation of abnormal cells of a similar shape.
Causes of the disease
Before starting treatment, it is necessary to find out the reasons that gave impetus to the development of epithelial metaplasia. If you eliminate only the visible signs of metaplasia, you will not be able to cope with it, and after a while the woman will again face the problem.
Often the cause is neoplasms such as warts and genital warts, provoked by HPV . For a long time, the pathology may not manifest itself in any way, but when activated, it can cause the appearance of growths on the internal genital organs. Herpes is also a common cause of metaplasia - it causes inflammatory processes in epithelial tissue, which leads to cell replacement.
Bacteria , like viruses , act as the cause of the development of metaplasia. Bacterial agents invade the nuclei of epithelial cells and change them, which leads to dysplasia.
Important! If a woman is predisposed to the occurrence of pathology, she should be more attentive to the condition of her reproductive organs and visit the gynecologist’s office every six months.
Often, pathological disorders in the tissue of the cervix are caused by sluggish and untreated infectious diseases that provoke inflammation. Women at risk:
- having bad habits - smoking, alcohol abuse;
- frequently changing sexual partners;
- those who have undergone operations related to the treatment of the genital organs, abortions and curettage are also included here;
- having chronic pathologies;
- suffered miscarriages.
Prognosis and prevention
To prevent any gynecological disease, including squamous metaplasia, it is important to eliminate all possible provoking factors and adhere to the following points:
- maintain personal hygiene;
- exclude frequent changes of sexual partners;
- visit a gynecologist in a timely manner for annual preventive examinations;
- get rid of drinking alcohol and smoking;
- make your diet complete and balanced;
- minimize the impact of harmful environmental factors.
Squamous metaplasia is a benign pathological process that occurs in the cervix. However, the lack of diagnostic measures and timely therapy can aggravate the situation and cause the development of malignant neoplasms.
Squamous (squamous) metaplasia is a term used to describe cellular, noncancerous changes in the epithelial lining of certain internal organs, such as the bladder, cervix, and lungs. Metaplasia occurs when persistent stress or irritation causes a reversible process in which differentiated epithelial cells of one type are converted into epithelial cells of another type. In squamous metaplasia, various epithelial cells are replaced as a result of the adaptation mechanism of squamous epithelium.
Changes in cell type can lead to decreased epithelial function. When abnormal stimuli are removed, the metaplastic cells return to their original form and function. The persistence of physiological stressors in areas susceptible to metaplasia can lead to dysplasia or.
Dysplastic cells, in the absence of timely elimination of the stressor or irritant, can transform into cancer cells.
The epithelium is made up of layers of different epithelial cells such as columnar, cuboidal and squamous cells. Columnar epithelial cells are elongated, cylinder-shaped cells that form the lining of the cervical canal (endocervix), intestines and stomach. Columnar cells whose nuclei are at different heights are called pseudostratified epithelial cells. Cuboidal epithelium is formed from cells resembling squares. Such cells are commonly found in exocrine glands and renal tubules. Flat epithelial cells, in turn, form smooth epithelium.
The process of development of squamous metaplasia and the resulting neoplastic cell changes can be clearly seen using the example of cervical metaplasia. The mucosa of the cervical canal, which is a cavity in the cervix, is usually formed by columnar epithelial cells. Estrogen and chronic exposure to acidic pH levels in the vagina provoke the process of squamous metaplasia, affecting the epithelium of the cervical canal. In response to irritating pH levels, fragile columnar epithelial cells begin to be replaced by stronger squamous cells.
Squamous metaplasia of the cervical canal also occurs as a result of fusion with the adjacent ectocervix.
Squamous cells of the ectocervix begin to fill the endocervix area, replacing columnar epithelial cells. When carcinogenic factors such as the presence of human papillomavirus act as irritants or stressors on metaplastic epithelial cells, cervical cancer is formed. A similar metaplastic process occurs when cigarette smoke persistently irritates the pseudostratified epithelial cells of the lung mucosa.
Cigarette smoke is a stressor that converts pseudostratified cells into much tougher squamous cells. However, even squamous cells, such as those in the bladder, can undergo squamous metaplastic changes. The bladder trigone, or inner triangular region, includes the squamous epithelial cells that form the lining of this area. When adult squamous cells of the bladder undergo chronic inflammation, metaplastic change occurs in these cells.
Cervical metaplasia is a pathology of the glandular epithelium, in which the cells change to squamous cells. The phenomenon belongs to the group of precancerous diseases and requires treatment.
Symptoms
Since metaplasia of cervical cells always occurs in the absence of significant symptoms, women should pay attention to discomfort during sex. The dysplastic epithelium is injured, and therefore pain and even spotting appear at the time or immediately after intimacy. It must be said that such a symptom in women before menopause is not so pronounced, since a number of processes occur in the reproductive system at this time, and practically the changes are attributed to the approaching menopause.
Signs of metaplasia become more intense in the presence of a provoking factor:
- infectious lesions;
- erosion;
- condylomas;
- Abundant cheesy discharge with a sour odor may be observed.
Note! Moreover, metaplasia, without having its own clinical picture, is often disguised as other gynecological problems. In any case, any changes should make a woman wary, especially if she is premenopausal.
What diagnostic methods exist?
If tissue replacement in the cervix or atypical cell division is suspected, a woman may be prescribed the following laboratory and instrumental tests:
- Examination using gynecological speculum - the doctor assesses the condition of the cervical epithelium; obvious changes are visible to the naked eye.
- Biopsy with microscopic examination - a specialist evaluates the structure and structure of cells, their location relative to each other, and also identifies even minor disturbances in the process of cell division.
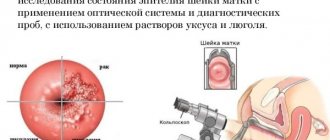
- Colposcopy - allows you to visualize the internal cavity of the cervix and evaluate its size, structure and shape.
- Curettage - this method is rarely used, if most of the cervix is affected.
- Ultrasound - ultrasound examination of the genitourinary area is necessary to exclude cysts, benign tumors and other pathologies. This method is often prescribed to young women as an alternative to curettage.
Treatment methods
Cervical metaplasia can be treated conservatively or using surgery . As a rule, doctors try to limit themselves to conservative methods, and only if positive dynamics are not observed, they prescribe surgical intervention.
Important! It should be immediately noted that treatment with folk methods in this case is ineffective; in trying to cope with the disease on her own, the woman misses precious time when metaplasia could be stopped with medications.
And that's the best case scenario. At worst, uncontrolled treatment with traditional methods can provoke complications and give impetus to the transformation of pathology into a malignant neoplasm. If we still talk about these methods, oils, extracts of medicinal plants, saline solutions and other recipes are used.
Operation
The operation is performed in the middle and advanced stages of epithelial metaplasia. In these cases, conservative treatment does not lead to a positive effect, and there is a risk of malignancy. Surgical treatment can be carried out in the following ways:
- Canal curettage - this method is used only when other methods are impossible. The method is traumatic.
- Cone excision - a conical section of tissue is excised; its volume depends on the depth of the lesion. In this case, it is possible to completely remove pathological tissue, but this is still a traumatic method compared to modern methods.
- Electrocoagulation - dysplastic cells are removed using electric current.
- Laser vaporization - under the influence of a laser beam, the modified cells are heated, resulting in their necrosis.
- Cryodestruction is cold destruction using liquid nitrogen. This intervention completely eliminates the presence of modified tissues and can be used for women who are planning to become pregnant.
- Cervical amputation is an organ-conserving operation during which part of the affected organ is removed. This is a radical method, it is indicated for extensive damage to the epithelium. After surgery, the cervix becomes shorter, which reduces a woman's chances of conceiving and carrying a child to term.
Your dermatologist
oncology
A precancerous disease (condition), or precancer, is considered to be congenital or acquired tissue changes that contribute to the occurrence of malignant neoplasms.
From a clinical point of view, obligate and facultative precancerous conditions are distinguished. For many tumors, such conditions are not defined, which creates certain difficulties in organizing preventive measures.
Obligate precancer , as a rule, is caused by genetic or congenital factors and sooner or later degenerates into cancer. Such diseases include familial colon polyposis, xeroderma pigmentosum, Bowen's dermatosis, adenomatous polyp of the stomach. Truly benign tumors generally do not become malignant.
Facultative precancer transforms into a malignant neoplasm relatively rarely. Facultative cancer is often not associated with hereditary and congenital tissue changes. The longer the facultative precancerous condition exists, the higher the likelihood of developing a malignant tumor, although most patients do not develop it during their lifetime. Facultative precancer includes dishormonal hyperplasia with proliferation of the epithelium of the mammary gland ducts, atrophic gastritis with deep restructuring of the mucous membrane, nonspecific ulcerative colitis, cervical erosion, cutaneous horn, keratoacanthoma, etc.
The concept of precancerous diseases has become widespread in both theoretical and practical oncology. They are the basis for the most important direction in oncology – the prevention of malignant neoplasms.
From the point of view of the pathomorphological approach, tissue areas with severe dysplasia are considered obligate precancer; all long-term tissue defects are considered optional. Precancerous diseases include a very wide range of conditions: nonspecific changes in tissues of inflammatory, dystrophic, dyshormonal nature, benign tumors, developmental defects, age-related changes, etc. The idea has become established that tumors do not arise without precancerous changes, i.e. cancer is always preceded precancer
In 1979, L. M. Shabad proposed the following formulation: precancer is microscopic multicentric multiple foci of non-inflammatory atypical growth of immature epithelium with a tendency to infiltrative growth, but without tissue destruction. He also identified 4 stages of blastomogenesis:
- uneven diffuse hyperplasia:
- focal proliferations;
- benign tumors;
- malignant tumors.
It is emphasized that one of these stages, more often the 3rd, may be absent (in such cases, focal proliferations are directly transformed into malignant tumors).
Nevertheless, along with the hypothesis about precancerous changes as an indispensable stage of the malignancy process, there is a point of view about the possibility of the occurrence of malignant neoplasms without a precancerous stage. This point of view cannot be categorically rejected, since cases of malignant tumors arising from morphologically unchanged tissues are well known. On the other hand, it is possible that the “absence” of a stage of malignancy may be associated with the rapid progression of the tumor and the lack of dynamic monitoring of the stages of carcinogenesis.
The desire to give more specific features to the pretumor period has led to the fact that dysplasia has become one of the most important morphological criteria, and now perhaps the main one.
It is obvious that it is impossible to equate the concepts “precancer” and “dysplasia”: the first is a broad biological concept, and the second reflects only morphological changes, which are often observed. On the other hand, tissue changes in the pretumor period cannot be reduced only to dysplasia.
All changes in cells and structures formed from them are associated with impaired differentiation of precursor cells. There are 3 main types of tissue differentiation disorders.
- Congenital malformations (congenital deformities, heterotopias, heteroplasias, hamartomas).
- Metaplasia is the replacement of one type of differentiated cellular elements by another due to chronic inflammation, endocrine effects and nutritional disorders. For example, the transitional epithelium of the bladder during chronic inflammation can turn into multilayered squamous or glandular prismatic; with prolonged vitamin A deficiency, squamous epithelial metaplasia of the respiratory tract epithelium develops; islands of stratified squamous keratinizing epithelium are found in the mammary, thyroid and prostate glands during chronic inflammatory processes and hormonal disorders. The phenomena of metaplasia are extremely diverse. They are possible not only in the epithelium, but also in connective tissue (for example, the appearance of bone and cartilage in post-traumatic scars).
- Dysplasia is characterized by the appearance of cells with the external characteristics of malignant neoplasms. Dysplastic changes often occur against the background of metaplasia. In a broad sense, the concept of “dysplasia” should include not only the entire spectrum of precancerous changes, but also invasive cancer.
However, in practice, dysplasia refers only to controlled and reversible disorders of epithelial differentiation of a precancerous nature as a result of the proliferation of cambial elements (undifferentiated precursor cells, stem cells) with the development of their atypia, loss of polarity and disruption of structure in the absence of invasion of the basement membrane. Dysplasia often develops in epithelial tissues and is manifested by disturbances not only of cellular composition, but also of architectonics. Cells lose their monomorphism, varying widely in size and shape. The nuclei become hyperchromic, too large in relation to the size of normal nuclei and cells. The number of mitoses increases, and they are found in unusual places in the epithelial lining. In dysplastic multilayered squamous epithelium, mitoses are detected at any level of the layer, including not only basal cells, as is normal, but also superficial sections.
Architectural disorders are characterized by changes in the normal structure of the epithelium, loss of polarity, and sometimes histotypic or organotypic characteristics. Dysplasia of multilayered squamous epithelium is manifested by the loss of vertical anisomorphism of the layer with subsequent replacement by basal-type cells instead of the progressive maturation of the basal elements towards the integumentary horny ones.
Thus, in multilayered squamous epithelium, dysplastic changes are manifested by focal proliferations with a violation of the vertical anisomorphy of the epithelial layer, basal cell hyperplasia, polymorphism, hyperchromia and enlargement of nuclei, an increase in the nuclear-cytoplasmic ratio, the phenomena of hyperkeratosis and parakeratosis, an increase in mitotic activity, occasionally with the appearance atypical mitoses. In this case, pathological elements to one degree or another replace the thickness of the epithelial layer.
Dysplasia of the glandular epithelium is characterized by disorganization of the structures of the glandular ducts, atypia and close arrangement of the glands with increased branching or, on the contrary, a flattened shape, budding; sometimes by papillary growths, pleomorphism, layering and hyperchromia of nuclei, changes in the tinctorial properties of the cytoplasm, often of the basophilic type, an increase in the nuclear-cytoplasmic coefficient, disruption of the polarity of cells and nuclei, multinucleation and changes in the functional activity of cellular elements - pathological keratinization, mucus formation, etc.
There are three degrees of dysplasia:
- weak (small);
- moderate (average);
- pronounced (severe);
- atypical epithelial hyperplasia.
From degree to degree, nuclear polymorphism and hyperchromia increases, cell proliferation increases, their life expectancy decreases, which leads to a rapid reduction in the cell population. At the same time, the polarity of epithelial cells and its histoarchitecture are disrupted. Many people tend to regard IV degree of dysplasia as non-invasive (intraepithelial) cancer. The likelihood of malignant transformation of regenerative, hyperplastic or metaplastic epithelium is quite low. The risk of malignancy increases with the appearance of dysplasia, with the greatest risk being the severe degree of dysplasia, when cellular disorders practically correspond to those of cancer. The high mitotic activity of cells in grade III dysplasia undoubtedly increases the likelihood of mutations and the appearance of cells with reactivation of genetic replication programs that are normally in a repressed state. In clinical oncology, severe dysplasia and cancer in situ are combined into the concept of “intraepithelial neoplasia” (cervical intraepithelial neoplasia, prostatic intraepithelial neoplasia, etc.), which is due to the same approach to the treatment of these groups of patients.
The term “cancer in situ” was proposed by Broders in 1932. This stage of tumor development is characterized by complete replacement of the epithelial layer with anaplastic elements, which in their cytological, light-optical, electron microscopic, biochemical and other characteristics are identical to tumor cells. The only reliable criterion distinguishing non-invasive cancer from invasive cancer is the visible preservation of the basement membrane. In addition, as a reflection of the changed parenchymal-stromal relationship, lymphoid-histiocytic infiltration occurs in the subepithelial base, which sharply decreases with the appearance of microinvasive growth and with the transition of the tumor to the stage of infiltrating carcinoma.
Despite the ongoing lively debate around the concept of “non-invasive (pre-invasive) cancer”, this term is gaining increasing recognition. The idea of squamous epithelial cancer in situ raises virtually no objections; the debate concerns mainly the signs of non-invasive cancer for the glandular epithelium. Clarification of these criteria allows for each localization of a malignant tumor to suggest the characteristics of the clinical course of cancer in situ of the breast, stomach, colon and rectum, endometrium, prostate, etc.
In general, the chain of sequential tissue changes during the process of blastomogenesis can be represented as follows:
- uneven diffuse hyperplasia
- focal proliferations, including regeneration and metaplasia,
- benign tumors
- dysplasia I degree
- dysplasia II degree
- dysplasia III degree
- non-invasive cancer
- invasive cancer.
Going through all stages of the formation of a malignant tumor is not necessary - any link can fall out.
Tumor development takes a long period. A malignant neoplasm can exist latently for several years, adysplastic changes - for decades. The progression of dysplastic changes does not necessarily lead to transformation into a tumor. Dysplasia may stop in its development or disappear completely. However, in a clinical setting there is no reason to expect normalization (regression) of a non-invasive cancer lesion.
Dysplastic changes, occurring equally in the unchanged mucosa, zones of hyperplasia and metaplasia or the focus of adenoma (papilloma), in cases of further development (dysplasia of the lll degree) with a high frequency evolve in the direction of cancer in situ and malignant tumors. In this regard, dysplasia of I and II degrees, as well as benign tumors without signs of severe dysplasia, should be classified as facultative precancer, and dysplasia of III degree - as obligate.
As for benign tumors, the assessment of the risk of their malignancy is characterized by wide variability depending on the tissue and organ affiliation. The likelihood of malignancy, for example, of tubular adenomas of the stomach or colon, is quite high, while the risk of malignancy of skin hydradenomas is practically zero.
At the same time, the detection of dysplastic changes in benign neoplasms should be considered by analogy with any other focus of dysplasia as an indicator of the risk of possible malignancy.
“Oncology” textbook, ed. V. I. Chissova, S. L. Daryalova 2007
| Search the site “Your dermatologist” |
Prognosis for recovery
Is this disease dangerous? Of course, squamous cell metaplasia of the cervix is a serious diagnosis that must be taken with full responsibility, but it is not a reason for panic. With timely diagnosis and proper therapy, the pathology is highly treatable and always results in a complete recovery for the patient.
As for the late visit to the doctor, if the malignant process has already started, the prognosis will no longer be so favorable. All women, especially those who are in the premenopausal period, should listen very carefully to their body, and at the slightest suspicion of pathology, immediately seek advice.
There is also a specific prevention of pathology - this is a vaccination against the human papillomavirus. It not only reduces the risk of metaplasia to zero, but also prevents the development of cancer in the cervix. But vaccination is only advisable for adolescents who have not yet become sexually active. Once the papilloma virus has already entered the body, it is no longer useful to vaccinate. Today, two vaccines are used that provide reliable protection against the papilloma virus for several years.
Important! Adult women who have tested negative for HPV can also be vaccinated. For such patients, the vaccine will also be effective.
Symptoms and causes of the disease
Before prescribing treatment, doctors must not only conduct a thorough diagnosis, but also establish the reasons that led to the pathological process. If you eliminate only the visible symptoms, the disease cannot be completely cured, and after some time, signs of metaplasia will appear again.
Among the most common provocateurs of the disease are genital warts and papillomas, which are caused by the human papillomavirus. The virus can lie dormant for a long time and, when activated, provoke growths on the internal organs of the woman’s reproductive system. If they are left unattended, they will soon degenerate into dysplasia and cancer. It should also be noted that the herpes virus can lead to inflammation of the cervical epithelium and its replacement.
Bacteria also play an important role in the appearance of metaplasia. Among them are:
- chlamydia;
- ureaplasma;
- gonococci;
- toxoplasma.
These bacteria penetrate the nuclei of epithelial cells and change their structure, causing dysplasia.
There is a certain risk group, which includes patients who:
- smoke;
- abuse alcohol;
- have chronic diseases of the genitourinary system;
- started having sex early;
- often change sexual partners;
- have undergone surgery on the genitals;
- had abortions;
- suffer from frequent miscarriages;
- have hormonal imbalances;
- were subjected to dramatization of the organs of the genitourinary system.
The pathology itself is not accompanied by any visible symptoms, but there are a number of signs that should alert a woman and cause her to see a doctor.
Some of these warning signs include:
- pain during sexual intercourse and bleeding;
- heavy bleeding during menstruation;
- menstrual irregularities;
- atypical vaginal discharge;
- rotten smell from the genitals;
- hormonal disorders;
- lower abdominal pain;
- general weakness and decreased performance;
- loss of appetite;
- sleep disorders;
- itching in the genital area;
- frequent urination and pain.
The first signs, as a rule, affect sexual intimacy - with active movements, the partner’s penis irritates the epithelial cells that are involved in the pathological process. There is discomfort during sexual intercourse, mild pain and blood.
Women during menopause need to be especially careful about their health. It must be said that a number of the above symptoms in women of climatic age can provoke natural changes in the body, and not bacteria and viral infections.
What do you need to remember?
- Metaplasia of the cervical region of the uterus is the process of transforming the glandular epithelium into flat, this is a precancerous condition;
- If the disease is not treated, it degenerates into cancer;
- There are three types of pathology: immature, squamous and with dyskaryosis.
- Most often, metaplasia occurs due to HPV;
- The disease is asymptomatic and is detected during a routine examination;
- The diagnosis can be made based on the results of a biopsy, colcoscopy, or ultrasound;
- Treatment can be conservative or surgical.
- The prognosis for timely initiation of therapy is favorable.
Used Books
- Diseases of the cervix, vagina and vulva / Ed. V.N. Prilepskaya. M.: Medpress, 2000. - 427 p.
- Diseases of the cervix: Clinical lectures. / Ed. V.N. Prilepskaya. M., 1997. - 460 p.
- Ivanova I.M. Colposcopic signs of pathological processes of the cervix associated with the human papillomavirus
- Kondratyeva E.A. Algorithm for diagnosis and management of patients with cervical pathology. // Gynecology. 2003. - T.5, No. 4. - pp. 166-170.
- Krasnopolsky V.I. Pathology of the vagina and cervix. / IN AND. Krasnopolsky / M.: Medicine, 1997.
Treatment of squamous metaplasia should be comprehensive
There are several classifications of cervical pathologies:
- histological,
- cytological,
- clinical and morphological,
- colposcopic.
There are three main groups of cervical diseases: background, precancerous and cancer.
Background or benign processes
– conditions in which there are no changes in the cells, i.e., the so-called normoplasia of the epithelium is preserved. Cells reproduce, grow, and differentiate correctly. These diseases include: cervical ectopia, ectropion, polyp, endometriosis, leukoplakia, papilloma, cervicitis, true erosion.
Ectopia of the cervix or ectopia of the columnar epithelium.
This is a special diagnosis and requires special emphasis. The condition of ectopia is detected in approximately half of gynecological patients. It represents a displacement of the boundaries of the epithelium, that is, the inner part of the cells seems to slide down. This is not a disease, but rather a violation of cellular boundaries. Usually the junction of the internal and external cells of the neck (transformation zone) is located in the inner part of the canal and is not visible. But if the border shifts to the vaginal part of the cervix, then this is visualized during examination.
Congenital uncomplicated form of ectopia
is not included in the nomenclature of pathologies, is not a disease and is a physiological condition. Just a few years ago, any red spot on the neck was called “erosion” and was mercilessly healed. That is why a huge number of Soviet and Russian women suffered from erosion, and this was the leading diagnosis! Today, the correct definition of displaced columnar epithelium is “ectopic columnar epithelium.” Physiological ectopia of the cervix is a normal variant in young women under 25 years of age; in older women it requires regular examination, cytological and colposcopic monitoring. The risk of developing cancer against the background of ectopia occurs when combined with another pathology - inflammation, leukoplakia, flat condylomas. The complicated form of ectopia is combined with inflammatory and precancerous processes and requires a careful approach to examination and treatment.
Ectropion
– eversion of the mucous membrane of the canal. It occurs after rupture and/or improper suturing of the cervix. This is a consequence of postpartum trauma or abortion. That is, acquired ectropion always has a traumatic origin; congenital is extremely rare and is usually combined with menstrual irregularities.
Cervical polyp
– growth of the mucous membrane of a round shape, with a smooth surface. When the polyp is located inside the cervical canal, there are no symptoms, but if it grows and protrudes from the cervical canal, it can manifest itself with bloody discharge outside menstruation and/or during sexual intercourse.
Cervical endometriosis
characterized by the appearance of foci of endometriosis on the cervix. Usually it is asymptomatic and is detected only upon examination in the form of red dots, the so-called “eyes”. Rarely manifests itself with bloody discharge or a feeling of discomfort. Cervical endometriosis occurs after surgical interventions using sharp instruments - endometrial cells penetrate into the puncture or incision site and take root there, as with any extragenital endometriosis. Cervical endometriosis, as a rule, does not pose any danger and requires routine monitoring and cytological examination.
Leukoplakia
– this is keratinization (thickening) of the surface layer of cells of the cervix. By the way, this is the oldest diagnosis and the name leukoplakia - “white plaque” - has not changed since 1887. Leukoplakia does not manifest itself in any way and is detected only during examination; colposcopy and Pap test confirm the diagnosis. If leukoplakia is simple, that is, it does not have any altered cells and is not combined with another pathology, it requires the usual screening examination method, and nothing more.
Cervical erosion.
We are talking about true erosion, that is, a defect in the mucosa with exposure of the underlying tissues (stroma). Synonym: cervical ulcer. A rather rare disease, detected in no more than 2% of women. True erosions are divided into trophic, traumatic, burn, cancer, syphilitic, tuberculosis.
Condylomas and papillomas - HPV (HPV)
– are called associated pathologies. They manifest themselves as epithelial growths, resulting from infection with the human papillomavirus. Genital condylomas (papillomas) are individual transparent papillae, have folds, outgrowths and villi. Flat condyloma looks like an irregular contour, slightly rising above the mucosa. These formations can be located both on the cervix and in the folds of the vagina, on the perineum and in the perianal area.
Processes are called precancerous
, in which changes occur in the structure and growth of cells with impaired differentiation. These processes include: CIN, leukoplakia with atypia, erythroplakia, adenomatosis. This is a group of pathological changes that occupy an intermediate position between normal cervical epithelium and cancer.
Attention! CIN – cervical intraepithelial neoplasia, synonym – cervical dysplasia.
Mechanism of disease development
Normally, a woman's cervix is lined with several types of cells. The vaginal part is in contact with an acidic environment and is represented by squamous epithelium. Inside, the cervical canal has an alkaline environment and is lined with columnar epithelium. The two types of cells have a clear boundary and in a healthy state do not overlap each other.
With squamous cell metaplasia of the cervix, a woman experiences a shift in the cell boundary. In the area of the cylindrical layer, reserve cells grow, which leads to the formation of a kind of growth. Subsequently, its surface is replaced. At this stage, the patient is diagnosed with immature metaplasia. Upon examination, the boundaries of the cells are clearly visible. Subsequently, tissue maturation occurs, and the surface of the pathological area takes the form of squamous epithelium. Characteristic signs of pathology may appear at the initial stage, and sometimes are absent at the final stage.
Varieties
With a detailed examination, the form of cervical metaplasia can be accurately determined. There are two of them in total:
- immature - a rather complex clinical case in which the degree of cell differentiation is low, but there is a high risk of the tissue acquiring the properties of a malignant tumor;
- squamous form - no changes are detected in the epithelium, however, its location and displacement towards the cervical canal indicate serious changes in the structure of the cervix
- metaplasia, combined with dyskaryosis, is the most mature form, in which cells acquire a certain shape and structure; the main difference between such epithelium and healthy epithelium is considered to be uncontrolled and unnatural division of nuclei.
Determining the form of pathology plays an important role in choosing further treatment tactics.
Combination with ectopia
In gynecological practice, a combination of ectopia and metaplasia is often encountered. This is a process of benign nature, which is characterized by the replacement of single-layer epithelial tissue lining the inside of the cervical canal with a multilayer one. This happens precisely due to squamous metaplasia.
Most often, the cause of this condition is dysfunction of the hormonal system, in particular excess production or supply of estrogen. Incorrect and uncontrolled use of oral contraceptives is also the cause of the development of metaplasia in combination with ectopia.
In the absence of proper treatment, the process of tissue replacement may worsen and severe inflammation of the tissues will begin, a decrease in local immunity and possible infection of the genital tract.
Symptoms
Obvious signs of changes in the epithelium may be absent for a long time. If a woman does not regularly visit a gynecologist for preventive examinations, she may find out about immature metaplasia quite late. Sometimes the pathology turns into cancer, and only its signs force a woman to seek medical help.
All girls, without exception, need to know about metaplasia, since this is a disease that can be asymptomatic. Patients may also have complaints about:
- painful sensations in the vagina during intimacy;
- periodic bleeding after sexual intercourse;
- bleeding not related to the cycle;
- menstruation disorders;
- increased volume of vaginal mucus;
- unpleasant odor coming from the genital tract;
- pulling sensations in the pelvis.
With human papillomavirus (HPV), women also find peculiar growths on the genitals. If the disease is accompanied by acute genital infections, the patient develops signs of intoxication.
Squamous metaplasia of the cervix often appears after age 50
Disease development process
Women over 50 years of age are susceptible to the development of pathology. With the onset of menopause, it is recommended to carefully monitor your health and not ignore visits to the gynecologist. The process of replacing single-layer cells of the endocervix with squamous epithelium develops over a long period of time, which makes it possible to identify and eliminate the pathology even before the appearance of the clinical picture.
A healthy cervix is lined with two forms of epithelial cells: squamous and columnar. They are separated by a zone of complete absence of epithelium. Unfavorable environmental factors provoke the emergence and development of squamous epithelium under the prismatic layer. Over time, the cells grow and begin to invade surrounding areas. Detection of such changes will confirm the diagnosis of metaplasia.
Factors provoking the process
Squamous metaplasia of the cervix develops against the background of general and local factors that negatively affect the body. The following have a negative impact on a woman:
- bad habits (smoking, alcohol);
- systematic disturbance of sleep and wakefulness;
- frequent colds;
- long-term depression;
- malnutrition (especially consumption of carcinogenic foods).
All this has an extremely adverse effect on the immune response, provoking changes in the structure of cells and tissues, facilitating the introduction of viruses and bacteria, as well as the colonization of tissues by atypical cells.
Bacteria and viruses, microtraumas during abortions and gynecological manipulations, and promiscuous sex life with frequent changes of partners have a local effect on the reproductive system.
Important!
The development of metaplastic cells occurs under the influence of herpes or bacterial infections (chlamydia, toxoplasmosis, ureaplasmosis), occurring against a background of weakened immunity and having a chronic form.
Diagnostics
Before choosing a treatment method, it is necessary to determine the extent and causes of changes in the tissues of the cervix.
When examined in mirrors, the gynecologist is able to see changes in the cell boundaries. However, a diagnosis cannot be made based solely on the results of a visual examination. A similar picture may occur with other diseases. Dysplasia and even cervical cancer are also characterized by changes in the boundary between the vaginal and inner surfaces of the cervix and the formation of growths.
To clarify the diagnosis, a woman is prescribed:
- cytological examination - using a sterile brush, the gynecologist takes some of the cells from the cervix and sends it for examination under a microscope;
- colposcopy is a hardware manipulation during which cervical tissue is examined under a microscope, processed with special reagents and, if necessary, sent for detailed study.
The results obtained in combination make it possible to accurately determine that a woman has metaplasia.
Diagnosis and clarification of diagnosis
Squamous metaplasia is not difficult to detect on the mucous membrane of the cervix. During a gynecological examination using a speculum, the doctor is able to determine that the epithelium has an unnatural structure, and its boundaries are broken or displaced.
Nothing more can be learned about the pathology during examination. To clarify the diagnosis, it is necessary to conduct an examination, which includes the following list of manipulations:
Colposcopy.
The mucous membrane of the cervix is studied under multiple magnification and treated with chemical compounds that allow the reaction to determine areas of increased risk of malignancy.
Biopsy.
A portion of the epithelium is collected and histologically studied, which provides accurate data on the nature and stage of the pathology.
Cytological examination.
Biomaterial is taken from several areas of the cervical mucosa, which makes it possible to determine the pathological process.
Bacteriological research.
Detects the presence of pathogenic microorganisms in a smear.
Complex diagnostics allows you to find out as much information as possible about the type of disease and differentiate it from others that have similar clinical manifestations: leukoplakia, cervicitis, polyps and the like.
The clinical picture of metaplasia is characterized by the appearance of colored discharge, breakthrough bleeding and pain during mechanical action on the cervical mucosa.
Treatment methods
Various methods are used in the treatment of cervical pathologies. If the disorder is caused by HPV, it is important to determine its type and assess the risks of cancer. This will allow predictions to be made regarding the chosen therapy. If there is a high risk of malignancy, it is recommended to immediately switch to radical methods and postpone taking medications until the postoperative period.
To suppress the activity of the virus, antiviral agents and immunomodulators are prescribed. They are used in the form of vaginal suppositories, tablets and injections. If, as a result of diagnostics, pathogens of latent infections were identified, antibacterial therapy is required.
Surgery for immature metaplasia is often used. This technique is advantageous because it allows you to get rid of pathological cells immediately and significantly reduces the risk of cancer. The operation can be performed in various ways. The appropriate method is selected by the doctor after assessing the patient’s condition:
- curettage of the cervical canal - involves clearing off pathological cells;
- excision - a technique for removing the epithelium of the cervical canal in the shape of a cone;
- laser treatment – involves the evaporation of pathological cells;
- electrocoagulation is a technique for cauterizing cells, after which a scar remains on the mucous membrane of the cervix.
The duration of the recovery period depends on the correction method. In the first days, a woman may have bloody vaginal discharge. Subsequently, they become ichorous and gradually take on a natural appearance. During the recovery period, it is not recommended to have sex, undergo thermal procedures and swim in public waters. After removal, the pathological area is sent for detailed analysis. Histology results allow us to determine the identity of the cells.
Forecast
If metaplasia is detected early, the prognosis is favorable. If the problem is identified at the initial stage, then complex treatment allows you to completely get rid of metaplasia. In the future, it is necessary to regularly visit the doctor, since the risk of relapse is quite high.
If the disease is detected in an advanced stage or atypical cells have already formed on the cervix, surgical intervention cannot be avoided. The prognosis in this case is less favorable, but adequate treatment and strict adherence to medical recommendations give good results.
How to recognize metaplasia
Cervical metaplasia develops asymptomatically for a long period, which allows the process to spread. However, tissue replacement can be easily diagnosed during a routine gynecological examination.
The clinical picture always shows metaplasia in combination with concomitant pathologies (papillomas, infections, erosions). Signs indicating a disorder of the cervix:
- failure of the menstrual cycle is one of the signs of dysfunction of the reproductive system; delayed menstruation, heavy or scanty discharge are a cause for alarm and contact an antenatal clinic;
- painful sexual intercourse (bloody discharge at the end of intimacy);
- vaginal discharge (of varying intensity and character: cheesy, milky, bloody, with or without odor);
- disruptions in hormonal regulation.
Important!
Given the absence of a specific picture of the lesion, any deviation from the norm in the functioning of the organs of the reproductive system should be a reason to visit a doctor. It is quite easy to ignore these symptoms, but such neglect can lead to an unfavorable outcome in the case of an advanced stage of metaplasia or a complicated course.
Diagnostics
Cervical metaplasia is diagnosed during a gynecological examination of a woman. If cancerous degeneration of the altered cells is suspected, biomaterial is taken, followed by histological examination.
Conclusion
The reproductive organs of the female body have a special anatomical structure, in which many diseases can be asymptomatic. The patient cannot independently detect changes in the tissue of the cervix, but a gynecologist can easily do this during a routine examination. The main prevention of metaplasia and its complications is regular examinations by a gynecologist. It is important for women during menopause and after menopause to remember that their risk of changes increases. It is recommended to visit a doctor at this age at least once every six months.