Proper functioning of the ovaries is important for planning pregnancy and its normal course. The ovaries are involved in the production of sex hormones, where the egg matures and releases from the follicle. Next, the egg must descend into the uterus through the fallopian tube.
The inflammatory process of the fallopian tubes and ovaries (salpingitis, oophoritis) disrupts the normal process of ovulation and the movement of the egg into the uterus. This applies to a greater extent to salpingitis, especially bilateral salpingitis. In the most serious cases, obstruction of the lumen of the tubes with scar tissue is observed with the development of their obstruction. In the case of isolated left-sided or right-sided salpingitis, the second tube retains its functional purpose and conception is possible in this case.
Salpingitis is an inflammatory process of the fallopian (uterine) tube. If one tube (left or right) is involved in the process, left-sided salpingitis or, respectively, right-sided salpingitis occurs. In the case of an inflammatory process in both fallopian tubes, bilateral salpingitis develops.
Causes of salpingitis
The microbial factor plays a leading role in the development of salpingitis. Salpingitis is caused by staphylococci, Escherichia coli, streptococci, Proteus, gonococci, Trichomonas, chlamydia, fungi and Mycobacterium tuberculosis. In the latter case, tuberculous salpingitis develops. In most cases, salpingitis is caused by associations of microorganisms (staphylococci and Escherichia coli).
Along with the microbial factor, provoking factors are of great importance. These include childbirth, abortion, intrauterine contraception, hysteroscopy, hysterosalpingography, which weaken the barrier mechanisms of the cervix. Behavioral factors are also important: early onset of sexual activity, sexual relations during menstruation, a large number of sexual partners and a high frequency of sexual contacts.
Signs of salpingitis
Currently, acute salpingitis with classic symptoms is rare, which is associated with the use of antibiotics and modification of pathogens. Acute salpingitis is characterized by increased body temperature, pain in the lower abdomen, and in the sacral area. Pain in acute salpingitis often radiates to the rectum. Acute salpingitis is accompanied by weakness, headache, deterioration of general condition, and frequent urination.
When examining a patient with acute salpingitis, an enlarged and sharply painful fallopian tube is identified. With left-sided salpingitis - on the left, with right-sided salpingitis - on the right, infiltration is determined in the area of the uterine appendages due to tissue swelling. Inflammatory infiltration and pain on both sides are observed with bilateral salpingitis.
Acute right-sided salpingitis sometimes causes some difficulties in diagnosis. Localization of pain on the right leads to the wrong direction - it is possible to suspect appendicitis if the pain appears for the first time and is accompanied by nausea, vomiting, weakness and fever. Therefore, a woman in such situations should be examined by a surgeon and a gynecologist. With chronic right-sided salpingitis, pain in the lower abdomen on the right worries periodically and the woman already knows about her diagnosis and is seen by a gynecologist.
Treatment of oophoritis
Treatment of chronic and acute oophoritis differs.
In case of acute oophoritis, a course of antibacterial therapy is prescribed using broad-spectrum antibiotics, often in combination with sulfonamide drugs. Painkillers and anti-inflammatory drugs are used, bed rest is advisable, and an ice pack is applied to the area of the affected ovary to relieve pain. When the signs of acute inflammation subside, they resort to physiotherapeutic procedures: electrophoresis, laser therapy, magnetic therapy, UHF and microwave therapy, etc. Treatment of oophoritis in acute form is carried out in a hospital setting.
Treatment of chronic oophoritis must be carried out consistently and persistently, otherwise it may result in loss of ovarian function. Antibacterial therapy is also used to treat chronic oophoritis, taking into account the identified microflora. Anti-inflammatory steroid drugs are prescribed. The main efforts are aimed at eliminating the infection and combating the adhesive process, for which injections and electrophoresis of absorbable drugs are prescribed. Physiotherapy and balneotherapy are the main methods in the treatment of chronic oophoritis.
It is necessary to understand that treatment of chronic oophoritis will require changing your usual lifestyle to a healthier one. General strengthening procedures are needed that stimulate the body's own defenses, switch to a healthy diet, give up bad habits and increase physical activity to eliminate congestion in the pelvis. Only if all these conditions are met can we talk about the possibility of a complete cure.
Signs of subacute salpingitis
When the acute process in the fallopian tubes subsides (subacute salpingitis), the woman’s general condition improves, pain in the lower abdomen decreases, and a decrease in body temperature is noted. When examined, the uterine appendages have clearer contours and are less painful due to reduced inflammation and swelling. During inflammation, the ends of the fallopian tube can become obliterated (closed), resulting in exudate accumulating in the cavity of the tube. In this case, the fallopian tube looks like a saccular formation. The exudate inside can be serous or purulent, in which case purulent salpingitis develops.
Signs of purulent salpingitis
Purulent salpingitis is a complication of exudative salpingitis. With purulent salpingitis, the woman’s condition sharply worsens: fever, chills occur, and intoxication increases (dry coated tongue, decreased blood pressure, tachycardia). Palpation of the abdomen is sharply painful, the muscles of the anterior abdominal wall are tense. Vaginal examination reveals a sharply painful, significantly enlarged fallopian tube. Purulent salpingitis is accompanied by symptoms of pelvioperitonitis - local limited peritonitis, which occurs due to infection of the pelvic peritoneum. When purulent contents break into the abdominal cavity, purulent salpingitis leads to diffuse peritonitis.
When purulent salpingitis is diagnosed, conservative treatment is not effective. In this case, only surgical treatment is indicated - removal of the focus of purulent destruction. But even in cases of unilateral tubectomy (removal of the fallopian tube) for purulent salpingitis, a woman after completion of rehabilitation can be referred for IVF.
Signs of chronic salpingitis
At chronic salpingitis, the general condition of the woman is satisfactory, normal body temperature, pain in the lower abdomen is persistent, but not very pronounced. The examination reveals a thickened, painful fallopian tube with limited mobility. Chr. Salpingitis occurs with exacerbations, which are provoked by various factors - overwork, hypothermia, concomitant infections, stress.
There are two options for exacerbations of salpingitis. In one case, an exacerbation is associated with an increase in the pathogenic properties of the same pathogens or the presence of another (secondary) infection. In this case, discharge from the genital tract, significant pain in the area of the uterine appendages during examination, and low-grade fever are observed. In the second variant of exacerbation of chronic In case of salpingitis, the symptoms of a violation of the woman’s general condition come to the fore: prolonged deterioration in health, weakness, increased irritability, and the role of the microbial factor is minimal. The examination reveals dense, moderately painful, enlarged uterine appendages. Chr. salpingitis can also be left-sided or right-sided.
Acute salpingoophoritis
The first symptom of acute salpingoophoritis is intense pain in the lower abdomen on the side where inflammation develops. As the inflammatory process in the appendages develops, the pain can not only intensify, but also become diffuse. In this case, the patient cannot say exactly where it hurts and complains of abdominal pain, sometimes radiating to the lower back or rectum.
Body temperature rises to significant levels (above 38°C), chills, dysuria and bloating often appear. The patient's general condition is deteriorating, and symptoms of intoxication are increasing - headache, nausea and loss of appetite.
A gynecological examination reveals the presence of severe cervicitis and a large amount of purulent or serous-purulent leucorrhoea. Palpation of the appendage area is sharply painful, symptoms of muscular protection of the anterior abdominal wall are pronounced. If you still manage to palpate the appendages, they are determined in the form of a painful doughy conglomerate without clear boundaries.
A general blood test indicates the presence of severe inflammation: the number of leukocytes and ESR increases.
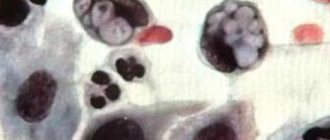
Microscopy of a smear of vaginal discharge and the cervical canal reveals an increased number of leukocytes, abundant coccal or other opportunistic flora. With a specific infection, gonococci are detected in smears.
Acute salpingoophoritis can be cured completely only with early detection and adequate treatment. Unfortunately, patients much more often seek help not at an early stage of the disease, but after unsuccessful attempts at self-treatment.
In uncomplicated situations, the symptoms of acute salpingoophoritis last no more than ten days, after which the inflammation acquires the features of a subacute and then a chronic process. The pain gradually subsides, and the patient’s general well-being improves significantly. This condition is mistakenly perceived by patients as recovery, while the process begins to acquire the features of a chronic, sluggish infection.
The most serious complications of acute purulent salpingoophoritis include:
— Accumulation of pus in the space delimited by the rectum and uterus with the formation of an abscess. One of the forms of local limited peritonitis.
- Diffuse purulent inflammation - pelvioperitonitis. It develops when the infection passes from the uterine appendages to the surrounding tissues or as a result of the opening of purulent formations in the appendages with subsequent spillage of purulent contents onto the surrounding tissues.
— Suppuration of the fallopian tube – acute purulent salpingitis. A cavity filled with pus forms in the tube - pyosalpinx.
- Tuboovarian abscess. As a result of purulent melting of the tissues of the fallopian tube and the ovarian wall, a single cavity with a capsule filled with pus is formed.
Complicated acute purulent salpingoophoritis requires immediate hospitalization and surgical intervention.
More often, exacerbation of salpingoophoritis is not accompanied by a bright clinical picture and has features of subacute inflammation.
Features of bilateral salpingitis
Bilateral salpingitis is more severe than unilateral salpingitis. A woman is worried about weakness, chills and fever, pain that covers the entire lower abdomen, frequent urination, pain or bleeding during sexual intercourse, abnormal leucorrhoea or vaginal discharge. Bilateral salpingitis is diagnosed by gynecological examination, ultrasound, echography, and, if necessary, laparoscopy.
With bilateral salpingitis, the likelihood of involvement of surrounding tissues in the process is several times higher than with isolated left-sided or right-sided salpingitis. A sluggish chronic inflammatory process leads to the formation of adhesions between the tubes, ovary and surrounding tissues. Therefore, chronic bilateral salpingitis is dangerous in terms of obstruction of both tubes and the development of tubal infertility.
Often, for chronic bilateral salpingitis, laparoscopic operations are resorted to. Detected adhesions are dissected, the normal location of the pelvic organs is restored, and the patency of the fallopian tubes is necessarily assessed. In case of chronic bilateral salpingitis, reconstructive plastic surgeries are performed - salpingotomy and salpingostomy, the purpose of which is to restore the patency of the fallopian tube.
Symptoms and course of the disease
The disease begins from the moment the infectious agent penetrates the lumen of the fallopian tube.
The infectious process goes through several stages in its development, each of which has a radically different symptomatology. Immediately after the invasion, the latent stage begins, which conceals the pathology from the patient and specialists and the onset of the infectious disease. During this period, bacteria do not actively grow, but only begin to colonize the walls of the fallopian tube.
After 5-20 days, depending on the strain of the pathogen, the stage of advanced clinical manifestations begins, characterized by a varied clinical picture. Symptoms of salpingoophoritis at this stage are represented by persistent and severe pain, localized in the umbilical-pubic-inguinal region, radiating to the lower back.
Bilateral salpingoophoritis is also combined with an infectious-toxic syndrome, which begins in response to intoxication with bacterial toxins or the inflammatory reaction itself. Spread headaches, muscle pain (especially in the extremities) appear, the temperature increases and the deterioration of the condition progresses.
Right-sided or left-sided salpingoophoritis have a less pronounced intoxication syndrome. After the acute form, either the patient’s convalescence begins and the clinic fades, or the process becomes chronic.
With an exacerbation of a chronic disease, signs of dysfunction of the reproductive system and disruption of the menstrual cycle are observed: inconsistent cyclic bleeding, oligo- or polymenorrhea, algodysmenorrhea, anovulatory cycles. The symptoms and drug treatment of tuberculous lesions of the fallopian tubes are very different from other forms: clinical manifestations are scanty, patients complain of infertility, which makes it possible to identify the pathological process.
A few words about tuberculous salpingitis
With tuberculous salpingitis, there must be a primary focus in the lungs, intrathoracic, intra-abdominal lymph nodes or bone tissue. Tuberculous salpingitis in most cases is chronic, and acute phenomena are observed only with a caseous process. The most common symptoms of tuberculous salpingitis are bloody discharge from the genital tract, pain in the lower abdomen, and severe pain during menstruation. When examined, most women exhibit enlarged appendages. The diagnosis is made on the basis of a biopsy - tuberculous granulomas are found in the endometrium.
Inflammation of the uterine appendages (salpingitis and oophoritis)
The term “adnexitis” defines the inflammatory process of the uterine appendages - tubes (salpingitis), ovaries (oophoritis) and ligaments. It should be noted that the inflammatory process in the fallopian tubes is rarely limited to isolated damage to the tubes. In the absence of treatment, the ovary is involved in the inflammatory process, in which case adnexitis occurs - salpingitis and oophoritis at the same time. This happens because the pelvic organs are closely connected. Adnexitis (salpingitis and oophoritis) is a common reason for visiting a gynecologist.
Bilateral salpingoophoritis
Bilateral infectious inflammation of the uterine appendages is much less common than unilateral one. The causes, symptoms and stages of development of the disease are similar to those with unilateral inflammation of the appendages.
Bilateral salpingoophoritis has only one distinctive feature - the symmetry of pathological processes in the ovaries and uterine tubes. Bilateral salpingoophoritis develops after opportunistic or pathogenic microflora enters both fallopian tubes, followed by infection of both ovaries.
Chronic bilateral salpingoophoritis is an absolute cause of infertility. In the case of a unilateral infectious lesion of the uterine appendages, the woman is left with one healthy tube and one healthy ovary, and the chance of pregnancy remains. If the infectious-inflammatory process covers all the uterine appendages, the likelihood of pregnancy decreases sharply.