When can IVF be done after hysteroscopy?
Only a doctor can decide how many weeks or months later IVF can begin after examining the uterus, based on the diagnostic results obtained.
If the specialist has not identified any pathologies, and the condition of the endometrium is normal, IVF after hysteroscopy is prescribed 10 days later. When various pathologies were identified in the patient during the procedure, the moment of its introduction into the IVF protocol is shifted by 5–6 months. For example, a woman may need a course of anti-inflammatory therapy or hormonal drugs with subsequent monitoring of the condition of the uterus, which will take six months or more. When polyps, fibroids and other neoplasms are removed, artificial insemination can be carried out after at least 3 months.
After diagnosis, the uterine mucosa is restored in 2–3 weeks. During this period, microtraumas of the endometrium and cervical canal heal; to prevent infection, the woman must take prescribed antibiotics. Within 3 days after the procedure, spotting and spotting may be observed on the underwear.
- carry out genital hygiene 2 times a day;
- measure body temperature twice a day;
- exclude swimming in ponds or hot baths (you can only take a shower);
- monitor the intensity of discharge.
For 2 weeks, the patient should abstain from sexual intercourse, douching and physical activity. Pain should not bother you for more than 4-5 days. If you have suspicious discharge, vaginal itching or other symptoms, you should visit a doctor.
After diagnostic hysteroscopy, if no pathologies are identified, IVF can be done within 15-30 days, that is, in the next menstrual cycle. If pathologies are identified, it takes time to carry out preliminary treatment if doctors consider it appropriate.
After hysteroscopy with biopsy, IVF can be prescribed after about 2-3 months, and after the procedure with curettage, IVF is planned no earlier than six months later. In each specific case, the doctor prescribes the timing of the in vitro fertilization protocol after hysteroscopy, taking into account individual risks and examination results.
Hysteroscopy and IVF
Hysteroscopy and IVF after this manipulation are discussed on infertility forums. Women are interested in how it can help, and when can IVF be done after hysteroscopy?
A detailed study of the uterine cavity will help identify small adhesions and polyps that are not visible on ultrasound, but can cause IVF failure. There are many reviews on the Internet where, after unsuccessful attempts, they did a hysteroscopy and found minor changes. And after they were eliminated, women became pregnant after the first protocol. Therefore, this procedure before IVF significantly increases the chances of getting pregnant.
Moreover, if a woman has already had a hysteroscopy, this does not mean that repeated manipulation is pointless. If two years ago, during the study, synechiae were dissected or a polyp was removed, this does not mean that they could not arise again. Therefore, with two or three unsuccessful IVF, reproductive specialists advise repeating the procedure.
When to do IVF after hysteroscopy, the doctor decides. It depends on the result obtained from the study. If during the study no pathologies were found, or only an endometrial biopsy was done, then the protocol can be entered into in the next cycle, although reproductive specialists advise waiting for the endometrium to fully recover, because stress after the intervention affects hormonal levels, which can adversely affect affect during in vitro fertilization.
Pregnancy after a diagnostic procedure
Often, hysteroscopy before IVF or in the process of searching for the causes of infertility is performed not for therapeutic purposes, but for diagnostic purposes. As a result of examining the uterus, it often turns out that no medical procedures are required. After all, it is not at all necessary that the doctor will find polyps, synechiae or fibroids inside the uterus.
Modern hysteroscopes are very small in size. A tube of minimal diameter is inserted into the uterus without dilating the cervical canal. The procedure for examining the uterine cavity is completely non-traumatic. It does not require restoration. Therefore, IVF after hysteroscopy can be done immediately. There is no need for a rehabilitation period.
If hysteroscopy before IVF reveals any problems that limit the possibility of artificial insemination, treatment may be required. Sometimes it is conservative, in other cases it is surgical. In such a situation, the duration of rehabilitation depends on the severity of the disease and the chosen treatment method. It happens that a doctor prohibits a woman from becoming pregnant for several months after hysteroscopy due to the increased risk of spontaneous abortion.
Does hysteroscopy reduce the effectiveness of IVF?
Hysteroscopy does not reduce, but increases the effectiveness of IVF. Actually, this is why the procedure is carried out. It is performed precisely in order to remove obstacles to achieving pregnancy.
During the manipulation, the doctor can excise polyps, destroy synechiae, or perform other actions that will lead to the formation of an anatomically correct uterine cavity and improve the condition of the endometrium. The operation can be traumatic. In this case, pregnancy is impossible until the endometrium is fully restored. This is unlikely to take more than 2-3 months. IVF is then carried out, which has a much higher chance of success.
It is intrauterine pathological processes that often become the reason that pregnancy does not occur even when high-quality embryos are transferred. After all, IVF affects many stages of reproductive function (ovum maturation, fertilization, embryo growth up to 3-5 days), but doctors still have little control over implantation processes. Therefore, without timely treatment of uterine diseases, including the hysteroscopic method, pregnancy is often impossible, or the likelihood of its occurrence is much lower.
Thus, hysteroscopy is an effective method of treating infertility. This operation usually does not have any negative health consequences. In capable hands, hysteroscopy helps a woman achieve the desired pregnancy.
If the examination is not scheduled
As already mentioned, not all women undergoing IVF are recommended by their doctor to undergo hysteroscopy. The modern approach of the World Health Organization to this issue is somewhat different - this organization strongly recommends hysteroscopy for everyone who goes for IVF. Firstly, this will improve the protocol, since the fertility specialist will have more initial information. Secondly, it will save patients time and money. After an unsuccessful attempt, a hysteroscopy will still have to be done, and it is better to do it before the first attempt to increase the chances of pregnancy.
If your doctor has not prescribed hysteroscopy, you can contact him with this question and ask him to add the examination to the appointment before IVF. This is a woman's right.
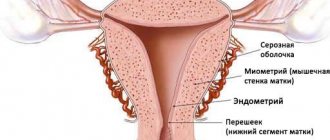
What is hysteroscopy
Hysteroscopy is a minimally invasive method of visual examination of the cervix and uterine cavity, which is performed using a hysteroscope - a special optical system.
Endoscopic examination before IVF is absolutely safe: it does not harm the woman’s health and does not interfere with pregnancy. The uniqueness of the method is that it allows you to simultaneously solve several issues regarding the prevention and detection of disorders of the patient’s gynecological health.
The method is used by specialists for the following purposes:
- Diagnostic (office): a qualitative examination of the uterus is performed.
- Surgical: they disrupt the integrity of the endometrium as a therapeutic measure.
- Control: evaluate the effect of the therapy.
IVF is an expensive undertaking. If a married couple has not received a quota or does not qualify for compulsory medical insurance, it is desirable that the attempt to transfer the embryo into the uterine cavity be successful. That is why doctors are trying their best to increase the chances of a favorable outcome of in vitro fertilization.
Hysteroscopy shows the doctor gynecological disorders or pathologies (adhesions, synechiae, polyps, bleeding) that may interfere with pregnancy or pregnancy, and at the same time treats them.
How is it carried out?
Hysteroscopy is performed using special equipment - a hysteroscope, which is a very thin and elegant probe with a built-in optical system. At the end of the probe there is a tiny video camera, which will broadcast the image to the monitor. The probe is inserted into the uterine cavity through the cervical canal.
For diagnostic purposes, hysteroscopy is performed with the thinnest probes, the diameter of which does not exceed 7 mm. This procedure is virtually painless for the patient and in most cases does not require anesthesia. The examination, although not the most pleasant, is not painful and not lengthy. The cervix is not dilated during this procedure; if a woman has increased sensitivity, she can be given pain relief.
Hysteroscope probes that are wider in diameter are used in operative hysteroscopy, when it is necessary not only to conduct a visual examination of the endometrium and uterine walls, but also to take tissue samples for analysis by biopsy.
Sometimes it becomes necessary not only to do a biopsy, but also to perform hysteroscopy with curettage, in order not only to assess the condition, but also to remove some nodes, adhesions, and neoplasms.
Before hysteroscopy, a woman must undergo all tests prescribed by the doctor. Typically, general blood and urine tests, a biochemical blood test, and a vaginal smear for microflora and infections are prescribed. If the laboratory diagnostic results are positive, the woman is sent for an ultrasound of the pelvic organs. And only then can she undergo hysteroscopy of the uterus.
Before IVF, hysteroscopy is prescribed between the 6th and 10th day of the menstrual cycle, the report is kept from the first day of the last menstruation. There is no need to go to the hospital for examination. If hysteroscopy is performed only as a diagnosis and is not accompanied by a biopsy or curettage, then the woman will stay in the clinic for no more than three hours. The procedure itself takes about 10-15 minutes.
After curettage, the hospital stay can last up to a day or a little more if any complications develop. The procedure in this case can last up to an hour. By the way, the likelihood of complications after the procedure is not so high - no more than 1%.
Before hysteroscopy, a woman is advised to refrain from eating for 12 hours. On the day of the procedure, you should do an enema, empty your bowels, and empty your bladder half an hour before the procedure. Taking aspirin and any drugs based on acetylsalicylic acid is prohibited at least a week before hysteroscopy to avoid bleeding.
Indications for endometrial hysteroscopy
Today, endometrial hysteroscopy, along with other diagnostic procedures, is included in the list of mandatory procedures for the diagnosis and treatment of infertility. It is especially important at the preparatory stage before various options for in vitro fertilization (IVF). Experts explain this by the fact that a visual examination of the uterine cavity, as well as an assessment of the structure and thickness of the endometrium, makes it possible to diagnose (and often immediately eliminate) pathologies that reduce the likelihood of successful embryo implantation during IVF.
For example, if during the procedure a specialist discovers polyps or adhesions or neoplasms, he can immediately remove them, saving the woman from repeated surgery. In addition, if abnormalities in the structure of the endometrium are detected, the gynecologist can take a tissue sample for histological examination and determine the cause of the changes.
What pathologies can be detected during hysteroscopy?
A minimally invasive diagnostic method allows you to detect:
- adenomyosis;
- areas of narrowing of the cervical canal;
- synechiae inside the uterus;
- endometrial hyperplasia;
- mucosal polyps;
- erosion;
- submucosal nodes;
- congenital pathologies of the reproductive organs;
- endometriosis in chronic form.
While assessing the condition of the uterus, a specialist may perform a minor operation: remove a benign neoplasm, adhesions, or septum that prevent the embryo from attaching, or cauterize the erosion. Often, women suffering from infertility are diagnosed with several diseases at the same time. The main advantage of the method is its information content - for example, ultrasound cannot show minor pathologies of the uterus.
Why is examination carried out before IVF?
If a married couple has already had an unsuccessful attempt at in vitro fertilization, hysteroscopy with separate diagnostic curettage (RDC) is mandatory. The specialist prescribes an endoscopic examination before in vitro fertilization and performs certain manipulations.
These include:
- assessment of patency of the cervical canal;
- determination of the condition of the internal mucous membrane;
- possibility of cauterization of erosions;
- cervical biopsy;
- carrying out dissection of septa or adhesions inside the uterus;
- removal of polyps.
Why is the procedure necessary before IVF? It allows you to select the necessary in vitro fertilization protocol scheme and treatment tactics for the doctor. This method replaces several diagnostic procedures for the patient - ultrasound, which sometimes cannot detect minor pathological changes in the uterus, and curettage in a hospital setting.
The study allows the doctor to detect the following disorders in the patient:
- congenital anomalies of the uterus;
- submucosal nodes;
- synechia;
- hyperplasia or atrophic processes in the endometrium;
- polyps;
- adenomyosis;
- foreign objects.
Quite often, women suffering from infertility have several types of disorders in the reproductive system. With the help of hysteroscopy, specialists can prepare the body for IVF as fully as possible, curing diseases.
On what day of the cycle should the study be performed?
Hysteroscopy before IVF must be performed on a certain day of the cycle - this will ensure maximum information content of the procedure. On what day the specialist will prescribe it will depend on the pathology he expects:
- Usually the procedure is carried out on days 5–10 of the cycle. At this time, the walls of the uterus are very thin, which allows for good visualization of defects: polyps, adhesions, fibroids, etc. If there are growths, they are removed - during this period of the cycle, blood loss will be minimal.
- On days 15–18 of the cycle, a specialist may recommend undergoing hysteroscopy to study the structure and functionality of the endometrial layer.
- The procedure is done extremely rarely 3–5 days before menstruation and is not performed during menstruation.
Methodology
Often, hysteroscopy before IVF is performed after the patient has been put under anesthesia. If there are contraindications to general anesthesia, epidural anesthesia may be used. The duration of the manipulation depends on the degree of complexity of the intervention that needs to be carried out. The examination will take minimal time, during which it will not be necessary to remove formations or solve other problems.
The patient is in a gynecological chair during the operation. The doctor uses a flexible hysteroscope, the optical system of which allows the image to be displayed on a monitor screen. Modern technologies allow video recording of the procedure.
As a rule, hysteroscopy before IVF is necessarily done from 6 to 10 days of the cycle. Most often, women do not experience severe discomfort during the procedure. Unpleasant sensations may occur that do not affect the operation.
Hysteroscopy is performed on certain days of the menstrual cycle
Sometimes there is a need to additionally decide on which day of the menstrual cycle to do the study. In the first half of the cycle, you can see defects and damage to the uterine mucosa because the endometrial layer is thinned. In addition, blood loss when removing tumors during this period is minimal. The functional state of the endometrium is examined in the second half of the cycle. Hysteroscopy is not performed directly during menstrual periods.
Indications
Hysteroscopy is a great help for fertility doctors. We can safely say that it increases the chances of successful IVF, since it allows the doctor to know all the “weak” points of the female body. An examination is not always prescribed, but only for certain indications, including:
- infertility caused by recurrent miscarriage (a history of several miscarriages or missed pregnancies);
- infertility caused by endometriosis;
- infertility due to a history of several abortions;
- if the doctor suspects polyps, adhesions, damage to the mucous membranes after operations;
- infertility due to uterine fibroids;
- idiopathic infertility, the cause of which has not been established;
- infertility associated with irregularities in the regular menstrual cycle.
Hysteroscopy is mandatory after several unsuccessful IVF attempts. The effectiveness of hysteroscopy is considered very high; the examination is classified as highly accurate.
Immunohistochemistry
Immunohistochemistry is a study that allows you to identify malignant neoplasms. Today, pipel biopsy with immunohistochemistry is considered one of the most modern methods of taking a sample of endometrial tissue. Such histoanalysis allows us to evaluate the rate at which tumor cells grow, the possibility of hormonal treatment and the response to chemotherapy.
Histoanalysis is an opportunity to quickly detect the presence of cancer cells. The results of histology after hysteroscopy directly depend on how well the biological material was taken and on the qualifications of the doctor conducting this study.
Histology after hysteroscopy can be re-assigned after some time. In some cases, hysteroscopy with RDV is prescribed before IVF. RDV is a separate diagnostic curettage. It is used to remove various tumors.
On what day of the cycle is RDV done? If a woman has uterine bleeding, the examination is carried out immediately after the start of menstruation. For menstrual dysfunction - on days 5-10. In the absence of ovulation - on the 2-3rd day of menstruation. If a tumor is suspected, the procedure is performed on any day of the menstrual cycle.
Contraindications
They try not to perform hysteroscopy if a woman has malignant tumors in the uterine area or severe stenosis of the cervical canal.
The diagnostic procedure is not carried out for women who were ill at the time of the examination with the flu, acute respiratory viral infection or any other disease - time is required to recover, after which the temporary ban will be lifted and the woman will be able to undergo the examination.
Some vascular and heart diseases, as well as uterine bleeding at the time of hysteroscopy, are considered a contraindication to the procedure. A relative contraindication is the absence of a history of pregnancy or childbirth.
Before the procedure, the doctor must analyze the patient's medical history, since sometimes hysteroscopy cannot be performed. Contraindications:
- general serious condition of the woman;
- uterine bleeding of any etiology;
- infectious diseases;
- poor blood clotting;
- cancerous tumors on the cervix;
- inflammation in the genitals;
- cervical stenosis.
Complications after manipulation rarely occur, since it is low-traumatic, and the technology for its implementation is well-honed by specialists. Possible adverse reactions:
- cramping abdominal pain;
- flatulence due to anesthesia;
- injury to the uterus;
- allergic reaction to drugs used for anesthesia;
- inflammation of the internal genital organs;
- air entering the blood vessels of the uterus.
How does the procedure work?
Before hysteroscopy, the woman is placed in a gynecological chair. General anesthesia is mainly used; doctors also use regional anesthesia.
The doctor disinfects the area of the external genital organs and the inner femoral surface with a special solution, after which he inserts a vaginal speculum and exposes the cervix. Next, a probe with Hegar dilators is inserted into the uterine cavity, after which a special liquid or gas is poured into it.
Did you know? The first sterilization of a woman was performed using a hysteroscope.
After this, a hysteroscope is inserted, which helps the doctor examine the size and shape of the uterus, its walls and possible pathologies. The doctor examines the color, texture and thickness of the internal mucous membrane and determines its correspondence to a specific day of the menstrual cycle.
The surface of the uterus in an enlarged form is visible on the monitor. If the doctor sees an abnormality that he can remove, he will immediately begin microscopic surgery.
The actions taken are recorded on disk. After the examination, the specialist removes the hysteroscope and the cervix is closed. After the anesthesia wears off and the patient awakens, medical workers monitor her condition for 2–3 hours.
Important! After hysteroscopy, taking a bath, visiting the sauna and steam bath, sexual intercourse and physical and psychological stress are strictly prohibited for 2 weeks. Hysteroscopy in preparation for IVF: video
https://youtu.be/joBOE1_WQjA
Price
You can have a hysteroscopy performed as prescribed by a doctor completely free of charge. It is carried out in most public hospitals and clinics, as well as at antenatal clinics. However, be prepared for the queue for the procedure to be impressive.
If you need to get the examination done faster, you should contact a private clinic that provides similar services. The cost can vary - from the basic 4-7 thousand for a diagnostic procedure to 30 thousand rubles for hysteroscopy with RDV and subsequent histological analysis of tissue from the uterine cavity. The best option for a woman planning IVF is to have a hysteroscopy with the doctor who will plan the IVF protocol.
What tests need to be done before hysteroscopy?
• A general blood test, as before most operations, allows you to assess the woman’s initial condition, this is important in order to predict tissue healing and an adequate immune response.
• Determination of electrolyte balance.
• Blood for HIV, hepatitis B and C, syphilis.
• Determination of hCG levels to exclude possible pregnancy, which is a contraindication to hysteroscopy.
• Screening for STIs and bacterial vaginosis.
• Papanicolaou test (cytological smear).
Hysterosapingography and ultrasound are less effective than hysteroscopy for assessing the uterine cavity.
MRI is performed when it is necessary to differentiate the septum from a bicornuate uterus.
To determine the cause of dysmenorrhea, for example, heavy periods, irregular bleeding, prolonged periods and in women who have not had periods for at least 6 months, an endometrial biopsy is performed.
In each case where tissue excision was performed, a biopsy is indicated.
Diagnostic hysteroscopy
During a hysteroscopic examination, the uterus is examined, allowing to assess the condition of the endometrium and identify the following pathologies:
- hyperplasia of the uterine mucosa;
- adnexal adenomyosis;
- polyps and adhesions in the reproductive organ;
- submucosal nodes;
- endometriosis;
- uterine cancer.
All these diseases can cause infertility. Hysteroscopy helps to identify and eliminate them in a timely manner.
The research is carried out as follows:
- Anesthesia is administered.
- The cervical canal is expanded using a special device.
- A hysteroscope (a thin tube equipped with a camera) is inserted into the cavity of the reproductive organ.
- The uterus is filled with gas or liquid, thus expanding it for a full examination.
- The image from the device is transmitted to the monitor screen.
- If necessary, curettage is performed.
- The biomaterial is placed in a container and sent for histological examination.
- All instruments are removed.
After the anesthesia wears off, the woman can leave the medical facility. In the future, she just needs to adhere to all medical recommendations.
The results obtained serve as the basis for choosing a strategy in preparation for in vitro fertilization.
Advantages of this procedure
Hysteroscopy before IVF is necessarily performed if there have already been several unsuccessful attempts at embryo transfer. Among the main advantages of this procedure is its high information content. The monitor clearly shows the condition of the inner layer of the reproductive organ. Thanks to this, it is possible to identify the pathological processes developing in it. Ultrasound examination will not give such a detailed picture.
In addition, when removing uterine polyps, curettage and dissection of adhesions, other tissues are not damaged. There is no need for an abdominal incision. The method is considered absolutely safe.
When performing this procedure, it is possible to terminate the pregnancy in a gentle way. Thanks to this, the chances of a positive IVF result are significantly increased.
Minuses
The main disadvantage of the method is limited capabilities. With its help, it is possible to dissect adhesions in the cervical canal and the reproductive organ itself, to remove polyps, fibroids and pathological foci of the endometrium. However, it is impossible to obtain information about the condition of the ovaries and distant parts of the fallopian tubes. It is in these areas that neoplasms and adhesions are localized, preventing successful conception.